Abstract
The complex relationships among social support, experienced stigma, psychological distress, and quality of life (QOL) among tuberculosis (TB) patients are insufficiently understood. The purpose of this study was to explore the interrelationships among social support, experienced stigma, psychological distress, and QOL and to examine whether experienced stigma and psychological distress play a mediating role. A cross-sectional survey was conducted between November 2020 and March 2021 in Dalian, Liaoning Province, Northeast China. Data were obtained from 473 TB patients using a structured questionnaire. Structural equation modelling was used to examine the hypothetical model. The research model provided a good fit to the measured data. All research hypotheses were supported: (1) social support, experienced stigma and psychological distress were associated with QOL; (2) experienced stigma fully mediated the effect of social support on psychological distress; (3) psychological distress fully mediated the effect of experienced stigma on QOL; and (4) experienced stigma and psychological distress were sequential mediators between social support and QOL. This study elucidated the pathways linking social support, experienced stigma, and psychological distress to QOL and provides an empirical basis for improving the QOL of TB patients.
Subject terms: Tuberculosis, Quality of life
Introduction
Tuberculosis (TB) is a major infectious disease that poses a serious threat to human health and has significant negative social and economic consequences1,2. It leads to poor health for millions of people every year and is a major public health problem1. In 2019, there were an estimated 10 million new cases of TB worldwide, of which approximately 833,000 were in China, accounting for 8.4% of the global total, ranking third1. TB is also the leading cause of death from infectious diseases globally, and approximately 1.41 million people died of TB in 2019, of whom approximately 33,000 died in China, accounting for 2.4% of the global total1. The burden of TB remains high in China. Although the suffering caused by TB has been acknowledged for thousands of years, most current TB programs and research have primarily focused on detection, microbiological treatment, prevention, and control, while the quality of life (QOL) of TB patients has been neglected3,4.
Although effective anti-TB drugs are available and TB patients have access to effective treatment, TB infectivity, chronic progression, long-term drug treatment over a period of at least 6 months and drug side effects have significantly affected patients’ daily lives, thus affecting their QOL5–7. Research has confirmed that TB patients tend to have poor QOL, demonstrating QOL significantly worse than that of the general population8,9. The World Health Organization (WHO) defined QOL as an individual’s perception of their position in life within the cultural context and value system in which they live and in relation to their goals, expectations, standards, and concerns10. In addition, QOL refers to a person’s subjective assessment of their life’s satisfaction and meaning11. QOL can affect treatment adherence in TB patients, while non-adherence to TB treatment is thought to be an important reason for the gap between high financial inputs and poor performance in TB control12–14. More importantly, impairments in QOL are associated with poor treatment outcomes, which can increase TB mortality and morbidity and negatively impact TB control15. Therefore, it is necessary to explore the factors that influence the QOL of TB patients and to improve the QOL of TB patients. Previous studies have analysed factors associated with QOL. They found that sex, age, education level, marital status, occupational status, monthly income, drug side effects, comorbidities, body mass index (BMI), type of TB, phase of treatment, stigma, depressive symptoms, and social support were associated with QOL2,6,16,17.
Social support refers to the amount of perceived and practical care received from family, friends and/or the community18. Previous studies have shown that social support affects the QOL of TB patients9,19. Patients with adequate social support from family, friends and community are likely to have better QOL20. Furthermore, social support was also an important predictor of stigma21. Patients with poor social support are more likely to be isolated and alienated, with manifestations such as being denied shared utensils and food by family members and losing their jobs, which may lead to stigma22,23. Additionally, good social support will increase life satisfaction and social confidence, enabling patients to adapt to a crisis and reducing the pressure of the patient’s role change, thus also reducing the risk of psychological distress24. Previous studies have also demonstrated that perceived social support is associated with psychological distress in TB patients during treatment25.
Because TB is transmitted by droplets and is highly contagious, patients with TB often experience great stigma, whether at home, in the workplace or in the community26. Studies of patients from a variety of backgrounds have indicated that between 42 and 82% of TB patients report stigma27,28. Research has suggested that social stigma may affect life satisfaction in TB patients during and even after treatment15, and TB-associated stigma is one of the most important aspects affecting QOL29. Stigma disrupts patients’ social interactions with others and reduces social functioning and ability to fulfil daily roles, ultimately endangering patients’ QOL2. In addition, studies conducted in rural China and Ethiopia have shown that experienced stigma is significantly associated with psychological distress30,31. TB patients who feel stigmatized may less frequently use health services and conceal their illness because of low self-esteem and social isolation. Moreover, studies have reported that TB-associated stigma is associated with psychological stress disorders. These factors can increase the risk of mental health problems, such as psychological distress21,32,33.
The main factor that affects the QOL of patients with TB is psychological distress34. Studies have indicated that once TB is diagnosed, a wide variety of psychological responses are observed, for example, 51.9% to 81% of TB patients suffer from psychological distress30,35,36. Studies have also reported that the presence of mental health problems is the strongest predictor of decreased QOL8, and depression is also believed to be an important cause of poor QOL in patients with chronic diseases37. Notably, psychosocial burdens may have a greater impact than clinical symptoms in TB patients34. Psychological distress may interfere with an individual’s immune response system and affect adherence to anti-TB treatment, which may lead to poor QOL and exacerbate mortality from the disease38,39.
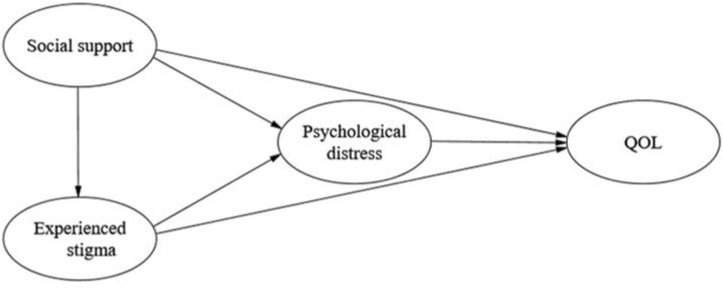
QOL of TB patients is generally neglected in existing national TB control programs17, and the lack of research on influencing factors of QOL may be one of the key reasons. As mentioned above, previous studies mainly relied on regression analysis and mostly explored only the direct relationships among variables. The pathways reflecting social support, experienced stigma, and psychological distress effects on QOL remain unclear. Without this understanding, it is difficult to determine precisely which variables should be the primary target of QOL priority interventions. Structural equation modelling (SEM), however, aims to decompose the direct and indirect effects of variables, discover the potential and important associations, and produce a more complete picture of causal effect mechanisms to understand the mechanisms and pathways that might explain these relationships40,41. In addition, the SEM incorporates measurement errors into the research model, which is more robust than the regression model42,43. The use of SEM enables us to untangle the complex relationships among social support, experienced stigma, psychological distress and QOL. Understanding the mechanisms and pathways of the relationship among social support, experienced stigma, psychological distress and QOL can help accurately determine the intervention objectives to improve QOL for TB patients, improve the effectiveness of intervention measures, achieve better clinical management, and ultimately increase the possibility of obtaining the best treatment outcomes and achieving the WHO’s strategy to end TB. Based on the above theory and empirical research results, we proposed a hypothetical model (Fig. 1). As illustrated in Fig. 1, the current study aimed to test the following hypotheses: (1) social support, experienced stigma, and psychological distress are associated with QOL (H1); (2) experienced stigma mediates the relationship between social support and psychological distress (H2); (3) psychological distress mediates the relationship between experienced stigma and QOL (H3); and (4) experienced stigma and psychological distress are sequential mediators from social support to QOL (H4). According to these research hypotheses, we suggest ways to improve the QOL of TB patients.
