Abstract
Background:
We aimed to describe the gender-based disparities in burn injury patterns, care received, and mortality across national income levels.
Methods:
In the WHO Global Burn Registry (GBR), we compared patient demographics, injury characteristics, care and outcomes by sex using Chi-square statistics. Logistic regression was used to identify the associations of patient sex with surgical treatment and in-hospital mortality.
Results:
Among 6,431 burn patients (38% female; 62% male), females less frequently received surgical treatment during index hospitalization (49% vs 56%, p<0.001), and more frequently died in-hospital (26% vs 16%, p<0.001) than males. Odds of in in-hospital death was 2.16 (95% CI: 1.73-2.71) times higher among females compared to males in middle-income countries.
Conclusions:
Across national income levels, there appears to be important gender-based disparities among burn injury epidemiology, treatment received and outcomes that require redress. Multinational registries can be utilized to track and to evaluate initiatives to reduce gender disparities at national, regional and global levels.
Keywords: Burns, World Health Organization, Global Burn Registry, Gender, Sex, Disparities
Introduction
Burn injuries are a leading cause of death and disability globally, with approximately 95% of the health burden occurring in low- and middle-income countries (LMICs).1 Burn injuries are estimated to cause more than 120,000 deaths annually, which represents and provides insight into the large number of underlying preventable burn injuries and near-miss incidentsp.2 Non-fatal burn injuries are more prevalent and can lead to lifelong disability and changes to body image, particularly with inadequate burn care.3 Burn injuries are also associated with challenges in community integration, loss of economic productivity, and social isolation for survivors and their families.4 These less frequently addressed comorbidities are particularly challenging for individuals who are already marginalized or disenfranchised at household, community and societal levels.
Burn injuries occur more frequently among vulnerable populations regardless of national income level, such as impoverished, psychiatrically ill and/or female populations. Women and girls are more often exposed to burn injury hazards in many LMICs.5 Many of these exposures occur in and around the household and are related to energy poverty and activities such as cooking and warming. High-risk cooking arrangements (e.g., ground-level cookstoves, open 3-stone fires), use of unsafe and poorly regulated liquified petroleum gas (LPG) cookstoves, and wearing traditional, loose, and often flammable clothing are commonplace in many LMIC settings.1 For example, a cluster-randomized survey of injuries in Ghana reported that the majority of households used a ground-level open fire with biomass fuels for cooking (e.g., wood, plant material, dung).6 In addition to unintentional injuries, fire, vitriol and chemicals are intentionally used to injure or maim women and girls as a form of gender-based violence.7,8 Epidemiological surveys from South Asia report that patients hospitalized with intentional burns were more often female, and that those injuries tended to be much larger and more strongly associated with death compared to unintentionally burn-injured patients.9
In addition to greater exposure to burn injury hazards, women and girls face disparities in multiple aspects of healthcare access and service delivery globally.10 These disparities are strongly tied to health literacy, financial capacity and independence, access to safe transportation, and lack of healthcare decision making within family structures.11 A report that examined barriers to surgical care among women in West Africa identified factors like inability to navigate the healthcare system, lack of social support and lack of privacy at health facilities were commonly cited barriers to seeking and receiving surgical care.12 In Pakistan, studies have reported that women have less access to surgical care, face social stigma in accessing care for certain conditions, and in some communities, must be accompanied by male relatives when outside the home—decreasing the likelihood of accessing care.13 Additionally, implicit gender bias among care providers further affects the care prescribed, health guidance, and risk of death and disability that women and girls experience.14 As example, a retrospective cohort study from Canada found that severely injured females were less likely than males to be transported or transferred to a designated trauma center despite similar geographic distribution of injury and injury severity.15 The underpinnings of gender-based disparities are multifactorial – highlighting the importance of documenting and attempting to understand the various facets in which sex and gender may impact care in an effort to identify opportunities to improve the experiences and outcome of women, girls, and gender minorities.
The World Health Organization (WHO) established the Global Burn Registry (GBR), a minimum dataset and central repository for hospitals and burn centers globally, to define burn injury epidemiology and support prevention and quality improvement initiatives. Although the GBR is in the early stages of use and promulgation, it provides a unique opportunity to investigate injuries with a global perspective. No study has examined gender disparities around burn injuries, care received, or death with a global perspective. Utilizing the GBR, we aimed to describe gender-based differences in burn injury epidemiology as well as burn surgery received and death across national income levels. By doing so, the findings might improve the understanding of the role of gender in burn injuries and inform future strategies and policies that aim to minimize gender-based disparities in burn injury and outcomes.
