Abstract
Objective:
To develop and evaluate the validity of a self-report measure of sleep practices for youth 8–17 years.
Methods:
Following recommended guidelines for the development of patient reported outcomes (PROs), sleep practice concepts were identified through expert (n=8) and child (n=28) concept elicitation interviews and a systematic literature review. Items were developed based on these concepts and tested in cognitive interviews with children (n=32). Psychometric analyses were applied to item response data collected from a diverse sample of youth 8–17 years (n=307). Construct validity was evaluated through tests of associations between sleep practices and sleep disturbance and sleep-related impairment. Finally, clinical validity of the tool was assessed by comparing scores of youth with and without a parent-identified sleep problem.
Results:
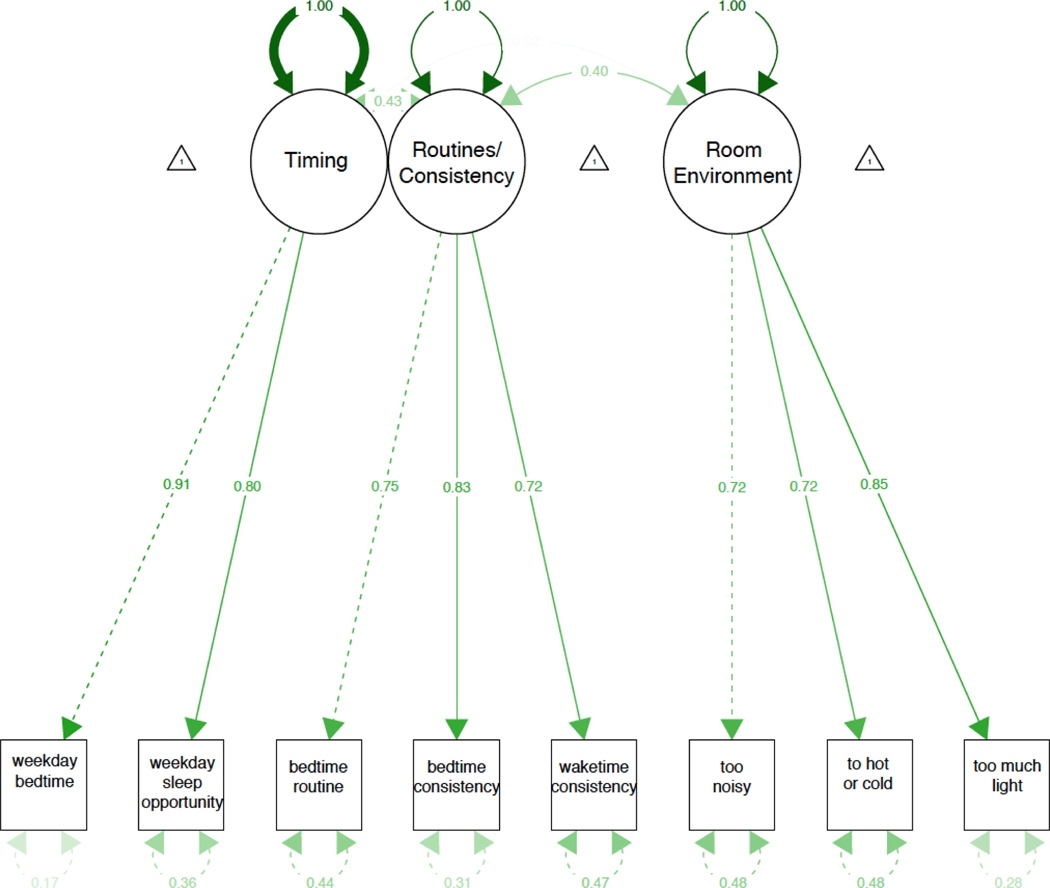
The final Pediatric Sleep Practices Questionnaire (PSPQ) included 15 items that were used to identify 5 sleep practices: sleep timing, sleep routines and consistency, technology use before bedtime, sleep environment, and the need for parental presence to fall asleep. A confirmatory factor analysis supported the hypothesized structure (all factor loadings ≥ 0.72) and PSPQ indices were significantly associated with self-reported sleep disturbances and sleep-related impairment. Finally, children with parent-reported sleep problems had shorter sleep opportunity, later bedtimes, greater need for parental presence, poorer bedtime routines, and more technology use than children without parent-reported sleep problems.
Conclusions:
The PSPQ was developed using best-practice PRO development methodology. The PSPQ can be used in clinical settings and for research assessment to capture modifiable sleep practices that may promote or interfere with healthy sleep.
Keywords: Person-reported outcome, sleep timing, sleep routines, pediatrics, sleep practices
Introduction
Just as health is not the absence of an illness, healthy sleep is not simply the absence of a sleep disorder (Buysse, 2014; Morgenthaler et al., 2015). Healthy sleep, including sufficient sleep duration and optimal sleep quality, is critical for overall health and well-being in children and adolescents. Numerous studies have demonstrated that insufficient and/or poor quality sleep result in impairments to cognitive and academic functioning (Beebe, 2011; Dewald, Meijer, Oort, Kerkhof, & Bogels, 2010; Short et al., 2018), increased negative mood and difficulties with emotion regulation (Dewald et al., 2010; Gregory & Sadeh, 2016), and poorer physical health outcomes (Chaput et al., 2016). However, sleep is a complex behavior that is influenced by intrinsic factors, including physiological sleep disorders (e.g., obstructive sleep apnea, periodic limb movements in sleep) (Mindell & Owens, 2015) and shifts in the circadian rhythm during puberty (Crowley, Acebo, & Carskadon, 2007), as well as extrinsic factors (e.g., neighborhood and family environment) (Bartel et al., 2016; Bartel, Gradisar, & Williamson, 2015; Hale, Emanuele, & James, 2015).
Healthy sleep practices, also referred to as sleep hygiene, are a group of extrinsic, modifiable factors that significantly impact sleep quantity and quality (Allen, Howlett, Coulombe, & Corkum, 2016; Irish, Kline, Gunn, Buysse, & Hall, 2015; Loghmanee & Cvengros, 2014). The most commonly recommended healthy sleep practices are: (1) maintain a consistent bedtime and wake time 7 nights a week; (2) establish a consistent bedtime routine; (3) limit light exposure and technology use at least 30–60 minutes prior to bedtime; (4) create a suitable room or sleep environment (e.g., cool, dark, comfortable); and (5) avoid caffeine 4–6 hours prior to sleep onset (Loghmanee & Cvengros, 2014).
A consistent sleep schedule that allows for an age-appropriate sleep opportunity has been shown to be related to total sleep time in children ages 6–10 years, with a late bedtime (after 9:00 pm) resulting in 60 minutes shorter sleep duration (Mindell, Meltzer, Carskadon, & Chervin, 2009). For adolescents, having a parent set bedtime is associated with increased sleep duration, less fatigue and sleepiness, and decreased symptoms of depression and suicidal ideation (Gangwisch et al., 2010; Short et al., 2011). Bedtime routines have also been shown to promote sleep in children, increasing sleep duration by almost one hour (Mindell et al., 2009).
Although neighborhood has been considered as a social determinant of sleep health (Hale et al., 2015), there is a paucity of research examining recommendations related to the bedroom environment, such as sleeping in a cool, dark, and comfortable room. A more recent recommendation has been for bedrooms to be technology free, with studies demonstrating that technology use (including television, computer, video games, and smart phones/tablets) prior to bedtime interferes with sleep due to these devices being stimulating, engaging, and light-emitting (which can delay the circadian rhythm) (Chang, Aeschbach, Duffy, & Czeisler, 2015; Loghmanee & Cvengros, 2014). Screen time has been associated with lower sleep efficiency, longer sleep onset latency, and poorer sleep quality in both children and adolescents (Bruni et al., 2015; Dube, Khan, Loehr, Chu, & Veugelers, 2017; Galland et al., 2017). Although the American Academy of Pediatrics has recommended that all technology be removed from the bedroom (Council on Communications and the Media, 2013), 96% of adolescents use technology in their bedroom in the hour before bedtime (Gradisar et al., 2013).
