Abstract
Background and purpose
The growth and development of the acetabulum in children with developmental dysplasia of hip (DDH) depends upon the extent of concentric reduction. Children in walking age often need open reduction with or without additional osteotomies to obtain congruous, stable reduction. The purpose of this study was to evaluate acetabular development in late diagnosed DDH treated by open reduction with or without femoral osteotomy.
Methods
This is a retrospective study of 29 children (40 hips) with idiopathic DDH, previously untreated managed by open reduction with or without femoral osteotomy. We analyzed preoperative and yearly postoperative radiographs up to 6 years of age for acetabular development by measuring acetabular index. Acetabular remodeling was assessed with a graphical plot of serial mean acetabular index. Those with AI < 30° at outcome measure point of 6 years of patient age were considered to have satisfactory acetabular remodeling.
Results
Mean age of surgery was 26.8 months. Open reduction alone was done in 14 hips and open reduction with concurrent femoral osteotomy done in 26 hips. The mean acetabular index pre operatively was 36.6° ± 5.9° which reduced to 29.7° ± 6° at 1-year follow-up and to 26.6° ± 5.9° at 2-year follow-up. 28 out of 40 hips were available for evaluation at outcome measure point of 6 years of age, which showed satisfactory remodeling in 24 hips with mean AI of 22.7° ± 5.7°. Maximum acetabular development was seen at 2 years post-surgery and better remodeling was seen in children operated at less than 2 years of age. 5 hips had changes of avascular necrosis of femoral head. There was no incidence of redislocation/subluxation at latest follow-up.
Conclusion
Open reduction in late-diagnosed developmental dysplasia of hip has potential for favourable acetabular development. Femoral osteotomy when required along with open reduction may suffice to address acetabular dysplasia found in the initial years of management of DDH.
Keywords: Developmental dysplasia hip, Acetabular development, Open reduction, Femur osteotomy, Walking age children
Introduction
The treatment goal in developmental dysplasia of hip is to obtain stable congruous reduction either by closed or open methods to promote normal hip development [1]. Many authors have reported that concentric reduction is the main factor affecting the acetabular development, and all acetabulae with DDH may develop satisfactorily if concentric reduction is obtained [2–5]. Failure to sufficiently remodel results in residual acetabular dysplasia which may need additional surgeries [6]. Majority of the earlier reports which have studied acetabular remodeling in older children involved open reduction alone [4, 7, 8]. Children in walking age often needs open reduction along with concomitant osteotomies of femur or pelvis to obtain stable, concentric reduction [9]. Also, there is lack of similar studies evaluating pattern of acetabular development in Indian children. The purpose of this study was to evaluate acetabular development following open reduction alone or open reduction with femoral side osteotomy for DDH in Indian children after walking age.
Materials and Methods
After obtaining institutional review board approval, medical records of children in walking age who had undergone DDH treatment at our institution between 2010 and 2019 were reviewed. Children in walking age (generally 12 months and beyond) with late diagnosed DDH with no prior intervention and who needed open reduction alone or open reduction with femoral side osteotomy were included in the study. Children who required acetabular procedures for stability of reduction at primary surgery were excluded from the study. Anteroposterior (AP) radiographs of pelvis with both hips of these children during preoperative and postoperative period were accessed. We measured acetabular index (AI) using lateral edge method as described by Hilgenreiner [10] and Tonnis [11] on preoperative radiographs and on yearly postoperative radiographs up to 6 years of age to assess pattern of acetabular remodeling. We selected acetabular index to monitor development as it is considered as one of the best predictor of late residual dysplasia up to age of 8 years [12]. Age of 6 years was selected as an outcome measuring point as the potential for acetabular remodeling diminishes after this age [8]. AI < 30° at 6 years of age was considered as satisfactory acetabular development [4, 7, 13]. Statistical analysis was performed using paired t test for comparisons within the same group and independent t test for comparisons between the two groups.
There were total of 40 hips (29 children with 18 unilateral and 11 bilateral DDH) who had undergone open reduction with or without femoral osteotomy during the study period. 21 were females and 8 were males. Mean age at surgery was 26.8 months ± 13.7 (range 10–62). Open reduction with varus derotation osteotomy of femur (VDRO) was done on 26 hips (65%) and 14 hips (35%) had undergone open reduction alone. All of these children had minimum follow-up of 2 years, 36 hips (90%) with 3-year follow-up and 28 hips (70%) were available for evaluation at outcome measure point of 6 years of age. The mean follow-up in our series was 64.6 months (range 24–96).