Methods
Global Burn Registry
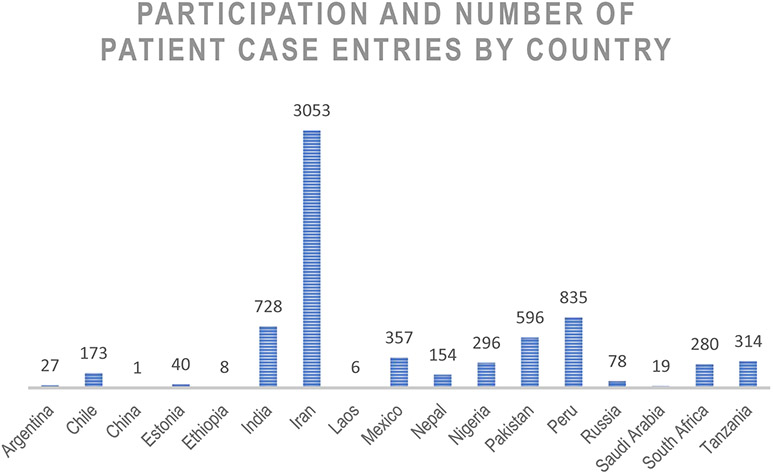
The GBR is a validated minimum dataset and repository that aims to provide an improved, standardized and global data collection system for burn injuries.16 GBR was officially launched in 2017, although data collection began in select centers in 2016. Twenty-nine centers from seventeen countries have contributed data.10 Collected data include patient demographics, injury mechanism, reported contributing factors, treatment facility, and basic patient treatment and outcome data. Patient data are entered into the GBR by participating centers using a standardized data collection tool. The registry is continuously updated, and the uploaded data are stored on network servers located at WHO headquarters in Geneva, Switzerland. Public and private versions of the registry data are maintained, with modifications made to the public data to eliminate potential patient identifiers. The private database is only available for approved personnel from contributing health facilities, and thus the publicly available version was utilized 17 For this study, the WHO GBR database was accessed on July 07, 2020 via http://www.who.int/violence_injury_prevention/burns/gbr/en/. Countries who have contributed to the Global Burn registry between 2016-2020 as well as their level of participation is noted in Figure 1.
Figure 1: Contributing countries and their respective participation in the Global Burn Registry*.
* Recorded participation from registry launch until data accessed on July 7, 2020.
Data Analysis
A retrospective cohort study was conducted in order to compare care and outcomes by sex utilizing the WHO GBR patient data from its inception in 2016 through July 2020. All burn-injured patients recorded in the registry with available sex and outcome data were included in this study. There were no other exclusion criteria. Patient sex, reported as male or female, was the exposure of interest; gender was not recorded. Facility capacity scores were calculated using pre-defined capacity “tiers of care” ranging from Tier 0 to Tier 3 using data regarding the availability of critical care, surgical care and allied services (e.g., nutrition, physiotherapy) (Table 1). Patient national income level is reported in the GBR based on the World Bank designations of country income level and was categorized as low-, middle-, or high-income. Descriptive statistics were used to describe patient demographics, injury mechanism, burn injury characteristics, care received, and outcomes (i.e., in-hospital mortality, condition on discharge). Differences in non-parametric medians and proportions were compared with Wilcoxon rank-sum and Chi-square or Fisher’s exact tests, respectively. 13 of these tests were performed.
Table 1:
Facility capacity scores defined
| Critical care | Surgery center, wound care, burn unit, blood transfusion |
Physiotherapy, nutrition, ancillary services |
|
|---|---|---|---|
| Tier 0 | None/Limited | None | None |
| Tier 1 | Full Capacity | Limited capacity | None |
| Tier 2 | Full Capacity | Full Capacity | Limited Capacity |
| Tier 3 | Full Capacity | Full Capacity | Full Capacity |
Capacity is defined as having all, some of none of the listed services, correlating with full, limited and no (none) capacity.
Logistic regression was performed to assess the associations between patient sex and surgical treatment during index hospitalization as well as patient sex and in-hospital mortality; the models were adjusted by patient age, % total body surface area (TBSA) of burn, pre-hospital delay (i.e., hours from injury to hospital presentation), and hospital length of stay (LOS) in days. Effect modification of these associations by country income was assessed using likelihood ratio tests to determine the significance of the interaction term between sex and the three-tiered national income level (low-, middle-, high-income). If effect modification was found, the regression models evaluating surgical treatment and in-hospital mortality by sex were stratified by national income and interpreted individually. Statistical analysis was completed in STATA v15.1 (StataCorp, USA).