Avoidance of caffeine is also commonly recommended to promote healthy sleep. However, the regular consumption of caffeine is common, with 63% of school-aged children and 83% of adolescents consuming caffeine at least once a week (Mitchell, Knight, Hockenberry, Teplansky, & Hartman, 2014). Studies have consistently found that children and adolescents who consume caffeine regularly have a shorter sleep duration (Calamaro, Thornton, & Ratcliffe, 2009; Drescher, Goodwin, Silva, & Quan, 2011; Meltzer et al., 2013a; Mindell et al., 2009).
Finally, while falling asleep independently is not a common sleep practice recommendation for school-aged children and adolescents, this extrinsic sleep onset association can be highly disruptive for both the child and the parent. Although primarily studied in young children, one study found that 22% of school-aged children (6–10 years) required a parent present at bedtime at least a few nights every week, and that 26% of these children had at least one parent-reported waking per night (Mindell et al., 2009).
Despite the importance of healthy sleep practices, there are few pediatric self-report measures of sleep practices. It is important to ask children and adolescents directly about their own sleep; as children get older parents become less involved with sleep routines and thus may not be accurate reporters (Mindell et al., 2009; Waters, Stewart-Brown, & Fitzpatrick, 2003; Wolfson & Carskadon, 1998). Only three self-report measures of sleep hygiene/sleep practices have been validated, the Children’s Sleep Hygiene Scale (Harsh, Easley, & LeBourgeois, 2002); the Adolescent Sleep Hygiene Scale (Storfer-Isser, LeBourgeois, Harsh, Tompsett, & Redline, 2013); and the Children’s Report of Sleep Patterns (Meltzer et al., 2013b; Meltzer et al., 2014); however, none include all relevant concepts, as further discussed below. Thus, there is a need for a self-report measure of sleep practices for children and adolescents that is comprehensive, conceptually derived, stakeholder informed, understandable, and developmentally appropriate. Such a measure could be used in both clinical and research settings to assess the presence of factors that promote or interfere with sleep. Therefore, the purpose of this study was to develop and validate a new self-report measure of pediatric sleep practices for children and adolescents (ages 8 to 17 years). The development of the Pediatric Sleep Practices Questionnaire (PSPQ) followed recommended guidelines for the development of patient reported outcomes (PRO) (HealthMeasures, 2017; Lasch et al., 2010). As this was a multi-step process, we present the methods and results from the qualitative development of the PSPQ items as Study 1, and the methods and results of the psychometric validation of the PSPQ items as Study 2.
The Children’s Hospital of Philadelphia’s (CHOP) Institutional Review Board reviewed and approved all study procedures (protocol numbers 15–012503 and 16–013083). Parents provided informed consent for children, and children assented to participate.
Study 1: Qualitative Development and Evaluation of the PSPQ
Methods
Sleep practice concepts were identified through (1) expert concept elicitation interviews, (2) child concept elicitation interviews, and (3) a systematic literature review to identify concepts measured by existing self- or parent-report sleep health measures. Based on these concepts, healthy sleep practice items were developed, and cognitive interviews with children were used to ensure these items were meaningful, developmentally appropriate, and understandable.
Expert concept elicitation interviews
Eight pediatric sleep medicine experts outside the study team were invited (and agreed) to participate in a recorded semi-structured telephone interview. Experts were chosen to provide a breadth of opinions from different sub-specialties, and were selected based on both the expert’s reputation in the field and a minimum of three peer-reviewed publications in the area of children’s sleep health. Interviewees represented the disciplines of clinical psychology (n=2), neuropsychology (n=1), experimental psychology (n=1), anthropology (n=1), neurology (n=1), neuroscience (n=1), and genetics (n=1). Four of the experts had experience with the development and validation of existing pediatric sleep measures. Experts were asked to identify common antecedents and consequences of poor sleep in children. The interview questions are available from the authors upon request. Interviews were audio recorded, transcribed, and analyzed for themes using a constant comparative method (Strauss & Corbin, 1998). Two investigators identified and coded meaningful units of text and thereafter, discussed code agreements and disagreements until consensus was achieved (Lasch et al., 2010).
Child Concept Elicitation Interviews
Pediatric sleep practices concepts were further refined based on concept elicitation interviews with 28 children ages 8–17 years-old (see Table 2 for participant characteristics). To maximize the measure’s content validity for children with diverse health and sleep-related experiences, we purposively sampled children without diagnosed sleep problem (n = 7, recruited from primary care), children undergoing diagnostic testing or treatment for sleep disorders (n = 7, recruited from a tertiary care specialty sleep clinic), and children with chronic kidney disease (CKD; n = 14, recruited from a nephrology clinic). CKD is associated with a high prevalence of sleep problems (Darwish & Abdel-Nabi, 2016; Stabouli, Papadimitriou, Printza, Dotis, & Papachristou, 2016).
Table 2.
Participant characteristics: n, %
| Concept elicitation interviewees n = 28 | Cognitive interviewees n = 32 | Psychometric sample n = 307 | |
|---|---|---|---|
|
|
|
|
|
| Recruitment location | |||
| Primary care | 7, 25% | 32, 100% | -- |
| Sleep clinic | 7, 25% | -- | -- |
| Nephrology clinic | 14, 50% | -- | -- |
| Internet panel | -- | -- | 307, 100% |
| Child age | |||
| 8–12 years | 15, 54% | 16, 50% | 169, 55% |
| 13–17 years | 13, 46% | 16, 50% | 138, 45% |
| Child gender, male | 11, 39% | 16, 50% | 147, 48% |
| Child race | |||
| White/Caucasian | 19, 68% | 20, 63% | 175, 57% |
| Black/African American | 6, 21% | 4, 13% | 89, 29% |
| Other | 3, 11% | 8, 25% | 43, 14% |
| Child ethnicity, Hispanic | 1, 4% | 1, 3% | 15, 5% |
Interviewees were asked to describe instances when they had a “hard” and “easy” time sleeping. Specific probes elicited information about children’s sleep and wake routines, room environments, and other factors that affect sleep quality. The interview questions are available from the authors upon request. Interviews were audio recorded and transcribed. Two investigators worked together to identify and code meaningful “chunks” of interview text. Then, they assigned each meaningful text unit to a pediatric sleep practice facet category (see Table 1 for final facet definitions). Using a constant comparison method where concepts are developed from the data by coding and analyzing responses at the same time (Kolb, 2012), investigators generated new facets for concepts that could not be mapped to the existing framework (Lasch et al., 2010). Interviews were conducted until concept saturation was achieved (i.e., the point at which additional interviews no longer yield new information) (Brod, Tesler, & Christensen, 2009; Cutliffe, 2000).
Table 1.
