Abstract
Objectives:
1) To determine the prevalence of overweight/obesity in adult persons with hemophilia (PwH) in Utah, and to explore the association between age, disease severity and race with BMI. 2) To provide recent data on the prevalence of overweight/obesity in the hemophilia population via a review of the literature.
Methods:
We conducted a retrospective cross section study of adult PwH who were seen at a Utah hemophilia treatment center from January 1, 2017 to December 31, 2019. The electronic database PubMed was searched for studies with observation periods from 01 January 2012 to 31 December 2019.
Results:
The age-adjusted prevalence for overweight/obesity in the adult Utah hemophilia population was higher than the overall Utah population and the general US population. After adjusting for race and age, mild hemophilia was associated with a 7.7% higher BMI (95% CI, 0.023 – 15.98%, P<0.05). Review of the literature demonstrated high levels of overweight/obesity in hemophilia communities globally with considerable heterogeneity between studies.
Conclusions:
Despite increasing awareness, prevalence of overweight/obesity in the hemophilia population remains high in comparison to the general population. There is a critical need to address this issue acutely at hemophilia treatment centers due to the considerable burden of obesity.
Keywords: Hemophilia, obesity, overweight, prevalence
Introduction
Hemophilia A and B are rare X-linked congenital bleeding disorder caused by a deficiency in coagulation factor VIII (FVIII) or factor IX (FIX), respectively. It is characterized by bleeding manifestations, including spontaneous bleeding episodes into muscles and joints, especially in persons with severe hemophilia (FVIII or FIX activity levels <1 international units per deciliter [IU/dl]) [1, 2]. Joint bleeding, which commonly affects weight-bearing joints, such as knees or ankles, can lead to the development of painful, disabling hemophilic arthropathy [3]. As a result, persons with hemophilia (PwH) often have limited exercise potential resulting in a sedentary lifestyle and difficulties in maintaining a healthy weight. Once overweight, the excess adiposity further accelerates loss-of-mobility in weight bearing joints, leading to further functional impairment [4]. This then becomes a vicious cycle that is difficult to overcome.
The use of prophylaxis clotting factor concentrates, regardless of age of initiation, is effective in reducing joint bleeding rates, total bleeding rates, and target joint bleeding [5]. More importantly, the early initiation of prophylaxis prior to age 4 years has been shown to result in preservation of overall joint motion [5]. However, this benefit was offset by having a higher than normal weight (overweight or obese) [5].
Obesity is a major public health problem in the US, especially in the adult population. From 1999 – 2000 through 2017 – 2018, the age-adjusted prevalence of obesity among US adults increased from 30.5% to 42.4% [6]. In addition, the prevalence of obesity varies by race and age groups. Among adults, the prevalence of obesity was highest in non-Hispanic black adults (49.6%) and among middle-aged adults aged 40 – 59 years (44.8%) [6].
To date, there have been several papers reviewing the epidemiological data on the prevalence of overweight and obesity in the US hemophilia population, as well as globally, with a call for increased awareness, diagnosis and recommended strategies for prevention and management [7–9]. However, these epidemiological studies occurred predominantly in the 1990s to late 2000s [10–15].
The aims of this study are 2-fold. Firstly, we set out to determine the prevalence of overweight and obesity in adult PwH in Utah and to explore the association between age, disease severity and race with BMI. Second, we sought to provide recent data on the prevalence of overweight and obesity in the hemophilia population via a systematic review of the literature.
Materials and Methods
Study population
The Utah Center for Bleeding & Clotting Disorders at the University of Utah Health is the only adult hemophilia treatment center (HTC) in the state of Utah. Adult persons with hemophilia (≥ 18 years of age) who have been seen at least once from January 1, 2017 to December 31, 2019 were included in this study. The following information were collected from the last clinic visit in the electronic medical record: age on the date of the last clinic visit, self-reported race and ethnicity, hemophilia severity, height, and weight. Race and ethnicity were reported as White, Asian, Hispanic (corresponding to White or Black race), American Indian/Alaskan Native and other.
Definitions
Hemophilia severity was classified as either severe (FVIII or FIX activity level <1 IU/dL), moderate (FVIII or FIX activity level 1 – 5 IU/dL) or mild (FVIII or FIX activity level >5 IU/dL and <40 IU/dL) [16]. PwH were divided into age categories that covered young adults (18 to 35 years), middle age (36 to 55 years), and older adults (56 years and older). Body mass index (BMI) was calculated based on the following equation, BMI = weight(kilograms)/[height (meters)]2. As per definitions by the Centers for Disease Control and Prevention (CDC), a normal BMI was defined as a BMI in the range 18.5 kg/m2 to <25 kg/m2. Underweight was defined as a BMI <18.5 kg/m2, overweight was defined as a BMI 25 to 29.9 kg/m2 and obesity was defined as a BMI ≥30 kg/m2. For the obesity category, this was further subclassified as class 1 (BMI 30 to <35 kg/m2, class 2 (BMI 35 to <40 kg/m2) and class 3 (BMI ≥ 40 kg/m2). Our focus was on the prevalence of overweight or obesity “overweight/obesity”. As this was a retrospective study, the study protocol was deemed exempt and approved by the University of Utah Institutional Review Board.