Of note, the results are reported by sex (female/male) as the GBR collects data by patient sex, however the introduction and discussion sections primarily utilize gender-based terminology as these disparities impact all who identify as women/girls.
Results
Patient Characteristics
GBR contained data from 6,965 total patients admitted with burn injuries in 2016-2020 from 17 countries. Patients with recorded sex and outcome data were included in this study (n=6,341) (Table 2). The median age of female patients was 23 years (IQR: 4-42 years) and of male patients was 24 years (IQR: 5-38 years). The age group distribution between female and male patients was similar: the majority of patients were 19-49 years old, followed by children less than 5 years of age. The majority of patients from both sexes were from middle-income countries (87% of female and 89% of male patients). Additionally, the distribution of reported contributing factors was similar, with the exception of a higher proportion of male patients with reported psychiatric illness as a contributing factor. Lastly, there was a similar distribution by sex of the treatment facility capacity: care was received most frequently at either tier 0 or tier 3 facilities by both male and female patients.
Table 2:
Global Burn Registry patient demographics by sex
| Female |
Male |
|||
|---|---|---|---|---|
| n= 2405 | (%) | n= 3936 | (%) | |
| Age group (years) | ||||
| <5 | 698 | 29 | 981 | 25 |
| 5-14 | 319 | 13 | 504 | 13 |
| 15-18 | 83 | 4 | 171 | 4 |
| 19-49 | 867 | 36 | 1761 | 48 |
| >50 | 438 | 18 | 519 | 13 |
| National income level * | ||||
| Low Income | 213 | 9 | 231 | 6 |
| Middle Income | 2083 | 87 | 3503 | 89 |
| High income | 109 | 5 | 202 | 5 |
| Contributing factor | ||||
| Alcohol/drugs | 149 | 6 | 348 | 9 |
| Psychiatric illness | 50 | 2 | 44 | 11 |
| Mental/Physical Disorder | 81 | 3 | 109 | 3 |
| Other disabilities | 138 | 6 | 234 | 6 |
| None | 1987 | 83 | 3401 | 86 |
| Facility Capacity ** | ||||
| Tier 0 | 892 | 37 | 1709 | 43 |
| Tier 1 | 354 | 15 | 487 | 12 |
| Tier 2 | 252 | 10 | 297 | 8 |
| Tier 3 | 907 | 38 | 1461 | 37 |
Income level determined by World Bank designation
Capacity Scoring defined in Table 2
Injury Characteristics
Females and males sustained flame burns at similar proportions (47% vs 48%, respectively) (Table 3). Females sustained scald burns more often than males (43% vs 32%; p<0.001). While the median burn size was the same between males and females, females burn size was positively skewed indicating that among those with above average burn size, females were more likely to have large burns compared to males (females 15% TBSA, IQR 10-35% vs males 15% TBSA, IQR 5-30%; Wilcoxon Rank Sum test p<0.001). Females were significantly more likely to have an associated inhalation injury (16% vs 12%; p<0.001) and had a higher median revised Baux (rBaux) score (median=46, IQR 20-77 vs 43, IQR 21-65, p<0.001). A larger proportion of female patients sustained burn injuries of the upper extremities (64% vs 60%; p=0.002), trunk (68% vs 59%; p<0.001) and feet and lower extremities than male patients (66% vs 61%; p<0.001).