Figure 1.
Hypothetical model of relationships among social support, experienced stigma, psychological distress, and QOL. QOL quality of life.
Methods
Study design and setting
A cross-sectional, questionnaire-based survey was carried out between November 2020 and March 2021 at three TB medical institutions in Dalian, Liaoning Province, Northeast China. The three medical institutions were selected based on the number of patients attending, type of patient and location. The first is the only tertiary specialized hospital for TB prevention and control in Dalian and is divided into northern and southern parts located in Ganjingzi District and Pulandian District, respectively. It currently has nearly 500 beds, serving the whole city’s TB patients, especially critically ill TB patients, as the main medical institution for TB patients in Dalian. The other two institutions are TB dispensaries located in Lushunkou District and Zhuanghe City (a county-level city), which serve only local TB patients with a milder instance of the disease.
Participants
TB patients who attended the selected TB medical institutions between November 2020 and March 2021 were recruited as participants. The inclusion criteria were patients with a definite TB diagnosis according to national TB program guidelines, aged 18 years or older and with a new or relapsed case of TB undergoing treatment. The exclusion criteria were patients with psychosis, communication problems, or difficulty understanding the questionnaire and completion of treatment. A total of 481 patients were recruited and completed a structured questionnaire. Of the 481 questionnaires obtained, eight were excluded due to logical errors or large amounts of missing data. Ultimately, this study included 473 TB patients, with a participation rate of 98.34%.
Ethics procedure
Ethical approval was provided by the Ethics Committee of Dalian Medical University, Liaoning Province, China. Before participating in the study, each participant was informed of the purpose of the study and how the results would be presented and received guarantees that their personal information would not be disclosed. Each participant voluntarily signed an informed consent form to participate in our study. All methods in our study were conducted in accordance with relevant guidelines and regulations (Declaration of Helsinki).
Measurement
A structured questionnaire consisting of questions concerning demographic characteristics, treatment status, social support, experienced stigma, psychological distress, and QOL was developed by reading a large amount of relevant literature and consulting experts in related fields. Demographic characteristics included sex, age, marital status and education level. Treatment status included the category of TB treatment, phase of treatment and self-assessed disease severity.
Social support
Social support was measured using the Oslo 3-item social support scale, a 3-item questionnaire that is commonly used to assess social support-related issues in clinical and community settings44. This questionnaire contains questions that ask patients about the number of people they feel close to and on whom they could count on for serious problems, how much people cared about them and the ease with which they could receive practical help from neighbours. Its overall score ranges from 3 to 14, with a high score indicating a high level of social support. In the current study, the scale’s Cronbach’s α reliability coefficient was 0.718.
Experienced stigma
Experienced stigma was assessed using a 9-item stigma questionnaire developed in accordance with Chinese social and cultural contexts45. The questionnaire assesses the stigma experienced by patients on the three dimensions of prejudice, discrimination, and rejection. Responses to each item were rated on a 4-point Likert scale, ranging from strongly disagree (= 1) to strongly agree (= 4). The scores of each item were summed to obtain the total score (range 9–36). Higher scores indicate higher levels of stigma experienced by TB patients. The scale showed good reliability and validity, and its Cronbach’s α in this study was 0.946.
Psychological distress
The Kessler Psychological Distress Scale (K-10) questionnaire was used to assess psychological distress in TB patients46. Numerous studies have demonstrated the reliability and validity of this scale30. The scale is composed of 10 items divided among four subscales: nervousness, agitation, fatigue and negative affect47. Negative affect includes hopelessness, low mood, sadness and a sense of worthlessness. An example of such an item is “How often did you feel hopeless in the last 30 days?”. The frequency of each item was recorded on a 5-point Likert scale, ranging from none of the time (= 1) to all the time (= 5). The overall score ranged from a low of 10 to a high of 50, indicating an increase in psychological distress. In this study, the scale had high internal consistency (Cronbach’s α = 0.929).
QOL
The QOL is an index of the satisfaction levels of the body, spirit, family and social life and the overall evaluation of life48. In the current study, a 6-item quality of life scale (QOL-6) developed by Phillips in 2002 was used to measure QOL in TB patients49. This scale consists of six items covering physical health, psychological health, economic circumstances, work, family relationships and relationships with nonfamily members. Patients were asked to rate the extent to which the six traits reflected their actual life situation over the past month. Each item was recorded on a 5-point Likert scale, ranging from very poor (= 1) to excellent (= 5). The overall score ranged from 6 to 30, with a high score reflecting good QOL. This scale has been used to assess the QOL of different populations17,49,50. In the current study, the scale had acceptable internal consistency (Cronbach’s α = 0.792). QOL was parcelled to produce three categories using the item parcelling method for the final model analysis51.
Statistical analysis
The complete and correct questionnaires were inputted into the database established using EpiData 3.1 software (EpiData Association, Odense, Denmark) by double entry to ensure the accuracy of the data. The data were exported to SPSS 21.0 (IBM Corporation, Armonk, State of New York) for preliminary statistical analysis. Descriptive statistical analysis included the frequency and percentage of classified data and the mean and standard deviation (SD) of continuous data. T tests and analysis of variance were used to compare QOL scores among different groups. Pearson correlation analysis was used to evaluate bivariate correlations. All comparisons were two-tailed, and P < 0.05 was considered statistically significant.
When multiple potential mediating variables and complex relationships were considered in the research model, we used AMOS 23.0 software (IBM Corporation, Armonk, New York, USA) to conduct structural equation modelling (SEM) to test the hypotheses. Confirmatory factor analysis (CFA) was carried out to test the reliability and validity of the constructs and combined with SEM to improve the research model42. The maximum likelihood method was used to estimate the parameters. Additionally, the 95% confidence interval (CI) was calculated using bootstrapping with 5000 resamples for all effects52. The bootstrapping performed was a non-parametric test that does not rely on assumptions of normal distribution, and the effect was considered statistically significant if the 95% CI did not include zero. The goodness-of-fit index (GFI), comparative fit index (CFI), Tucker-Lewis index (TLI), standardized root mean square residual (SRMR), and root mean squared error of approximation (RMSEA) were calculated to examine the fit of the model. GFI, CFI and TLI values were greater than 0.900, and SRMR and RMSEA values were less than 0.080, indicating adequate goodness of fit53.