Child Sleep Behavior facets: Summary of qualitative item development and review
| Interviewsa | Existing PRO measuresb | Cognitive Interview Itemsc | |||
|---|---|---|---|---|---|
| Experts n=8 | Child n=28 | n=10 | Tested | Retained | |
|
| |||||
| Timing: bedtime, wake time (eliminated “during school breaks”; not universally understood as summers vs. weekends vs. winter holiday) | 7 (88%) | 13 (46%) | 6 (60%) 1,3,5,7,8,10 | 6 | 4 |
| Bedtime | 7 (88%) | 8 (29%) | 2 (20%)3,7 | 3 | 2 |
| Wake time | −7 (88%) | 6 (21%) | 3 (30%)1,7,10 | 3 | 2 |
| Sleep opportunity | 6 (75%) | 4 (14%) | 5 (50%)1,3,5,7,8 | 3d | 2d |
| Routines and consistency : regular bedtime routine, consistent sleep schedule | 6 (75%) | 11 (42%) | 2 (20%) 1,3 | 5 | 3 |
| Bedtime routines | 3 (38%) | 8 (29%) | -- | 3 | 1 |
| Bedtime consistency | 6 (75%) | 4 (14%) | 2 (20%)1,3 | 1 | 1 |
| Wake time consistency | 6 (75%) | 4 (14%) | -- | 1 | 1 |
| Technology : use of technology immediately before bed or upon nighttime waking | 6 (75%) | 12 (43%) | 0 (0%) | 7 | 3 |
| Television/video viewing | 6 (75%) | 2 (7%) | -- | 2 | 1 |
| Computer/tablet/phone use | 5 (63%) | 10 (36%) | -- | 3 | 1 |
| Videogame playing | 4 (50%) | 1 (4%) | -- | 1 | 1 |
| Listened to music (valence unclear) | -- | 4 (14%) | -- | 1 | 0 |
| Sleep environment : noise/quiet, temperature, airflow, light | 5 (63%) | 14 (50%) | 0 (0%) | 5 | 4 |
| Noise/quiet | 3 (38%) | 8 (29%) | -- | 1 | 1 |
| Temperature (too hot and too cold) | 3 (38%) | 5 (19%) | -- | 2 | 2 |
| Light/darkness: different interpretation of dark room (too light) | 3 (38%) | 2 (7%) | -- | 2 | 1 |
| Sleep onset association : need for assistance to fall asleep | 4 (50%) | 0 (0%) | 1 (10%) 1 | 3 | 1 |
| Need someone to fall asleep | 4 (50%) | -- | 1 (10%)1 | 3 | 1 |
Number of experts and children who identified concepts for each facet (percentage within interviewee group);
Existing pediatric sleep PRO measures that include items for each facet (% of the 10 most commonly used measures): 1 = Children’s Sleep Habits Questionnaire (CSHQ);(J A Owens et al., 2000) 2 = Pediatric Sleep Questionnaire (PSQ);(Chervin et al., 2000) 3 = Sleep self-report (SSR);(Judith A Owens et al., 2000) 4 = Obstructive sleep apnea QoL;(Franco et al., 2000) 5 = Sleep Disturbance Scale for Children (SDSC);(Ferreira et al., 2009) 6 = Epworth Sleepiness Scale (ESS);(Johns, 1991) 7 = School Sleep Habits Survey (SSHS);(Wolfson & Carskadon, 1998) 8 = Pediatric Daytime Sleepiness Scale (PDSS);(Drake et al., 2003) 9 = Morningness-Eveningness Scale for Children (MESC);(Carskadon et al., 1993) 10 = Sleep Questionnaire (Simonds & Parraga);(Johnson et al., 2005);
Number of items tested in cognitive interviews and retained after child cognitive interviews;
Sleep opportunity variables were derived from bedtime and waketime.
Systematic review of existing child sleep health measures
A systematic literature review was conducted to identify child- or parent-report measures of pediatric sleep health. The search was conducted in MEDLINE, CINHAL, PsychINFO, and HaPI (Health and Psychosocial Instruments). Search terms were selected to capture constructs of the sleep experience (e.g., sleep disorders, wakefulness), self-report instruments (e.g., self-report, self-assessment), and measurement (e.g., questionnaires, health survey) within each of the databases. Searches were limited to research involving children (<18 years of age) and articles published in English. Two investigators reviewed the articles to identify sleep health PRO measures and the frequency with which they were used in published studies.
Classification of Item Concepts and Item Expression Generation
Based on the sleep concepts elicited in the expert and child interviews as well as the item concepts derived from the review of existing measures, the initial pool of pediatric sleep practice items were generated. Item concepts were transformed into child-report item expressions (questionnaire items). With the exception of bedtime/wake time questions, all used a 7-day recall period and a 5-point Likert response scale (never, almost never, sometimes, almost always, always).
Cognitive interviews
Cognitive interviewing is a qualitative method used to assess how respondents process and respond to questions, and is commonly used in measure development to identify problems with item comprehension, recall, and other cognitive processes that could be remediated through question rewording, reordering, or more extensive instrument revisions (Fortune-Greeley et al., 2009; Irwin, Varni, Yeatts, & DeWalt, 2009). In this study, cognitive interviews were conducted with 32 children ages 8–17 years (Table 2) recruited from primary care clinics. Following the PROMIS scientific specifications for cognitive interviewing, this sample size allowed for each item to be tested with 4–5 children, a number that has been found to be sufficient to determine the comprehensibility of items, which is the primary goal of the interviews (Bevans et al., 2018; Irwin et al., 2009). None of the children had previously completed a concept-elicitation interview. After completing the original 32-item Pediatric Sleep Practices Questionnaire via paper-and-pencil questionnaire, children were asked to read each item aloud, restate the item in their own words, and explain their response. Cognitive interviews were audio recorded and transcribed. Two investigators worked together to code items based on the degree to which interviewees’ understanding of the item was consistent with its intended meaning (1 = poor/different than intended; 2 = partial; 3 = fully consistent). Any differences in investigators’ ratings were resolved through discussion. Each item was initially tested with 4–5 children (at least two of whom were 8–11 years old). Items with average ratings of less than 2 were removed or iteratively revised and retested using the same cognitive interview procedures until they were adequately understood.
Results
Expert concept elicitation interviews
All experts recognized the need for improved PRO measures of pediatric sleep practices that are critical for promoting or interfering with sleep health. Almost all experts (88%) identified the need to capture the timing of sleep patterns (e.g., bedtime, wake time, sleep duration), with the majority (75%) also commenting on the importance of consistent pre-sleep routines and schedules, as well as the negative impact of technology use in the bedroom and prior to sleep onset. More than half of the experts (63%) discussed how differences in room environment can influence sleep quantity and quality, with half of the experts (50%) discussing the role of parental presence, co-sleeping, or room sharing on sleep outcomes. However, expert opinions differed regarding the age at which children can reliably and accurately report on their own sleep, in particular sleep patterns. Whereas some experts (57%) argued for reliance on parent-report until between age 10 and 12 years, other experts (43%) felt that children as young as 8 years of age can provide valid responses to developmentally appropriate questions about their room environments and pre-sleep behaviors. Table 1 shows the frequency with which experts identified sleep health concepts representative of the final facets.
Child Concept Elicitation Interviews
The room environment was identified by half of participants as interfering (e.g., too loud, too cold) or promoting (e.g., relaxing music, dark room) sleep. Many participants (46%) discussed how their bedtimes, wake times, and amount of sleep contributed to whether they had a “good night” of sleep or felt well-rested the next day. In terms of routines and consistency, participants discussed shifting their sleep schedules on weekends, with later bedtimes and wake times, while others reported that school schedules or homework resulted in later bedtimes or earlier wake times. Eight youth (29%) described having a bedtime routine that helped promote sleep. Technology use was described by 12 participants (43%), with computer/tablet/phone use the most common prior to bedtime or during the night (n=10). Based on these child interview findings we revised and expanded the pediatric sleep practices conceptual framework.
Systematic review of existing child sleep health measures
The literature search yielded 2,490 citations. Of these, 634 articles described the development or application of 329 unique PRO measures of pediatric sleep. The 10 most commonly used measures in the published research literature were included in 6 to 53 articles (M = 17.3; SD = 14.5) (Carskadon, Vieira, & Acebo, 1993; Chervin, Hedger, Dillon, & Pituch, 2000; Drake et al., 2003; Ferreira et al., 2009; Franco et al., 2000; Johns, 1991; Johnson, Wiggs, Stores, & Huson, 2005; Owens, Spirito, & McGuinn, 2000; Owens et al., 2000; Wolfson & Carskadon, 1998). They included 172 items. Of these only 19 items (11%) referred to sleep practices. Of the 10 most commonly used measures, 6 measured sleep timing (e.g., bedtime, wake time, sleep opportunity time), 2 assessed bedtime consistency, and only 1 asked about whether the child fell asleep alone. None of the 10 commonly used tools assessed bedtime or wake time consistency, the room environment, or technology use before bed or upon nighttime waking (Table 1). In addition to these 10 measures, other questionnaires that included items related to healthy sleep practices were reviewed to identify any items not previously captured.
Classification of Item Concepts and Item Expression Generation
We generated an initial pool of 32 pediatric sleep practice items (Table S1 – online supplement) based on the sleep concepts elicited in the expert and child interviews (timing, room environment, diet/caffeine, parental presence, technology, routine/consistency) as well as the item concepts derived from the review of existing measures. Since the existing measures failed to assess many of the concepts that children identified in the elicitation interviews, the item pool was largely informed by interview findings. Each item concept provided information about a single, unique, and universally applicable sleep practice.