Table 3:
Burn injury etiology, characteristics, and outcomes for female vs male patients
| Female | Male | ||||
|---|---|---|---|---|---|
| n | (%) | n | (%) | p value | |
| Burn etiology | |||||
| Flame | 1136 | 47 | 1871 | 48 | |
| Scald | 1038 | 43 | 1267 | 32 | <0.001* |
| Other (contact, steam, electrical, chemical, etc.) | 231 | 10 | 798 | 20 | |
| Burn injury | |||||
| TBSA percent, (median, IQR) | 15 | 10-35 | 15 | 5-30 | <0.001^ |
| Baux score (median, IQR) | 46 | (20 - 77) | 43 | (21 - 65) | <0.001^ |
| Inhalation injury | 384 | 16 | 455 | 12 | <0.001* |
| Burn location | |||||
| Face and neck | 1124 | 47 | 1958 | 50 | 0.020* |
| Upper extremities (except hands) | 1526 | 64 | 2346 | 60 | 0.002* |
| Hand | 1160 | 54 | 2160 | 55 | <0.001* |
| Trunk | 1633 | 68 | 2327 | 59 | <0.001* |
| Lower extremities | 1594 | 66 | 2411 | 61 | <0.001* |
| Care utilization | |||||
| Hours from injury to presentation (median, IQR) | 20 | (5 - 96) | 17 | (5 - 73) | 0.893^ |
| Length of stay in days (median, IQR) | 9.5 | (4.7 - 17.5) | 10.4 | (5.3 - 18.0) | 0.162^ |
| Surgery performed during index hospitalization | 1183 | 49 | 2201 | 56 | <0.001* |
| Discharge condition | |||||
| Death | 635 | 26 | 630 | 16 | <0.001* |
| Discharged home with disability | 186 | 8 | 400 | 10 | |
| Discharged home with no disability | 1584 | 66 | 2906 | 74 | |
Chi-Square test
Wilcoxon Rank Sum test
Care Utilization and Outcomes
On average, female patients had a slightly longer pre-hospital delay than males; however, there was no statistically significant difference (median=20 hours, IQR 5-96 vs 17 hours, IQR 5-73; p=0.89). Female patients had a shorter median hospital LOS compared to male patients (median=9.5 days, IQR 4.7-17.5 vs 10.4 days, IQR 5.3-18.0; p=0.16). However, female patients underwent surgical treatment during the index hospitalization less frequently than male patients (49% vs 56%; Chi-Square test with p<0.001). Additionally, female burn-injured patients died more frequently in-hospital than male patients did and were more often discharged home with a disability than male patients (death: 26% vs 16%, respectively; discharged with disability: 74% vs 66%, respectively; Chi-Square test with p<0.001).
Differences by Sex Across National Income Levels
Statistically significant effect modification by national income level was found in the association between sex and surgical treatment as well as sex and in-hospital mortality, adjusted for patient age, % TBSA, prehospital in hours, and hospital LOS in days. Since this indicated that the relationship between sex and the outcome of interest differed by levels of national income, the models were stratified and interpreted individually for each national income context. The analyses of association between sex and surgical treatment when stratified by national income level demonstrated that in middle-income countries, female patients were significantly less likely than males to undergo surgical treatment during the index hospitalization than males (aOR=0.83, 95% CI: 0.74-0.93, p=0.001) (Table 4). In low-income countries females were less likely to undergo surgical treatment (aOR=0.77, 95% CI: 0.48-1.24, p=0.284), although this difference was not statistically significant. There was no evidence for a sex difference in surgical treatment in high-income countries (aOR=1.37, 95% CI: 0.74-2.54, p=0.313). In the analyses of association between sex and in-hospital mortality for burn-injured patients, females in both low-income countries and middle-income countries had higher odds of in-hospital death (low-income: aOR=2.08, 95% CI: (1.01-4.29), p=0.048; middle-income: aOR 2.16, 95% CI: 1.73-2.71, p<0.001) (Table 5). There was no evidence found to support differences in in-hospital mortality by sex in high-income countries (aOR 0.66, 95% CI: 0.20-2.19, p=0.493).