All open reductions were performed by a single surgeon using Smith Peterson approach. After opening the joint capsule, hypertrophied ligamentum teres, redundant capsule and fibro fatty tissue were excised. Joint was reduced and checked for stability. The decision to include additional osteotomy was based on the parameters described by Zadeh et al. [9]. Varus derotation femur osteotomy was done to those hips which needed abduction beyond 30° and internal rotation beyond neutral position for stable reduction. None of these cases required flexion beyond 30° for stability to warrant pelvic osteotomy. We regularly injected 1 ml of radio-opaque dye into the joint following reduction and capsulorrhaphy and confirmed the extent of cartilaginous acetabulum (Fig. 1). As we observed sufficient cartilaginous acetabulum providing adequate stability and cover to femoral head even in cases with high preoperative acetabular index, we did not add pelvic osteotomy routinely. For those hips which required pelvic osteotomy for stability, the senior author’s preference was Dega/Pemberton osteotomy. However, these cases have not been included in the present study as we intended to evaluate acetabular remodeling without pelvic procedures. Femoral osteotomy was fixed using 3.5 mm dynamic compression plate (DCP). Joint was transfixed with k wire in all cases and hip spica cast was given. K wire was removed at 1-month follow-up at out-patient clinic by making a window in the hip spica and spica cast was continued for another 1 month. Following removal of hip spica, hip abduction brace and physiotherapy was advised for 1–2 months. DCP plate was removed routinely after 1-year post-surgery.
Fig. 1.
a Anteroposterior radiograph of a 30 months old girl showing right DDH. b Intraoperative C-arm image following dye injection into the joint showing well developed cartilaginous acetabulum (white arrow). c C-arm image confirming well reduced joint with k wire transfixation and varus derotation femur osteotomy
Results
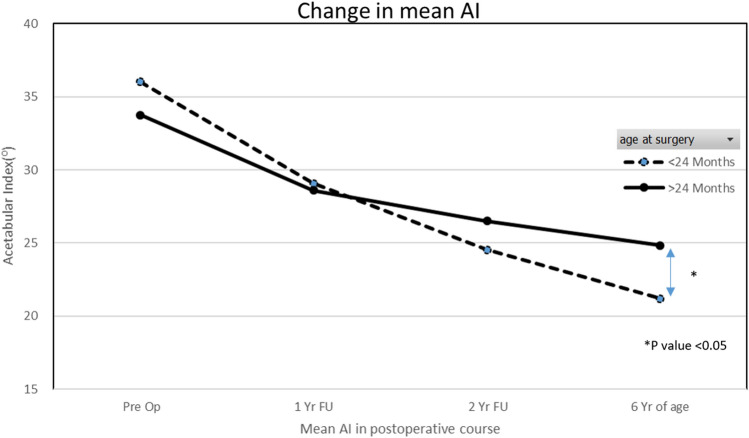
Preoperative evaluation revealed 2 hips with International Hip Dysplasia Institute (IDHI) grade 2, 13 hips with grade 3 and 25 hips with grade 4 dislocation. The mean acetabular index pre operatively was 36.6° ± 5.9° which reduced to 29.7° ± 6° at 1-year follow-up and further to 26.6° ± 5.9° at 2-year follow-up (Fig. 2). The acetabular index improved to 23.8° ± 4.9° at 3-year follow-up available for 36 hips. The mean AI at outcome measure point of 6 years of age was 22.7° ± 5.7°. This accounted for overall reduction of 38% in AI. Only 28 out of 40 hips (70%) were available for evaluation at 6 years of age. Satisfactory acetabular remodeling (AI < 30°) was found in 24 out of these 28 hips (85%) (Fig. 3). 4 hips found to have unsatisfactory acetabular remodeling and these children were offered secondary surgeries to address residual dysplasia but their parents decided to wait further. (Fig. 4). Out of 12 hips that were lost to follow-up and could not be included for outcome measurement, 5 hips showed AI < 30° at completion of 2-year follow-up.