Statistical analysis for Utah study population
Descriptive statistics were used for the study population. Continuous variables were reported as medians and inter-quartile ranges (IQR). The crude prevalence of overweight/obesity was determined for the overall study population. The age-adjusted prevalence of overweight/obesity was calculated based on direct standardization to the 2000 U.S. Standard Population [17]. The prevalence of overweight and obese was also calculated for the different patient groups: age category, disease severity and race. Due to limited numbers, race and ethnicity were analyzed as non-Hispanic whites vs. all others. The chi-squared or Fisher’s exact test (when expected cell counts were less than 5) was used to compare the differences in prevalence of overweight/obesity with age, disease severity and race.
Linear regression was used to compare BMI with age, disease severity and race, where BMI was logarithmically transformed to achieve approximate normality. Hemophilia disease severity was categorized into mild or non-mild (moderate and severe) severity. We determined the percent difference in BMI corresponding to white vs non-white and mild vs non-mild disease by exponentiating the regression model coefficients, subtracting one and multiplying by 100%. Age was divided by 10 to enable interpretation of results as a 10-year increase in age. All three variables were included in the multivariable model as they were found to be associated with BMI or previously known to be associated with BMI. Ninety-five percent confidence intervals (CIs) and p-values were also reported. Statistical significance was assessed at the 0.05 level and all tests were two-tailed.
Studies selected for literature review
To determine the prevalence of overweight/obesity in the adult (≥18 years of age) hemophilia population, we searched the electronic database PubMed (https://www.ncbi.nlm.nih.gov/pubmed) for published studies where the observation period was within the last 8 years (01 January 2012 – 31 December 2019). The search strategies used are available in Supplemental Material 1. If a study encompassed at least 2 years of the specified observation period, the study was included. If the observation period was not stated, then the year of publication was used instead. References cited within these studies were also manually reviewed for additional studies of interest. Abstracts from the American Society of Hematology annual meetings (2012 – 2019), the International Society on Thrombosis and Hemostasis meetings (2012 – 2019) and the World Federation of Hemophilia biannual meetings (2012 – 2020) were also comprehensively searched. Studies specifically looking at the pediatric hemophilia population were excluded. If a study included hemophilia patients between the ages of 18 and 21, but was part of a pediatric study, the study was excluded if the adult data was not extractable. Studies specifically looking at a cohort of PwH with hepatitis B, hepatitis C, cardiovascular disease and/or HIV were excluded to avoid confounding the association between hemophilia and obesity. Articles were also excluded if they were non-English language and non-human articles, contained no original data, no relevant data, or were duplicate studies. For each study included, data regarding the number of hemophilia patients, age of the study population, country of enrolled patients and prevalence of overweight/obesity were extracted.
Statistical analysis for literature review
Studies were grouped by region (North America, Europe and global). Pooled estimates were calculated using a random-effects model. The pooled prevalence of overweight/obesity overall and by region were each expressed as weighted mean prevalence with 95% CIs. Heterogeneity among studies was quantified using between-study variance τ2, the percentage of variation due to heterogeneity rather than chance I2, and H2 statistics [18]. Cochran’s Q test assessed statistically significant differences in heterogeneity across studies. All statistical analyses were performed using the meta commands in Stata v16.1 (College Station, TX, USA) [19].
Results
Study population characteristics
A total of 149 adult PwH were seen at the Utah Center for Bleeding & Clotting Disorders at the University of Utah Health within the study period. Five PwH had no height documented and were excluded from the study. The baseline demographics of the 144 adult PwH are presented in Table 1. Over two-thirds of the study population have hemophilia A, and over half have severe hemophilia. The study population largely self-identified as White (n=124, 86.1%).
Table 1.
Baseline demographics of the 144 adult Utah PwH included in the study
| Characteristics | n | % | |
|---|---|---|---|
| Type and severity | |||
| Hemophilia A | 98 | 68.1 | |
| Mild | 29 (20.1) | ||
| Moderate | 5 (3.5) | ||
| Severe | 64 (44.4) | ||
| Hemophilia B | 46 | 31.9 | |
| Mild | 17 (11.8) | ||
| Moderate | 18 (12.5) | ||
| Severe | 11 (7.6) | ||
| Self-reported race | |||
| White or Caucasian | 124 | 86.1 | |
| Asian | 4 | 2.8 | |
| Hispanic | 8 | 5.6 | |
| American Indian and Alaska Native | 1 | 0.7 | |
| Other | 5 | 3.5 | |
| Decline to disclose | 2 | 1.4 | |
| Age category | |||
| Young adult | 84 | 58.3 | |
| Middle age | 46 | 32.0 | |
| Older adult | 14 | 9.7 | |
| BMI category | |||
| Underweight | 3 | 2.1 | |
| Normal | 45 | 31.3 | |
| Overweight | 55 | 38.2 | |
| Obese | 41 | 28.5 | |
| Class I | 24 (16.7) | ||
| Class II | 12 (8.3) | ||
| Class III | 5 (3.5) |
The subcategories for disease severity and BMI are presented as n (percentages). The percentage is based on the overall study population, n=144.