Table 4:
Logistic regression models of association between sex and receiving surgical treatment at index hospitalization by national income level
| Crude Odds Ratio OR (95% CI) |
Adjusted Odds Ratio* aOR (95% CI) |
p-value | |
|---|---|---|---|
| Low income country | |||
| Female | 1.09 | 0.77 (0.48-1.24) | p=0.284 |
| Male | referent | referent | - |
| Middle income country | |||
| Female | 0.74 | 0.83 (0.74-0.93) | p=0.001 |
| Male | referent | referent | - |
| High income country | |||
| Female | 1.25 | 1.37 (0.74-2.54) | p=0.313 |
| Male | referent | referent | - |
Adjusted by age, %TBSA, pre-hospital delay and hospital length of stay (LOS) in days
Table 5:
Logistic regression models of association between sex and in-hospital death by national income level
| Crude Odds Ratio OR (95% CI) |
Adjusted Odds Ratio* aOR (95% CI) |
p-value | |
|---|---|---|---|
| Low income country | |||
| Female | 1.92 | 2.08 (1.01-4.29) | p=0.048 |
| Male | referent | referent | - |
| Middle income country | |||
| Female | 1.95 | 2.16 (1.73-2.71) | P<0.001 |
| Male | referent | referent | - |
| High income country | |||
| Female | 0.49 | 0.66 (0.20-2.19) | p=0.493 |
| Male | referent | referent | - |
Adjusted by age, %TBSA, pre-hospital delay and hospital LOS in day
Discussion
This study aimed to describe differences in burn injury characteristics by gender globally, as well as differences in surgical treatment and discharge outcomes across national income levels utilizing the GBR database. Our analyses revealed several key findings that warrant more directed attention. First, our analyses of patient observations in the WHO GBR, revealed women sustained more severe burn injuries, The injuries were slightly larger more frequently associated with concomitant inhalation injury, and included a high proportion of injury distribution to highly functional anatomic areas such as the arms and legs. Secondly, women who sought burn care, especially those in middle-income countries—where the majority of the GBR data is reported from—appeared to have lower odds of undergoing surgical treatment for burn injuries compared to men. We also found that women have higher odds of in-hospital death after burn injury in low- and middle-income countries. However, these same associations were not found in a high-income country context. Our findings highlight areas for further inquiry into gender-based differences in burn injury and care. More broadly, these early analyses and findings demonstrate the potential of the GBR to serve as both an epidemiological and advocacy tool for burn care prevention, care and advocacy practitioners around the world.
Our analyses indicated that of the patient observations in the WHO GBR, women and girls tend to have more severe injuries with a slightly larger burn size and more frequent inhalation injury. While the differences in injury severity were small, and in the case of the revised Baux score differences, have unclear clinical significance, they cumulatively signal to underlying disparities. Additionally, while our analysis revealed both women and men often sustained injuries to highly functional anatomic areas such as the arms and legs, these injuries occurred more frequently in women. These injury patterns have major implications beyond survival on long-term disability and functional recovery, as they may require treatments and resources with limited availability in LMICs. Many LMICs have limited availability of critical care capacity such as ICU beds or ventilators to manage acute burn shock or inhalation injury, or may have limited providers with critical care training.18,19 Further, surgical treatment for burn injuries to highly functional areas such as the hands, feet or face often require specialist care from sub-specialist reconstructive surgeons, who are often not widely available/accessible.20 Patients unable to undergo surgical treatment of deep burns in areas of high functional importance with procedures like excision and grafting frequently develop wound contractures. Contractures (including those resulting from a seemingly “small” 1% TBSA injury of the hand) can be debilitating and cause near total loss of function of affected limbs in severe cases.21 Further, for those patients who do receive surgical treatment in the acute injury period, intensive physiotherapy therapy in both the inpatient and outpatient setting are still required to regain, maintain, and maximize function. Without robust and comprehensive care across the entire injury lifecycle from pre-hospital treatment and acute care to long-term rehabilitation, it is often the most vulnerable populations including impoverished individuals or women and girls who are at risk of developing the long-term complications that contribute to loss of economic productivity and challenges with community integration.
Further, we found that women and girls may have lower odds of receiving surgical treatment following burn injury during the index hospitalization in middle-income settings. There is limited literature specifically delineating burn care provision in resource-limited contexts by gender, and to our knowledge, this disparity has not been previously reported. However, there is emergency surgical literature from sub-Saharan Africa which reports similar findings. In a single institution study at Kamuzu Central Hospital in Malawi, women presenting with a diagnosis of acute peritonitis presented later, experienced longer delays to operative intervention, and underwent significantly fewer operative interventions for peritonitis than compared to men.22 A multi-center study in Ghana which characterized the rate of obstetric and gynecologic procedures, found an annual national cesarian section operation rate suggestive of inadequate access to essential obstetric care and overall inadequate surgical capacity.23 These studies in sub-Saharan Africa bring attention to gender-based differences for the basic “Bellwether” procedures24 in LMIC. The differences are likely more pronounced for burn procedures, given that burn care is a sub-specialized field with far fewer points of access to care within health systems than emergency general and obstetric/gynecologic surgical care. Further, these findings contrast with studies of burn care delivery by sex from high-income countries. For example, a recent study in the United States (U.S.) found no difference in time to first surgery on the basis of sex in burn-injured patients.25 This highlights the potential role of national income level and respective health system infrastructure/capacity in the gender-based differences in burn care provision. However, the specific factors that may drive these differences in low- and middle-income countries are not well described, and further research is critical to delineate them, particularly in light of the functional and social impact such care disparity may have on burn-injured women and girls globally.
