Abstract
Symptoms of attention-deficit/hyperactivity disorder (ADHD) in childhood have been found to be predictive of compromised cognitive function, and possibly even dementia, in later adulthood. This study aimed to test vascular risk as a hypothesized moderator or mediator of this association, because individuals with elevated ADHD symptoms frequently have comorbid vascular disease or risk factors which are recognized to contribute to later-life cognitive decline. Data from 1,092 adults aged 18–85 were drawn from the Enhanced Nathan Kline Institute Rockland Sample. Childhood ADHD symptoms (assessed using the Adult ADHD Clinical Diagnostic Scale) were assessed as predictors of cognitive functioning in adulthood (assessed using subtests from the University of Pennsylvania Computerized Neurocognitive Battery, the Delis-Kaplan Executive Functioning System, and the Wechsler Memory Scale). Vascular risk factors (including diabetes, tobacco use, obesity, hypertension, and hypercholesterolemia) were tested as both a moderator and mediator of this relationship. Childhood ADHD symptoms and vascular risk factors were both independently associated with later-life cognition, but vascular risk was not a significant moderator or mediator of relationships between ADHD symptoms and cognition in statistical models. Results from this large community sample suggest that the relationship between ADHD symptoms and cognition is not accounted for by vascular risk. This question should also be investigated in clinical samples.
Subject terms: ADHD, Human behaviour
Introduction
Persistent symptoms of attention-deficit/hyperactivity disorder (ADHD) affect at least 3% of adults and seniors1,2. Its cognitive features (inattention, distractibility, impulsivity) tend to be associated with disruptions in executive functions (i.e., complex regulatory processes controlled in part by the frontal lobes)3,4. For example, increased ADHD symptoms in older adults, assessed as a continuous variable using the Conners Adult ADHD Rating Scale, have been linked to lower performance on tasks of working memory5 and retrieval6, as well as slowed reaction time6. This aligns with findings of compromised frontal lobe integrity in ADHD7 which, in older adults, may be compounded by the known deleterious effects of aging on frontal brain regions and processes8,9.
ADHD symptoms have recently been linked to accelerated cognitive decline later in life. Adults with a history of clinically-diagnosed ADHD may have higher likelihood of developing dementia than do adults without ADHD10–12. Similarly, individuals with Lewy body dementia retrospectively report more severe ADHD symptoms in childhood than do healthy controls13. The mechanistic processes underlying this proposed relationship are unknown. One possibility is that ADHD symptoms may increase risk for later-life cognitive impairment by promoting the accumulation of brain health-compromising factors and behaviors throughout adulthood14. Vascular risk factors, as well as health behaviors that jeopardize vascular health, have been associated with cognitive performance across numerous studies. Diabetes15–19, tobacco use18,20, obesity21–23, hypertension17,18,24–26, and hypercholesterolemia18,27 have all been linked to lower cognitive performance in older adults. These factors seem to have particular relevance for executive functions, as aggregate scores for vascular risk (e.g., hypertension, diabetes, and smoking) relate negatively to global measures of executive function28,29 as well as specific measures of switching and working memory30.
It is now well-recognized that ADHD symptoms are associated with increased risk of vascular medical comorbidities and engagement in harmful behaviors that may cumulatively compromise cerebrovascular and cognitive health throughout adulthood31. For instance, young people with ADHD are more likely than those without to develop diabetes later in life12,32, and those with high levels of ADHD symptoms are more prone to heavy daily cigarette smoking than those with low symptom levels33. ADHD symptoms have been robustly linked to later-life risk for overweight and obesity12,34, which may contribute to a secondary association between ADHD symptoms and hypertension in adults35. ADHD symptomatology has also been linked to higher blood concentrations of low-density lipoprotein (LDL) cholesterol36, which contributes to atherosclerosis and vascular disease with age37. In non-ADHD psychiatric samples, these comorbidities and health behaviors have been shown to account for a substantial proportion of variance in cognitive performance38.This relationship has not been tested in ADHD, but raises the possibility that impairments in executive functioning and potential accelerated cognitive decline and dementia risk in ADHD may be due in part to the disorder’s association with vascular risk factors. A corollary to this hypothesis is that active vascular risk management may alleviate some of the cognitive difficulties associated with ADHD symptoms.
In light of the known adverse cognitive effects of vascular risk factors in epidemiological studies of adults and seniors, and considering their association with symptoms of ADHD, this study’s objective is to investigate whether previously-reported associations between ADHD symptoms and cognitive impairment10,11,13 may be driven by vascular risk factors (diabetes, smoking, obesity, hypertension, and hypercholesterolemia). We hypothesize that the relationship between ADHD symptoms and cognitive performance will be mediated or moderated by these factors, and we focus on frontal/executive aspects of cognitive performance (processing speed, reaction time, working memory, cognitive flexibility, and inhibitory control) because these are the most associated with ADHD symptomatology in adults and have been robustly linked to physical health, as described above. We also focus on ADHD symptoms in childhood as they are more likely to have preceded, rather than followed, the presence of vascular risk factors.
Materials and methods
Participants
This study used data from the Enhanced Nathan Kline Institute Rockland Sample (NKI-RS)39, a lifespan, cross-sectional community sample of individuals aged 6–85 years. Only data from participants 18 or older were retained for the present study (N = 1,092). The NKI-RS has institutional ethical approval at the Nathan Kline Institute (#226,781 and #239,708) and at Montclair State University (#000983A and #000983B), all participants within this sample provided written informed consent to participate, and all phenotypic protocols developed by the Child Mind Institute’s Scientific Research Council were followed39.
Materials
All data described below were collected within the scope of a larger protocol administered over two days39.
ADHD variables
ADHD symptoms were assessed using the Adult ADHD Clinical Diagnostic Scale (ACDS)40.This clinician-administered interview retrospectively assesses childhood ADHD in adult participants, and the interview then follows with an expanded assessment of recent symptomology (i.e., past 6 months). Although childhood symptoms (averaged across items) were the main focus of the current study, a current symptoms score was also computed (averaged across items) to examine possible associations with outcomes in an exploratory fashion.
Vascular health variables
Consistent with prior studies of vascular risk and cognition eg., 41, the following risk factors were included in the present study. Diabetes was defined as either a self-reported diagnosis of diabetes on a medical history questionnaire, or a fasting glucose level of ≥ 140.0 mg/dL on bloodwork. Tobacco use in the past two years (yes/no) was ascertained using the Fagerstrom Test for Nicotine Dependence42. Obesity was quantified as body mass index (BMI) > 30 kg/m2. Participants with systolic blood pressure > 140.0 mm/Hg were considered hypertensive. Non-high-density lipoprotein (non-HDL) was isolated from total cholesterol volumes to define hypercholesterolemia, as recommended in prior literature43, by subtracting HDL from total cholesterol. Values > 158 mg/dL were considered to reflect hypercholesterolemia.