The median age was 33 years (IQR, 25 – 45). Over half of the cohort (n=84, 58.3%) were in the young adults category, whereas only 9.7% (n=14) were in the older adults category. The oldest patient was 79 years and the youngest was 18 years. The median BMI was 27.5 kg/m2 (IQR, 23.6 – 31.0), falling within the overweight range. A normal BMI was found in 31.3% (n=45), whereas 38.2% (n=55) were overweight and 28.5% (n=41) were obese. Three adult PwH were in the underweight category. The highest BMI was 45.8 kg/m2 and the lowest BMI was 17.3 kg/m2.
Prevalence of overweight/obesity
Two-thirds of the study population were either overweight (38.2%, n=55) or obese (28.5%, n=41). The age-adjusted prevalence of overweight/obesity in adult PwH and comparisons with the Utah population and general US population are shown in Table 2 [20, 21]. The age-adjusted prevalence of overweight/obesity adult PwH was 73.2% (95% CI, 58.5 – 87.7), whereas for an obese adult PwH, the age-adjusted prevalence was 31.4% (95% CI, 21.8 – 41.0). The prevalence of overweight/obesity in adult PwH in Utah based on age category, disease severity and race are shown in Figure 1.
Table 2.
Age-adjusted prevalence of overweight and/or obese in adult PwH in Utah, the general Utah population and the general US population
| Age-adjusted prevalence | Adult PwH in Utah (%, 95% CI) | Utah population (%, 95% CI)* | US population (%, 95% CI)** |
|---|---|---|---|
| Overweight or obese | 73.2 (58.5, 87.7) | 63.4 (62.2, 64.6) | 65.9 (65.5, 66.2) |
| Obese | 31.4 (21.8, 41.0) | 28.4 (27.3, 29.5) | 31.1 (30.8, 31.4) |
Figure 1.
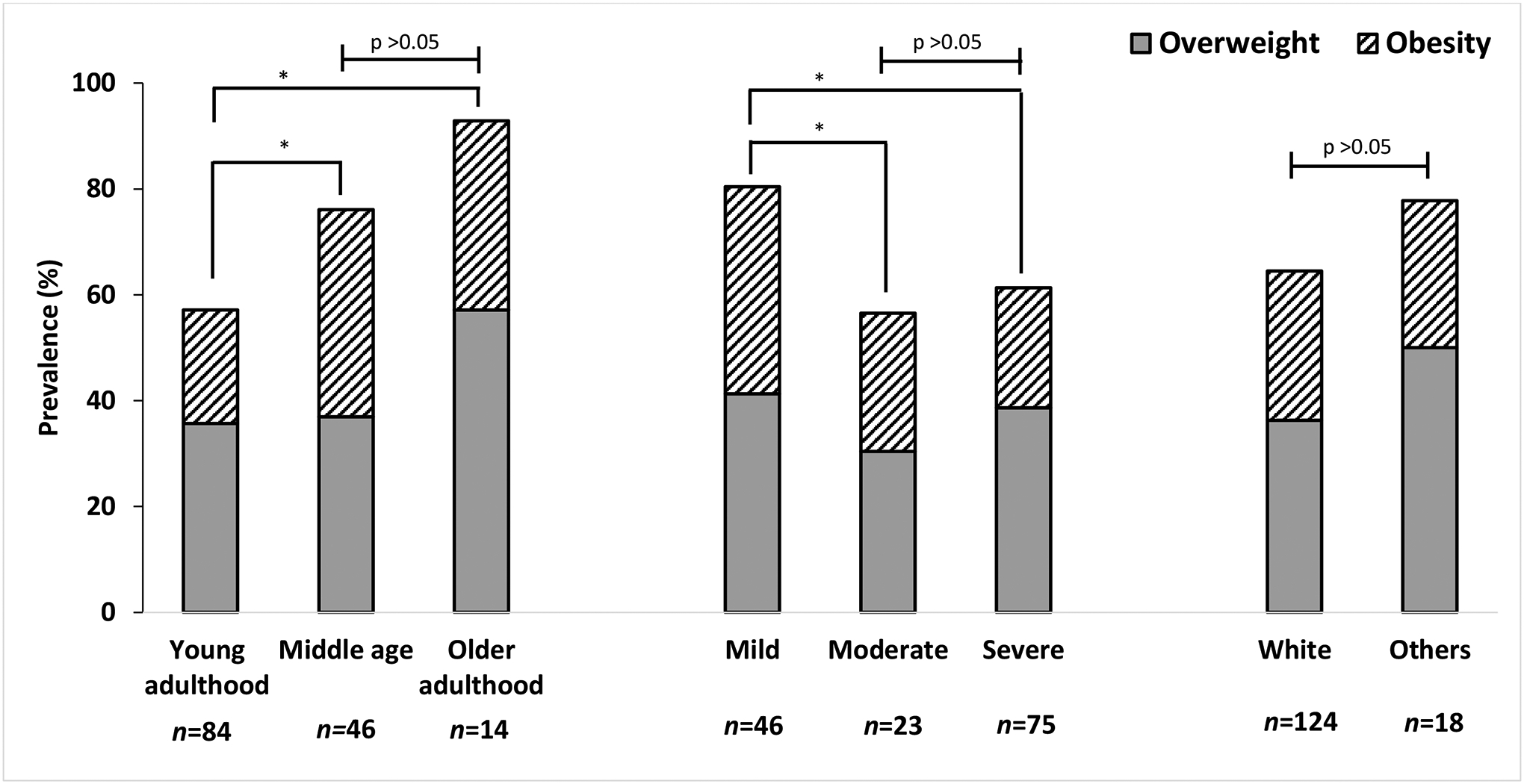
Prevalence of being overweight and obese among adult PwH in Utah based on age category, severity of disease and self-reported race
* P <0.05
Prevalence by age category, disease severity and race
Across all age categories, the majority of PwH were overweight/obese. With increasing age, the prevalence of overweight adult PwH increased from 36% (n=30) in young adults to 57% (n=8) in older adults. Similarly, the prevalence of adult PwH with obesity increased from 21% (n=18) in young adults to 36% (n=5) in older adults. The prevalence of overweight/obesity was significantly lower for PwH in young adults than for those in middle age (P <0.05) and older adults (P <0.05) (Figure 1). There was no significant difference in this prevalence between middle age PwH and those in older adults (P >0.05).