Results
Participants’ demographic characteristics and treatment status
Among the 473 participants, the mean age was 48.36 (SD = 17.58) years, and most participants (60.04%) were aged 45 years or older. There were more than twice as many male participants (69.13%) as female participants (30.87%). There were slightly more participants with a high school education or above (34.88%) than those with a middle school education (33.19%) or a primary education or below (31.92%). Nearly two-thirds of the participants (65.33%) were married, and only 72 (15.22%) had relapsed. More than half of the patients (59.20%) were in a continuous phase of treatment, and nearly one-third (29.60%) felt that their current condition was severe. Among the respondents, the average QOL score was 20.41 (SD = 3.65). Age, marital status, education level, treatment category, treatment phase and self-assessed severity were significantly associated with QOL (P < 0.05) (Table 1).
Table 1.
Participants’ demographic characteristics and treatment status and their associations with QOL.
| Variables | Total n (%) | Quality of life | P value | |
|---|---|---|---|---|
| Mean | SD | |||
| Sex | 0.391 | |||
| Male | 327 (69.13) | 20.32 | 3.76 | |
| Female | 146 (30.87) | 20.63 | 3.38 | |
| Age (years) | < 0.001 | |||
| 18–30 | 107 (22.62) | 22.11 | 2.96 | |
| 31–44 | 82 (17.34) | 20.93 | 3.72 | |
| 45 or above | 284 (60.04) | 19.63 | 3.63 | |
| Marriage status | < 0.001 | |||
| Single | 116 (24.52) | 21.02 | 3.91 | |
| Married | 309 (65.33) | 20.61 | 3.40 | |
| Divorced or widowed | 48 (10.15) | 17.69 | 3.46 | |
| Education level | < 0.001 | |||
| Primary or below | 151 (31.92) | 19.01 | 3.69 | |
| Middle school | 157 (33.19) | 20.17 | 3.53 | |
| High school or above | 165 (34.88) | 21.91 | 3.14 | |
| Treatment category | 0.005 | |||
| New | 401 (84.78) | 20.61 | 3.62 | |
| Relapse | 72 (15.22) | 19.31 | 3.64 | |
| Treatment phase | 0.023 | |||
| Intensive phase | 193 (40.80) | 20.86 | 3.28 | |
| Continuous phase | 280 (59.20) | 20.11 | 3.86 | |
| Self-assessed severity | < 0.001 | |||
| Mild | 333 (70.40) | 21.26 | 3.39 | |
| Severe | 140 (29.60) | 18.41 | 3.47 | |
SD standard deviation.
Significant values are given in bold.
Correlations of the variables
The mean scores of social support, experienced stigma, and psychological distress were 9.71 (SD = 2.27), 18.86 (SD = 7.14), and 19.62 (SD = 7.49), respectively. Social support was negatively correlated with experienced stigma (r = − 0.263, P < 0.01) and psychological distress (r = − 0.151, P < 0.01) and positively correlated with QOL (r = 0.579, P < 0.01). In addition, experienced stigma was positively correlated with psychological distress (r = 0.453, P < 0.01) and negatively correlated with QOL (r = − 0.429, P < 0.01). Psychological distress was negatively correlated with QOL (r = − 0.480, P < 0.01) (Table 2).
Table 2.
Descriptive statistics and correlations among study variables.
| Variables | Mean ± SD | Social support | Experienced stigma | Psychological distress |
|---|---|---|---|---|
| Social support | 9.71 ± 2.27 | |||
| Experienced stigma | 18.86 ± 7.14 | − 0.263** | ||
| Psychological distress | 19.62 ± 7.49 | − 0.151** | 0.453** | |
| QOL | 20.41 ± 3.65 | 0.579** | − 0.429** | − 0.480** |
QOL quality of life, SD standard deviation.
All correlations were significant. **P < 0.01.
Reliability and validity of the constructs
Through factor analysis, the unstandardized estimates of each item were significant (P < 0.001), and the standardized factor loadings of each item were > 0.5, which met the physical requirements of factor analysis, indicating that each item has a substantial effect on the measurement of latent variables. The CR value represents the internal consistency of the construct. The higher the CR is, the greater the internal consistency of the tested factors. In this study, all CR values were > 0.7, indicating that the constructs exhibited acceptable internal consistency. Moreover, AVE is the average of the explanatory power of the calculated latent variable to the observed variable. The higher the AVE is, the higher the convergent validity. The value of AVE is recommended to be greater than 0.5. In this study, the AVE ranged from 0.500 to 0.819, which implied that the interpretation degree of latent variables with respect to the observed variables was good and the convergent validity of the constructs was high. The values of s in the diagonal were greater than or slightly lower than the Pearson correlation coefficient of other related constructs. This fact indicates that the discriminant validity among factors is significant and that each factor can be well separated. Overall, these constructs exhibited good reliability and validity54,55 (Tables 3, 4).
Table 3.
Reliability analysis of the constructs.
| Construct | Item | Parameter significance estimation | Std. | SMC | CR | |||
|---|---|---|---|---|---|---|---|---|
| Unstd. | S.E. | t value | P | |||||
| Social support | ss1 | 1.000 | 0.900 | 0.810 | 0.739 | |||
| ss2 | 0.892 | 0.101 | 8.839 | *** | 0.661 | 0.437 | ||
| ss3 | 0.521 | 0.065 | 8.027 | *** | 0.502 | 0.252 | ||
| Experienced stigma | Rejection | 1.000 | 0.926 | 0.857 | 0.931 | |||
| Prejudice | 0.957 | 0.032 | 29.510 | *** | 0.885 | 0.783 | ||
| Discrimination | 0.907 | 0.029 | 30.802 | *** | 0.904 | 0.817 | ||
| Psychological distress | Nervousness | 1.000 | 0.783 | 0.613 | 0.905 | |||
| Agitation | 1.167 | 0.061 | 19.174 | *** | 0.807 | 0.651 | ||
| Fatigue | 1.113 | 0.057 | 19.627 | *** | 0.821 | 0.674 | ||
| Negative affect | 1.162 | 0.051 | 22.670 | *** | 0.942 | 0.887 | ||
| QOL | qol1 | 1.000 | 0.630 | 0.397 | 0.795 | |||
| qol2 | 1.180 | 0.100 | 11.814 | *** | 0.880 | 0.774 | ||
| qol3 | 0.800 | 0.065 | 12.377 | *** | 0.732 | 0.536 | ||
Three items of the Oslo social support scale are labelled ss1, ss2, and ss3. Three categories of the QOL scale are labelled qol1, qol2, and qol3.
QOL quality of life, Unstd. unstandardized estimate, S.E. standard error, Std. standardized estimate/factor loading, SMC squared multiple correlations, CR composite reliability.
***P < 0.001.
Table 4.
