Abstract
Introduction
Leg-length difference (LLD) is common in patients with developmental dysplasia of the hip (DDH). LLD of > 1 cm at skeletal maturity is reported in > 40% of patients, with the majority related to ipsilateral overgrowth. A longer DDH leg might lead to excessive mechanical loading at the acetabular margin, resulting in compromised acetabular development. We hypothesised that the LLD would negatively influence acetabular development. If so, it would be advantageous to identify such patients early in the course of follow-up, and address this if necessary.
Methods
A retrospective study was conducted on a consecutive series of DDH patients managed surgically at the Royal National Orthopaedic Hospital, Stanmore, United Kingdom. We included patients with adequate long-leg radiographs at the age of 4–8 years (early-FU) and skeletal maturity (final-FU). Bilateral cases and those who underwent surgical procedures for hip dysplasia during the follow-up period were excluded. Measurements including leg length and centre-edge-angle (CE-angle) were obtained at the 2 time points.
Results
Twenty-seven patients were included, mean age at early-FU 5.7 (± 0.9) years, and 13.9 (± 1.0) years at final-FU. Mean LLD at early-FU was 9.5 (± 7.6) mm and 10.9 (± 9.4) mm at final-FU, p = 0.337. Correlation between early- and final-FU LLD was 0.68 (p < 0.001). The mean CE-angle at early follow-up was 14.6° (± 9.8), this improved to 23.2° (± 8.2) at skeletal maturity (p = 0.003, paired samples t-test). Linear regression analysis showed a non-significant trend towards less CE-angle improvement in patients with more initial residual dysplasia and more initial LLD.
Conclusion
Most leg-length differences can be identified early in the follow-up period, nevertheless, considerable individual changes in LLD are observed on continued follow-up. Furthermore, a trend was observed towards impaired acetabular improvement in patients with more LLD. These findings justify careful clinical and radiological monitoring of LLD from an early stage in the follow-up period.
Supplementary Information
The online version contains supplementary material available at 10.1007/s43465-021-00492-5.
Keywords: Developmental dysplasia of the hip, Hip dysplasia, Leg length difference, Leg length discrepancy, Long leg dysplasia, Residual dysplasia
Introduction
Patients with developmental dysplasia of the hip (DDH) are known to be at risk for the development of a leg length difference (LLD) during growth. Overgrowth of the ipsilateral limb is common in unilateral DDH; a LLD of more than 1 cm is reported in over 40% of patients [1, 2]. This difference is typically identified in those who have undergone surgery, although asymmetry of femoral lengths has also been reported in those managed conservatively [1, 3].
A discrepancy in leg length is known to influence gait and may be a potential cause of back pain [4, 5]. However, in DDH patients, additional concern is raised due to the potential negative influence of a longer leg on acetabular development secondary to excessive mechanical loading at the acetabular margin [6, 7].
Early identification of those at risk of developing a significant LLD would be advantageous to adjust management in a timely manner. This would lead to an increased vigilance for persistence or progression of residual dysplasia in such patients, with the possibility to apply conservative measures and/or surgical growth modulating interventions to prevent ‘long leg dysplasia’ from exacerbating the dysplasia.
A few reports have looked into risk factors predicting the development of a LLD in patients with DDH. To date the only risk factor for development of a longer DDH leg that has been identified is a history of femoral osteotomy, especially when performed between the ages of 2–4 [1–3]. The cause for femoral overgrowth has been attributed to increased physeal activity secondary to local postoperative hyperaemia [1, 6]. Patterns of development of leg length discrepancy have been described by Shapiro. In theory the LLD development following DDH treatment would follow a Shapiro type III, where there is early increase of LLD that reaches a plateau phase up to skeletal maturity [8]. Therefore, we hypothesised that for patients surgically treated for DDH, the LLD should already be identifiable early in the follow-up period.
The aim of the present study was to analyse the relationship between LLD early in the follow-up period and at skeletal maturity. Furthermore, we aimed to assess to what extent the presence of a LLD at early follow-up contributes to impaired acetabular development.
Methods
A retrospective cohort study was conducted on a consecutive series of patients with DDH treated in the period January 2008–December 2020 at the Royal National Orthopaedic Hospital, Stanmore, United Kingdom. The local medical ethics committee agreed with conduction of the study. Due to its retrospective nature, an informed consent procedure was not deemed necessary.
We included all patients with adequate long leg radiographs between the age of 4–8 and at skeletal maturity. Bilateral cases and patients with conditions reported to influence leg lengths (e.g., neuromuscular conditions, skeletal dysplasia) were excluded. Patients that were surgically treated for DDH after the initial long leg film or those undergoing surgery within 2 years prior to the initial long leg film were excluded, because either the intervention itself or hyperaemia induced overgrowth could potentially influence leg length at skeletal maturity [8–10]. In our institution patients with successful Pavlik harness treatment are not followed up until skeletal maturity, and therefore this cohort was not included in the present study [11].