The prevalence of overweight/obesity was significantly higher for PwH with mild disease, as compared to moderate disease (P <0.05) or severe disease (P <0.05). The difference in this prevalence was not statistically significant between those with moderate and severe disease (P >0.05). There were no differences in overweight/obesity by race.
Bivariate and multivariable analysis
On bivariate analysis, persons with mild hemophilia were found to have a 10.6% higher BMI than persons with moderate or severe hemophilia (95% CI, 3.24 – 18.6%, P<0.05). For each 10-year increase with age, BMI increased by 3.16% (95% CI, 0.76 – 5.61%, P<0.05). After adjusting for race and age category, only mild hemophilia was associated with a 7.7% higher BMI (95% CI, 0.023 – 15.98%, P<0.05) (Table 3).
Table 3.
Bivariate and multivariable associations with percent change in body mass index (BMI) using data from the Utah adult hemophilia population
| Variable | Bivariate analysis | Multivariable analysis | ||||
|---|---|---|---|---|---|---|
| % Change in BMI per unit | 95% CI | p-value | % Change in BMI per unit | 95% CI | p-value | |
| White vs non-White | 1.53 | −8.1, 12.2 | 0.7663 | 0.46 | −8.97, 10.86 | 0.927 |
| Age (per 10-year increase) | 3.16 | 0.76, 5.61 | 0.0099 | 2.3 | −0.22, 4.88 | 0.074 |
| Mild vs non-mild severity | 10.6 | 3.24, 18.6 | 0.0045 | 7.7 | 0.023, 15.98 | 0.049 |
Pooled prevalence for overweight/obesity
A total of 162 records were identified and assessed for inclusion by a single reviewer (M.Y.L). Of these, 150 were excluded and 12 studies remained in the final analysis (Figure 2 and Table 4) [22–33].
Figure 2.
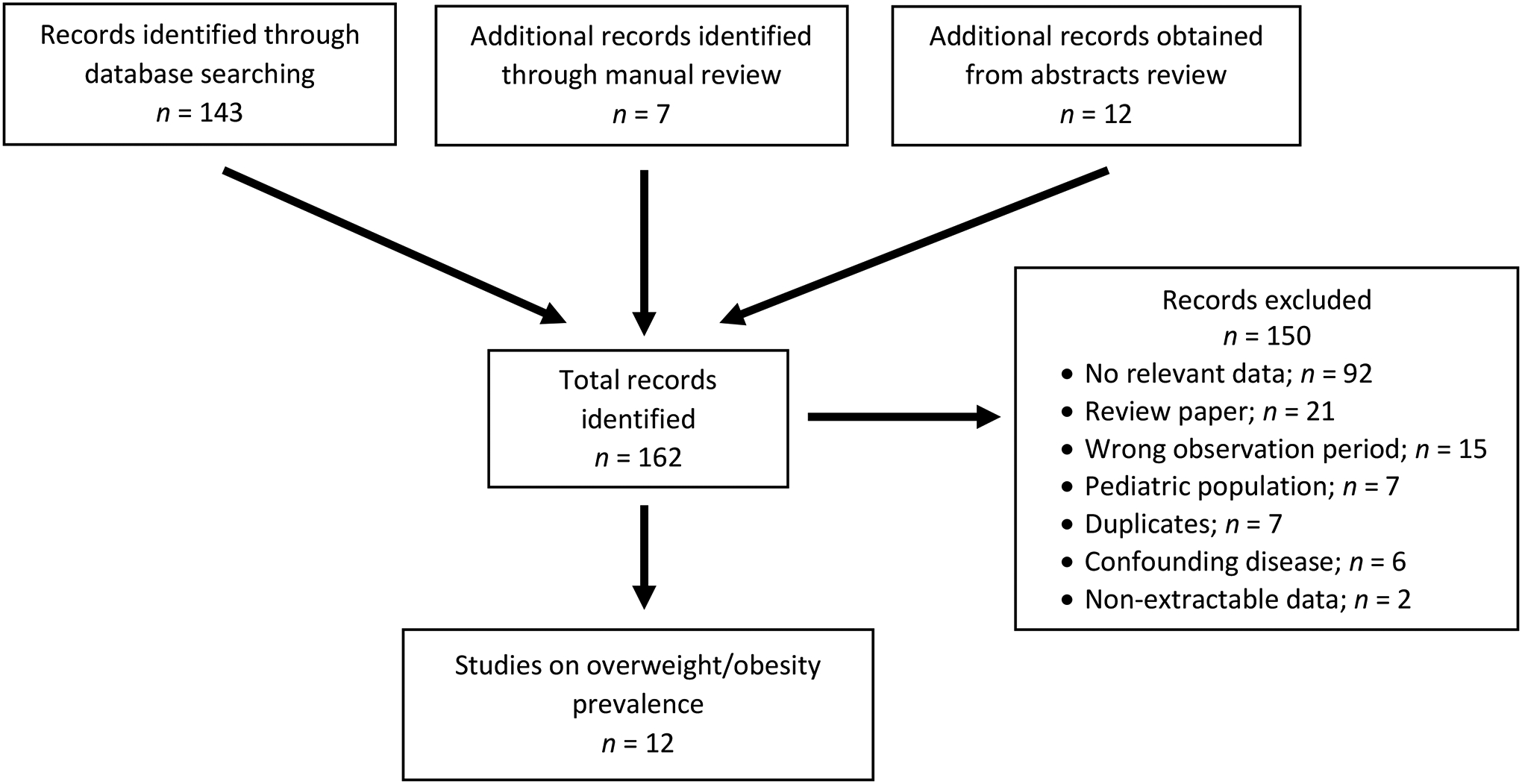
Study selection
Table 4.
Epidemiology studies for prevalence of overweight and obesity in adult PwH, 2012 – 2019
| Study | Location | Type of Study | Observation Period | Study Population | Age (yrs) | No. of PwH | Prevalence (%) | ||
|---|---|---|---|---|---|---|---|---|---|
| Overweight | Obese | At least overweight | |||||||
| North America | |||||||||
| Cisak [22] | Kentucky | Single-center | 2005–2014 | All severity HA and HB | ≥30 | 59 | 33.9% (n=20) | 40.7% (n=24) | 74.6% (n=44) |