Cognitive variables
Cognitive performance was assessed using subtests of the University of Pennsylvania Computerized Neurocognitive Battery (CNB)44, the Delis-Kaplan Executive Functioning System (D-KEFS)45, and the Wechsler Memory Scale-Revised (WMS-R)46. Domains assessed included switching (i.e., shifting flexibly between tasks)47, working memory (i.e., temporary storage and manipulation of information in a complex task)48, reaction time (i.e., decision-making latencies to respond to visual stimuli)49, and processing speed (i.e., response latencies to simple cognitive tasks requiring little to no complex processing)50. A detailed description of the variables, along with any transformations applied to the data, appears as Supplementary Information.
Statistical analyses
Analyses were performed in Mplus 8.1. Since some variables were treated as categorical, we used the Weighted Least Square—Means and Variance adjusted (WLSMV) estimator. The WLSMV estimator includes participants with missing data and provides consistent estimates when the data is missing-at-random conditional on covariates51. Missing data in the predictors was dealt with by imputing 20 datasets52. In structural equation modeling, model fit can be assessed using various indexes53,54. The χ2 is a measure of exact fit and should ideally be small and non-significant. It is often significant and other fit indices are often used. The Comparative Fit Index (CFI) and the Tucker-Lewis Index (TLI) are measures of relative fit. Values above 0.90 and 0.95 indicate good excellent fit, respectively. The Root Mean Square Error of Approximation should be small, with values below 0.08 and 0.05 indicating good and excellent fit, respectively.
Consistent with recent models of executive function3,55 we used a bifactor model to capture three components of executive function (EF). This model is a bifactor S-1 model56, which comprises a general factor as well as s-1 specific factors. Here, this implies that two out of the three components of EF have a specific factor. The component without a specific factor (i.e., inhibition) can be interpreted as a reference component that accounts for variance in other components. Its variance is captured in the general factor (gEF), and the variance it shares with the other two EF components is absorbed by the general factor. As a result, the two specific factors can be interpreted as residual variance shared by indicators after accounting for the variance of the reference component (i.e., inhibition). The model therefore has the following factors: (1) a general EF factor (gEF) capturing inhibition as well as its covariance with all other EF indicators; (2) a specific Switching factor (sSwitch) capturing variance shared by indicators of switching over and above what was accounted for by gEF; 3) a specific Working Memory factor (sWM) capturing variance shared by indicators of working memory, over and above what was accounted for by gEF.
To ensure that the gEF, sSwitch and sWM factors captured independent sources of variance, they were not allowed to correlate by statistically constraining their covariance to zero (i.e., they were orthogonal). We also modeled a Reaction Time factor (RT) and a Processing Speed factor (PS), both of which were allowed to correlate with each other and with the three components of executive function. Finally, we included a method factor capturing variance shared by tasks measured in the CNB battery, because we expected a priori that tasks from within the same battery (i.e., D-KEFS vs. CNB) would be more correlated with each other than with tasks from a different battery. Thus, tasks from a specific battery would share common variance that is not shared with tasks from another battery; this variance is assumed to be a methodological artifact. The inclusion of latent factors to account for this kind of artifact is common when using multi-trait, multi-method data57. Although it is theoretically possible to include a method factor for each assessment battery, this strategy often results in statistical problems such as lack of convergence, as was the case in our data. A common solution consists of excluding the method factor for one assessment battery; this was the approach used here. More specifically, we created a latent factor to capture variance that was specific to the CNP battery. Thus, its variance was orthogonal (i.e., uncorrelated) with all other latent factors. This CNP latent factor included loading on the six CNP tasks. All six loadings were statistically significant, indicating that these tasks indeed shared common variance that was not accounted for by the other factors.
Our analyses were performed in four steps. First, we fitted a measurement model with only the outcomes (i.e., EF, RT and PS) to ensure that the hypothesized factor structure adequately fit the data. Second, we documented the associations between childhood ADHD symptoms and vascular risk factors by running an analysis where these were entered simultaneously as predictors of cognitive outcomes using multiple linear regressions. Third, we tested whether cumulative vascular risk mediated the association between ADHD symptoms and cognitive outcomes (Fig. 1). In other words, we aimed to see if the association between ADHD symptoms and cognition was best accounted for by vascular risk severity. For that purpose, we ran a series of structural equation models to test whether ADHD symptoms were associated indirectly with EF, RT and PS via vascular risk factors. The significance of the indirect effect was tested using 1000 bootstrap samples. Finally, we tested whether cumulative vascular risk moderated the association between childhood ADHD symptoms and cognitive outcomes (Fig. 2). In other words, we wanted to see if the strength of the association between ADHD symptoms and cognition varied as a function of vascular risk severity. Age was entered into the regressions as a categorical factor (18–65 years, > 65 years) to mitigate bias introduced by there being very young participants in the sample who were less likely to have cardiovascular risk factors. The age distribution in NKI-RS is bimodal, with peaks around 18 and around 60, and comparatively fewer middle-aged participants; creating an 18–65 group ensured sufficient heterogeneity within this group in terms of age and health risks.
Figure 1.
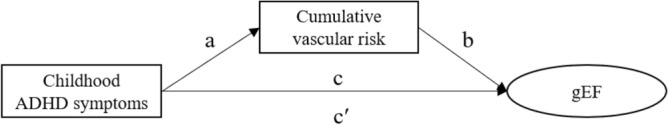
Conceptual model depicting the mediating role of cumulative vascular risk in the association between childhood ADHD symptoms and gEF. Notes. The indirect effect of ADHD symptoms on gEF via cumulative vascular risk is calculated by multiplying the “a” and “b” paths. The direct effect (c’) represents the effect of childhood ADHD symptoms on gEF after controlling for cumulative vascular risk. The total effect (c path) is the sum of the indirect (a*b) and direct (c’) effects. The same model is applied for each cognitive outcome.
Figure 2.
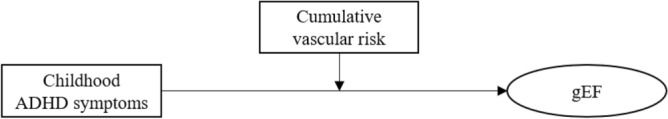
Conceptual model of the moderating role of cumulative vascular risk. Note. The association between childhood ADHD symptoms and gEF varies as a function of the level of cumulative vascular risk. The same model is applied to each cognitive outcome.
Because age contributes independently to declines in executive functioning58 and vascular risk59, we also considered the moderating effect of age on these factors by conducting analyses testing whether age predicted either the cumulative risk score or executive functioning, including an interaction between the predictors and age as a categorical factor.
Results
Participants
Participant characteristics are reported in Table 1. The sample was 63.8% female and 75.7% White, with an average age of 47.2 years (SD = 18.0) and an average education of 15.5 years (SD = 2.3). Childhood ADHD symptom scores within the sample ranged from 0 to 30 (M = 2.0, SD = 4.0), and 50 participants (4.6%) met diagnostic criteria for one of the ADHD subtypes (22 inattentive, 5 hyperactive/impulsive, 9 combined, and 14 not otherwise specified) as determined by an NKI-RS clinician during assessment. Fifteen participants in the sample (1.4%) were taking stimulant medications at the time of testing (amphetamine/dextroamphetamine in six cases, methylphenidate in five, and lisdexamfetamine in four). The two most frequent vascular risk factors in the sample were obesity and hypercholesterolemia, observed in 30.5% and 23.9% of cases respectively. Most people had no vascular risk factors (42.9%), fewer people had only one (35.3%) or two risk factors (17.6%), and a small proportion of people had three or more risk factors (4.2%).