Cognitive interviews
Of the 32 Pediatric Sleep Practices Questionnaire items tested in the cognitive interviews, 6 (19%) were retained without revision, 9 (28%) were revised and retained, and 17 (53%) were eliminated. Detailed information about the history of each item, including the original version, decision and rationale to retain or eliminate, and the final version can be found in Table S1 (online supplement). In summary, two items that referred to bedtime and wake time “during school breaks” were eliminated because they were not consistently understood. Two technology items were eliminated because their specific content was subsumed by more general technology-use items, and a third technology item was removed because it was not clearly understood. Four items about parental presence at sleep onset or falling asleep and waking up in different locations were removed because they were redundant or were not well understood. Similarly, all three diet/caffeine items were removed as they were not well understood. Upon completion of the cognitive interviews, 15 items remained, assessing sleep timing (4 items), sleep routines and consistency (3 items), technology use before bedtime (3 items), room environment (4 items), and the need for a parent or other person present to fall asleep (presence, 1 item).
Study 2: Psychometric Evaluation of the Pediatric Sleep Practices Questionnaire
Methods
Participants.
A preliminary assessment of the instrument’s psychometric properties was conducted using data collected with 307 children and adolescents ages 8–17 years. Parent reported demographic characteristics can be found in Table 2. Participants were recruited from an online panel from the US population (GfK Knowledge Panel) (Dennis, 2010; DiSogra, Dennis, & Fahimi, 2010). Sampling weights were used to create a final sample representative of the US population of children in the 2015 Current Population Study (see Forrest et al., 2018 for more details). Children were excluded if the parent reported that the child had an intellectual or developmental disability that prevented them from responding to questionnaire items.
Measures.
Socio-demographics and parent-reported sleep problem.
Children reported on their own gender and age. Parents identified children’s race and ethnicity, and were asked to identify whether their child had a sleep problem (yes/no).
Pediatric Sleep Practices Questionnaire (PSPQ).
As previously described, the final Pediatric Sleep Practices Questionnaire (PSPQ) included 15 items that measure sleep timing (4 items), sleep routines and consistency (3 items), technology use before bedtime (3 items), room environment (4 items), and the need for a parent or other person present to fall asleep (presence, 1 item).
Bedtime and wake time were scored as a number representing the first part of the 30-minute interval in military time (e.g., 8:00 p.m. to 8:29 p.m. = 20, 10:30 to 10:59 p.m. = 22.5, 6:00 to 6:29 a.m. = 6). Sleep opportunity (reported bedtime to reported wake time) was calculated as [(24 - bedtime) + wake time]. Weekend oversleep (i.e., difference between weekend and weekday sleep opportunity) was calculated as the difference between weekend sleep opportunity and weekday sleep opportunity. Bedtimes and sleep opportunity were classified based on prior studies and consensus guidelines (Gangwisch et al., 2010; Mindell et al., 2009; Paruthi et al., 2016; Wolfson & Carskadon, 1998). Because sleep opportunity includes sleep onset time, it is assumed that actual sleep duration will be shorter than sleep opportunity. For children under 13 years of age, bedtimes between 9:00 and 10:00 p.m. were classified as “late” and after 10:00 p.m. as “very late.” For children ages 13 and older, bedtimes between 10:00 and 11:00 p.m. were considered “late” and after 11:00 p.m. was considered “very late.” For children under 13 years of age sleep opportunity was considered “insufficient” if 8.5 to 9.5 hours and “very insufficient” if fewer than 8.5 hours. Sleep opportunity for adolescents (13 to 17 years) was classified as “insufficient” if between 7.5 and 8.5 hours, with fewer than 7.5 hours classified as “very insufficient.” For children of all ages, the difference between weekend and weekday sleep opportunity of 1–2 hours was consider “large” and 2 or more hours “very large.”
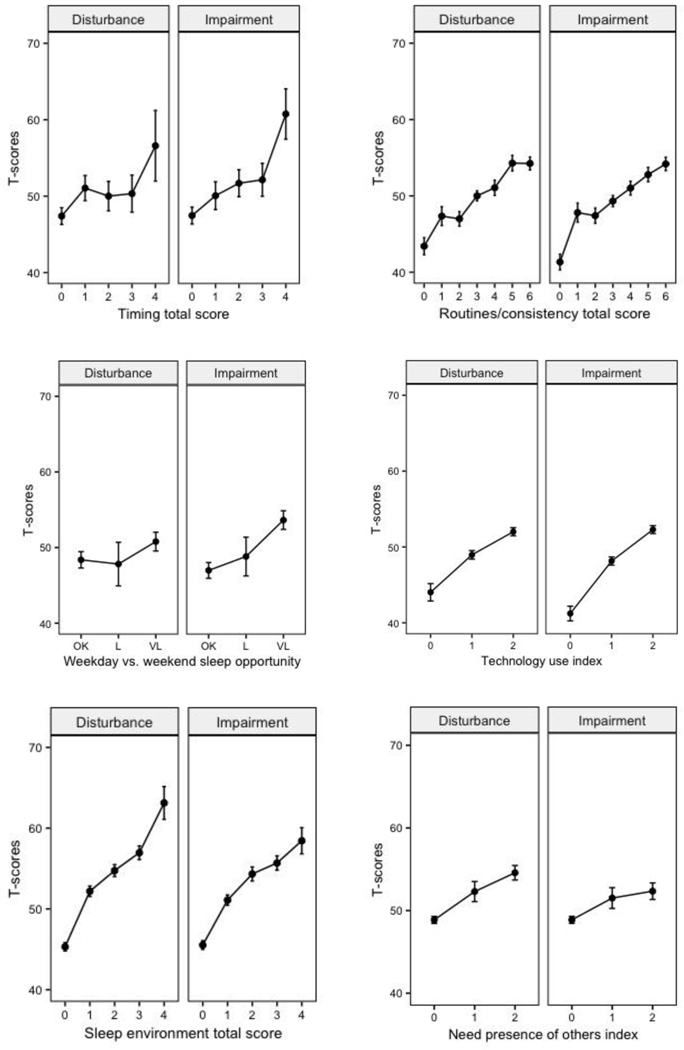
All other items used Likert response categories (never-almost never-sometimes-almost always-always), with item responses coded such that higher values indicate poorer sleep practices (e.g., inconsistent bedtime routine, frequent use of electronic devices before bed). Given the potential for overlap between the technology items, the highest response for these three items was selected to represent the frequency of their technology use before bed. Similarly, the highest response to the “too hot” and “too cold” items was selected to represent temperature discomfort of children’s room environment. Because most items were negatively skewed and the lowest response categories were infrequently endorsed, we converted 5-point response scales to 3-point scales for the purposes of scoring (Table 3). We combined categories based on visual inspection of each item’s dose-response curve, which showed average sleep disturbance and sleep-related impairment scores as a function of sleep practice frequency. Coding/scoring procedures are found in the online supplement appendix, and item dose-response curves can be seen in Figure S1 (online supplement).
Table 3.