Validity analysis of the constructs.
| AVE | QOL | Psychological distress | Experienced stigma | Social support | |
|---|---|---|---|---|---|
| QOL | 0.569 | 0.754 | |||
| Psychological distress | 0.706 | − 0.494 | 0.840 | ||
| Experienced stigma | 0.819 | − 0.470 | 0.492 | 0.905 | |
| Social support | 0.500 | 0.778 | − 0.174 | − 0.326 | 0.707 |
QOL quality of life, AVE average of variance extracted.
The bold values on the diagonal in the table are s, and the values underneath the bold value represent the Pearson correlation coefficients between the constructs.
Fit indices of the overall research model
Table 5 shows the fit indices of the overall research model. To evaluate the fit of the overall model, the following commonly used fitness indices were used: Chi-square test of the model fit = 395.162; degrees of freedom = 125; Chi-square/DF = 3.161; GFI = 0.914; CFI = 0.939; TLI = 0.916; SRMR = 0.072; RMSEA = 0.068. In this context, GFI, CFI and TLI values greater than 0.900 indicate good model fit. SRMR and RMSEA values less than 0.080 suggest adequate model fit. All the fitness indices in the current study met the practical standards or thresholds and reached the ideal level, which indicated that the overall research model fit well56 (Table 5).
Table 5.
Fit indices of the overall research model.
| Index | Criteria | Research model | Support or not |
|---|---|---|---|
| Chi-square | Small is better | 395.162 | Support |
| DF | Large is better | 125 | Support |
| Chi-square/DF | 1 < Chi-square/DF < 5 | 3.161 | Support |
| GFI | > 0.900 | 0.914 | Support |
| CFI | > 0.900 | 0.939 | Support |
| TLI | > 0.900 | 0.916 | Support |
| SRMR | < 0.080 | 0.072 | Support |
| RMSEA | < 0.080 | 0.068 | Support |
DF degrees of freedom, GFI goodness-of-fit index, CFI comparative fit index, TLI Tucker-Lewis index, SRMR standardized root mean square residual, RMSEA root mean squared error of approximation.
Effect analysis of the research model
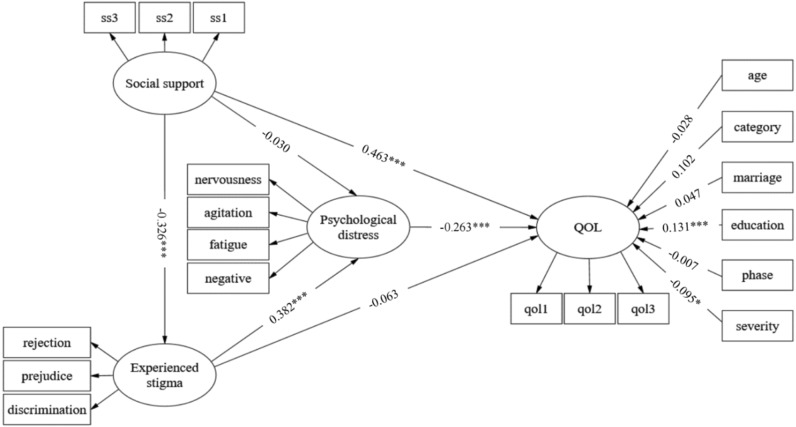
Figure 2 shows the research model with unstandardized path coefficients. Age, marital status, education level, treatment category, treatment phase and self-assessed severity acted as covariates. Education level was positively associated with QOL (β = 0.131, P < 0.001), while self-assessed severity was negatively associated with QOL among TB patients (β = − 0.095, P < 0.05). As shown in Table 6, the total effect of social support on psychological distress was − 0.154 (95% CI (− 0.245, − 0.068) and (− 0.243, − 0.067)). Social support significantly predicted psychological distress via experienced stigma (95% CI (− 0.187, − 0.075) and (− 0.184, − 0.074)). However, the direct effect of social support on psychological distress was nonsignificant (95% CI (− 0.117, 0.052) and (− 0.114, 0.054)). Therefore, experienced stigma fully mediates the effect of social support on psychological distress. The total effect of experienced stigma on QOL was − 0.163 (95% CI (− 0.246, − 0.088) and (− 0.249, − 0.090)). Experienced stigma significantly predicted QOL via psychological distress (95% CI (− 0.156, − 0.095) and (− 0.156, − 0.059)). However, the direct effect of experienced stigma on QOL was also nonsignificant (95% CI (− 0.137, 0.012) and (− 0.137, − 0.011)). Thus, psychological distress fully mediates the effect of experienced stigma on QOL. The total effect of social support on QOL was 0.524 (95% CI (0.435, 0.635) and (0.435, 0.635)), and the direct effect was 0.463 (95% CI (0.386, 0.562) and (0.384, 0.561)), accounting for 88.36% of the total effect. In addition, social support significantly predicted QOL via the sequential mediation variables of experienced stigma and psychological distress (95% CI (0.017, 0.058) and (0.016, 0.057)), whose estimated multiple indirect effect was only 0.033, accounting for 6.30% of the total effect. In sum summary, all the hypotheses were supported (Fig. 2, Table 6).
Figure 2.
Pathway analysis of the relationships among social support, experienced stigma, psychological distress, and QOL. All the coefficients have been unstandardized in the figure. Three items of the Oslo social support scale are labelled ss1, ss2, and ss3. Three categories of the QOL scale are labelled qol1, qol2, and qol3. Age, treatment category, marriage status, education level, treatment phase and self-assessed severity acted as covariates. ***P < 0.001, *P < 0.05. QOL quality of life, negative negative affect, category treatment category, marriage marriage status, education education level, phase treatment phase, severity self-assessed severity. Fit of the model: Chi-square test of the model fit = 395.162; degrees of freedom = 125; GFI = 0.914; CFI = 0.939; TLI = 0.916; SRMR = 0.072; RMSEA = 0.068.
Table 6.
Analysis results of mediating variables (5000 bootstrap samples).