Table 1.
Characteristics of the study sample.
| Age (mean years, SD) | 47.2 (18.0) |
| Sex (% female) | 63.8% |
| Education (mean years, SD) | 15.5 (2.3) |
| Race | |
| American Indian or Native Alaskan | 0.9% |
| Asian | 4.9% |
| Black or African American | 15.5% |
| Native Hawaiian or Other Pacific Islander | 0.5% |
| White | 75.7% |
| Other Race | 2.4% |
| Clinical diagnosis of ADHD (determined by NKI-RS clinicians) | 4.6% |
| Vascular risk factors | |
| Diabetes (self-reported, or fasting glucose level ≥ 140.0 mg/dL) | 5.9% |
| Tobacco use in last 2 years (self-reported) | 12.7% |
| Obesity (BMI > 30 kg/m2) | 30.5% |
| Hypertension (systolic blood pressure > 140.0 mm/Hg) | 9.4% |
| Hypercholesterolemia (non-HDL cholesterol > 158 mg/dL) | 23.9% |
| Number of vascular risk factors | |
| 0 | 42.9% |
| 1 | 35.3% |
| 2 | 17.6% |
| 3 | 3.6% |
| 4 | 0.5% |
| 5 | 0.1% |
ADHD: attention-deficit/hyperactivity disorder. BMI: body mass index. gEF: general executive factor. HDL: high density lipoprotein. NKI-RS: Nathan Kline Institute Rockland Sample. PS: processing speed factor. RT: reaction time factor. SD: standard deviation. sSwitch: Switching factor. sWM: working memory factor.
Measurement model
The fit of the model was good to very good, χ2 (85) = 312.037, p < 0.0001, CFI = 0.951, TLI = 0.931, RMSEA = 0.050 (Fig. 3). All factor loadings were significant except one (digit span backward onto sWM), showing that indicators loaded well onto their hypothesized factor. RT and PS were associated with all EF latent factors, except for RT which was not associated with sWM. In terms of effect size, gEF showed medium to large associations with RT and PS (r = -0.28, p < 0.001 and r = 0.45, p < 0.001), sWM showed small associations with both RT and PS (r = 0.08, p > 0.05 and r = 0.19, p < 0.001), and sSwitch showed large associations with RT and PS (r = -0.46, p < 0.001 and r = -0.87, p < 0.001). RT and PS were also significantly associated (r = 0.48, p < 0.001).
Figure 3.
Confirmatory factor analysis of the cognitive outcomes with standardized factor loadings. Notes. Double-headed arrows represent correlations between latent factors. The methodological factor capturing covariance between indicators measured in the Pennsylvania Computerized Neurocognitive Battery (CNB) battery is not depicted for the sake of clarity. Cond4 = Condition 4. CPT—RT-LT = Continuous Performance Test reaction time on letter trials. CPT—RT-NT = Continuous Performance Test reaction time on number trials. CWI—CN/WR = Color Word Interference color naming/word reading. DF = Design Fluency. gEF = General executive function. TMT—LS = Trail Making Test letter sequencing. TMT—NS = Trail Making Test number sequencing. TMT-VS = Trail Making Test visual scanning. PS = Processing speed. RT = Reaction time. Sort = Sorting. Spec = Specificity. VF = Verbal fluency. WM = Working memory.
Associations between each risk factor and cognitive measures
Inspection of associations between ADHD symptoms and EF revealed that childhood ADHD symptoms were correlated with gEF (r = -0.10, p = 0.018) and sWM (r = 0.10, p = 0.025), but there were no significant associations between current ADHD symptoms and any variable. Thus, there were differential associations despite the fact that childhood and current ADHD symptoms were moderately associated (r = 0.53, p < 0.001). Given this finding, the following analyses were performed using childhood ADHD symptoms unless otherwise noted.
To investigate associations between individual risk factors and cognitive measures, all risk factors were entered simultaneously as predictors of each of the five cognitive outcomes in multiple linear regressions. These effects are reported in Table 2. For gEF, there was a medium negative effect of age and smoking, as well as a small negative effect of childhood ADHD symptoms, obesity, and hypertension. The only significant effect for sWM was a small positive effect of childhood ADHD symptoms. For sSwitch, there was a large negative effect of age, as well as a moderate positive effect of being female. For RT, there was a medium negative effect of age, a small negative effect of being female, and a medium negative effect of diabetes. For PS, there was a large negative effect of age, a medium negative effect of hypertension and a small negative effect of smoking (because higher RT and PS scores represent worse performance, positive effect sizes in Tables 2 and 3 represent deleterious effects on cognition).
Table 2.
Standardized effects of individual risk factors predicting each outcome entered simultaneously in multiple linear regressions.
| gEF | sWM | sSwitch | RT | PS | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| β | p value | β | p value | β | p value | β | p value | β | p value | |
| Age (≥ 65 years) | −.50* | .000 | .03 | .845 | −1.07* | .000 | .59* | .000 | 1.10* | .000 |
| Sex (female) | −.06 | .523 | −.10 | .363 | .44* | .006 | .20* | .020 | −.04 | .554 |
| Childhood ADHD symptoms | −.11* | .008 | .10* | .033 | .06 | .398 | .02 | .722 | .01 | .706 |
| Vascular risk factors | ||||||||||
| Diabetes | −.04 | .836 | −.20 | .307 | −.46 | .178 | .43* | .011 | .26 | .052 |
| Smoking | −.51* | .000 | −.14 | .380 | .03 | .892 | .07 | .559 | .25* | .011 |
| Obesity | −.32* | .000 | .22 | .058 | .24 | .151 | .02 | .791 | .10 | .155 |
| Hypertension | −.35* | .010 | −.07 | .659 | −.19 | .481 | .23 | .155 | .41* | .000 |
| Hypercholesterolemia | .15 | .137 | −.09 | .441 | -.19 | .284 | −.03 | .759 | .04 | .611 |
*p < .05. ADHD: ttention-deficit/hyperactivity disorder. gEF: general executive factor. PS: processing speed factor. RT: reaction time factor. sSwitch: Switching factor. sWM: working memory factor. All effects (except ADHD symptoms) are standardized using only the outcome variance (STDY in MPlus) and reflect the increase in standard deviation of the outcome for an increase of one in the raw metric of the predictor. Effect sizes may therefore be interpreted using Cohen’s d (small: d = .20, medium: d = .50, large: d = .80). ADHD symptoms were continuous so their effects were standardized using for the predictor and the outcome variances (STDYX in MPlus). Effect sizes may therefore be interpreted using Cohen’s r (small: r = .10, medium: r = .30, large: r = .50). Because higher RT and PS scores represent worse performance, positive effects represent deleterious effects on cognition.
Table 3.