| Ullman [23] | US | Multiple centers | 2009–2013 | All severity HB | 18–64 | 54 | NR | NR | 59.3% (n=32) |
| Sun [24] | US & Canada | Two centers | US (2011–2014); Canada (2010–2014) | All severity HA and HB | ≥18 | 135 | NR | 21% (n=29) | NR |
| Sood [25] | US | Multiple centers | 2012–2015 | Moderate/severe HA and HB | 54–73 | 200 | NR | 29.5% (n=59) | NR |
| Witkop [26] | US | Multiple centers | 2013–2014 | All severity HA and HB; History of joint bleeding or joint pain | ≥18 | 381 | 36.2% (n=138) | 28.6% (n=109) | 64.8% (n=247) |
| Europe | |||||||||
| Holme [27] | Europe | 16 centers | 2011–2013 | All severity HA and HB | ≥40 | 532 | 41.4% (n=220) | 13% (n=69) | 54.4% (n=289) |
| Olivieri [28] | Germany | Seven centers | 2015 | Severe HA with negative inhibitor history | ≥18 | 78 | 26.9% (n=21) | 7.7% (n=6) | 46.6% (n=27) |
| Hrdlickova [29] | Czech Republic | Single-center | 2016* | All severity HA and HB | ≥18 | 76 | 56.6% (n=43) | 17% (n=13) | 73.6% (n=56) |
| Von Mackensen [30] | United Kingdom | 4 centers | 2016* | All severity HA and HB | 17–66 | 50 | 38% (n=19) | 26% (n=13) | 64% (n=32) |
| Global | |||||||||
| Chang [31] | Taiwan | Two centers | 2006–2014 | Moderate/severe HA and HB | |||||
| ≥50 | 25 | 32% (n=8) | 16% (n=4) | 48% (n=12) | |||||
| Lambert [32] | Ivory Coast | Single-center | 2017 | All severity HA and HB | >18 | 25 | NR | NR | 12% (n=3) |
| Duarte [33] | Brazil | Single-center | 2019* | All severity HA and HB | ≥30 | 59 | NR | NR | 15.3% (n=9) |
Year of publication used
US, United States; yrs, years; PwH, persons with hemophilia; NR, not reported
Using epidemiological observation data from the last 8 years (2012 – 2019), the prevalence of being overweight/obese in adult PwH varied widely from 12% to 74.6%. In North America, this prevalence ranged from 59.3% to 74.6% (I2=36.98% of variability due to heterogeneity). A similar prevalence but with wider variability was seen in Europe, ranging from 46.6% in Germany to as high as 73.6% in Czech Republic (I2=92.55%). Globally, there were only 3 epidemiological studies reporting the prevalence of overweight/obese in PwH: 12% in Ivory Coast, 15.3% in Brazil and 54% in Taiwan (I2=95.40%).
