Abstract
Objective:
Previous research suggests that people with asthma may experience a worsening of symptoms following hurricanes due to changes in environmental exposures, discontinuity in chronic disease management, and stress. The objective of this study was to estimate changes in asthma-related emergency department (ED) visits in North Carolina following Hurricane Irene, which made landfall in August 2011.
Methods:
Changes in asthma-related ED visits in September–December of 2010 and 2011 were examined using data from the Healthcare Cost and Utilization Project State Emergency Department and Inpatient Databases. A Poisson generalized linear model was used to estimate the association between FEMA disaster declarations following Hurricane Irene and county-level asthma-related ED visits controlling for month, year, and county.
Results:
Following Hurricane Irene, disaster declarations were made for 38 of 100 counties in North Carolina. In September 2010, the rate of asthma-related ED visits for North Carolina was 6 per 10,000 person months. In September 2011, rates of asthma-related ED visits were similar in counties with and without disaster declarations (7 and 5 per 10,000 person months, respectively). When adjusting for covariates, there was little or no difference in the rate of asthma ED visits before and after the hurricane between counties with and without a disaster declaration (RR[95%CI]=1.02[0.97, 1.08]).
Conclusions:
Although risk factors for asthma exacerbations increase following hurricanes, these results found little evidence of an increase in asthma-related ED visits in North Carolina following Hurricane Irene.
INTRODUCTION
Extreme weather events, such as hurricanes and tropical storms, can have wide-ranging impacts on human health. While hurricane preparedness planning usually focuses on preparing healthcare systems to care for people with communicable disease and injury, people with chronic diseases can also experience changes in their health following a hurricane. One of the most common chronic diseases in the United States is asthma, affecting more than 25 million Americans [1]. When asthma is not well controlled it can lead to emergency department (ED) visits, hospitalizations, and missed school and work days.
Following large hurricanes in the United States, asthma exacerbations have been observed as a result of increases in environmental triggers like mold, discontinuity in chronic disease care, and increases in stress and anxiety [2]. These asthma exacerbations have been documented using emergency department data. For example, previous studies have observed an increase in asthma ED visits following Hurricanes Maria and Irma in the U.S. Virgin Islands and Hurricane Sandy in New Jersey [3, 4].
Hurricane Irene hit the coast of North Carolina as a category 3 hurricane on August 27, 2011. It caused power outages for more than 660,000 North Carolina residents and $686 million in damages across the state [5]. Although mold in homes, an asthma trigger, was reported after Hurricane Irene [6], there has been no examination of whether asthma visits increased following this hurricane. This study sought to identify if there were changes in ED visits for asthma in the months following Hurricane Irene in affected counties in North Carolina.
METHODS
HEALTHCARE COST AND UTILIZATION PROJECT (HCUP) DATA
The number of asthma-related ED visits in North Carolina was summarized by county from the Healthcare Cost and Utilization Project (HCUP) State Emergency Department Database (SEDD) and State Inpatient Database (SID) for years 2010 and 2011. HCUP SEDD captures discharge data on all ED visits that do not result in an inpatient stay and HCUP SID captures all inpatient hospital stays, including those that started in the emergency department [7]. Combined, the SEDD and SID databases capture more than 97% of all ED visits in the state of North Carolina. For this analysis, SEDD data was combined with SID data that started in the emergency department.
ASTHMA EMERGENCY DEPARTMENT VISITS
ED visits from SEDD were included in this analysis if the primary diagnosis was for asthma (ICD-9 493.XX). ED visits from SID were included if the patient had an inpatient stay with a primary diagnosis for asthma after being admitted to the emergency department. County of the patient’s residence and county of the hospital visited were available for all visits. Patient’s billing address, rather than the hospital location, was used to determine exposure in order to account for hospital closures and post-hurricane relocation.
HURRICANE IRENE EXPOSURE MEASURES
Counties were separated into two categories: (1) those that were affected by Hurricane Irene and (2) those that were not. Hurricane-affected counties were identified based on Federal Emergency Management Agency (FEMA) disaster declarations for Hurricane Irene [8]. Major disaster declarations can be declared for all types of disasters and are primarily used to allocate individual and public assistance. Disaster declarations are made if the disaster’s impact is larger than what the state and local government is able to handle without federal assistance. For this analysis, FEMA disaster declarations (declared vs. not declared) were used to create a dichotomous disaster declaration variable to define exposure to hurricane damage in a zip code. A sensitivity analysis was conducted using an alternative exposure metric of rainfall levels immediately following Hurricane Irene [9]. For this sensitivity analysis, counties in North Carolina were categorized based on rainfall level as ≤2 inches of rain, 2–7 inches of rain, and >7 inches of rain.