Standardized effects of individual risk factors and cumulative vascular risk factors predicting each outcome entered simultaneously in multiple linear regressions.
| gEF | sWM | sSwitch | RT | PS | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| β | p value | β | p value | β | p value | β | p value | β | p value | |
| Age (≥ 65 years) | −.46* | .000 | .04 | .781 | −1.18* | .000 | .62* | .000 | 1.13* | .000 |
| Sex (female) | −.02 | .840 | −.10 | .363 | .42* | .008 | .19* | .026 | −.05 | .411 |
| Childhood ADHD symptoms | −.12* | .005 | .11* | .029 | .06 | .354 | .01 | .812 | .01 | .718 |
| Vascular risk factors | ||||||||||
| One risk factor | −.22* | .024 | −.15 | .218 | −.01 | .970 | .14 | .130 | .14 | .053 |
| Two risk factors | −.35* | .003 | .04 | .783 | −.02 | .910 | .10 | .405 | .27* | .003 |
| ≥ Three risk factors | −.78* | .000 | .03 | .904 | −.18 | .664 | .37 | .082 | .62* | .000 |
*p < .05. ADHD: ttention-deficit/hyperactivity disorder. gEF: general executive factor. PS: processing speed factor. RT: reaction time factor. sSwitch: Switching factor. sWM: working memory factor. All effects (except ADHD symptoms) are standardized using only the outcome variance (STDY in MPlus) and reflect the increase in standard deviation of the outcome for an increase of one in the raw metric of the predictor. Effect sizes may therefore be interpreted using Cohen’s d (small: d = .20, medium: d = .50, large: d = .80). ADHD symptoms were continuous so their effects were standardized using for the predictor and the outcome variances (STDYX in MPlus). Effect sizes may therefore be interpreted using Cohen’s r (small: r = .10, medium: r = .30, large: r = .50). Because higher RT and PS scores represent worse performance, positive effects represent deleterious effects on cognition.
Effect of cumulative vascular risk
To then test whether vascular risk factors predict cognitive functioning according to a cumulative model, we computed a cumulative vascular risk score by creating a sum of the five risk factors, regardless of their nature. As there were few people with three or more risk factors (see above), we recoded the cumulative risk score into four categories: 0, 1, 2 and ≥ 3 risk factors.
This cumulative score was used to predict cognitive functioning while also controlling for sex, age and childhood ADHD symptoms (see Table 3 and Fig. 4). For gEF, there was a medium negative effect of age, as well as a small negative effect of childhood ADHD symptoms. Vascular risk factors predicted significantly poorer gEF, with increasing number of risk factors showing increasingly larger effects. The only significant effect for sWM was a small positive effect of childhood ADHD symptoms. For sSwitch, there was a large negative effect of age, as well as a medium positive effect of being female. For RT, there was a medium to large negative effect of age, and a small negative effect of being female. For PS, there was a large negative effect of age, as well as a negative effect of vascular risk, with 2 and ≥ 3 risk factors being significantly associated with poorer processing speed.
Figure 4.
Associations between the number of vascular risk factors and cognitive functioning. Notes. Effects correspond to those from the model estimated and reported in Table 3. All effects are standardized using only the outcome variance (STDY in MPlus) and reflect the increase in standard deviation of the outcome for an increase of one in the raw metric of the predictor. Effect sizes may therefore be interpreted using Cohen’s d (small: d = .20, medium: d = .50, large: d = .80). gEF: general executive factor. PS: processing speed factor. RT: reaction time factor. sSwitch: Switching factor. sWM: working memory factor.
Because vascular risk factors were associated with both gEF and PS, we tested whether the link between vascular risk factors and gEF was accounted for by their effects on processing speed. We ran the model reported in Table 3 but regressed gEF on PS to see whether the effect of vascular risk factors on gEF would diminish. The direct effect of PS on gEF was moderate to large in magnitude (β = 0.424, p = 0.002) and the magnitude of the effects of the number of risk factors was reduced by about half (1 risk factor: β = 0.152, p = 0.107, 2 risk factors: β = 0.236, p = 0.033, ≥ 3 risk factors: β = 0.496, p = 0.013). Although vascular risk factors were indirectly associated to gEF via PS (total effect: b = 0.232, p = 0.000, indirect effect: 0.077, p = 0.011), accounting for about a third of this association (0.077/0.232 = 33.19%), ADHD symptoms were not associated with gEF via PS (total effect: b = 0.933, p = 0.014, indirect effect: 0.035, p = 0.786).
Mediating role of cumulative vascular risk
Contrary to our expectations, there was no association between ADHD symptoms in childhood and cumulative vascular risk (path a in the model shown in Fig. 1) after accounting for age and sex, OR = 1.378, 95% CI [0.684, 2.772]. Consistent with the fact that path a of the mediation model was not significant, we found no evidence that vascular risk factors mediated the link between ADHD symptoms in childhood and any of the cognitive outcomes.
Moderating role of cumulative vascular risk
We then tested whether the association between ADHD symptoms and cognition was moderated by cumulative vascular risk, as this does not rely on the assumption that ADHD symptoms and cumulative vascular risk are associated. Also contrary to our hypothesis, we found no evidence that childhood ADHD symptoms moderated the effect of the number of vascular risk factors (detailed results not reported).
Moderating effect of age
There was no significant interaction between age categories (above/below age 65) and ADHD symptoms in predicting cumulative risk score (b = 0.227, p = 0.791). In predicting the EF components, we looked at the interactions between age and either cumulative risk or ADHD symptoms. None of the interactions were significant in predicting gEF, sWM or sShifting.
Exploratory analyses
We considered the possibility that ADHD symptom subtypes may have differential associations with health outcomes (e.g., perhaps the hyperactive/impulsive subtype is at higher risk for vascular risk factors and poor self care relative to the inattentive subtype). To explore the possibility that meaningful effects of individual symptom subtypes may have been lost in the consolidation of subtypes into a global ADHD measure, we reconducted the above mediation and moderation analyses using inattentive and hyperactive/impulsive symptoms in separate models. All results remained non-significant (detailed results not reported).
Discussion
Using a large community sample, this study aimed to investigate whether the relationship between ADHD symptoms and frontally mediated aspects of cognitive performance could be accounted for by vascular risk factors, which have been commonly reported in ADHD31 and are recognized to increase risk for cognitive impairment in adults18,41,60–62. Although we found that childhood ADHD symptoms and current vascular risk factors were independently associated with aspects of current cognitive performance, we found no evidence that vascular risk mediated or moderated the relationship between ADHD and cognition.
First, we found that childhood ADHD symptoms had only weak negative effects on current general executive functioning (path c in Fig. 2). Although this is contrary to historical conceptualizations of ADHD as primarily a dysexecutive disorder, there is growing recognition that executive dysfunction is not universal in ADHD63. These findings may also reflect community sampling within the NKI-RS, which resulted in relatively few (4.6%) cases who met diagnostic criteria for clinical ADHD. Surprisingly, we found small positive effects of childhood ADHD symptoms on the specific working memory factor, a finding which is particularly difficult to reconcile with prior reports of moderate-magnitude negative associations between ADHD symptoms and working memory performance in adults64. However, because we used a bifactor model, the specific WM and Switching factors are in fact residuals, as they exclude any variance shared with inhibition. Further, the sWM factor was also poorly captured in this sample, given that backwards digit span did not load significantly onto it. Given the factor loadings, the sWM factor captures shared variance by both n-back indicators, and it may thus be argued that this model is capturing task-specific variance rather than true working memory abilities.