Fig. 2.
The mean AI preoperatively was 36.6° which changed to 29.7° at 1 year, 26.6° at 2 years following surgery. It further reduced to 22.7° when patient attained 6 years of age. There was 38% reduction in mean AI at 6 years of age
Fig. 3.
a Anteroposterior (AP) radiograph of a 20 months (m) old girl showing right DDH. b Radiograph taken at 6 months following open reduction showing well reduced hip. c, d Radiographs at 12 months and 26 months follow-up showing progressive acetabular development with downward slope. e Radiograph at 6 years of age showing good acetabular remodeling. f Further remodeling noted in the AP radiograph at 9 years of age
Fig. 4.
a Anteroposterior radiograph of a 24 months (m) old boy showing left DDH. b child was treated with open reduction and varus derotation osteotomy. 6 m follow-up radiograph showing reduced hip with increased medial joint space with healed osteotomy site. c 26 m follow-up radiograph showing upward slope of acetabular roof. d Poor acetabular remodeling noted at 6 years age radiograph with persistent increased medial joint space
Age at surgery was ≤ 24 months for 26 hips. Of these, 11 hips had open reduction alone and 15 hips had additional femoral osteotomy. There was 41% reduction of AI at 6 years of age in these children. 14 hips had their surgery after 24 months of age with majority of them (11/14 hips) needing open reduction and femur osteotomy for better stability. AI reduced by 27% in them (Fig. 5). This difference in change of AI between two age groups was statistically significant as found by Student’s t test (p value 0.0004). Maximum remodeling was seen in first two years following surgery in both the age groups (Fig. 6). At the latest follow-up, 5 hips had changes of avascular necrosis (Fig. 7). Out of these, 4 hips of OR with femoral osteotomy had AVN compared 1 hip that underwent OR alone. 7 hips had coxa magna changes with femoral head size ≥ 20% of the opposite side. The incidence of coxa magna was found to be more in OR with femur osteotomy (5 hips) compared to OR alone (2 hips). There were no incidence of re-dislocation/subluxation in any of the treated children.
Fig. 5.
Comparison of change in mean AI between two age groups at the time of surgery (group A ≤ 24 months, group B > 24 months). The AI was 36° pre operatively which changed to 21.2° at 6 years with 41% reduction in group A children. The AI changed by 26% from 33.7° to 24.8° in group B children. These difference in changes was statistically significant with better remodeling observed in children aged ≤ 24 m at the time of surgery
Fig. 6.
Graphical representation of yearly acetabular index trend in patients with long follow-up (P1—patient no.1 with age at surgery 12 months, P2—patient no. 2 at 13 m, P3—patient no.3 at 23 m, P4—patient no.4 with age at surgery 46 m). Change in AI was maximum in first 2 years following surgery
Fig. 7.
a Anteroposterior radiograph of a 18 months (m) old boy with left DDH. b Radiograph at 7 m following open reduction. c 2-year follow-up radiograph showing changes of avascular necrosis in the femoral ossific nucleus. d, e Follow-up radiographs showing flat broad femoral head, short neck with progressive acetabular remodeling. f Further acetabular remodeling with coxa breva noted at 10 years of age
Discussion
The treatment of DDH in children after walking age demands open reduction to address contracted soft tissues, high displacement of femoral head with increased anteversion and dysplastic acetabulum [14, 15]. Following concentric and stable reduction of the joint, acetabulum continues to grow and remodel over several years, the upper limit of which is still debatable [16–19]. Previous studies which have analysed the remodeling pattern of acetabulum following open reduction recommended that maximum development of acetabulum was seen during first 4 years following surgery [6–8].
Akagi et al. [4] in one of the earliest studies on acetabular development following open reduction without additional surgeries, noted satisfactory outcome in 14 out of 22 hips at mean follow-up of 15 years. Kagawa et al. [8] analyzed 43 hips diagnosed with complete hip dislocation after walking age, treated with open reduction alone. With final follow-up of 13.9 years of their cases, they noted improvement in acetabular index 1 year after surgery and recommended that acetabular remodeling continues beyond 6 years of patient age with maintenance of good concentricity.