Additionally, in the GBR, burn-injured women had significantly increased odds of in-hospital mortality compared to men in LMICs. Higher rates of female mortality in trauma and burn-injured patients have been reported in multiple instances. In two separate U.S.-based studies from National Burn Repository (NBR) data, female patients were found to have an estimated 30% higher mortality following admission for burn injury than males patients.26,27 Literature from other high-income countries report more varied associations: while burn centers in New Zealand and Australia demonstrate a higher risk of death in female patients28, in Austria and Sweden, patient sex was not demonstrably associated with increased burn patient mortality.29,30 The variability in the literature by country suggests that there may be underlying factors contributing to gender-based differences in mortality that are hospital, region, or health system specific. However, the specific factors contributing to the association of female sex with mortality in burn injuries are not well delineated. Given the limited data related to sex- and gender-based differences in burn injury outcomes in LMIC, there are only hypotheses of the underlying reasons for the differences. To further explore this concept, we recommend a combination of community-based, and region- and national-specific evaluations. This will help elucidate differences in exposures to hazards, access to the healthcare system, or unconscious provider gender bias not only to determine the presence of gender-based differences in burn care and outcomes, but to describe the underlying reasons for those differences.
This study demonstrated that the development and use of the GBR is an important step in understanding the global burden of burn injuries and as a tool to uncover specific epidemiologic trends and bring attention to disparities experienced by vulnerable populations. This is particularly important and useful within many LMICs where there are few central databases. There are several national-level centralized data repositories for burn patient epidemiology and outcomes in high-income countries. For example, the NBR of the American Burn Association (ABA) sees contribution from 100+ burn centers in the U.S, Canada, Switzerland and Sweden, and is a source of extensive epidemiological research and data-driven initiatives each year. The ABA has also instituted that contribution to the NBR is required for verification as a burn center, which may explain the high level of participation by burn centers.31 Similar nation-level registries exist in Australia/New Zealand and England.32 As demonstrated in our findings and discussion, the literature on gender-based burn care delivery and outcomes data is largely limited to high-income countries despite the majority of burn injury occurring in LMICs. We hypothesize this is partially due to more robust data collection platforms and databases available in high resource settings such as national burn registries. In order to recognize and address aspects of burn care equity in LMIC such as differences in outcomes by gender, it is imperative to develop and promulgate robust yet feasible data collection platforms such as the GBR. By using a platform like the GBR, centers and countries can conduct internal audits, iteratively track progress over cycles of quality improvement or program development, and gauge their epidemiology and outcomes in comparison to other countries or regions. Participation in the GBR from more centers will further increase the validity and diversity of data and may ultimately serve to inform and improve aspects of burn prevention and burn care delivery globally.
There are some limitations to this study to discuss prior to drawing conclusions from our analyses. First, this analysis only includes patients who were admitted to a center that reported to the WHO GBR. Often, these centers have specialized plastic surgery or burn units, and may be more urban, larger and/or better resourced—meaning that patients cared for at community health posts or first-level hospitals are less likely to be included. Given this is a hospital-based minimum dataset, there is limited information regarding high-risk behaviors, “near miss” incidents, community-based care, the patient journey to accessing burn care including barriers. There is also limited adjunct patient information on co-morbidities and exact distribution and depth of burn injury in the GBR, which may impact the need for surgery and outcomes like length of stay and death. Additionally, given that hospitals from only 17 countries have participated thus far in the GBR, and in unequal proportions, we recognize the data are vulnerable to selection bias. The majority of patients in the registry are from middle-income countries; furthermore, Iran is a particularly large contributor of data to the registry, accounting for nearly half of the patient entries. Although the data is skewed and most represents those populations, we aimed to minimize some of this bias by accounting for effect modification and carrying out the analyses by national income level. It is also possible that the significant effect modification found across levels of national income may be due to the vast difference in the proportion of injuries reported from each context. Future research should reassess these findings if and when more countries begin reporting their data to the GBR. Lastly, this is an exploratory analysis to assess potential differences in burn care and outcomes by sex and thus no adjustment for multiple comparisons has been made. However, the results should be considered hypothesis generating and provide the basis upon which future research may build. Despite these limitations, the data and analysis may provide early insight and a current baseline from the GBR regarding gender-based disparities in burn care globally.