Item-level sleep practices descriptive statistics and bivariate associations with sleep disturbance and sleep-related impairment
| Descriptive statistics | Sleep disturbance (B) | Sleep related impairment (B) | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| All Children (n = 307) | Ages 8–12 (n=171) | Ages 13–17 (n=136) | All children | Ages 8–12 | Ages 13–17 | All children | Ages 8–12 | Ages 13–17 | |
|
| |||||||||
| Weekday bedtime (time), M(SD) | 21:31 (1:01) | 21:06 (0:50) | 22:02 (1:00) | ||||||
| Recommendeda | 61% | 59% | 63% | ref | ref | ref | ref | ref | ref |
| Latea | 29% | 33% | 23% | 0.48 | 1.39 | 0.20 | 2.57 | 2.20 | 3.92 |
| Very latea | 10% | 7% | 14% | 4.70+ | 6.35 | 2.71 | 4.91* | 4.30 | 4.76 |
| Weekday sleep opportunity (h), M(SD) | 9.08 (1.20) | 9.62 (0.98) | 8.43 (1.13) | ||||||
| Recommendedb | 62% | 67% | 57% | ref | ref | ref | ref | ref | ref |
| Insufficientb | 26% | 24% | 28% | 0.83 | 1.49 | −0.31 | 2.24 | 1.33 | 2.42 |
| Very insufficientb | 12% | 9% | 15% | 3.77 | 2.40 | 3.19 | 5.46* | 5.79+ | 4.36 |
| Δ weekday vs. weekend sleep opportunity (h), M(SD) | 1.12 (1.65) | 0.53 (1.38) | 1.87 (1.63) | ||||||
| Small Δ (< 1 hour) | 58% | 72% | 41% | ref | ref | ref | ref | ref | ref |
| Moderate Δ (1–2 hours) | 8% | 9% | 6% | −1.18 | −1.94 | 1.56 | 1.33 | −0.04 | 3.45 |
| Large Δ (> 2 hours) | 34% | 19% | 53% | 2.01 | −0.08 | 1.68 | 4.97*** | 5.46* | 3.43 |
| Followed a bedtime routine, M(SD) | 1.10 (0.81) | 0.94 (0.81) | 1.30 (0.77) | ||||||
| Always (0) | 28% | 36% | 19% | ref | ref | ref | ref | ref | ref |
| Almost always (1) | 33% | 34% | 33% | 3.75**** | 3.11** | 4.41** | 3.88**** | 3.29** | 3.80** |
| Never, almost never, sometimes (2) | 39% | 30% | 49% | 6.37**** | 5.99*** | 6.43**** | 7.04**** | 6.40**** | 6.52*** |
| Tried to fall asleep at about the same time every night, M(SD) | 1.17 (0.73) | 1.11 (0.75) | 1.25 (0.71) | ||||||
| Always (0) | 20% | 23% | 16% | ref | ref | ref | ref | ref | ref |
| Almost always (1) | 43% | 43% | 44% | 3.64*** | 3.97*** | 2.91* | 3.66*** | 3.39** | 3.74* |
| Never, almost never, sometimes (2) | 37% | 34% | 40% | 8.27*** | 7.49*** | 8.53*** | 7.50**** | 6.99**** | 7.35*** |
| Woke up at about the same time every morning, M(SD) | 1.06 (0.71) | 0.99 (0.71) | 1.15 (0.69) | ||||||
| Always (0) | 22% | 26% | 18% | ref | ref | ref | ref | ref | ref |
| Almost always (1) | 50% | 49% | 50% | 3.58*** | 3.60*** | 2.95* | 4.01*** | 3.89*** | 3.15* |
| Never, almost never, sometimes (2) | 28% | 25% | 32% | 7.99*** | 9.36*** | 5.82*** | 6.81*** | 8.36*** | 4.00** |
| Technology use before bed, M(SD) | 1.38 (0.67) | 1.22 (0.70) | 1.56 (0.59) | ||||||
| Never (0) | 11% | 15% | 5% | ref | ref | ref | ref | ref | ref |
| Almost never, sometimes (1) | 41% | 47% | 34% | 4.76*** | 5.63*** | 1.58 | 5.93*** | 5.47*** | 6.23** |
| Almost always, always (2) | 48% | 38% | 61% | 7.63**** | 6.74*** | 6.13* | 9.95*** | 8.69*** | 10.22*** |
| Problems sleeping because too noisy, M(SD) | 0.25 (0.47) | 0.25 (0.48) | 0.25 (0.45) | ||||||
| Never (0) | 77% | 78% | 76% | ref | ref | ref | ref | ref | ref |
| Almost never, sometimes (1) | 21% | 20% | 23% | 6.85*** | 6.44*** | 7.14*** | 6.94*** | 6.52*** | 7.17*** |
| Almost always, always (2) | 2% | 2% | 1% | 11.01*** | 11.38*** | 12.11* | 9.48*** | 8.92** | 13.34** |
| Problems sleeping because too hot or too cold, M(SD) | 0.44 (0.57) | 0.41 (0.55) | 0.47 (0.58) | ||||||
| Never (0) | 60% | 62% | 58% | ref | ref | ref | ref | ref | ref |
| Almost never, sometimes (1) | 37% | 35% | 38% | 7.71*** | 8.96*** | 7.22*** | 6.95*** | 7.47*** | 6.08*** |
| Almost always, always (2) | 4% | 3% | 5% | 16.29*** | 14.16*** | 17.33*** | 11.39*** | 10.33*** | 11.81*** |
| Problems sleeping because too much light, M(SD) | 0.24 (0.45) | 0.23 (0.45) | 0.25 (0.45) | ||||||
| Never (0) | 77% | 79% | 76% | ref | ref | ref | ref | ref | ref |
| Almost never, sometimes (1) | 21% | 20% | 23% | 6.99*** | 6.65*** | 7.16*** | 6.76*** | 5.98*** | 7.09*** |
| Almost always, always (2) | 1% | 1% | 1% | 7.44* | 7.02* | 8.07* | 5.13* | 9.13* | 1.89 |
| Needed someone to fall asleep, M(SD) | |||||||||
| Never (0) | 77% | 69% | 87% | ref | ref | ref | ref | ref | ref |
| Almost never (1) | 9% | 10% | 7% | 2.77 | 2.59 | 4.35 | 2.33 | 1.53 | 4.44* |
| Sometimes, almost always, always (2) | 14% | 21% | 6% | 5.40**** | 5.40*** | 10.83*** | 4.09*** | 4.58*** | 8.14*** |
Notes:
Weekday bedtimes: recommended = at/before 21:00 for ages 8–12, at/before 22:00 for ages 13–17; late = after 21:00 and at/before 22:00 for ages 8–12, after 22:00 and at/before 23:00 for ages 13–17, very late = after 22:00 for ages 8–12; after 23:00 for ages 13–17.
Weekday sleep opportunity: recommended = ≥ 9.50 for ages 8–12, ≥ 8.50 for ages 13–17; insufficient = 8.50–9.50 for ages 8–12, 7.50–8.50 for ages 13–17; very insufficient = < 8.50 for ages 8–12, < 7.50 for ages 13–17.
p values using Sidak correction for multiple comparisons:
p < 0.10;
p < 0.05;
p < 0.01;
p < 0.001;
p < 0.0001.
ref = reference category
Sleep Disturbance and Sleep-Related Impairment.
Children completed the Patient Reported Outcome Measurement Information System® (PROMIS) Pediatric Sleep Disturbance (SD) and Sleep Related Impairment (SRI) item banks. The SD item bank assesses difficulties with sleep onset, sleep continuity, and sleep quality. The SRI item bank focuses on daytime sleepiness, sleep offset, and the impact of sleepiness on cognitive functioning, affect and behaviors, and daily activities. For both scales, raw to T-score conversions were established based on a large general population sample (Forrest et al., 2018), with a general population mean of 50, and standard deviation of 10. Higher scores reflect greater severity of sleep disturbances or sleep-related impairments. Both measures have been shown to be reliable, precise, and valid (Bevans et al., 2018; Forrest et al., 2018).
Procedure.
Adult members of the GfK panel, an online panel of participants in the U.S., known to have children ages 8–17 years were informed that their child may be eligible to participate in the study. Those who consented for their child’s participation were administered sociodemographic questions. Thereafter, they were instructed to ask their child to complete all three child-report questionnaires (PSPQ, PROMIS SD and SRI). Data collection continued until age and gender quotas were met, however population representativeness for other socio-demographic characteristics was not achieved through quota sampling. Therefore, weights were iteratively adjusted until the weighted sample’s distributions of gender, age, race/ethnicity, education, U.S. Census region, metropolitan area, household internet access, and language (English/Spanish) matched those in the most recent Current Population Survey (CPS) (Lohr, 2009).
Data Analyses.
Item-level means, standard deviations, and response category frequencies were calculated for all children, and for children ages 8–12 years and adolescents ages 13–17 years. We evaluated bivariate associations between sleep practice items and the sleep health outcomes (sleep disturbance and sleep related impairment) using separate linear regression models in which moderately and severely problematic levels of each sleep practice were compared to the recommended or preferred level. We fit a confirmatory factor analytic (CFA) model to the data using the lavaan package in R to assess the structural validity of the hypothesized sleep timing, routines/consistency, and room environment dimensions. Since technology and presence of another person to fall asleep were represented by a single item index, they were excluded from the factor analysis. Total scores for sleep timing, routines/consistency, and room environment were calculated by summing each scale’s respective items.