Our results additionally revealed mild to moderate negative associations between vascular risk and aspects of cognitive function (path b in Fig. 2), in particular general executive abilities, processing speed and reaction time. The relationship between vascular disease burden and impairments in speeded responding is well documented e.g.,65–70 and is thought to be caused by damage to white matter fibre tracts within frontal-subcortical neuronal circuits71. Also consistent with previous research72, the deleterious effects of vascular risk factors on cognition were additive, with increasing number of risk factors showing increasingly larger effects.
The central question in this study was whether vascular risk factors explained a significant portion of the association between ADHD symptoms and cognitive outcomes. Contrary to our hypothesis, results from this sample demonstrated that the respective effects of ADHD symptoms and vascular risk factors on cognition are largely independent. After controlling for cumulative vascular risk, the direct effect of childhood ADHD symptoms on cognition remained significant, indicating that the association between ADHD symptoms and cognition is not accounted for by the presence or severity of vascular risk factors. At the same time, we found no evidence that childhood ADHD symptoms were linked to vascular health in adulthood in this sample (i.e., a non-significant path a in Fig. 2), which was relatively surprising considering others’ findings of heightened vascular risk in adults with significant childhood ADHD symptoms. Obesity appears to be the most consistent vascular-related comorbidity among adults with ADHD73. Other vascular risk factors are more debated, with some studies finding increased prevalence of comorbidities such as hypertension and diabetes74, and others reporting similar prevalence estimates of cardiovascular disease and most vascular risk markers between adults with and without ADHD75. Even upon testing a model which does not rely on the assumption that ADHD symptoms and vascular risk are associated (i.e., a moderation model), we again found no evidence that vascular risk influenced the direction or strength of the relationship between ADHD symptoms and cognitive outcomes.
These results tentatively suggest that prior reported associations between ADHD and cognitive impairment10,11,13 are not likely driven by vascular disease burden, although our cross-sectional sample composed primarily of non-clinical cases of ADHD precludes definitive conclusions about risk of cognitive decline in clinical ADHD. There is substantial evidence that midlife health factors influence cognitive decline several decades later41,62, and the dataset we used for this study unfortunately did not allow to account for temporal effects between vascular risk and cognition. We are aware of one study examining relationships between ADHD, cognitive outcomes and vascular risk factors longitudinally across a decade, which reported that any associations between a history of diagnosed ADHD and subsequent dementia are lost after controlling for diabetes and obesity10. This suggests that these vascular risk factors may account for considerable variance in the relationship between clinical ADHD and 10-year dementia risk; additional prospective longitudinal studies will be needed to validate these findings in adults across the ADHD symptom severity spectrum, with richer cognitive and behavioural outcomes. Further, there has been increasing recognition of other medical and physical conditions in ADHD12,76 that were not examined here but that may also contribute to cognitive changes into later adulthood, such as liver disease77, epilepsy78 and obstructive sleep apnea79. These conditions should be explored as potential mediators in future work. Similarly, given high rates of depression in ADHD80,81, and the links between vascular disease, depression, and impaired executive function82,83, it will be relevant to investigate the contributions of depression to cognitive decline in later-life ADHD. We are aware of at least one previous study reporting that ADHD symptoms were indirectly associated with cognition via depressive symptoms6, and it will be worthwhile to extend this to clinical ADHD cohorts and examine risk of dementia status.
In addition, NKI-RS constitutes a community sample, which includes very few cases of clinical ADHD (only 50 cases, or 4.6% of the sample) with even fewer of these in the older-adult range (10 cases, or 1% of the sample). It is possible that only individuals with very severe symptoms of ADHD experience significant vascular burden, potentially due to chronic stimulant medication use84, poor dietary and exercise habits85, or increased vascular inflammatory reactivity86, and adults over age 50 may be especially susceptible74. Our sample may have been underpowered to detect these effects due to few older adults with severe ADHD symptoms. Lastly, it may also be worthwhile for future work to examine the impacts of pharmacological management of ADHD in later life. Available medications include both stimulant and non-stimulant psychotropics, and each may differentially affect ADHD domains and quality of life87.
Conclusion
In summary, results from this large community sample suggest that vascular risk does not play a significant role in explaining the relationship between milder, non-clinical childhood ADHD symptoms and cognition. This question should also be investigated in clinical samples of individuals with more severe ADHD symptomatology, for whom vascular health and cognition may be particularly compromised.
Supplementary Information
Author contributions
BLC conceptualized the study and drafted the manuscript. BLC and AP obtained the data. AP designed and conducted all analyses, and produced all figures. SG conducted the literature review, and cleaned and prepared the data for analysis. ZI provided conceptual guidance with regard to study design, and intellectual contributions to data interpretation. All authors reviewed and approved the manuscript.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Brandy L. Callahan and André Plamondon.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-03782-y.
References
- 1.Michielsen M, Semeijn E, Comijs HC, et al. Prevalence of attention-deficit hyperactivity disorder in older adults in the Netherlands. Br. J. Psychiatry. 2012;201(4):298–305. doi: 10.1192/bjp.bp.111.101196. [DOI] [PubMed] [Google Scholar]
- 2.Hesson J, Fowler K. Prevalence and correlates of self-reported ADD/ADHD in a large national sample of Canadian adults. J Atten. Disord. 2018;22(2):191–200. doi: 10.1177/1087054715573992. [DOI] [PubMed] [Google Scholar]