| Relationships | Point estimation | Product of coefficients | Bootstrapping | ||||
|---|---|---|---|---|---|---|---|
| Bias-corrected 95% CI | Percentile 95% CI | ||||||
| S.E | Z | Lower | Upper | Lower | Upper | ||
| Effect from SS to PD | |||||||
| Indirect effect | |||||||
| SS → ES → PD | − 0.124 | 0.028 | − 4.429 | − 0.187 | − 0.075 | − 0.184 | − 0.074 |
| Direct effect | |||||||
| SS → PD | − 0.030 | 0.044 | − 0.682 | − 0.117 | 0.052 | − 0.114 | 0.054 |
| Total effect | |||||||
| SS → PD | − 0.154 | 0.045 | − 3.422 | − 0.245 | − 0.068 | − 0.243 | − 0.067 |
| Effect from ES to QOL | |||||||
| Indirect effect | |||||||
| ES → PD → QOL | − 0.100 | 0.025 | − 4.000 | − 0.156 | − 0.059 | − 0.156 | − 0.059 |
| Direct effect | |||||||
| ES → QOL | − 0.063 | 0.038 | − 1.658 | − 0.137 | 0.012 | − 0.137 | 0.011 |
| Total effect | |||||||
| ES → QOL | − 0.163 | 0.041 | − 3.976 | − 0.246 | − 0.088 | − 0.249 | − 0.090 |
| Effect from SS to QOL | |||||||
| Indirect effect | |||||||
| SS → ES → QOL | 0.021 | 0.013 | 1.615 | − 0.002 | 0.049 | − 0.003 | 0.047 |
| SS → PD → QOL | 0.008 | 0.012 | 0.667 | − 0.013 | 0.033 | − 0.014 | 0.032 |
| SS → ES → PD → QOL | 0.033 | 0.011 | 3.000 | 0.017 | 0.058 | 0.016 | 0.057 |
| Direct effect | |||||||
| SS → QOL | 0.463 | 0.045 | 10.289 | 0.386 | 0.562 | 0.384 | 0.561 |
| Total effect | |||||||
| SS → QOL | 0.524 | 0.052 | 10.077 | 0.435 | 0.635 | 0.435 | 0.635 |
SS social support, ES experienced stigma, PD psychological distress, QOL quality of life, S.E. standard error, CI confidence interval.
Discussion
Patients with TB often have symptoms such as cough, chest pain, low fever, fatigue, and loss of appetite. In addition, the treatment of TB is a complex and lengthy process, requiring many medications and a long period of treatment. These factors significantly affect the QOL of patients17. However, to date, the complex relationships among social support, experienced stigma, psychological distress, and QOL in patients with TB have not been fully explored. To our knowledge, this study was the first to use SEM to explore the interrelationships among social support, experienced stigma, psychological distress, and QOL and to examine whether experienced stigma and psychological distress play mediating roles.
In the current study, factor analysis indicated that each construct displayed good reliability and validity, which further verified the stable structure of the scale in TB patients and provides a basis for future studies to measure the social support, experienced stigma, psychological distress, and QOL of TB patients. More importantly, the fitness indices exhibited good model fit, indicating that our proposed research model is reasonable and provides key information for improving the QOL of TB patients. Moreover, this study found that education level was associated with QOL in terms of demographic characteristics. Previous studies have also demonstrated that education level is an important predictor of QOL, such that a higher education level has a positive effect on the QOL of TB patients2,9. Patients with higher levels of education contribute to greater knowledge about TB from the outside world. Knowledge of TB can improve health-related behaviors such as taking anti-TB drugs on time and seeking care in a timely manner57. This will contribute to the effective control of the disease and reduce the patients’ stigma, thus reducing psychological distress and improving the QOL. However, patients with low levels of education may lack a correct understanding of TB. This often leads to doubt about the ability to cure TB and reduced self-efficacy58. Patients with low self-efficacy also have stronger stigma experience59, which increases the risk of psychological distress and affects the QOL of patients. This study also found that patients with perceived severe illness had worse QOL than those with mild illness. Previous studies have also demonstrated that worse physical symptoms are associated with lower physical health-related QOL and higher mental health-related QOL among TB patients60. Understandably, patients with more severe disease have more complex clinical conditions and longer treatment times, as well as increased patient concerns, which may be particularly damaging to QOL. In addition, it is understandable that the more severe the illness are, the more obvious the symptoms. Obvious symptoms, especially a prolonged cough, may lead to a greater degree of accidental disclosure of the illness. This will have a negative impact on access to social support, increase stigma and psychological distress and threaten QOL.
The results also showed that social support demonstrated a significant, direct effect on the QOL of patients with TB. Social support helps improve patients’ QOL20, which has also been found in studies on patients with traumatic brain injury61. A possible explanation is that patients who receive adequate social support might have improved health outcomes. Moreover, consistent with previous studies, stigma was a predictor of QOL62. Stigma can damage patients’ self-esteem and self-efficacy, lead to patients’ isolation from society and self-concealment, and ultimately endanger patients’ QOL63. In addition, psychological distress exerted a direct effect on QOL in our study. Studies have reported that untreated depression is independently associated with poorer QOL39. Another study also demonstrated that mental distress had a significant effect on QOL6. Patients with psychological distress were less likely to adhere to treatment regimens, thus eliminating the chance of successful treatment, impairing their function, and reducing QOL39,64.
Previous research has demonstrated that patients who receive an adequate amount of social support are likely to have the best mental health outcomes20. Our results suggest that social support can also have an indirect negative effect on psychological distress through experienced stigma. Sufficient social support can increase patients’ self-esteem and make patients more likely to be diagnosed in a timely manner and to comply with treatment, thus reducing the occurrence of psychological distress65,66. In addition, our results confirmed that psychological distress moderated the relationship between experienced stigma and QOL. It is not difficult to understand that the experience of stigma will lead to patients’ feelings of inferiority, lack of confidence and low emotional well-being, which threaten patients’ emotions and cause psychological distress, thus affecting their QOL33. Our results also indicated that experienced stigma and psychological distress are sequential mediators from social support to QOL, a relationship that has not been demonstrated in previous studies. However, the findings seem logical because patients with better social support have more emotional and financial resources, which makes them face less discrimination and stress, and are likely to use drugs with fewer side effects; thus, they may have improved QOL65,67.
In the current study, SEM was used to test the mediating variables. In epidemiological studies, the assessment of mediation has been widely used to open up the “black box”, allowing us to discern complex relationships between variables68. In practice, understanding the interrelationships among social support, experienced stigma, psychological distress and QOL provides an opportunity to intervene effectively in QOL among patients with TB, and it allows for interventions to be tailored to these specific pathways. Specifically, interventions aimed at improving the QOL of TB patients should focus on increasing social support for patients. At the same time, the role of experienced stigma and psychological distress should also be understood and addressed. Given that experienced stigma and psychological distress mediated the effect of social support on QOL in TB patients, interventions should be combined with measures to eliminate stigma and reduce psychological distress. This was essential for improving the QOL of TB patients. Previous studies have demonstrated that family functions and doctor-patient communication are the most important sources of social support for patients69. The attitude of family members has an important influence on TB patients. There are widespread psychological burdens among TB patients, such as lack of confidence in a cure and fear of treatment failure70. Constant encouragement from and care by family members can increase patients’ confidence and their feelings of being taken care of. Therefore, family members can be educated and trained to provide better support for patients. Doctors also play an important role in the treatment of TB, and a good doctor-patient relationship is the fundamental factor to ensure the normal operation of the treatment process. It is necessary to require medical staff to establish the concept of patient-centred service and to show respect and humanistic care in the process of medical service delivery71. It is also important to provide more financial support for patients. Although the country has established some free TB treatment policies, some items, such as the cost of expensive adjuvant drugs, are not included in the free package. Previous studies have also found that TB clubs, composed of health workers and TB patients, have been successful in reducing stigma among TB patients72. In addition, community awareness and patient education may contribute significantly to a reduction in stigma73.