ANALYSIS
Asthma visits for all 100 counties in North Carolina were aggregated by month for September through December in the years 2010 and 2011. All counties were considered to be not disaster-affected in 2010. For all months in 2011, counties with a FEMA disaster declaration were considered disaster-affected and counties without a FEMA disaster declaration were considered not disaster-affected. Although the hurricane occurred in August 2011, for counties that received a FEMA disaster declaration following Hurricane Irene, all months for 2011 were considered disaster-affected due to the long-term environmental effects of hurricanes. Similarly, for the sensitivity analysis, the reference group was composed of asthma counts for all counties in 2010 and counts for counties in 2011 that had ≤2 inches of rain following Hurricane Irene.
A difference of differences analysis was conducted on a log scale using a Poisson generalized linear model to estimate the impact of Hurricane Irene on asthma ED visits. The model controlled for county, month, and year and accounted for correlation between monthly-county rates within the same year using an autoregressive-1 correlation structure. Analyses were conducted in SAS 9.4 (SAS Institute, Cary, North Carolina).
RESULTS
There were 39,688 visits for asthma captured by HCUP in North Carolina for the 8 months in this analysis (September–December, 2010–2011) (Table 1). The month with the most visits was September 2010 with 5,591 visits and the month with the least visits was December 2010 with 4,002 visits. Overall, there was no meaningful difference in the number of asthma ED visits between fall 2010 and fall 2011 with the 4 months in each year having 19,846 and 19,842 visits respectively.
Table 1:
Asthma ED Visit Rates by FEMA Disaster Declaration in North Carolina, September–December, 2010–2011
| Rate of asthma ED visits within disaster declared counties | Rate of asthma ED visits within non-disaster declared counties | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Month | Year | Cases | Population | Rate per 10,000 person-months | Month | Year | Cases | Population | Rate per 10,000 person- months |
| September | 2010 | 1,652 | 2,161,881 | 7.64 | September | 2010 | 3,939 | 7,398,353 | 5.32 |
| October | 2010 | 1,580 | 2,161,881 | 7.31 | October | 2010 | 3,767 | 7,398,353 | 5.09 |
| November | 2010 | 1,459 | 2,161,881 | 6.75 | November | 2010 | 3,447 | 7,398,353 | 4.66 |
| December | 2010 | 1,192 | 2,161,881 | 5.51 | December | 2010 | 2,810 | 7,398,353 | 3.80 |
| September | 2011 | 1,450 | 2,174,552 | 6.67 | September | 2011 | 3,451 | 7,481,849 | 4.61 |
| October | 2011 | 1,500 | 2,174,552 | 6.90 | October | 2011 | 3,543 | 7,481,849 | 4.74 |
| November | 2011 | 1,551 | 2,174,552 | 7.13 | November | 2011 | 3,496 | 7,481,849 | 4.67 |
| December | 2011 | 1,445 | 2,174,552 | 6.65 | December | 2011 | 3,406 | 7,481,849 | 4.55 |
The age of patients who visited the emergency department for asthma in North Carolina during these months ranged from under one year old to 101 years old; 44% of visits were for patients aged 18 years or younger. Examining the sex of patients, 53% of asthma-related ED visits were by women. Examining the race and ethnicity of patients, 54% of asthma ED visits were by Non-Hispanic Black patients, 37% by non-Hispanic White patients, 3% by Hispanic or Latino patients, and the remaining 6% by patients of other racial and ethnic groups. Describing ED visit payment methods, 11% of patient visits were covered by Medicare, 42% by Medicaid, 22% by private insurance, and 22% were self-paid.
Following Hurricane Irene, 38 of 100 counties in North Carolina had disaster declarations, mostly along the eastern coast and counties adjacent to the coastal counties (Figure 1). Examining asthma-related ED visit rates across all counties in North Carolina, in September 2010 the asthma-related ED visit rate was 6 per 10,000 person months. This is compared with September 2011, following Hurricane Irene, when rates of asthma-related ED visits were similar in counties with and without disaster declarations (7 per 10,000 person months and 5 per 10,000 person months, respectively) (Table 1). In difference of differences analyses, rates of asthma ED visits counties affected differed little, if at all, from rates in counties not affected by the hurricane (rate ratio [95% confidence interval]=1.02 [0.97, 1.08]) when adjusting for county, month, and year and accounting for correlation between monthly-county rates within the same year. In sensitivity analyses using rainfall levels instead of disaster declaration as the exposure metric, there was little or no difference in the rate of asthma ED visits between counties that experienced >7 inches of rain and 2–7 inches of rain compared to those that had ≤2 inches of rain following Hurricane Irene (RR [95% CI]=0.93 [0.85, 1.02] and 1.01 [0.95, 1.09] respectively) when controlling for the same factors as in the primary model.