Conclusions
This study highlights gender-based differences in burn epidemiology, care delivery, and outcomes from the WHO GBR. Despite being in the early stages of use, the database and these analyses lead to important recommendations to further our understanding of the role of gender in burn injury epidemiology, to understand the gender-based disparities in burn care delivery and outcomes, and to develop strategies to improve our understanding in this important area.
Our recommendations include:
Specifically develop research focus on disparities in burn care at local and regional levels in LMIC;
Deepen the understanding of why these gender-based inequities exist utilizing methods such as qualitative patient interviews to capture data that missed by minimum datasets and registries;
Promulgation of WHO GBR to understand local, national and global burn epidemiology in order to understand and promote gender equity in burn care systems.
Highlights.
Females may sustain more severe burn injuries than males globally
Disparities may exist in burn injury surgical care and outcomes by sex
Gender disparities are more apparent in low- and middle-income country scenarios
WHO Global Burn Registry can demonstrate epidemiological patterns and disparities
Identified patterns and disparities can inform quality improvement initiatives
Acknowledgements
The authors would like to thank the Harborview Injury Prevention and Research Center’s INSIGHT Training Program for their contributions to the study.
Funding
This work was supported by the R25-TW009345 from the Fogarty International Center, US National Institutes of Health and 5R25HD094336-02 through the Pediatric Injury Prevention Student Internship (INSIGHT) Training Program, US National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the World Health Organization.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to report.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Kajal Mehta, Department of Surgery, University of Washington, Seattle, WA, USA.
Hana Arega, School of Public Health, University of Washington, Seattle, WA, USA.
Natalie L. Smith, School of Medicine, University of Washington, Seattle, WA, USA.
Kathleen Li, Krieger School of Arts & Sciences, The Johns Hopkins University, Baltimore, MD, USA.
Emma Gause, Harborview Injury Prevention & Research Center, Seattle, WA, USA.
Joohee Lee, Public Health Concern Trust-Nepal, Kathmandu, Nepal.
Barclay Stewart, Harborview Injury Prevention & Research Center, Seattle, WA, USA; Department of Surgery, University of Washington, Seattle, WA, USA.
References
- 1.Mock C, Peck M & Peden M A WHO plan for burn prevention and care. https://apps.who.int/iris/handle/10665/97852 (2008). [Google Scholar]
- 2.James SL et al. Epidemiology of injuries from fire, heat and hot substances: global, regional and national morbidity and mortality estimates from the Global Burden of Disease 2017 study. Inj. Prev 26, i36–i45 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Peck MD, Kruger GE, van der Merwe AE, Godakumbura W & Ahuja RB Burns and fires from non-electric domestic appliances in low and middle income countries: Part I. The scope of the problem. Burns 34, 303–311 (2008). [DOI] [PubMed] [Google Scholar]
- 4.Van Loey NEE & Van Son MJM Psychopathology and Psychological Problems in Patients with Burn Scars. Am. J. Clin. Dermatol 4, 245–272 (2003). [DOI] [PubMed] [Google Scholar]
- 5.Peck MD Epidemiology of burns throughout the world. Part I: Distribution and risk factors. Burns 37, 1087–1100 (2011). [DOI] [PubMed] [Google Scholar]
- 6.Mehta K et al. Incidence of childhood burn injuries and modifiable household risk factors in rural Ghana: A cluster-randomized, population-based, household survey. Burns J. Int. Soc. Burn Inj (2020) doi: 10.1016/j.burns.2020.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Epidemiology of burns throughout the World. Part II: Intentional burns in adults. Burns 38, 630–637 (2012). [DOI] [PubMed] [Google Scholar]
- 8.Stewart BT et al. 278 A Comprehensive Legislative Framework to Address Chemical Assault. J. Burn Care Res 40, S116–S117 (2019). [Google Scholar]
- 9.Lama BB et al. Intentional burns in Nepal: a comparative study. Burns J. Int. Soc. Burn Inj 41, 1306–1314(2015). [DOI] [PubMed] [Google Scholar]
- 10.Sen G & Östlin P Gender inequity in health: why it exists and how we can change it. 1–12 http://www.tandfonline.com/doi/abs/10.1080/17441690801900795 (2008). [DOI] [PubMed] [Google Scholar]