This study has several limitations that need to be addressed in future studies. First, although SEM was applied, the causal relationship between the variables could not be inferred due to the cross-sectional nature of the data. Therefore, longitudinal studies are needed to validate the current findings. Second, the study sample only included TB patients from Dalian, Liaoning Province, Northeast China, which limited the ability to generalize the results to individuals from other regions with different social and cultural backgrounds. Future research should expand the study area to determine the suitability of our study model. Additionally, the study was limited to TB patients who already had access to health care, while those who did not seek any care were not recruited. The latter are probably the most marginalized and affected by TB, and their participation could enrich our findings. The study also did not include healthy people as controls. Therefore, the results may not capture the impact of TB on patients alone. Finally, only quantitative analysis was conducted in this study, and data were collected through patient self-reports. Patients may hide certain facts, which may cause our results to be underestimated. Extensive interviews and qualitative analysis are needed for a more comprehensive assessment.
Conclusion
This study empirically explored the interrelationships among social support, experienced stigma, psychological distress, and QOL and tested whether experienced stigma and psychological distress played a mediating role. Using the SEM method, we found that (1) social support, experienced stigma and psychological distress affect the QOL of patients with TB; (2) experienced stigma mediates the relationship between social support and psychological distress; (3) psychological distress mediates the relationship between experienced stigma and QOL; and (4) experienced stigma and psychological distress are sequential mediators from social support to QOL. Understanding and managing the QOL of TB patients may lead to better outcomes, and the results of this study provide useful information to help TB patients achieve better QOL.
Acknowledgements
We are very grateful to the doctors at Dalian TB hospital and Zhuanghe and Lushun TB dispensaries for their support and assistance in carrying out this study. We would also like to thank the efforts of the data collectors and the valuable information provided by all study participants.
Author contributions
L.Z. and X.C. conceived and designed the research and advanced the whole research. X.C. analysed the data and drafted the manuscript. X.C., J.X., Y.C., R.W., H.J., Y.P., Y.D., M.S., L.D., M.G. and J.W. were involved in data collection, entry, and verification. All authors read and approved the final manuscript and agreed to take responsibility for all aspects of the work.
Data availability
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization . Global Tuberculosis Report 2020. WHO; 2020. [Google Scholar]
- 2.Dires A, Hagos T, Yitayal M, Amare G, Aschalew AY. Quality of life and associated factors among patients with tuberculosis at the University of Gondar comprehensive specialized hospital, Ethiopia. Qual. Life Res. 2021;30(4):1173–1181. doi: 10.1007/s11136-020-02717-w. [DOI] [PubMed] [Google Scholar]
- 3.Hershkovitz I, Donoghue HD, Minnikin DE, et al. Detection and molecular characterization of 9,000-year-old Mycobacterium tuberculosis from a Neolithic settlement in the Eastern Mediterranean. PLoS ONE. 2008;3(10):e3426. doi: 10.1371/journal.pone.0003426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Atif M, Sulaiman SA, Shafie AA, et al. Impact of tuberculosis treatment on health-related quality of life of pulmonary tuberculosis patients: A follow-up study. Health Qual. Life Outcomes. 2014;12:19. doi: 10.1186/1477-7525-12-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thomas BE, Shanmugam P, Malaisamy M, et al. Psycho-socio-economic issues challenging multidrug resistant tuberculosis patients: A systematic review. PLoS ONE. 2016;11(1):e0147397. doi: 10.1371/journal.pone.0147397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Juliasih NN, et al. Factors affecting tuberculosis patients' quality of life in Surabaya, Indonesia. J. Multidiscip. Healthcare. 2020;13:1475–1480. doi: 10.2147/JMDH.S274386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dar SA, Shah NN, Wani ZA, Nazir D. A prospective study on quality of life in patients with pulmonary tuberculosis at a tertiary care hospital in Kashmir, Northern India. Indian J. Tuberc. 2019;66(1):118–122. doi: 10.1016/j.ijtb.2018.07.002. [DOI] [PubMed] [Google Scholar]
- 8.Brown J, Capocci S, Smith C, Morris S, Abubakar I, Lipman M. Health status and quality of life in tuberculosis. Int. J. Infect. Dis. 2015;32:68–75. doi: 10.1016/j.ijid.2014.12.045. [DOI] [PubMed] [Google Scholar]
- 9.Gao XF, Rao Y. Quality of life of a migrant population with tuberculosis in West China. Int. J. Tuberc. Lung Dis. 2015;19(2):223–230. doi: 10.5588/ijtld.13.0866. [DOI] [PubMed] [Google Scholar]
- 10.Whoqol Group The World Health Organization quality of life assessment (WHOQOL): Position paper from the World Health Organization. Soc. Sci. Med. 1995;41(10):1403–1409. doi: 10.1016/0277-9536(95)00112-k. [DOI] [PubMed] [Google Scholar]
- 11.Sarafino EP, Smith TW. Health Psychology Biopsychosocial Interaction. Wiley; 2011. [Google Scholar]
- 12.Munro SA, Lewin SA, Smith HJ, Engel ME, Fretheim A, Volmink J. Patient adherence to tuberculosis treatment: A systematic review of qualitative research. PLoS Med. 2007;4(7):e238. doi: 10.1371/journal.pmed.0040238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kastien-Hilka T, Abulfathi A, Rosenkranz B, Bennett B, Schwenkglenks M, Sinanovic E. Health-related quality of life and its association with medication adherence in active pulmonary tuberculosis—A systematic review of global literature with focus on South Africa. Health Qual. Life Outcomes. 2016;14:42. doi: 10.1186/s12955-016-0442-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mohammed S, Nagla S, Morten S, Asma E, Arja A. Illness perceptions and quality of life among tuberculosis patients in Gezira, Sudan. Afr. Health Sci. 2015;15(2):385–393. doi: 10.4314/ahs.v15i2.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jaber AA, Khan AH, Syed Sulaiman SA, Ahmad N, Anaam MS. Evaluation of health-related quality of life among tuberculosis patients in two cities in yemen. PLoS ONE. 2016;11(6):e0156258. doi: 10.1371/journal.pone.0156258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Karyani AK, Rashidian A, Sefiddashti SE, Sari AA. Self-reported health-related quality of life (HRQoL) and factors affecting HRQoL among individuals with health insurance in Iran. Epidemiol. Health. 2016;38:e2016046. doi: 10.4178/epih.e2016046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Qiu L, Tong Y, Yang Q, Sun N, Gong Y, Yin X. Reliability and validity of a smart quality of life scale for patients with tuberculosis. J. Public Health. 2019;28:575. [Google Scholar]