Patient and treatment characteristics were obtained regarding age at diagnosis, age at final follow-up, side affected, and treatment modalities utilised. In our institution for patients with DDH and a LLD, an intervention aimed at equalising leg length, usually a contra-lateral distal femoral epiphysiodesis, is routinely offered to patients with a LLD of 1.5 cm or more. For this subgroup of patient’s data on type of leg length equalisation procedure, age at intervention, length difference at intervention and at skeletal maturity were obtained.
Assessment of Leg Length
According to the Royal National Orthopaedic Hospital DDH follow-up protocol, the first radiological assessment of leg length is performed at an age of approximately 5 years [11]. This first long leg radiograph was used for the initial assessment of leg length difference. To assess final LLD, the first radiograph at skeletal maturity was used. For patients that underwent an epiphysiodesis to correct leg length, the last long leg standing film before the procedure was used for final length measurements.
Measurements were performed on calibrated, standardised standing long leg radiographs, with patients positioned with patellae facing forward. Measurements included total leg length, femoral length and tibial length, and was obtained using Traumacad (Brainlabs, Petach-Tikva, Israel) software [12]. Acetabular coverage was measured using the lateral centre-edge angle of Wiberg (CE-angle) [13], and the presence of proximal femoral avascular necrosis (AVN) was classified according to Kalamchi and MacEwan [14].
Statistical Analysis
For descriptive statistics of continuous variables, means with standard deviations were reported and for discrete variables, counts and percentages are presented.
Mean LLD between the DDH affected and the unaffected leg were compared between early follow-up (early-FU) and final follow-up (final-FU), using a paired samples t-test for each of the leg segments measured (total leg length, tibial length, total femoral length) and reported as mean differences with 95% confidence intervals. The relationship between LLD at early-FU and final-FU was analysed using Pearson’s R.
Difference in LLD between patients that underwent epiphysiodesis and patients that did not undergo epiphysiodesis was compared using independent-samples t-test and change in LLD before and after epiphysiodesis was compared using paired-samples t-test. Similar comparisons were made for patients that had multiple operations for DDH versus patients that had a single intervention. Furthermore, an analysis was made on differences between DDH treatment groups regarding LLD at skeletal maturity and change in LLD between early FU and skeletal maturity, using a Kruskal–Wallis test.
Change in CE-angle was assessed between early-FU and final-FU, using paired-samples t-test. Influence of LLD at early-FU on change in CE-angle was analysed in a linear regression, with severity of residual dysplasia at early FU and AVN grade as co-variates.
All data analysis was performed using IBM® SPSS software, version 24.0
Results
Out of 77 consecutive DDH patients with appropriate radiological follow-up, 27 could be included. Reasons for exclusion were: surgery within 2 years (before or after) of early-FU radiological assessment n = 33, bilateral DDH n = 11, non-measurable radiographs n = 4, inadequate medical records n = 2. Mean age at first long leg film follow-up was 5.7 (± 0.9) years and mean age at final follow-up was 13.9 (± 1.0) years. Baseline characteristics, AVN grade and surgical treatment details are presented in Table 1, six patients (22.2%) underwent multiple operations for DDH.
Table 1.
Patient characteristics
| Sex | Female 25: Male 2 |
| Side affected | Right 18: Left 9 |
| Mean age at diagnosis | 13.6 months (± 10.5) months |
| Treatment type (n [%]) | |
| Closed reduction | 4 (14.8%) |
| Open reduction | 4 (14.8%) |
| OR and femoral osteotomy | 7 (25.9%) |
| OR and pelvic osteotomy | 3 (11.1%) |
| OR and femoral and pelvic osteotomy | 9 (33.3%) |
| Multiple operations | 6 (22.2%) |
| AVN grade | |
| No AVN or Type 1 | 18 (66.7%) |
| Type 2 | 8 (29.6%) |
| Type 3 | 1 (3.7%) |
| Surgical procedure to address LLD | 9 (33.3%) |
Data presented as mean (standard deviation) or as count (percentage) depending on data type
OR open reduction, AVN avascular necrosis, LLD leg length difference
Mean LLDs at early and final follow-up are presented in Table 2. Mean change in total LLD between early FU and skeletal maturity was 1.4 mm (95% CI − 1.5–4.4), p = 0.337. The change in LLD showed a normal distribution, with individual changes in LLD ranging from − 14 to 18 mm (Fig. 1). Correlation for total LLD between early FU and final FU was 0.68 (p < 0.001, Pearson’s r) and for the femoral length difference the correlation was 0.84 (p < 0.001, Pearson’s r). The relationship between LLD at early FU and at skeletal maturity is visualised in Fig. 2.
Table 2.