The overall pooled prevalence of overweight/obesity in the global adult hemophilia population was 50.7% (95% CI, 36.9 – 64.6%) (Supplemental Figure 3A). When assessing the North American and European population alone, this estimation rose to 66.1% (95% CI, 59.6 – 72.6%) and 56.5% (95% CI, 40.4 – 72.7%), respectively.
Focusing on the prevalence of obesity only, this ranged from 7.7% in Germany to 40.7% in Kentucky, USA. The overall pooled prevalence of obesity in the global adult hemophilia population was 22.5% (95% CI, 16.3 – 28.7, I2 = 88.94%) (Supplemental Figure 3B). This estimation was higher in the North American population (28.7%, 95% CI, 22.9 – 34.5, I2 = 64.05%) but lower in the European population (14.4%, 95% CI, 8.2 – 20.6, I2 = 72.73%).
Discussion
This cross-sectional retrospective study indicates that 2 out of 3 adult PwH in the state of Utah have higher than normal weight, of which adult PwH with obesity make up 28.5%. However, given that Utah is known to be the youngest state population in the US with a median age of 31 years vs 38.2 years nationally, we calculated the age-adjusted prevalence for comparison purposes [34]. After adjusting for age, the prevalence for overweight and obese in the adult Utah hemophilia population was higher than the overall Utah population and the general US population. As for obesity, the prevalence in the adult Utah hemophilia population was higher than the Utah population but similar to the general US population. This is particularly concerning since Utah is a relatively healthy state, consistently ranking fifth from the bottom (46 out of 51) for obesity for the past 5 years (2013 – 2017) [35]. These findings are alarming and highlight a critical need to address the issue acutely at our HTC. Despite the increased awareness, we do not routinely address the impact of weight and lack a protocol to do so, similar to what has been reported by the majority of US HTCs [36, 37]. We plan to address this deficiency by formally incorporating guidelines and lifestyle interventions as described in the review by Wilding et al as part of our hemophilia comprehensive visit [8].
It has been suggested that the higher prevalence of overweight/obesity may be due to chronic hemophiliac arthropathy in the severe hemophilia population, which make up half of the overall hemophilia population. However, the association between overweight/obesity with hemophilia severity has been conflicting, either showing no association or a negative association with severe hemophilia [12, 38, 39]. In our study, we found that PwH with mild severity had higher BMI, which persisted after adjusting for age and race. To some extent, this corroborates the findings of McNamara et al who reported that severe hemophilia was associated with 15.1% lower BMI as compared to non-severe hemophilia [38]. A key difference in our study is that we looked at the association of BMI among mild hemophilia vs non-mild (moderate and severe) hemophilia. This categorization was made a priori due to the fact that more than half of the moderate severity cohort in our study were on prophylaxis factor concentrate regimen, suggesting that they had a more severe phenotype, similar to those with severe hemophilia.
Results from the literature review demonstrate high levels of overweight/obesity in hemophilia communities globally. However, the majority of epidemiological data are from North American and Europe, and there is considerable heterogeneity between studies which should lead to caution in the interpretation of the results. More data outside developed countries are needed to further clarify the prevalence of overweight/obesity in the global hemophilia population, particularly in developing countries. This need could feasibly be addressed by incorporating overweight/obesity data elements as part of the questionnaire in the World Federation of Hemophilia (WFH) Annual Global Survey that is completed nationally by WFH members. Emerging data can be used to increase awareness, and advocate for better care with targeted strategies for the hemophilia population.
Our study had several strengths. For the variables age and BMI, we determined associations using BMI classifications (normal, overweight and obese) and age categories, as well as age and BMI as continuous variables. The former method is helpful for visualization and is easier to conceptualize, but the cutoff used, especially in the age categories, can over- or under-estimate the effect seen. The use of continuous variables in a multivariable analysis removes this limitation. As for the pooled prevalence of overweight and/or obesity, we only used epidemiological studies from the past 8 years to determine a current estimate as the prevalence of obesity in the US, and globally continues to increase on an annual basis.
The main limitation of this study is that besides age, race and hemophilia severity, we did not explore other possible associations such as human immunodeficiency virus (HIV) status, hepatitis C status, chronic liver disease, or physical activity – all of which could have confounded the results. A second limitation is that there are a small number of adult PwH whose care is being actively managed by community oncology practices due to insurance restrictions. Thus, our findings may not be representative of the Utah haemophilia population. However, in the last 2 years, due to efforts from the Payer Relations and Contracting Department at our institution, the Utah Center for Bleeding & Clotting Disorders is now an in-network facility for a majority of payers, resulting in a transfer of care of adult PwH to our HTC for ongoing management. Third, our hemophilia cohort was predominantly White, which is representative of the state of Utah, but may not be generalizable to the general US population.