- 11.Dave D, Nagarajan N, Canner J, Kushner AL & Stewart BT Rethinking burns for low & middle-income countries: Differing patterns of burn epidemiology, care seeking behavior, and outcomes across four countries. Burns 44,1228–1234 (2018). [DOI] [PubMed] [Google Scholar]
- 12.Gyedu A et al. Barriers to essential surgical care experienced by women in the two northernmost regions of Ghana: a cross-sectional survey. BMC Womens Health 16, 27 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Irfan FB, Irfan BB & Spiegel DA Barriers to Accessing Surgical Care in Pakistan: Healthcare Barrier Model and Quantitative Systematic Review. J. Surg. Res 176, 84–94 (2012). [DOI] [PubMed] [Google Scholar]
- 14.Marcolini EG, Albrecht JS, Sethuraman KN & Napolitano LM Gender Disparities in Trauma Care: How Sex Determines Treatment, Behavior, and Outcome. Anesthesiol. Clin 37, 107–117 (2019). [DOI] [PubMed] [Google Scholar]
- 15.Gomez D et al. Gender-associated differences in access to trauma center care: A population-based analysis. Surgery 152, 179–185 (2012). [DOI] [PubMed] [Google Scholar]
- 16.WHO ∣ Global Burn Registry. WHO; http://www.who.int/violence_injury_prevention/burns/gbr/en/. [Google Scholar]
- 17.WHO ∣ Participating in and using the Global Burn Registry - Frequently Asked Questions. WHO; http://www.who.int/violence_injury_prevention/burns/gbr/faqs/en/. [Google Scholar]
- 18.Vukoja M et al. A survey on critical care resources and practices in low- and middle-income countries. Glob. Heart 9, 337–342.e1–5 (2014). [DOI] [PubMed] [Google Scholar]
- 19.Murthy S, Leligdowicz A & Adhikari NKJ Intensive care unit capacity in low-income countries: a systematic review. PloS One 10, e0116949 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ringo Y & Chilonga K Burns at KCMC: Epidemiology, presentation, management and treatment outcome. Burns 40, 1024–1029 (2014). [DOI] [PubMed] [Google Scholar]
- 21.Sasor SE & Chung KC Upper Extremity Burns in the Developing World: A Neglected Epidemic. Hand Clin. 35, 457–466 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reid TD et al. Sex Disparities in Access to Surgical Care at a Single Institution in Malawi. World J. Surg 43, 60–66 (2019). [DOI] [PubMed] [Google Scholar]
- 23.Gyedu A et al. Estimating obstetric and gynecologic surgical rate: A benchmark of surgical capacity building in Ghana. Int. J. Gynaecol. Obstet. Off. Organ Int. Fed. Gynaecol. Obstet 148, 205–209 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.O’Neill KM et al. Bellwether Procedures for Monitoring and Planning Essential Surgical Care in Low- and Middle-Income Countries: Caesarean Delivery, Laparotomy, and Treatment of Open Fractures. World J. Surg 40, 2611–2619 (2016). [DOI] [PubMed] [Google Scholar]
- 25.Karimi K et al. Increased mortality in women: sex differences in burn outcomes. Burns Trauma 5, 18 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bedri H et al. A National Study of the Effect of Race, Socioeconomic Status, and Gender on Burn Outcomes. J. Burn Care Res. Off. Publ. Am. Burn Assoc 38, 161–168 (2017). [DOI] [PubMed] [Google Scholar]
- 27.Kerby JD et al. Sex differences in mortality after burn injury: results of analysis of the National Burn Repository of the American Burn Association. J. Burn Care Res. Off. Publ. Am. Burn Assoc 27, 452–456 (2006). [DOI] [PubMed] [Google Scholar]
- 28.Moore EC, Pilcher DV, Bailey MJ, Stephens H & Cleland H The Burns Evaluation and Mortality Study (BEAMS): predicting deaths in Australian and New Zealand burn patients admitted to intensive care with burns. J. Trauma Acute Care Surg 75, 298–303 (2013). [DOI] [PubMed] [Google Scholar]
- 29.Ederer IA et al. Gender has no influence on mortality after burn injuries: A 20-year single center study with 839 patients. Burns J. Int. Soc. Burn Inj 45, 205–212 (2019). [DOI] [PubMed] [Google Scholar]
- 30.Pompermaier L et al. Are there any differences in the provided burn care between men and women? A retrospective study. Burns Trauma 6, 22 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.ABA Registry and Quality Programs. American Burn Association https://ameriburn.org/aba-registry-and-quality-programs/.
- 32.Ajami S & Lamoochi P Comparative study on National Burn Registry in America, England, Australia and Iran. J. Educ. Health Promot 3, 106 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]