- 3.Miyake A, Friedman NP. The nature and organization of individual differences in executive functions: four general conclusions. Curr. Dir. Psychol. Sci. 2012;21(1):8–14. doi: 10.1177/0963721411429458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stuss D, Alexander M. Executive functions and the frontal lobes: a conceptual view. Psychol. Res. 2000;63(3–4):289–298. doi: 10.1007/s004269900007. [DOI] [PubMed] [Google Scholar]
- 5.Callahan BL, Plamondon A. Examining the validity of the ADHD concept in adults and older adults. CNS Spectr. 2018;1:1–8. doi: 10.1017/S1092852918001190. [DOI] [PubMed] [Google Scholar]
- 6.Das D, Cherbuin N, Easteal S, Anstey K. Attention deficit/hyperactivity disorder symptoms and cognitive abilities in the late-life cohort of the PATH through life study. PLoS ONE. 2014;9(1):1–12. doi: 10.1371/journal.pone.0086552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Biederman J, Faraone SV. Attention-deficit hyperactivity disorder. Lancet (London, England). 2005;366(9481):237–248. doi: 10.1016/S0140-6736(05)66915-2. [DOI] [PubMed] [Google Scholar]
- 8.Kievit RA, Davis SW, Mitchell DJ, et al. Distinct aspects of frontal lobe structure mediate age-related differences in fluid intelligence and multitasking. Nat. Commun. 2014;5(1):5658. doi: 10.1038/ncomms6658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zanto, T.P., Gazzaley, A. Chapter 20 - Aging of the frontal lobe. In: D’Esposito M, Grafman JHBT-H of CN, eds. The Frontal Lobes. Vol 163. Elsevier; pp. 369–389. doi:10.1016/B978-0-12-804281-6.00020-3
- 10.Fluegge K, Fluegge K. Antecedent ADHD, dementia, and metabolic dysregulation: A US based cohort analysis. Neurochem. Int. 2018;112:255–258. doi: 10.1016/j.neuint.2017.08.005. [DOI] [PubMed] [Google Scholar]
- 11.Tzeng N-S, Chung C-H, Lin F-H, et al. Risk of dementia in adults with ADHD: A nationwide, population-based cohort study in Taiwan. J. Atten. Disord. 2019;23(9):995–1006. doi: 10.1177/1087054717714057. [DOI] [PubMed] [Google Scholar]
- 12.Du Rietz E, Brikell I, Butwicka A, et al. Mapping phenotypic and aetiological associations between ADHD and physical conditions in adulthood in Sweden: A genetically informed register study. Lancet Psychiatry. 2021 doi: 10.1016/S2215-0366(21)00171-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Golimstok A, Rojas JI, Romano M, Zurru MC, Doctorovich D, Cristiano E (2011) Previous adult attention-deficit and hyperactivity disorder symptoms and risk of dementia with Lewy bodies : A case—control study. 1:78–84. 10.1111/j.1468-1331.2010.03064.x [DOI] [PubMed]
- 14.Callahan BL, Bierstone D, Stuss DT, Black SE. Adult ADHD: risk factor for dementia or phenotypic mimic? Front. Aging Neurosci. 2017;9:1–15. doi: 10.3389/fnagi.2017.00260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Broadley MM, White MJ, Andrew B. A systematic review and meta-analysis of executive function performance in type 1 diabetes mellitus. Psychosom. Med. 2017;79(6):684–696. doi: 10.1097/PSY.0000000000000460. [DOI] [PubMed] [Google Scholar]
- 16.Demakakos P, Muniz-Terrera G, Nouwen A. Type 2 diabetes, depressive symptoms and trajectories of cognitive decline in a national sample of community-dwellers: A prospective cohort study. PLoS ONE. 2017;12(4):5827. doi: 10.1371/journal.pone.0175827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Knopman D, Boland LL, Mosley T, et al. Cardiovascular risk factors and cognitive decline in middle-aged adults. Neurology. 2001;56(1):42–48. doi: 10.1212/WNL.56.1.42. [DOI] [PubMed] [Google Scholar]
- 18.Whitmer RA, Sidney S, Selby J, Johnston SC, Yaffe K. Midlife cardiovascular risk factors and risk of dementia in late life. Neurology. 2005;64(2):277–281. doi: 10.1212/01.WNL.0000149519.47454.F2. [DOI] [PubMed] [Google Scholar]
- 19.Yaffe K, Blackwell T, Kanaya AM, Davidowitz N, Barrett-Connor E, Krueger K. Diabetes, impaired fasting glucose, and development of cognitive impairment in older women. Neurology. 2004;63(4):658–663. doi: 10.1212/01.WNL.0000134666.64593.BA. [DOI] [PubMed] [Google Scholar]
- 20.Richards M, Jarvis MJ, Thompson N, Wadsworth MEJ. Cigarette smoking and cognitive decline in midlife: Evidence from a prospective birth cohort study. Am. J. Public Health. 2003;93(6):994–998. doi: 10.2105/AJPH.93.6.994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Benito-León J, Mitchell AJ, Hernández-Gallego J, Bermejo-Pareja F. Obesity and impaired cognitive functioning in the elderly: A population-based cross-sectional study (NEDICES) Eur. J. Neurol. 2013;20(6):899–e77. doi: 10.1111/ene.12083. [DOI] [PubMed] [Google Scholar]
- 22.Deckers K, van Boxtel MPJ, Verhey FRJ, Köhler S. Obesity and cognitive decline in adults: Effect of methodological choices and confounding by age in a longitudinal study. J. Nutr. Health. Aging. 2017;21(5):546–553. doi: 10.1007/s12603-016-0757-3. [DOI] [PubMed] [Google Scholar]
- 23.Pedditizi E, Peters R, Beckett N. The risk of overweight/obesity in mid-life and late life for the development of dementia: A systematic review and meta-analysis of longitudinal studies. Age Ageing. 2016;45:14–21. doi: 10.1093/ageing/afv151. [DOI] [PubMed] [Google Scholar]
- 24.Qiu C, Winblad B, Fratiglioni L. The age-dependent relation of blood pressure to cognitive function and dementia. Lancet Neurol. 2005 doi: 10.1016/S1474-4422(05)70141-1. [DOI] [PubMed] [Google Scholar]
- 25.Gifford KA, Badaracco M, Liu D, et al. Blood pressure and cognition among older adults: a meta-analysis. Arch. Clin. Neuropsychol. 2013;28(7):649–664. doi: 10.1093/arclin/act046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Iadecola C, Yaffe K, Biller J, et al. Impact of hypertension on cognitive function: a scientific statement from the American Heart Association. Hypertens (Dallas, Tex 1979) 2016;68(6):67–94. doi: 10.1161/HYP.0000000000000053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ma C, Yin Z, Zhu P, Luo J, Shi X, Gao X. Blood cholesterol in late-life and cognitive decline: a longitudinal study of the Chinese elderly. Mol. Neurodegener. 2017;12(1):24. doi: 10.1186/s13024-017-0167-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Blumenthal JA, Smith PJ, Mabe S, et al. Lifestyle and neurocognition in older adults with cardiovascular risk factors and cognitive impairment. Psychosom Med. 2017;79(6):719–727. doi: 10.1097/PSY.0000000000000474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liebel SW, Jones EC, Oshri A, et al. Cognitive processing speed mediates the effects of cardiovascular disease on executive functioning. Neuropsychology. 2017;31(1):44–51. doi: 10.1037/neu0000324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nishtala A, Preis SR, Beiser A, et al. Midlife cardiovascular risk impacts executive function: Framingham offspring study. Alzheimer Dis. Assoc. Disord. 2014;28(1):16–22. doi: 10.1097/WAD.0b013e3182a715bc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nigg JT. Attention-deficit/hyperactivity disorder and adverse health outcomes. Clin. Psychol. Rev. 2013;33(2):215–228. doi: 10.1016/j.cpr.2012.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chen M-H, Pan T-L, Hsu J-W, et al. Risk of type 2 diabetes in adolescents and young adults with attention-deficit/hyperactivity disorder. J. Clin. Psychiatry. 2018;79(3):1. doi: 10.4088/JCP.17m11607. [DOI] [PubMed] [Google Scholar]