Gholve et al. [6] evaluated 49 cases of DDH in walking age children treated by OR with or without femoral/pelvic osteotomy and noted mean AI remodeling from 44° to 20° during initial 4 years. 73% (19 out of 27 hips) of their patients who did not receive concurrent femoral osteotomy at the time of open reduction needed additional procedures for dysplasia and they recommended it as a strong predictor of secondary procedure for dysplasia.
Kothari et al. [20] in their systematic review on effect of bony surgery on results of anterior open reduction of DDH in walking age children noted that the hips treated with open reduction alone had lowest rates of AVN and satisfactory radiological and clinical results as compared to hips that underwent open reduction combined with pelvic and/or femoral osteotomy. However, the rate of requirement of secondary surgical procedures following open reduction alone was 10–15 times more compared to open reduction with pelvic and/or femoral osteotomy. Based on these findings, they concluded that combining pelvic osteotomy with anterior OR as the preferred management option for late diagnosed DDH.
However, many studies based on magnetic resonance evaluation of acetabulum in DDH have shown that the cartilaginous anatomy of the acetabulum is different from bony anatomy visible on radiographs and needs to be evaluated accurately and separately. They recommend cartilaginous acetabulum is fully formed at birth and remains constant throughout childhood. This cartilaginous anlage provides stability to the reduced femoral head and represents the true potential for acetabular growth in younger children [21–23]. Zadeh et al. [9] evaluated 95 hips with DDH treated by open reduction at mean age of 28 months. They used test of stability as an assessment tool to decide the need for concomitant osteotomy following open reduction. Majority of their cases (63 out of 95 hips) required open reduction and femur osteotomy for stable reduction and 90% of these achieved satisfactory radiological outcome. In the present study, the same principle of checking the position of joint stability intraoperatively to decide on femoral/pelvic osteotomy were employed. Sufficient cartilaginous component of acetabulum offering good cover and stability to the femoral head was noted even in cases where pre-operative radiograph showed significant acetabular dysplasia. None of these hips needed flexion beyond 30° for stable reduction and hence we refrained from adding pelvic osteotomies. Out of 28 hips available for evaluation at outcome measure point of 6 years of age, 24 hips showed satisfactory acetabular remodeling with mean AI of 22.6° in our series.
The role of age at reduction on acetabular development is still controversial, with few reports emphasizing no influence of timing of intervention on acetabular remodeling [16, 24] and few studies showing better acetabular development in children who had treatment less than 2 years of age [9, 13]. we found better remodeling in children who had surgery aged < 24 months. The rate of avascular necrosis was 12.5% (5 hips) in our series which remains a major risk of open reduction in late diagnosed DDH cases. Open reduction with femoral osteotomy was found to be associated with more incidence of AVN (4/5 hips). Coxa magna was found in 7 hips in our study (17.5%) and its reported incidence following open reduction is 33–36%. The incidence of coxa magna was found to be more in OR with femur osteotomy (5 hips) compared to OR alone (2 hips). Surgical invasion causing synovitis of hip, hyperaemia and over widening of the acetabulum by excessive limbus excision were the possible reasons reported in literature for development of coxa magna [25, 26]. There was no incidence of subluxation/re-dislocation at the latest follow-up.
Some of the major limitations of this study includes its retrospective study design with a small sample size. Our study has got limited follow-up and outcome measurement at 6 years of age may not represent the full remodeling potential of acetabulum which may continue several years. A significant proportion of cases (12 hips) was lost to follow-up in our series and could not be included for outcome evaluation. This might have influenced the interpretation of our findings. The influence of pelvic inclination on radiographic assessment and measurement errors due to difficulty in marking the exact, outermost edge of the acetabulum cannot be ruled out. Further, multimodality assessment of acetabular development using computed tomography and magnetic resonance imaging would be ideal.
Conclusion
Open reduction in late-diagnosed developmental dysplasia of hip has potential for favourable acetabular development. Femoral osteotomy when required, along with open reduction may be sufficient to address acetabular dysplasia found in the initial years of management of DDH.
Acknowledgements
We like to thank Mr Ganesh Dharanendra for his assistance in statistical analysis of the data.