Figure 1:
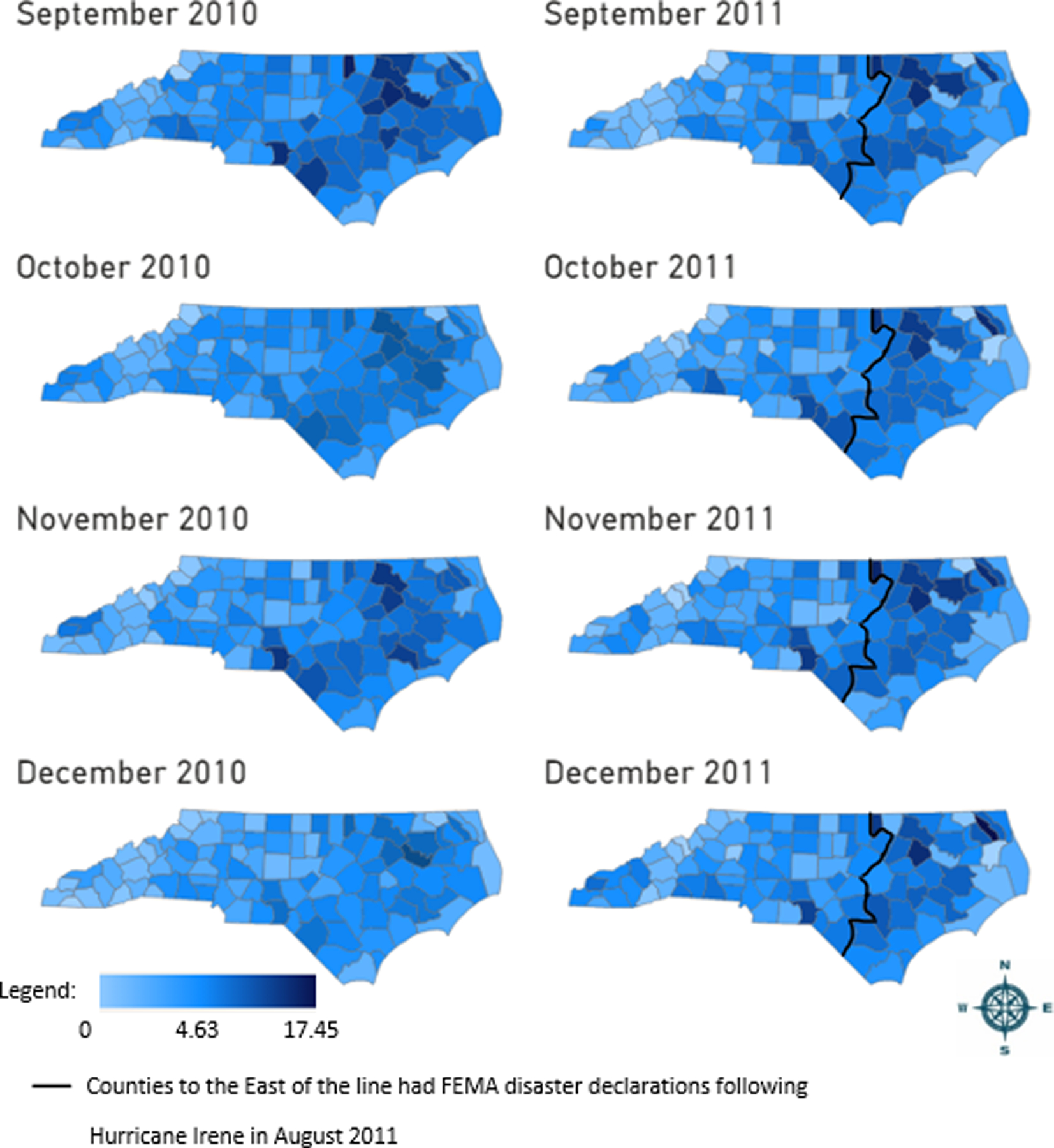
Rate of asthma ED visits by county in North Carolina, September–December, 2010–2011
DISCUSSION
In this study, we examined changes in county-level ED visits for asthma in North Carolina following Hurricane Irene. Although asthma triggers introduced following hurricanes can increase asthma exacerbations, we observed little evidence of a change in asthma ED visits following Hurricane Irene. There are several potential explanations for these results. It is possible that aggregating visits by county masked a true association between hurricane-related exposures and asthma exacerbations. A more granular level of exposure, for example an individual-level estimate of home flooding or displacement, may have been better suited to identify potential impacts of Hurricane Irene on patients with asthma. Alternatively, it is possible that there was no impact of Hurricane Irene on asthma in North Carolina. Another study found an impact from hurricanes on people with asthma examined the effects of Hurricane Katrina [2]. Hurricane Katrina was a category 5 hurricane when it made landfall and had a higher economic and infrastructural impact on the New Orleans community than Hurricane Irene had on North Carolina. It is possible that hurricane Katrina, a larger magnitude storm with those greater impacts, had more effects on patients with asthma. Additionally, there may have been more knowledge of how to control asthma following a storm among the people impacted by Hurricane Irene than those living in New Orleans during Hurricane Katrina.