- 33.Galéra C, Salla J, Montagni I, et al. Stress, attention deficit hyperactivity disorder (ADHD) symptoms and tobacco smoking: The i-Share study. Eur. Psychiatry. 2017;45:221–226. doi: 10.1016/j.eurpsy.2017.07.007. [DOI] [PubMed] [Google Scholar]
- 34.Cortese S, Faraone SV, Bernardi S, Wang S, Blanco C. Adult attention-deficit hyperactivity disorder and obesity: Epidemiological study. Br. J. Psychiatry. 2013;203(01):24–34. doi: 10.1192/bjp.bp.112.123299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fuemmeler BF, Østbye T, Yang C, McClernon FJ, Kollins SH. Association between attention-deficit/hyperactivity disorder symptoms and obesity and hypertension in early adulthood: A population-based study. Int. J. Obes. 2011;35(6):852–862. doi: 10.1038/ijo.2010.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Irmisch G, Richter J, Thome J, Sheldrick AJ, Wandschneider R. Altered serum mono- and polyunsaturated fatty acid levels in adults with ADHD. ADHD Atten. Deficit. Hyperact. Disord. 2013;5(3):303–311. doi: 10.1007/s12402-013-0107-9. [DOI] [PubMed] [Google Scholar]
- 37.Wang HH, Garruti G, Liu M, Portincasa P, Wang DQ-H. Cholesterol and lipoprotein metabolism and atherosclerosis: recent advances in reverse cholesterol transport. Ann Hepatol. 2017;16:21–36. doi: 10.5604/01.3001.0010.5495. [DOI] [PubMed] [Google Scholar]
- 38.Bendayan R, Mascio A, Stewart R, Roberts A, Dobson RJ. Cognitive Trajectories in Comorbid Dementia With Schizophrenia or Bipolar Disorder: The South London and Maudsley NHS Foundation Trust Biomedical Research Centre (SLaM BRC) Case Register. Am. J. Geriatr. Psychiatry. Off. J. Am. Assoc. Geriatr. Psychiatry. 2020 doi: 10.1016/j.jagp.2020.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nooner KB, Colcombe SJ, Tobe RH, et al. The NKI-rockland sample: A model for accelerating the pace of discovery science in psychiatry. Front. Neurosci. 2012;6:152. doi: 10.3389/fnins.2012.00152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Adler L, Cohen J. Diagnosis and evaluation of adults with attention-deficit/hyperactivity disorder. Psychiatr. Clin. North Am. 2004;27(2):187–201. doi: 10.1016/j.psc.2003.12.003. [DOI] [PubMed] [Google Scholar]
- 41.Exalto LG, Quesenberry CP, Barnes D, Kivipelto M, Biessels GJ, Whitmer RA. Midlife risk score for the prediction of dementia four decades later. Alzheimer’s Dement. 2014;10(5):562–570. doi: 10.1016/j.jalz.2013.05.1772. [DOI] [PubMed] [Google Scholar]
- 42.Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström test for nicotine dependence: A revision of the Fagerström tolerance questionnaire. Br. J. Addict. 1991;86(9):1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- 43.Moriyama K, Takahashi E. Non-HDL cholesterol is a more superior predictor of small-dense LDL cholesterol than LDL cholesterol in Japanese subjects with TG levels <400 mg/dL. J. Atheroscler. Thromb. 2016;23(9):1126–1137. doi: 10.5551/jat.33985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gur R, Ragland JD, Moberg PJ, et al. Computerized neurocognitive scanning: I. Methodology and validation in healthy people. Neuropsychopharmacology. 2001;25(5):766–776. doi: 10.1016/S0893-133X(01)00278-0. [DOI] [PubMed] [Google Scholar]
- 45.Delis DC, Kaplan E, Kramer JH. Delis Kaplan Executive Function System: Technical Manual. Psychological Corporation; 2001. [Google Scholar]
- 46.Wechsler D. Manual for the Wechsler Memory Scale-Revised. The Psychological Corporation; 1987. [Google Scholar]
- 47.Diamond A. Executive functions. Annu Rev Psychol. 2013;64(1):135–168. doi: 10.1146/annurev-psych-113011-143750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Baddeley A. Working memory. Science. 1992;255(5044):556–559. doi: 10.1126/science.1736359. [DOI] [PubMed] [Google Scholar]
- 49.Salthouse TA. Aging and measures of processing speed. Biol Psychol. 2000;54(1–3):35–54. doi: 10.1016/S0301-0511(00)00052-1. [DOI] [PubMed] [Google Scholar]
- 50.Sheppard LD, Vernon PA. Intelligence and speed of information-processing: A review of 50 years of research. Pers Individ Dif. 2008;44(3):535–551. doi: 10.1016/J.PAID.2007.09.015. [DOI] [Google Scholar]
- 51.Asparouhov, T., & Muthén, B. Weighted Least Squares Estimation with Missing Data. (2010).
- 52.Asparouhov, T., & Muthén, B. Multiple Imputation with Mplus. (2010).
- 53.Yu C-Y. Evaluating cutoff criteria of model fit indices for latent variable models with binary and continuous outcomes. Unpubl Dr Diss. 2002.
- 54.Marsh, H.W., Hau, K.-T., Grayson, D. Goodness of fit in structural equation models. In: Maydeu-Olivares A, McArdle JJ, eds. Multivariate Applications Book Series. Contemporary Psychometrics: A Festschrift for Roderick P. McDonald. Mahwah, NJ: Lawrence Erlbaum Associates Publishers; 2005:275–340.
- 55.Snyder HR, Miyake A, Hankin BL. Advancing understanding of executive function impairments and psychopathology: Bridging the gap between clinical and cognitive approaches. Front. Psychol. 2015;6:328. doi: 10.3389/fpsyg.2015.00328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Burns GL, Geiser C, Servera M, Becker SP, Beauchaine TP. Application of the Bifactor S - 1 Model to Multisource Ratings of ADHD/ODD Symptoms: An Appropriate Bifactor Model for Symptom Ratings. J. Abnorm. Child Psychol. 2020;48(7):881–894. doi: 10.1007/s10802-019-00608-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Geiser C, Hintz FA, Leonard Burns G, Servera M. Structural equation modeling of multiple-indicator multimethod-multioccasion data: A primer. Pers. Individ. Dif. 2019;136:79–89. doi: 10.1016/j.paid.2017.04.032. [DOI] [Google Scholar]
- 58.Ferguson HJ, Brunsdon VEA, Bradford EEF. The developmental trajectories of executive function from adolescence to old age. Sci. Rep. 2021;11(1):1382. doi: 10.1038/s41598-020-80866-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Costantino S, Paneni F, Cosentino F. Ageing, metabolism and cardiovascular disease. J. Physiol. 2016;594(8):2061–2073. doi: 10.1113/JP270538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.O’Brien JT, Markus HS. Vascular risk factors and Alzheimer’s disease. BMC Med. 2014;12(1):218. doi: 10.1186/s12916-014-0218-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Okonkwo OC, Cohen RA, Gunstad J, Tremont G, Alosco ML, Poppas A. Longitudinal trajectories of cognitive decline among older adults with cardiovascular disease. Cerebrovasc. Dis. 2010;30(4):362–373. doi: 10.1159/000319564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kivipelto M, Helkala EL, Laakso MP, et al. Midlife vascular risk factors and Alzheimer’s disease in later life: longitudinal, population based study. BMJ. 2001;322(7300):1447–1451. doi: 10.1136/bmj.322.7300.1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Willcutt E, Doyle A, Nigg J, Faraone S, Pennington B. Validity of the executive function theory of attention-deficit/hyperactivity disorder: A meta-analytic review. Biol. Psychiatry. 2005;57(11):1336–1346. doi: 10.1016/j.biopsych.2005.02.006. [DOI] [PubMed] [Google Scholar]