Funding
The authors declare no funding was received for this study.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard statement
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed consent
For this type of study informed consent is not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Murphy RF, Kim YJ. Surgical management of pediatric developmental dysplasia of the hip. Journal of American Academy of Orthopaedic Surgeons. 2016;24(9):615–624. doi: 10.5435/JAAOS-D-15-00154. [DOI] [PubMed] [Google Scholar]
- 2.Chen IH, Kuo KN, Lubicky JP. Prognosticating factors in acetabular development following reduction of developmental dysplasia of the hip. Journal of Pediatric Orthopaedics. 1994;14(1):3e8. doi: 10.1097/01241398-199401000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Lindstrom JR, Ponseti IV, Wenger DR. Acetabular development after reduction in congenital dislocation of the hip. Journal of Bone and Joint Surgery American Volume. 1979;61(1):112Y118. doi: 10.2106/00004623-197961010-00020. [DOI] [PubMed] [Google Scholar]
- 4.Akagi S, Tanabe T, Ogawa R. Acetabular development after open reduction for developmental dislocation of the hip. 15-year follow-up of 22 hips without additional surgery. Acta Orthopaedic Scandinavica. 1998;69(1):17Y20. doi: 10.3109/17453679809002348. [DOI] [PubMed] [Google Scholar]
- 5.Harris NH, Lloyd-Roberts GC, Gallien R. Acetabular development in congenital dislocation of the hip With special reference to the indications for acetabuloplasty and pelvic or femoral realignment osteotomy. The Journal of Bone and Joint Surgery British Volume. 1975;57(1):46Y52. [PubMed] [Google Scholar]
- 6.Gholve PA, Flynn JM, Garner MR, Millis MB, Kim YJ. Predictors for secondary procedures in walking DDH. Journal of Pediatric Orthopaedics. 2012;32(3):282–289. doi: 10.1097/BPO.0b013e31824b21a6. [DOI] [PubMed] [Google Scholar]
- 7.Albinana J, Dolan LA, Spratt KF, Morcuende J, Meyer MD, Weinstein SL. Acetabular dysplasia after treatment for developmental dysplasia of the hip. Implications for secondary procedures. The Journal of Bone and Joint Surgery British Volume. 2004;86(6):876–886. doi: 10.1302/0301-620X.86B6.14441. [DOI] [PubMed] [Google Scholar]
- 8.Kagawa Y, Endo H, Tetsunaga T, Fujii Y, Miyake T, Ozaki T. Acetabular development after open reduction to treat dislocation of the hip after walking age. Journal of Orthopaedic Science. 2016;21(6):815–820. doi: 10.1016/j.jos.2016.07.007. [DOI] [PubMed] [Google Scholar]
- 9.Zadeh HG, Catterall A, Hashemi-Nejad A, Perry RE. Test of stability as an aid to decide the need for osteotomy in association with open reduction in developmental dysplasia of the hip. The Journal of Bone and Joint Surgery British Volume. 2000;82(1):1727. doi: 10.1302/0301-620X.82B1.0820017. [DOI] [PubMed] [Google Scholar]
- 10.Hilgenreiner H. Classic. Translation: Hilgenreiner on congenital hip dislocation. Journal of Pediatric Orthopaedics. 1986;6:202–214. doi: 10.1097/01241398-198603000-00016. [DOI] [PubMed] [Google Scholar]
- 11.Tönnis D. Normal values of the hip joint for the evaluation of X-rays in children and adults. Clinical Orthopaedics and Related Research. 1976;119:39–47. [PubMed] [Google Scholar]
- 12.Li Y, Guo Y, Li M, Zhou Q, Liu Y, Chen W, Li J, Canavese F, Xu H. Multi-center Pediatric Orthopedic Study Group of China. Acetabular index is the best predictor of late residual acetabular dysplasia after closed reduction in developmental dysplasia of the hip. International Orthopaedics. 2018;42(3):631–640. doi: 10.1007/s00264-017-3726-5. [DOI] [PubMed] [Google Scholar]