We evaluated the tool’s construct validity by testing for associations between the sleep practices scales/single item indices and both sleep disturbance and sleep related impairment using one-way analysis of variance (ANOVA) and Tukey’s multiple comparison procedure. We further evaluated PSPQ construct validity by comparing responses of children with and without parent-reported sleep problems. We used using Chi-Square analyses for single-item indicators (Δ weekday vs. weekend sleep opportunity, technology use before bed, needed someone to fall asleep) and one-way ANOVA for continuous scales (sleep timing, routines/consistency, room environment).
Results
Table 3 shows item descriptive statistics and univariate associations between sleep practices and outcomes for all children, and separately for youth ages 8–12 and 13–17 years. In an initial 3-factor CFA model, the difference between weekend and weekday sleep opportunity loaded poorly on the sleep timing factor (factor loading = 0.59). Although this item did not contribute to a sleep timing scale, we retained it as an independent indicator item. The final 3-factor CFA model adequately fit the data according to multiple fit indices (comparative fit index = 1.00, Tucker-Lewis index = 0.99, root mean square error of approximation = 0.04) and all factor loadings exceeded 0.72 (Figure 1). Pediatric Sleep Practices Questionnaire scale/index descriptive statistics and intercorrelations are shown in Table 4. We observed statistically significant, positive associations between sleep practices and outcomes. Exposure-response relationships between scores on the sleep practices scales and measures of sleep disturbance and sleep-related impairment are shown in Figure 2. Finally, as seen in Table 5, the responses for the PSPQ items and scales differed for children whose parents reported a sleep problem (n=108, 7%), with shorter sleep opportunity, later bedtimes, and more parental presence, as well as poorer bedtime routines and more technology use among children with a reported sleep problem.
Figure 1.
Confirmatory factor model containing Sleep Practice items that contribute to timing, routines/consistency, and sleep environment scales.
Table 4.
Scale-level sleep practices descriptive statistics, intercorrelations, and associations with sleep disturbance and sleep-related impairment
| Descriptive statistics | Spearman correlations | One-way ANOVA, F(p) Pairwise comparisonsa | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||||
| Scale | M (SD) | Possible range | Observed range | % min | % max | 1 | 2 | 3 | 4 | 5 | Sleep disturbance | Sleep-related impairment |
|
|
|
|
||||||||||
| 1. Timingb | 0.97 (1.22) | 0–4 | 0–4 | 50.33 | 5.69 | -- | 2.81 (< 0.05) 0,1,2,3 < 4 | 2.96 (< 0.05) 0,1 < 4 | ||||
| 2. Routines/ consistencyc | 3.34 (1.80) | 0–6 | 0–6 | 8.82 | 16.24 | 0.25 | -- | 20.62 (<.0001) 0,1,2 < 3,4 < 5,6 | 20.59 (<.0001) 0 < 1,2,3 < 4,5,6 | |||
| 3. Δ weekday vs. weekend sleep opportunity | 0.76 (0.93) | 0–2 | 0–2 | 58.0 | 34.0 | 0.37 | 0.21 | -- | 1.85 (0.1595) | 9.35 (< .001) 0 < 2 | ||
| 4. Technology use before bed | 1.38 0.67 | 0–2 | 0–2 | 10.68 | 48.22 | 0.28 | 0.30 | 0.28 | -- | 25.63 (<.0001) 0 < 1 < 2 | 46.71 (<.0001) 0 < 1 < 2 | |
| 5. Room environmentd | 0.89 (1.08) | 0–6 | 0–4 | 50.54 | 0.00 | 0.02 | 0.28 | −0.02 | 0.06 | -- | 62.19 (<.0001) 0 < 1 < 2,3 < 4 | 49.98 (<.0001) 0 < 1 < 2,3,4 |
| 6. Presence of someone elsef | 0.37 (0.72) | 0–2 | 0–2 | 77.03 | 14.42 | −0.07 | 0.09 | −0.08 | 0.03 | 0.19 | 17.53 (<.0001) 0,1 < 2 | 10.44 (<.001) 0,1 < 2 |
Notes:
Multiple pairwise comparisons using Tukey’s honest significant difference test;
weekday bedtime (time) + weekday sleep opportunity;
Followed a bedtime routine + Tried to fall asleep at about the same time every night + Woke up at about the same time every morning;
Problems sleeping because too noisy + Problems sleeping because too hot or too cold + Problems sleeping because too much light.
Figure 2.
Sleep disturbance and sleep-related impairment T-scores by sleep behavior scale/index scores
Table 5.
Comparison of PSPQ responses for children with and without parent reported sleep problem
| Parent-Reported Sleep Problem | No Parent-Reported Sleep Problem | Test statistic | |
|---|---|---|---|
|
|
|||
| Timinga: M (SD) | 1.44 (1.48) | 0.94 (1.19) | F(2,454)=0.86, p = 0.42 |
| Routines/consistencyb: M (SD) | 4.20 (1.54) | 3.26 (1.81) | F(1,927) = 3.36, p < 0.05 |
| Room environmentc: M (SD) | 1.24 (1.32) | 0.86 (1.06) | F(2,909) = 3.05, p < .05 |
| Δ weekday vs. weekend sleep opportunity: % (n) | X2(2) = 8.57, p < 0.05 | ||
| Small Δ (< 1 hour) | 33.3% (n = 9) | 60.7% (n = 256) | |
| Moderate Δ (1–2 hours) | 7.4% (n = 2) | 8.1% (n = 35) | |
| Large Δ (> 2 hours) | 59.3% (n = 16) | 32.2% (n = 138) | |
| Technology Use: % (n) | X2(2) = 4.80, p = 0.0905 | ||
| Never | 5.6% (n = 4) | 11.1% (n = 95) | |
| Almost never, sometimes | 34.7% (n = 25) | 41.5% (n = 355) | |
| Almost always, always | 59.7% (n = 43) | 47.3% (n = 404) | |
| Needed someone to fall asleep: % (n) | X2(2) = 12.56, p < 0.01 | ||
| Never | 67.6% (n = 48) | 77.9% (n = 673) | |
| Almost never | 4.2% (n = 3) | 8.8% (n = 76) | |
| Sometimes, almost always, always | 28.2% (n = 20) | 13.3% (n = 115) | |
weekday bedtime (time) + weekday sleep opportunity (possible range = 0–4);
Followed a bedtime routine + Tried to fall asleep at about the same time every night + Woke up at about the same time every morning (possible range = 0–6);
Problems sleeping because too noisy + Problems sleeping because too hot or too cold + Problems sleeping because too much light (possible range = 0–6).
Discussion
The Pediatric Sleep Practices Questionnaire (PSPQ) was developed using best-practice methodology for the development and validation of a patient-reported outcome questionnaire. To ensure that sleep practices are captured in a developmentally appropriate and clinically meaningful way, concepts were derived not only from existing measures, but also input from pediatric sleep experts and children. Cognitive interviews were utilized to ensure that items were understood by both children and adolescents. The final 15 PSPQ items assess areas known to either facilitate or interfere with sleep health in children and adolescents: sleep timing, sleep routines and consistency, technology use, the room environment, and the presence of another person at sleep onset. This study makes a significant contribution to the field as no previous measure of sleep practices has been developed using such rigorous methodology (Spruyt & Gozal, 2011).
The PSPQ sleep timing scale allows for an examination of both bedtime and sleep opportunity, two variables known to have an impact on sleep and daytime functioning. Notably, youth who reported both very late bedtimes and a very insufficient sleep opportunity also reported more sleep disturbances and greater sleep-related impairment (i.e., poorer daytime functioning). This is consistent with previous studies that have demonstrated the negative effects of both later bedtimes (Gangwisch et al., 2010; Mindell et al., 2009; Short et al., 2011) and shorter sleep duration (Beebe, 2011; Chaput et al., 2016; Gregory & Sadeh, 2016).