- 18.Li H, Ji Y, Chen T. The roles of different sources of social support on emotional well-being among Chinese elderly. PLoS ONE. 2014;9(3):e90051. doi: 10.1371/journal.pone.0090051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alene KA, Clements ACA, McBryde ES, et al. Mental health disorders, social stressors, and health-related quality of life in patients with multidrug-resistant tuberculosis: A systematic review and meta-analysis. J. Infect. 2018;77(5):357–367. doi: 10.1016/j.jinf.2018.07.007. [DOI] [PubMed] [Google Scholar]
- 20.Zarova C, Chiwaridzo M, Tadyanemhandu C, Machando D, Dambi JM. The impact of social support on the health-related quality of life of adult patients with tuberculosis in Harare, Zimbabwe: A cross-sectional survey. BMC Res. Notes. 2018;11(1):795. doi: 10.1186/s13104-018-3904-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen X, Du L, Wu R, et al. Tuberculosis-related stigma and its determinants in Dalian, Northeast China: A cross-sectional study. BMC Public Health. 2021;21(1):6. doi: 10.1186/s12889-020-10055-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rajeswari R, Muniyandi M, Balasubramanian R, Narayanan PR. Perceptions of tuberculosis patients about their physical, mental and social well-being: A field report from south India. Soc. Sci. Med. 2005;60(8):1845–1853. doi: 10.1016/j.socscimed.2004.08.024. [DOI] [PubMed] [Google Scholar]
- 23.Tadesse S. Stigma against tuberculosis patients in Addis Ababa, Ethiopia. PLoS ONE. 2016;11(4):e0152900. doi: 10.1371/journal.pone.0152900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Qiu L, Yang Q, Tong Y, Lu Z, Gong Y, Yin X. The mediating effects of stigma on depressive symptoms in patients with tuberculosis: A structural equation modeling approach. Front. Psychiatry. 2018;9:618. doi: 10.3389/fpsyt.2018.00618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Masumoto S, Yamamoto T, Ohkado A, Yoshimatsu S, Querri AG, Kamiya Y. Prevalence and associated factors of depressive state among pulmonary tuberculosis patients in Manila, The Philippines. Int. J. Tuberc. Lung Dis. 2014;18(2):174–179. doi: 10.5588/ijtld.13.0335. [DOI] [PubMed] [Google Scholar]
- 26.Datiko DG, Jerene D, Suarez P. Stigma matters in ending tuberculosis: Nationwide survey of stigma in Ethiopia. BMC Public Health. 2020;20(1):190. doi: 10.1186/s12889-019-7915-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Abioye IA, Omotayo MO, Alakija W. Socio-demographic determinants of stigma among patients with pulmonary tuberculosis in Lagos, Nigeria. Afr. Health Sci. 2011;11(Suppl 1):S100–S104. doi: 10.4314/ahs.v11i3.70078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dodor EA, Neal K, Kelly S. An exploration of the causes of tuberculosis stigma in an urban district in Ghana. Int. J. Tuberc. Lung Dis. 2008;12(9):1048–1054. [PubMed] [Google Scholar]
- 29.Moya EM, Biswas A, Chávez Baray SM, Martínez O, Lomeli B. Assessment of stigma associated with tuberculosis in Mexico. Public Health Action. 2014;4(4):226–232. doi: 10.5588/pha.14.0065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ayana TM, Roba KT, Mabalhin MO. Prevalence of psychological distress and associated factors among adult tuberculosis patients attending public health institutions in Dire Dawa and Harar cities, Eastern Ethiopia. BMC Public Health. 2019;1:1–9. doi: 10.1186/s12889-019-7684-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Xu M, Markstrom U, Lyu J, Xu L. Survey on tuberculosis patients in rural areas in China: Tracing the role of stigma in psychological distress. Int. J. Environ. Res. Public Health. 2017;14(10):1171. doi: 10.3390/ijerph14101171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Molla A, Mekuriaw B, Kerebih H. Depression and associated factors among patients with tuberculosis in Ethiopia: A cross-sectional study. Neuropsychiatr. Dis. Treat. 2019;15:1887–1893. doi: 10.2147/NDT.S208361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Duko B, Gebeyehu A, Ayano G. Prevalence and correlates of depression and anxiety among patients with tuberculosis at WolaitaSodo University Hospital and Sodo Health Center, WolaitaSodo, South Ethiopia, cross sectional study. BMC Psychiatry. 2015;15:214. doi: 10.1186/s12888-015-0598-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kastien-Hilka T, Rosenkranz B, Sinanovic E, Bennett B, Schwenkglenks M. Health-related quality of life in South African patients with pulmonary tuberculosis. PLoS ONE. 2017;12(4):e0174605. doi: 10.1371/journal.pone.0174605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Coker A, Kuyinu Y, Mohammed A. Psychological distress and psychiatric symptoms among patients receiving treatment for tuberculosis in a teaching hospital in Lagos, Nigeria. J. Community Med. Primary Health Care. 2011;1–2:25–40. [Google Scholar]
- 36.Peltzer K, Naidoo P, Matseke G, Louw J, McHunu G, Tutshana B. Prevalence of psychological distress and associated factors in tuberculosis patients in public primary care clinics in South Africa. BMC Psychiatry. 2012;12:89. doi: 10.1186/1471-244X-12-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Katon WJ. Epidemiology and treatment of depression in patients with chronic medical illness. Dialogues Clin. Neurosci. 2011;13(1):7–23. doi: 10.31887/DCNS.2011.13.1/wkaton. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Duko B, Dana LM, Ayano G. Psychological distress among TB patients in sub-Saharan Africa. Int. J. Tuberc. Lung Dis. 2020;24(11):1200–1204. doi: 10.5588/ijtld.20.0158. [DOI] [PubMed] [Google Scholar]
- 39.Ambaw F, Mayston R, Hanlon C, Medhin G, Alem A. Untreated depression and tuberculosis treatment outcomes, quality of life and disability, Ethiopia. Bull. World Health Organ. 2018;96(4):243–255. doi: 10.2471/BLT.17.192658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nusair K, Hua N. Comparative assessment of structural equation modeling and multiple regression research methodologies: E-commerce context. Tour. Manage. 2010;3:314–324. [Google Scholar]
- 41.Mota-Veloso I, Celeste RK, Fonseca CP, et al. Effects of attention deficit hyperactivity disorder signs and socio-economic status on sleep bruxism and tooth wear among schoolchildren: Structural equation modelling approach. Int. J. Pediatr. Dent. 2017;27(6):523–531. doi: 10.1111/ipd.12291. [DOI] [PubMed] [Google Scholar]
- 42.Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. Guilford Press; 2018. [Google Scholar]
- 43.Brunner J, Austin PC. Inflation of type I error rate in multiple regression when independent variables are measured with error. Can. J. Stat. 2009;37:33–46. [Google Scholar]
