Transcatheter aortic valve replacement (TAVR) has become the preferred treatment for elderly patients with symptomatic severe aortic stenosis (AS) [1]. Left untreated, symptomatic AS is lethal with high 1-year mortality rates [2]. The Coronavirus disease-2019 (COVID-19) pandemic urged for reallocations of resources. Dedicated COVID-19 wards and intensive care units (ICU) prioritized COVID-19 care and elective healthcare was postponed. Furthermore, cardiology societies issued statements favoring telehealth and less-invasive catheter based treatment strategies over conventional cardiac surgery to limit ICU occupation and catalyze early discharge [3]. COVID-19 regulations delayed the diagnosis of severe AS because of higher thresholds to perform echocardiography in the outpatient clinic, postponed referrals for aortic valve replacement (AVR) and, conversely, triggered longer AVR waiting lists. In our center TAVR has transformed into a procedure under local anesthesia without default ICU monitoring, promoting early ambulation and shorter hospital stay. In this single center, observational cohort study, we evaluated changes in the clinical presentation of patients referred for transcatheter aortic valve treatment including TAVR and balloon aortic valvuloplasty (BAV) in the year before vs. during the COVID-19 outbreak in the Netherlands that started February 27th 2020.
All patients who underwent TAVR or BAV between February 2019 and February 2021 were included in this study. Patients were divided into a pre-COVID-19 cohort and a COVID-19 era group relative to the day of the outbreak. Main study parameters were current admission for acute heart failure (HF) with decompensated AS, baseline New York Heart Association (NYHA) functional class, left ventricular ejection fraction (LVEF) and invasively measured left ventricular end diastolic pressure (LVEDP). Additionally, we recorded time spent in the ICU and 30-day all-cause mortality. All patients provided written informed consent for the intervention and subsequent data analysis for research purposes. Group differences were analyzed using a student's t-test, Mann Whitney U test, Chi-Square or Fishers where appropriate. A two-sided p < 0.05 was considered statistically significant. Statistical analyses were performed with SPSS 25.0 (IBM, Armonk, NY).
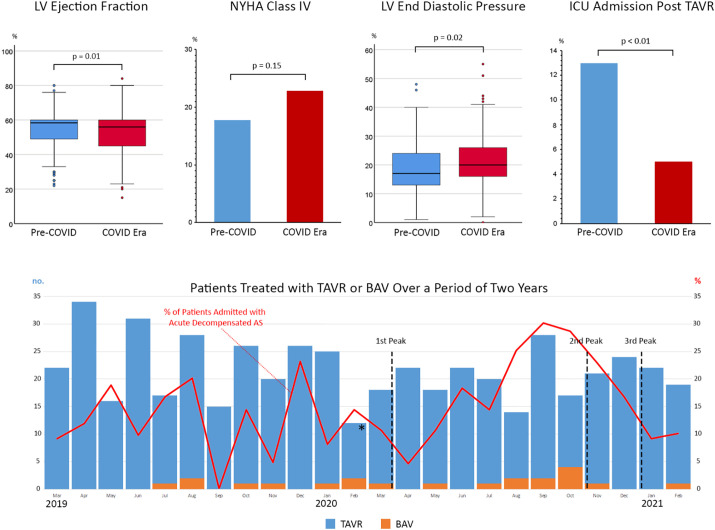
A total of 538 patients underwent either TAVR or BAV and were included in this analysis. Pre-COVID-19 and COVID-19 era cohorts comprised 277 and 261 patients, respectively. Both cohorts appeared to be matched in terms of age and STS-score (with medians of 80 years [IQR74–85] vs. 79 years [IQR74–83] (p = 0.10) and 2.6% [IQR1.7–3.9] vs. 2.4% [IQR1.7–3.4] (p = 0.12) respectively). The relative proportion of men was higher during the COVID-19 era (51% and 61% in pre- and during COVID-19 periods, p = 0.02), 5% had a history of proven COVID-19 infection. Compared to patients presenting in the pre-COVID era, median LVEF was lower (56% [IQR45–60] vs. 59% [IQR49–60], p = 0.01) and slightly more patients presented with acute HF due to decompensated AS (16.9% vs. 13.0%, p = 0.21) in the COVID-19 era. NYHA class IV was observed in 18.0% and 23.1% in pre- and during COVID-19 groups respectively (p = 0.15) (Fig. 1 ). Median mean transaortic gradient determined by transthoracic echocardiography was 38 mmHg [IQR31–47] in the pre-COVID-19 and 38 mmHg [IQR29–47] in the COVID-19 era (p = 0.70). Invasively measured LVEDP assessed directly prior to TAVR was significantly higher in the COVID-19 cohort vs. pre-COVID cohort, 21 mmHg [IQR16–26] versus 17 mmHg [IQR13–24] respectively (p < 0.01).
Fig. 1.
(Top row) Clinical parameters comparing pre-COVID and COVID era cohorts. (Bottom row) Bar chart representing the number of patients treated with TAVR/BAV over a two-year period. Asterisk and dotted lines mark the start of the outbreak and subsequent outbreak peaks respectively. The red line represents the fraction of patients admitted with acute decompensated aortic stenosis relative to the total TAVR/BAV patients. TAVR: Transcatheter Aortic Valve Replacement. BAV: Balloon Aortic Valvuloplasty.
BAV was similar throughout the study window (5.0% vs. 3.2%, p = 0.31). Post-procedural admission to the ICU was more common before vs. during the COVID era (13% vs. 5% respectively, p < 0.01). The median length of in-hospital stay (7 [IQR4–11] days vs. 6 [IQR4–11] days, p = 0.77) and thirty-day all-cause mortality was similar for both cohorts (2.2% vs. 3.1%, p = 0.51, for pre- and during COVID-19 cohorts).
In conclusion, we found that the COVID-19 pandemic negatively impacted patient profiles at the time of treatment for AS. Patients presented with lower LVEF, increased LVEDP and were thus referred at a more advanced stage in the disease process. This might be explained by a clear societal promotion of telehealth with a subsequent decay in outpatient clinic activities and fewer transthoracic echocardiography studies to make a timely diagnosis of severe AS. Reduced ICU resources, unchanged hospital stay and preserved short term outcome results might attest to the streamlined simplified TAVR program that was already established before the COVID-19 outbreak and made our program able to cope with these unprecedented challenges.
Declaration of Competing Interest
Joost Daemen received institutional grant/research support from Astra Zeneca, Abbott Vascular, Boston Scientific, ACIST Medical, Medtronic, Pie Medical, and ReCor medical. Nicolas Van Mieghem received research grant support from Abbott Vascular, Boston Scientific, Medtronic, Edwards Lifesciences, Daiichi Sankyo, PulseCath BV. The other authors have no conflict of interest to declare.
References
- 1.Otto C.M., Nishimura R.A., Bonow R.O., Carabello B.A., Erwin J.P., 3rd, Gentile F., et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021;143:e72–e227. doi: 10.1161/CIR.0000000000000923. [DOI] [PubMed] [Google Scholar]
- 2.Leon M.B., Smith C.R., Mack M., Miller D.C., Moses J.W., Svensson L.G., et al. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med. 2010;363:1597–1607. doi: 10.1056/NEJMoa1008232. [DOI] [PubMed] [Google Scholar]
- 3.Shah P.B., Welt F.G.P., Mahmud E., Phillips A., Kleiman N.S., Young M.N., et al. Triage considerations for patients referred for structural heart disease intervention during the COVID-19 pandemic: an ACC/SCAI position statement. JACC Cardiovasc Interv. 2020;13:1484–1488. doi: 10.1016/j.jcin.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]