- 64.Alderson RM, Kasper LJ, Hudec KL, Patros CHG. Attention-deficit/hyperactivity disorder (ADHD) and working memory in adults: A meta-analytic review. Neuropsychology. 2013;27(3):287–302. doi: 10.1037/a0032371. [DOI] [PubMed] [Google Scholar]
- 65.Badran A, Hollocks MJ, Brookes RL, Morris RG, Markus HS. Framingham vascular age is associated with worse cognitive performance in the middle-aged and elderly. Neuropsychol. Dev. Cogn. Sect. B, Aging Neuropsychol. Cogn. 2019;26(4):531–540. doi: 10.1080/13825585.2018.1499866. [DOI] [PubMed] [Google Scholar]
- 66.Kramer JH, Reed BR, Mungas D, Weiner MW, Chui HC. Executive dysfunction in subcortical ischaemic vascular disease. J Neurol. Neurosurg. Psychiatry. 2002;72(2):217–220. doi: 10.1136/jnnp.72.2.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Cees De Groot J, De Leeuw F-E, Oudkerk M, et al. Cerebral white matter lesions and cognitive function: The Rotterdam scan study. Ann. Neurol. 2000;47(2):145–151. doi: 10.1002/1531-8249(200002)47:2<145::AID-ANA3>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 68.O’Brien JT, Erkinjuntti T, Reisberg B, et al. Vascular cognitive impairment. Lancet Neurol. 2003;2(2):89–98. doi: 10.1016/S1474-4422(03)00305-3. [DOI] [PubMed] [Google Scholar]
- 69.Black SE. Vascular cognitive impairment: epidemiology, subtypes, diagnosis and management. J. R. Coll. Physicians. Edinb. 2011;41(1):49–56. doi: 10.4997/JRCPE.2011.121. [DOI] [PubMed] [Google Scholar]
- 70.van den Berg E, Geerlings MI, Biessels GJ, Nederkoorn PJ, Kloppenborg RP. White Matter Hyperintensities and Cognition in Mild Cognitive Impairment and Alzheimer’s Disease: A Domain-Specific Meta-Analysis. J Alzheimers Dis. 2018;63(2):515–527. doi: 10.3233/JAD-170573. [DOI] [PubMed] [Google Scholar]
- 71.Duering M, Gesierich B, Seiler S, et al. Strategic white matter tracts for processing speed deficits in age-related small vessel disease. Neurology. 2014;82(22):1946–1950. doi: 10.1212/WNL.0000000000000475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Dregan A, Stewart R, Gulliford MC. Cardiovascular risk factors and cognitive decline in adults aged 50 and over: a population-based cohort study. Age Ageing. 2013;42(3):338–345. doi: 10.1093/ageing/afs166. [DOI] [PubMed] [Google Scholar]
- 73.Cortese S, Moreira-Maia CR, St Fleur D, Morcillo-Peñalver C, Rohde LA, Faraone SV. Association Between ADHD and Obesity: A Systematic Review and Meta-Analysis. Am. J. Psychiatry. 2016;173(1):34–43. doi: 10.1176/appi.ajp.2015.15020266. [DOI] [PubMed] [Google Scholar]
- 74.Chen Q, Hartman CA, Haavik J, et al. Common psychiatric and metabolic comorbidity of adult attention-deficit/hyperactivity disorder: A population-based cross-sectional study. PLoS ONE. 2018;13(9):e0204516. doi: 10.1371/journal.pone.0204516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hodgkins P, Montejano L, Sasané R, Huse D. Cost of illness and comorbidities in adults diagnosed with attention-deficit/hyperactivity disorder: a retrospective analysis. Prim Care Compan. CNS Disord. 2011;13(2):1. doi: 10.4088/PCC.10m01030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Cortese S, Solmi M, Arrondo G, et al. Association between mental disorders and somatic conditions: Protocol for an umbrella review. Evid. Based Ment. Health. 2020;23(4):135–139. doi: 10.1136/ebmental-2020-300158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bassendine MF, Taylor-Robinson SD, Fertleman M, Khan M, Neely D. Is Alzheimer’s disease a liver disease of the brain? J. Alzheimers Dis. 2020;75(1):1–14. doi: 10.3233/JAD-190848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Stefanidou M, Beiser AS, Himali JJ, et al. Bi-directional association between epilepsy and dementia The Framingham Heart Study. Neurology. 2020;95(24):E3241–E3247. doi: 10.1212/WNL.0000000000011077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Weihs A, Frenzel S, Grabe HJ. The link between obstructive sleep apnoea and neurodegeneration and cognition. Curr. Sleep Med. Rep. 2021;7(3):87–96. doi: 10.1007/s40675-021-00210-5. [DOI] [Google Scholar]
- 80.Sobanski E, Brüggemann D, Alm B, et al. Psychiatric comorbidity and functional impairment in a clinically referred sample of adults with attention-deficit/hyperactivity disorder (ADHD) Eur. Arch. Psychiatry Clin. Neurosci. 2007;257(7):371–377. doi: 10.1007/s00406-007-0712-8. [DOI] [PubMed] [Google Scholar]
- 81.Sobanski E. Psychiatric comorbidity in adults with attention-deficit/hyperactivity disorder (ADHD) Eur. Arch. Psychiatry Clin. Neurosci. 2006;256(1):i26–i31. doi: 10.1007/s00406-006-1004-4. [DOI] [PubMed] [Google Scholar]
- 82.Lugtenburg A, Oude Voshaar RC, Van Zelst W, Schoevers RA, Enriquez-Geppert S, Zuidersma M. The relationship between depression and executive function and the impact of vascular disease burden in younger and older adults. Age Ageing. 2017;46(4):697–701. doi: 10.1093/ageing/afx043. [DOI] [PubMed] [Google Scholar]
- 83.Sneed JR, Culang-Reinlieb ME. The vascular depression hypothesis: an update. Am. J. Geriatr. Psychiatry. 2011;19(2):99–103. doi: 10.1097/jgp.0b013e318202fc8a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Hennissen L, Bakker MJ, Banaschewski T, et al. Cardiovascular Effects of Stimulant and Non-Stimulant Medication for Children and Adolescents with ADHD: A Systematic Review and Meta-Analysis of Trials of Methylphenidate, Amphetamines and Atomoxetine. CNS Drugs. 2017;31(3):199–215. doi: 10.1007/s40263-017-0410-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Landau Z, Pinhas-Hamiel O. Attention Deficit/Hyperactivity, the Metabolic Syndrome, and Type 2 Diabetes. Curr. Diab. Rep. 2019;19(8):46. doi: 10.1007/s11892-019-1174-x. [DOI] [PubMed] [Google Scholar]
- 86.Yang LL, Stiernborg M, Skott E, Söderström Å, Giacobini M, Lavebratt C. Proinflammatory mediators and their associations with medication and comorbid traits in children and adults with ADHD. Eur. Neuropsychopharmacol. J. Eur. Coll. Neuropsychopharmacol. 2020;41:118–131. doi: 10.1016/j.euroneuro.2020.10.005. [DOI] [PubMed] [Google Scholar]
- 87.Cortese S. Pharmacologic treatment of attention deficit-hyperactivity disorder. N. Engl. J. Med. 2020;383(11):1050–1056. doi: 10.1056/NEJMra1917069. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.