- 13.Abousamra O, Deliberato D, Singh S, Klingele KE. Closed vs open reduction in developmental dysplasia of the hip: The short-term effect on acetabular remodeling. Journal of Clinical Orthopaedics and Trauma. 2020;11(2):213–216. doi: 10.1016/j.jcot.2019.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Klisic P, Jankovic L, Basara V. Long-term results of combined operative reduction of the hip in older children. Journal of Pediatric Orthopaedics. 1988;8(5):532e4. doi: 10.1097/01241398-198809000-00006. [DOI] [PubMed] [Google Scholar]
- 15.Dimitriou JK, Cavadias AX. One-stage surgical procedure for congenital dislocation of the hip in older children. Long-term results. Clinical Orthopaedics and Related Research. 1989;246:308. doi: 10.1097/00003086-198909000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Brougham DI, Broughton NS, Menelaus MB. The predictability of acetabular development after closed reduction for congenital dislocation of the hip. Journal of Bone and Joint Surgery British Volume. 1988;70:733–736. doi: 10.1302/0301-620X.70B5.3192570. [DOI] [PubMed] [Google Scholar]
- 17.Cherney DL, Westin GW. Acetabular development in the infant’s dislocated hips. Clinical Orthopaedics. 1989;242:98–103. doi: 10.1097/00003086-198905000-00010. [DOI] [PubMed] [Google Scholar]
- 18.Salter RB. Specific guidelines in the application of the principle of innominate osteotomy. Orthopedic Clinics of North America. 1972;3(1):14956. doi: 10.1016/S0030-5898(20)32185-4. [DOI] [PubMed] [Google Scholar]
- 19.Schwartz DR. Acetabular development after reduction of congenital dislocation of the hip: a follow-up study of fifty hips. Journal of Bone and Joint Surgery American. 1965;47-A:705–714. doi: 10.2106/00004623-196547040-00005. [DOI] [PubMed] [Google Scholar]
- 20.Kothari A, Grammatopoulos G, Hopewell S, Theologis T. How does bony surgery affect results of anterior open reduction in walking-age children with developmental hip dysplasia? Clinical Orthopaedics and Related Research. 2016;474(5):1199–1208. doi: 10.1007/s11999-015-4598-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li LY, Zhang LJ, Li QW, Zhao Q, Jia JY, Huang T. Development of the osseous and cartilaginous acetabular index in normal children and those with developmental dysplasia of the hip: a cross-sectional study using MRI. Journal of Bone and Joint Surgery. British Volume. 2012;94(12):1625–1631. doi: 10.1302/0301-620X.94B12.29958. [DOI] [PubMed] [Google Scholar]
- 22.Zamzam MM, Kremli MK, Khoshhal KI, Abak AA, Bakarman KA, Alsiddiky AM, Alzain KO. Acetabular cartilaginous angle: a new method for predicting acetabular development in developmental dysplasia of the hip in children between 2 and 18 months of age. Journal of Pediatric Orthopaedics. 2008;28(5):518–523. doi: 10.1097/BPO.0b013e31817c4e6d. [DOI] [PubMed] [Google Scholar]
- 23.Douira-Khomsi W, Smida M, Louati H, Hassine LB, Bouchoucha S, Saied W, Ladeb MF, Ghachem MB, Bellagha I. Magnetic resonance evaluation of acetabular residual dysplasia in developmental dysplasia of the hip: a preliminary study of 27 patients. Journal of Pediatric Orthopaedics. 2010;30(1):37–43. doi: 10.1097/BPO.0b013e3181c877d7. [DOI] [PubMed] [Google Scholar]
- 24.Forlin E, Choi IH, Guille JT, Bowen JR, Glutting J. Prognostic factors in congenital dislocation of the hip treated with closed reduction. The importance of arthrographic evaluation. Journal of Bone and Joint Surgery. British Volume. 1992;74(8):1140e52. doi: 10.2106/00004623-199274080-00003. [DOI] [PubMed] [Google Scholar]
- 25.Imatani J, Miyake Y, Nakatsuka Y, Akazawa H, Mitani S. Coxa magna after open reduction for developmental dislocation of the hip. Journal of Pediatric Orthopaedics. 1995;15(3):337e41. doi: 10.1097/01241398-199505000-00015. [DOI] [PubMed] [Google Scholar]
- 26.Nemoto N, Taira K, Maseda M, Nagao S, Yamaguchi T, Sato M. Clinical outcome of developmental dysplasia of the hip after walking age. The Journal of the Japanese Pediatric Orthopaedic Association. 2012;21(2):2515. [Google Scholar]