In conclusion, we demonstrated that the prevalence of overweight/obesity in the Utah hemophilia population is alarmingly high, especially after adjusting for age, with mild hemophilia disproportionately affected as compared to non-mild hemophilia. The obesity burden on the hemophilia population cannot be overstated given that obesity worsens hemophilic arthropathy, influences pharmacokinetics of weight-based clotting factor dosing, and is a risk factor for cardiovascular diseases, among others. If we hope to make an impact, weight management should be formally incorporated into the hemophilia care pathway, and considered equally as important as managing breakthrough bleeds during the comprehensive care visit.
Supplementary Material
Supplemental Figure 3A. Forest plot of the pooled prevalence of overweight/obesity from epidemiological studies in the past 8 years, 2012 – 2019
Supplemental Figure 3B. Forest plot of the pooled prevalence of obesity from epidemiological studies in the past 8 years, 2012 – 2019
Funding
The research reported in this publication was supported in part by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1TR002538. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict-of-interest disclosures
The authors stated that they had no interests which might be perceived as posing a conflict or bias.
References
- [1].Roberts HR KN, Escobar MA. Hemophilia A and hemophilia B. New York, NY: McGraw Hill; 2010. [Google Scholar]
- [2].Srivastava A, Brewer AK, Mauser-Bunschoten EP et al. Guidelines for the management of hemophilia. Haemophilia 2013; 19:e1–47. [DOI] [PubMed] [Google Scholar]
- [3].Soucie JM, Cianfrini C, Janco RL et al. Joint range-of-motion limitations among young males with hemophilia: prevalence and risk factors. Blood 2004; 103:2467–2473. [DOI] [PubMed] [Google Scholar]
- [4].Soucie JM, Wang C, Siddiqi A et al. The longitudinal effect of body adiposity on joint mobility in young males with Haemophilia A. Haemophilia 2011; 17:196–203. [DOI] [PubMed] [Google Scholar]
- [5].Manco-Johnson MJ, Soucie JM, Gill JC, Joint Outcomes Committee of the Universal Data Collection USHTCN. Prophylaxis usage, bleeding rates, and joint outcomes of hemophilia, 1999 to 2010: a surveillance project. Blood 2017; 129:2368–2374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of Obesity and Severe Obesity Among Adults: United States, 2017–2018. In: National Center for Health Statistics Data Brief. Centers for Disease Control and Prevention; 2020. [Google Scholar]
- [7].Kahan S, Cuker A, Kushner RF et al. Prevalence and impact of obesity in people with haemophilia: Review of literature and expert discussion around implementing weight management guidelines. Haemophilia 2017; 23:812–820. [DOI] [PubMed] [Google Scholar]
- [8].Wilding J, Zourikian N, Di Minno M et al. Obesity in the global haemophilia population: prevalence, implications and expert opinions for weight management. Obes Rev 2018; 19:1569–1584. [DOI] [PubMed] [Google Scholar]
- [9].Wong TE, Majumdar S, Adams E et al. Overweight and obesity in hemophilia: a systematic review of the literature. Am J Prev Med 2011; 41:S369–375. [DOI] [PubMed] [Google Scholar]
- [10].Fransen van de Putte DE, Fischer K, Pulles AE et al. Non-fatal cardiovascular disease, malignancies, and other co-morbidity in adult haemophilia patients. Thromb Res 2012; 130:157–162. [DOI] [PubMed] [Google Scholar]
- [11].Lim MY, Pruthi RK. Cardiovascular disease risk factors: prevalence and management in adult hemophilia patients. Blood Coagul Fibrinolysis 2011; 22:402–406. [DOI] [PubMed] [Google Scholar]
- [12].Majumdar S, Morris A, Gordon C et al. Alarmingly high prevalence of obesity in haemophilia in the state of Mississippi. Haemophilia 2010; 16:455–459. [DOI] [PubMed] [Google Scholar]
- [13].Miesbach W, Alesci S, Krekeler S, Seifried E. Comorbidities and bleeding pattern in elderly haemophilia A patients. Haemophilia 2009; 15:894–899. [DOI] [PubMed] [Google Scholar]
- [14].Sharathkumar AA, Soucie JM, Trawinski B et al. Prevalence and risk factors of cardiovascular disease (CVD) events among patients with haemophilia: experience of a single haemophilia treatment centre in the United States (US). Haemophilia 2011; 17:597–604. [DOI] [PubMed] [Google Scholar]
- [15].Ullman M, Zhang QC, Brown D et al. Association of overweight and obesity with the use of self and home-based infusion therapy among haemophilic men. Haemophilia 2014; 20:340–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Makris M, Oldenburg J, Mauser-Bunschoten EP et al. The definition, diagnosis and management of mild hemophilia A: communication from the SSC of the ISTH. J Thromb Haemost 2018; 16:2530–2533. [DOI] [PubMed] [Google Scholar]
- [17].Klein RJ S C. Age adjustment using the 2000 projected U.S. population. Healthy People Statistical Notes, no. 20. In: Hyattsville, MD: National Center for Health Statistics. 2001. [PubMed] [Google Scholar]
- [18].Higgins JP, Thompson SG (2002) Quantifying Heterogeneity in a Meta- Analysis. Stat Med 21(11): 1539–1558.. [DOI] [PubMed] [Google Scholar]
- [19].StataCorp. 2019. Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC. [Google Scholar]
- [20].Retrieved Tue, 07 July 2020 from the Utah Department of Health, Indicator-Based Information System for Public Health Web site: https://ibis.health.utah.gov/ibisph-view/indicator/complete_profile/Obe.html.