Having a bedtime routine and a consistent sleep schedule are also well-known to impact sleep quantity and quality. Along these lines, differences in both sleep disturbances and sleep-related impairment were found for the PSPQ sleep routines and consistency, with youth who reported an infrequent bedtime routine and/or inconsistent sleep-wake schedules also reporting greater sleep disturbances and sleep-related impairment. These inconsistencies often result in weekend oversleep (i.e., 2 or more hours more sleep on weekends/holidays) or “social jetlag” (i.e., delaying sleep-wake schedule by 2 or more hours on weekends/holidays) that is common among adolescents (Crowley, Wolfson, Tarokh, & Carskadon, 2018; Owens, 2014). In this sample, weekend oversleep was associated with greater sleep-related impairment, highlighting the significant sleep debt that builds up with insufficient weekday sleep.
With the rapid rise of available technology to children and adolescents (e.g., smartphones, tablets, laptops), there is significant concern about how these devices impact sleep quantity and quality. The PSPQ technology indicator shows a linear relationship between technology use and reported sleep disturbances and sleep-related impairment, with increased frequency of use related to more sleep disturbances and sleep-related impairment.
While few studies have examined the common recommendation for a cool, dark, and comfortable bedroom, the PSPQ room environment scale showed that youth who reported more difficulties with sleep because of noise, light, and/or uncomfortable temperatures also reported more sleep disturbances and greater sleep-related impairment. For some children and adolescents, the room environment is beyond their control (e.g., neighborhood variables, family factors). However, whenever possible a sleep promoting room environment is critical for youth.
Parental presence at bedtime is commonly seen among young children with insomnia (sleep onset associations). However, the PSPQ identified that 21% of school-aged children and 6% of adolescents continue to need someone present to help them fall asleep. Further, presence was associated with greater sleep disturbances and greater sleep-related impairment. Thus, interventions need to focus on addressing factors that may result in the need for parental presence at bedtime (e.g., anxiety).
Finally, with the commonly used screener question “does your child have a sleep problem,” the PSPQ was able to distinguish between children with and without a parent-reported sleep problem in terms of sleep duration, timing, parental presence, routines, and technology. However, further clinical validation is needed with known samples of youth with sleep disturbances and/or chronic health conditions known to disturb sleep.
Several limitations should be noted. First, children who completed concept elicitation and cognitive interviews were recruited from a children’s hospital in a large northeastern city. As such, African American children are over-represented and Hispanic children and rural residents are under-represented. In addition, the psychometric sample required parents/caregivers of participating children to be members of the GfK panel. Although substantial efforts are made to maximize diversity of this panel, some population subgroups remain under-represented (Forrest et al., 2018). Second, all questionnaires were completed by children or adolescents, with the possibilities for biased and/or inaccurate self-report. In addition, although parents were instructed to allow their child to complete the survey independently, we were unable to verify families’ compliance with this request. Future studies should include objective sleep outcomes (e.g., actigraphy) to further validate the PSPQ. Third, actual sleep duration requires questions of sleep onset latency and wake after sleep onset. As these are not measures in the PSPQ, we are only able to extrapolate “sleep opportunity.” However, without a sufficient sleep opportunity, it is not possible for a youth to obtain a sufficient sleep duration as it can be assumed that actual sleep duration is at least 15–30 minutes shorter than the sleep opportunity. Finally, further validation is needed, including test-retest reliability and responsiveness to treatment. In addition, developmental norms should be created.
The Pediatric Sleep Practices Questionnaire can be used in clinical settings and for research assessments as a way to capture different factors that may promote or interfere with healthy sleep. The PSPQ was developed using rigorous qualitative procedures, including input from pediatric sleep experts and children/adolescents, as well as cognitive interviews to ensure the appropriateness and understandability of items. Despite the large number of existing pediatric sleep questionnaires, this measure addresses a major gap in terms of a comprehensive self-report outcome measure of healthy sleep practices for children and adolescents.
Supplementary Material
Acknowledgements:
This work was funded by the Patient-Centered Outcomes Research Institute (ME-1403-12211; PI Forrest) and the National Institutes of Health (R01 HL119441; PI Meltzer).
Note: Anna de la Motte is now at Drexel University
Contributor Information
Lisa J. Meltzer, Department of Pediatrics, National Jewish Health
Christopher B. Forrest, Department of Pediatrics, Perelman School of Medicine, University of Pennsylvania
Anna de la Motte, Applied Clinical Research Center, Children’s Hospital of Philadelphia.
Jodi A. Mindell, Department of Psychology, Saint Joseph’s University, Sleep Center, Children’s Hospital of Philadelphia
Katherine B. Bevans, College of Public Health, Temple University
References
- Allen SL, Howlett MD, Coulombe JA, & Corkum PV (2016). ABCs of SLEEPING: A review of the evidence behind pediatric sleep practice recommendations. Sleep Medicine Reviews, 29, 1–14. [DOI] [PubMed] [Google Scholar]
- Bartel K, Williamson P, van MA, Cassoff J, Meijer AM, Oort F. et al. (2016). Protective and risk factors associated with adolescent sleep: findings from Australia, Canada, and The Netherlands. Sleep Medicine, 26, 97–103. [DOI] [PubMed] [Google Scholar]
- Bartel KA, Gradisar M, & Williamson P. (2015). Protective and risk factors for adolescent sleep: a meta-analytic review. Sleep Medicine Reviews, 21, 72–85. [DOI] [PubMed] [Google Scholar]
- Beebe DW (2011). Cognitive, behavioral, and functional consequences of inadequate sleep in children and adolescents. Pediatric Clinics of North America, 58, 649–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bevans KB, Meltzer LJ, De La Motte A, Kratchman A, Viel D, & Forrest CB (2018). Qualitative development and content validation of the PROMIS Pediatric Sleep Health items. Behavioral Sleep Medicine, 1–15. [DOI] [PubMed] [Google Scholar]
- Brod M, Tesler LE, & Christensen TL (2009). Qualitative research and content validity: developing best practices based on science and experience. Quality of Life Research, 18, 1263–1278. [DOI] [PubMed] [Google Scholar]
- Bruni O, Sette S, Fontanesi L, Baiocco R, Laghi F, & Baumgartner E. (2015). Technology use and sleep quality in preadolescence and adolescence. Journal of Clinical Sleep Medicine, 11, 1433–1441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buysse DJ (2014). Sleep health: can we define it? Does it matter? Sleep, 37, 9–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calamaro C, Thornton B, & Ratcliffe S. (2009). Adolescents living the 24/7 lifestyle: Effects of caffeine and technology. Pediatrics, 123, e1005–e1010. [DOI] [PubMed] [Google Scholar]
- Chang AM, Aeschbach D, Duffy JF, & Czeisler CA (2015). Evening use of light-emitting eReaders negatively affects sleep, circadian timing, and next-morning alertness. Proceedings of the National Academy of Science U.S.A, 112, 1232–1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaput JP, Gray CE, Poitras VJ, Carson V, Gruber R, Olds T. et al. (2016). Systematic review of the relationships between sleep duration and health indicators in school-aged children and youth. Applied Physiology Nutrition Metabolism, 41, S266–S282. [DOI] [PubMed] [Google Scholar]
- Council on Communications and the Media. (2013). Children, adolescents, and the media. Pediatrics, 132, 958–961. [DOI] [PubMed] [Google Scholar]
- Crowley SJ, Acebo C, & Carskadon MA (2007). Sleep, circadian rhythms, and delayed phase in adolescence. Sleep Medicine, 8, 602–612. [DOI] [PubMed] [Google Scholar]
- Crowley SJ, Wolfson AR, Tarokh L, & Carskadon MA (2018). An update on adolescent sleep: New evidence informing the perfect storm model. Journal of Adolescence, 67, 55–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutliffe J. (2000). Methodological issues in grounded theory. Journal of Advanced Nursing, 31, 1476–1484. [DOI] [PubMed] [Google Scholar]