- 44.Dalgard OS, Dowrick C, Lehtinen V, et al. Negative life events, social support and gender difference in depression: A multinational community survey with data from the ODIN study. Soc. Psychiatry Psychiatr. Epidemiol. 2006;41(6):444–451. doi: 10.1007/s00127-006-0051-5. [DOI] [PubMed] [Google Scholar]
- 45.Xu M, Markström U, Lyu J, Xu L. Survey on tuberculosis patients in rural areas in China: Tracing the role of stigma in psychological distress. Int. J. Environ. Res. Public Health. 2017;14(10):1171. doi: 10.3390/ijerph14101171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol. Med. 2002;32(6):959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- 47.Brooks RT, Beard J, Steel Z. Factor structure and interpretation of the K10. Psychol. Assess. 2006;18(1):62–70. doi: 10.1037/1040-3590.18.1.62. [DOI] [PubMed] [Google Scholar]
- 48.Hörnquist JO. Quality of life: Concept and assessment. Scand. J. Soc. Med. 1990;18(1):69–79. doi: 10.1177/140349489001800111. [DOI] [PubMed] [Google Scholar]
- 49.Phillips MR, Yang G, Zhang Y, Wang L, Ji H, Zhou M. Risk factors for suicide in China: A national case-control psychological autopsy study. Lancet (London, England) 2002;360(9347):1728–1736. doi: 10.1016/S0140-6736(02)11681-3. [DOI] [PubMed] [Google Scholar]
- 50.Qiu L, Tong Y, Lu Z, Gong Y, Yin X. Depressive symptoms mediate the associations of stigma with medication adherence and quality of life in tuberculosis patients in China. Am. J. Trop. Med. Hyg. 2019;100(1):31–36. doi: 10.4269/ajtmh.18-0324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yang C, Nay S, Hoyle RH. Three approaches to using lengthy ordinal scales in structural equation models: Parceling, latent scoring, and shortening scales. Appl. Psychol. Meas. 2010;34(2):122–142. doi: 10.1177/0146621609338592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav. Res. Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 53.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Mdeling. 1999;6:1–55. [Google Scholar]
- 54.Segars AH. Assessing the unidimensionality of measurement: A paradigm and illustration within the context of information systems research. Omega Int. J. Manage. Sci. 1997;1:107–121. [Google Scholar]
- 55.Fornell CUM, Larcker DF. Evaluating structural equation models with unobservable variables and measurement error. J. Mark. Res. 1981;1:39–50. [Google Scholar]
- 56.Jackson DL, Gillaspy JA, Purc-Stephenson R. Reporting practices in confirmatory factor analysis: An overview and some recommendations. Psychol. Methods. 2009;14(1):6–23. doi: 10.1037/a0014694. [DOI] [PubMed] [Google Scholar]
- 57.Howley MM, Rouse CD, Katz DJ, Colson PW, Hirsch-Moverman Y, Royce RA. Knowledge and attitudes about tuberculosis among U.S.-Born Blacks and Whites with tuberculosis. J. Immigr. Minority Health. 2015;17(5):1487–1495. doi: 10.1007/s10903-014-0105-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Buregyeya E, Kasasa S, Mitchell EM. Tuberculosis infection control knowledge and attitudes among health workers in Uganda: A cross-sectional study. BMC Infect. Dis. 2016;16(1):416. doi: 10.1186/s12879-016-1740-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Li X, Huang L, Wang H, Fennie KP, He G, Williams AB. Stigma mediates the relationship between self-efficacy, medication adherence, and quality of life among people living with HIV/AIDS in China. AIDS Patient Care STDS. 2011;25(11):665–671. doi: 10.1089/apc.2011.0174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Park S, George M, Choi JY. Quality of life in Korean tuberculosis patients: A longitudinal study. Public Health Nurs. 2020;37(2):198–205. doi: 10.1111/phn.12691. [DOI] [PubMed] [Google Scholar]
- 61.Farmer JE, Clark MJ, Sherman AK. Rural versus urban social support seeking as a moderating variable in traumatic brain injury outcome. J. Head Trauma Rehabil. 2003;18(2):116–127. doi: 10.1097/00001199-200303000-00003. [DOI] [PubMed] [Google Scholar]
- 62.Link BG, Phelan JC. Stigma and its public health implications. Lancet (London, England) 2006;367(9509):528–529. doi: 10.1016/S0140-6736(06)68184-1. [DOI] [PubMed] [Google Scholar]
- 63.Guo N, Marra F, Marra CA. Measuring health-related quality of life in tuberculosis: A systematic review. Health Qual. Life Outcomes. 2009;7:14. doi: 10.1186/1477-7525-7-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Tola HH, Karimi M, Yekaninejad MS. Effects of sociodemographic characteristics and patients' health beliefs on tuberculosis treatment adherence in Ethiopia: A structural equation modelling approach. Infect. Dis. Poverty. 2017;6(1):167. doi: 10.1186/s40249-017-0380-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.de Vries SG, Cremers AL, Heuvelings CC, et al. Barriers and facilitators to the uptake of tuberculosis diagnostic and treatment services by hard-to-reach populations in countries of low and medium tuberculosis incidence: A systematic review of qualitative literature. Lancet Infect. Dis. 2017;17(5):e128–e143. doi: 10.1016/S1473-3099(16)30531-X. [DOI] [PubMed] [Google Scholar]
- 66.Arcêncio RA, de Almeida CJ, Touso MM, et al. Preliminary validation of an instrument to assess social support and tuberculosis stigma in patients' families. Public Health Action. 2014;4(3):195–200. doi: 10.5588/pha.13.0095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Li CT, Chu KH, Reiher B, Kienene T, Chien LY. Evaluation of health-related quality of life in patients with tuberculosis who completed treatment in Kiribati. J. Int. Med. Res. 2017;45(2):610–620. doi: 10.1177/0300060517694491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hafeman DM, Schwartz S. Opening the Black Box: A motivation for the assessment of mediation. Int. J. Epidemiol. 2009;38(3):838–845. doi: 10.1093/ije/dyn372. [DOI] [PubMed] [Google Scholar]
- 69.Lee LT, Chen CJ, Suo J, Chen SC, Chen CY, Lin RS. Family factors affecting the outcome of tuberculosis treatment in Taiwan. J. Formos. Med. Assoc. 1993;92(12):1049–1056. [PubMed] [Google Scholar]
- 70.Theron G, Peter J, Zijenah L, et al. Psychological distress and its relationship with non-adherence to TB treatment: A multicentre study. BMC Infect. Dis. 2015;15:253. doi: 10.1186/s12879-015-0964-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Du L, Xu J, Chen X, et al. Rebuild doctor-patient trust in medical service delivery in China. Sci. Rep. 2020;10(1):21956. doi: 10.1038/s41598-020-78921-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Demissie M, Getahun H, Lindtjørn B. Community tuberculosis care through "TB clubs" in rural North Ethiopia. Soc. Sci. Med. 2003;56(10):2009–2018. doi: 10.1016/s0277-9536(02)00182-x. [DOI] [PubMed] [Google Scholar]
- 73.Duko B, Bedaso A, Ayano G, Yohannis Z. Perceived stigma and associated factors among patient with tuberculosis, Wolaita Sodo, Ethiopia: Cross-sectional study. Tuberc. Res. Treat. 2019;2019:5917537. doi: 10.1155/2019/5917537. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.