- [21].Retrieved Tue, 07 July 2020 from the Utah Department of Health, Indicator-Based Information System for Public Health Web site: https://ibis.health.utah.gov/ibisph-view/indicator/complete_profile/OvrwtObe.html.
- [22].Cisak KI, Pan J, Rai SN et al. Prevalence of Hypertension, Diabetes, Obesity and Smoking in Patients with Hemophilia Followed at a Single Treatment Center. Blood 2015; 126:4692. [Google Scholar]
- [23].Ullman M, Curtis R, Lou M et al. Is Hemophilia B Clinically Less Severe Than Hemophilia A? Evidence from the Hugs Va and Vb Studies Blood 2019; 134:58. [Google Scholar]
- [24].Sun HL, Yang M, Sait AS et al. Haematuria is not a risk factor of hypertension or renal impairment in patients with haemophilia. Haemophilia 2016; 22:549–555. [DOI] [PubMed] [Google Scholar]
- [25].Sood SL, Cheng D, Ragni M et al. A cross-sectional analysis of cardiovascular disease in the hemophilia population. Blood Adv 2018; 2:1325–1333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Witkop M, Neff A, Buckner TW et al. Self-reported prevalence, description and management of pain in adults with haemophilia: methods, demographics and results from the Pain, Functional Impairment, and Quality of life (P-FiQ) study. Haemophilia 2017; 23:556–565. [DOI] [PubMed] [Google Scholar]
- [27].Holme PA, Combescure C, Tait RC et al. Hypertension, haematuria and renal functioning in haemophilia - a cross-sectional study in Europe. Haemophilia 2016; 22:248–255. [DOI] [PubMed] [Google Scholar]
- [28].Olivieri M, Konigs C, Heller C et al. Prevalence of Obesity in Young Patients with Severe Haemophilia and Its Potential Impact on Factor VIII Consumption in Germany. Hamostaseologie 2019; 39:355–359. [DOI] [PubMed] [Google Scholar]
- [29].Hrdlickova R, Blahutova S, Cermakova Z. Cardiovascular risk assessment in haemophilia patients at University Hospital in Ostrava. Haemophilia 2016; 22:3–138. [Google Scholar]
- [30].von Mackensen S, Harrington C, Tuddenham E et al. The impact of sport on health status, psychological well-being and physical performance of adults with haemophilia. Haemophilia 2016; 22:521–530. [DOI] [PubMed] [Google Scholar]
- [31].Chang CY, Li TY, Cheng SN et al. Obesity and overweight in patients with hemophilia: Prevalence by age, clinical correlates, and impact on joint bleeding. J Chin Med Assoc 2019; 82:289–294. [DOI] [PubMed] [Google Scholar]
- [32].Lambert C, Meite N, Sanogo I et al. Haemophilia in Cote d’Ivoire (the Ivory Coast) in 2017: Extensive data collection as part of the World Federation of Hemophilia’s twinning programme. Haemophilia 2019; 25:236–243. [DOI] [PubMed] [Google Scholar]
- [33].Duarte BP, Costa M, Costa NCM et al. Cardiovascular Clinical and Laboratory Profiles of Hemophilia Patients from the Brazilian Hemophilia Treatment Center of Pernambuco (HEMOPE). Res Pract Thromb Haemost 2019; 3:PB1432. [Google Scholar]
- [34].Retrieved Tue, 07 July 2020 from the Utah Department of Health, Indicator-Based Information System for Public Health Web site: https://ibis.health.utah.gov/ibisph-view/indicator/complete_profile/AgeDistPop.html.
- [35].Adult Obesity Rates. In: State of Childhood Obesity: 2020.
- [36].Adams E, Deutsche J, Okoroh E et al. An inventory of healthy weight practices in federally funded haemophilia treatment centres in the United States. Haemophilia 2014; 20:639–643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Wang M, Peltier S, Baumann K et al. Awareness, Care and Treatment In Obesity maNagement to inform Haemophilia Obesity Patient Empowerment (ACTION-TO-HOPE): Results of a survey of US haemophilia treatment centre professionals. Haemophilia 2020; 26 Suppl 1:20–30. [DOI] [PubMed] [Google Scholar]
- [38].McNamara M, Antun A, Kempton CL. The role of disease severity in influencing body mass index in people with haemophilia: a single-institutional cross-sectional study. Haemophilia 2014; 20:190–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Hofstede FG, Fijnvandraat K, Plug I et al. Obesity: a new disaster for haemophilic patients? A nationwide survey. Haemophilia 2008; 14:1035–1038. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure 3A. Forest plot of the pooled prevalence of overweight/obesity from epidemiological studies in the past 8 years, 2012 – 2019
Supplemental Figure 3B. Forest plot of the pooled prevalence of obesity from epidemiological studies in the past 8 years, 2012 – 2019