- Darwish AH, & Abdel-Nabi H. (2016). Sleep disorders in children with chronic kidney disease. International Journal of Pediatric Adolescent Medicine, 3, 112–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis J. (2010). Knowledgepanel: Processes and procedures contributing to sample representativeness and tests for self-selection bias. Retrieved from http://www.knoweldgenetworks.com/ganp/docs/KnowledgePanelR-Statistical-Methods-Note.pdf
- Dewald JF, Meijer AM, Oort FJ, Kerkhof GA, & Bogels SM (2010). The influence of sleep quality, sleep duration and sleepiness on school performance in children and adolescents: A meta-analytic review. Sleep Medicine Reviews, 14, 179–189. [DOI] [PubMed] [Google Scholar]
- DiSogra C, Dennis J, & Fahimi M. (2010). On the quality of ancillary data available for address-based sampling. Proceedings of the American Statistical Association, 4174–4183. [Google Scholar]
- Drescher AA, Goodwin JL, Silva GE, & Quan SF (2011). Caffeine and screen time in adolescence: associations with short sleep and obesity. Journal of Clinical Sleep Medicine, 7, 337–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dube N, Khan K, Loehr S, Chu Y, & Veugelers P. (2017). The use of entertainment and communication technologies before sleep could affect sleep and weight status: a population-based study among children. International Journal of Behavior Nutrition and Physical Activity, 14, 97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forrest CB, Meltzer LJ, Marcus CL, De La Motte A, Kratchman A, Buysse DJ et al. (2018). Development and validation of the PROMIS Pediatric Sleep Disturbance and Sleep-Related Impairment item banks. Sleep. [DOI] [PubMed] [Google Scholar]
- Fortune-Greeley AK, Flynn KE, Jeffery DD, Williams MS, Keefe FJ, Reeve BB et al. (2009). Using cognitive interviews to evaluate items for measuring sexual functioning across cancer populations: improvements and remaining challenges. Quality of Life Research, 18, 1085–1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galland BC, Gray AR, Penno J, Smith C, Lobb C, & Taylor RW (2017). Gender differences in sleep hygiene practices and sleep quality in New Zeland adolescents aged 15 to 17 years. Sleep Health, 3, 77–83. [DOI] [PubMed] [Google Scholar]
- Gangwisch JE, Babiss LA, Malaspina D, Turner JB, Zammit GK, & Posner K. (2010). Earlier parental set bedtimes as a protective factor against depression and suicidal ideation. Sleep, 33, 97–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gradisar M, Wolfson AR, Harvey AG, Hale L, Rosenberg R, & Czeisler CA (2013). The sleep and technology use of Americans: findings from the National Sleep Foundation’s 2011 Sleep in America poll. Journal of Clinical Sleep Medicine, 9, 1291–1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gregory AM, & Sadeh A. (2016). Annual Research Review: Sleep problems in childhood psychiatric disorders--a review of the latest science. Journal of Child Psychology and Psychiatry and Allied Disciplines, 57, 296–317. [DOI] [PubMed] [Google Scholar]
- Hale L, Emanuele E, & James S. (2015). Recent updates in the social and environmental determinants of sleep health. Current Sleep Medicine Reports, 1, 212–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harsh JR, Easley A, & LeBourgeois MK (2002). An instrument to measure children’s sleep hygiene. Sleep, 24, A219. [Google Scholar]
- HealthMeasures. (2017). Measure Development & Research. Retrieved from http://www.healthmeasures.net/explore-measurementsystems/promis/measure-development-research
- Irish LA, Kline CE, Gunn HE, Buysse DJ, & Hall MH (2015). The role of sleep hygiene in promoting public health: A review of empirical evidence. Sleep Medicine Reviews, 22, 23–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irwin DE, Varni JW, Yeatts K, & DeWalt DA (2009). Cognitive interviewing methodology in the development of a pediatric item bank: a patient reported outcomes measurement information system (PROMIS) study. Health Quality of Life Outcomes., 7, 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolb SM (2012). Grounded theory and the constant comparative method: valid research strategies for educators. Journal of Emerging Trends in Educational Research and Policy Studies, 3, 83–86. [Google Scholar]
- Lasch KE, Marquis P, Vigneux M, Abetz L, Arnould B, Bayliss M. et al. (2010). PRO development: rigorous qualitative research as the crucial foundation. Quality of Life Research, 19, 1087–1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loghmanee DA, & Cvengros JA (2014). Promoting health sleep practices. In Sheldon SH, Ferber R, Kryger MH, & Gozal D. (Eds.), Principles and Practice of Pediatric Sleep Medicine (2nd ed., pp. 63–66). Philadelphia, PA: Elsevier. [Google Scholar]
- Lohr S. (2009). Sampling: design and analysis. Toronto, ON: Nelson Education. [Google Scholar]
- Meltzer LJ, Avis KT, Biggs S, Reynolds AC, Crabtree VM, & Bevans KB (2013a). The Children’s Report of Sleep Patterns (CRSP): a self-report measure of sleep for school-aged children. Journal of Clinical Sleep Medicine, 9, 235–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meltzer LJ, Avis KT, Biggs S, Reynolds AC, Crabtree VM, & Bevans KB (2013b). The Children’s Report of Sleep Patterns (CRSP): a self-report measure of sleep for school-aged children. Journal of Clinical Sleep Medicine, 9, 235–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meltzer LJ, Brimeyer C, Russell K, Avis KT, Biggs S, Reynolds AC et al. (2014). The Children’s Report of Sleep Patterns: validity and reliability of the Sleep Hygiene Index and Sleep Disturbance Scale in adolescents. Sleep Medicine, 15, 1500–1507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mindell JA, Meltzer LJ, Carskadon MA, & Chervin RD (2009). Developmental aspects of sleep hygiene: findings from the 2004 National Sleep Foundation Sleep in America Poll. Sleep Medicine, 10, 771–779. [DOI] [PubMed] [Google Scholar]
- Mindell JA, & Owens JA (2015). A Clinical Guide to Pediatric Sleep: Diagnosis and Management of Sleep Problems (Third ed.). Philadelphia, PA: Wolters Kluwer. [Google Scholar]
- Mitchell DC, Knight CA, Hockenberry J, Teplansky R, & Hartman TJ (2014). Beverage caffeine intakes in the U.S. Food Chemical Toxicology, 63, 136–142. [DOI] [PubMed] [Google Scholar]
- Morgenthaler TI, Croft JB, Dort LC, Loeding LD, Mullington JM, & Thomas SM (2015). Development of the National Healthy Sleep Awareness Project sleep health surveillance questions. Journal of Clinical Sleep Medicine, 11, 1057–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owens J. (2014). Insufficient sleep in adolescents and young adults: an update on causes and consequences. Pediatrics, 134, e921–e932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paruthi S, Brooks LJ, D’Ambrosio C, Hall W, Kotagal S, Lloyd RM et al. (2016). Recommended Amount of Sleep for Pediatric Populations: A Statement of the American Academy of Sleep Medicine. Journal of Clinical Sleep Medicine. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Short MA, Blunden S, Rigney G, Matricciani L, Coussens S, Reynolds M. et al. (2018). Cognition and objectively measured sleep duration in children: a systematic review and meta-analysis. Sleep Health, 4, 292–300. [DOI] [PubMed] [Google Scholar]
- Short MA, Gradisar M, Wright H, Lack LC, Dohnt H, & Carskadon MA (2011). Time for bed: parent-set bedtimes associated with improved sleep and daytime functioning in adolescents. Sleep, 34, 797–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spruyt K, & Gozal D. (2011). Pediatric sleep questionnaires as diagnostic or epidemiological tools: A review of currently available instruments. Sleep Medicine Reviews, 15, 19–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stabouli S, Papadimitriou E, Printza N, Dotis J, & Papachristou F. (2016). Sleep disorders in pediatric chronic kidney disease patients. Pediatric Nephrology, 31, 1221–1229. [DOI] [PubMed] [Google Scholar]
- Storfer-Isser A, LeBourgeois MK, Harsh J, Tompsett CJ, & Redline S. (2013). Psychometric properties of the Adolescent Sleep Hygiene Scale. Journal of Sleep Research, 22, 707–716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strauss A, & Corbin J. (1998). Basics of qualitative research: Techniques and procedures for developing grounded theory (2nd ed.). London, England: Sage. [Google Scholar]
- Waters E, Stewart-Brown S, & Fitzpatrick R. (2003). Agreement between adolescent self-report and parent reports of health and well-being: results of an epidemiological study. Child Care Health and Development, 29, 501–509. [DOI] [PubMed] [Google Scholar]
- Wolfson AR, & Carskadon MA (1998). Sleep schedules and daytime functioning in adolescents. Child Development, 69, 875–887. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.