A strength of this study was the use of HCUP data which captured >97% of ED visits in North Carolina for the months included in this analysis. Another strength of this study is the use of FEMA disaster declarations as a proxy for hurricane impact. Using FEMA disaster declarations helped capture all effects of Hurricane Irene such as flooding, home damage, hospital closures and disruptions in day-to-day life, each of which may lead to asthma exacerbations. Moreover, the comparison of asthma ED visits between fall of 2010 and fall of 2011 helped control for the seasonal trends in asthma exacerbations associated with allergy and flu seasons as well as children returning to school [10].
A limitation of this study was that no information was available on whether individuals relocated following Hurricane Irene. Using billing zip code to determine whether an individual resided in a county affected by the hurricane may have resulted in misclassification of people who had moved, but had not updated their mailing address, or those working or vacationing in a different area at the time of the hurricane. Furthermore, the North Carolina HCUP dataset only captures ED visits in North Carolina and not ED visits North Carolina residents may have made outside of the state after Hurricane Irene. Because this study used county-level FEMA disaster declarations to determine hurricane exposure, no individual-level information on flooding or home damage was captured. Within each county, there may have been substantial variation in individual-level exposure to post-hurricane asthma triggers such as mold which would not have been captured by this county-level exposure metric.
This study adds to our understanding of the impact of hurricanes on patients with asthma by quantifying the impact of Hurricane Irene on asthma ED visits in North Carolina. Further research could be helpful in identifying the impact of hurricanes on people with asthma. For example, studies that follow individuals with asthma after a hurricane could provide more robust measures of post-hurricane exposures and capture a wider range of the impact of hurricanes on asthma. Changes in asthma control, medication usage, and symptoms may all be impacted by post-hurricane exposures and are not fully captured by ED data. A better understanding of the impact of hurricanes of all magnitudes on people with asthma would help public health agencies prepare patients and healthcare providers for asthma-specific needs following hurricanes.
ACKNOWLEDGEMENTS
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
REFERENCES
- 1.Centers for Disease Control and Prevention. FastStats: Asthma. 2017. [cited 2020; Available from: https://www.cdc.gov/nchs/fastats/asthma.htm.
- 2.Rath B, et al. , Adverse respiratory symptoms and environmental exposures among children and adolescents following Hurricane Katrina. Public health reports (Washington, D.C. : 1974), 2011. 126(6): p. 853–860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chowdhury MAB, et al. , Health Impact of Hurricanes Irma and Maria on St Thomas and St John, US Virgin Islands, 2017–2018. American Journal of Public Health, 2019. 109(12): p. 1725–1732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tsai S, et al. , Development and Application of Syndromic Surveillance for Severe Weather Events Following Hurricane Sandy. Disaster Medicine and Public Health Preparedness, 2016. 10(3): p. 463–471. [DOI] [PubMed] [Google Scholar]
- 5.North Carolina Department of Public Safety. Hurricane Irene 2011. 2012; Available from: https://www.ncdps.gov/emergency-management/recent-disasters/hurricane-irene-2011.
- 6.Federal Emergency Management Agency (FEMA). Be Safe, Don’t Stay in a Home Infested with Mold or Mildew. 2011. [cited 2020; Available from: https://www.fema.gov/news-release/2011/09/18/be-safe-dont-stay-home-infested-mold-or-mildew.
- 7.Healthcare Cost and Utilization Project (HCUP). SID Database Documentation. 2019. [cited 2019; Available from: https://www.hcup-us.ahrq.gov/db/state/siddbdocumentation.jsp.
- 8.Federal Emergency Management Agency. North Carolina Hurricane Irene (DR-4019). 2011. [cited 2019; Available from: https://www.fema.gov/disaster/4019.
- 9.National Weather Service. Hurricane Irene Aug 27, 2011. 2011. [cited 2020; Available from: https://www.weather.gov/ilm/HurricaneIreneAug272011.
- 10.Eggo RM, et al. , Respiratory virus transmission dynamics determine timing of asthma exacerbation peaks: Evidence from a population-level model. Proceedings of the National Academy of Sciences of the United States of America, 2016. 113(8): p. 2194–2199. [DOI] [PMC free article] [PubMed] [Google Scholar]