Leg length difference
| Early follow-up | FU at skeletal maturity* | Change (95% CI) | p value | |
|---|---|---|---|---|
| Total LLD | 9.5 (7.6) | 10.9 (9.4) | 1.4 (− 1.5–4.4) | 0.337 |
| Femoral difference | 8.1 (6.5) | 9.8 (8.7) | 1.7 (− 0.2–1.9) | 0.074 |
| Tibial difference | 0.7 (2.8) | 1.8 (3.9) | 1.1 (− 0.6–1.4) | 0.192 |
| Total LLD stratified for treatment group | ||||
| Closed reduction (n = 4) | 7.5 (4.5) | 7.8 (6.4) | 0.3 (− 3.3–3.8) | 0.836 |
| Open reduction (n = 4) | 9.5 (8.4) | 9.5 (10.6) | 0.0 (− 10.3–10.3) | 0.999 |
| OR and femoral osteotomy (n = 7) | 10.3 (9.7) | 12.6 (11.5) | 2.3 (− 3.6–8.1) | 0.375 |
| OR and pelvic osteotomy (n = 3) | 4.7 (4.2) | 11.0 (8.9) | 6.3 (− 13.0–25.6) | 0.293 |
| OR and femoral and pelvic osteotomy (n = 9) | 11.4 (7.8) | 11.7 (10.1) | 0.2 (− 7.6–8.1) | 0.950 |
Data presented as mean (standard deviation), comparison using paired samples t-test
CI confidence interval, LLD leg length difference, OR open reduction
*Measurement at skeletal maturity X-ray or at moment of epiphysiodesis for epiphysiodesis patients
Fig. 1.
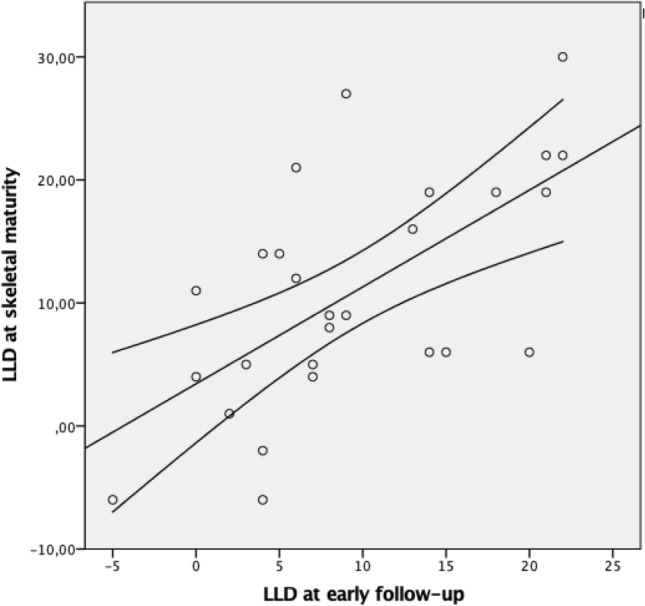
Visualisation of leg-length difference at early follow-up (x-axis) versus leg-length difference at final follow-up (y-axis). All measurements in millimeters. Line of best fit with corresponding 95% confidence interval
Fig. 2.
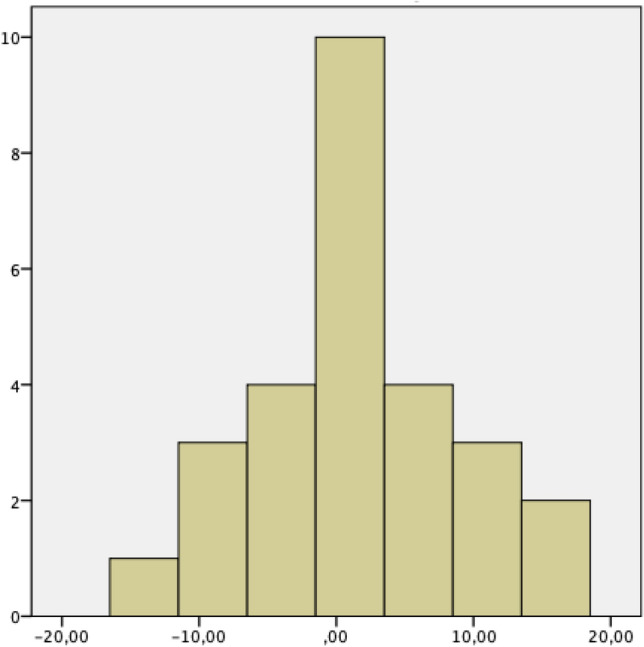
Histogram presenting change in leg-length difference in millimetres between early and final follow-up (x-axis), for number of patients (y-axis) in the cohort
LLD stratified for treatment group are presented in Table 2. No differences between treatment groups was observed regarding LLD at skeletal maturity and change in LLD between early FU and skeletal maturity; test for between groups differences p = 0.895 and p = 0.723, respectively (Kruskal–Wallis). Nine patients underwent multiple procedures; in two patients this was closed reduction first and open reduction second, femoral and pelvic osteotomy second, in two patient closed reduction first and open reduction second and in one patient femoral osteotomy first and femoral and pelvic osteotomy second. No statistical differences were observed between patients with multiple vs. single procedures regarding LLD at skeletal maturity (9.7 [9.4] mm vs 15.2 [8.9] mm, p = 0.360), or change in CE-angle between early FU and skeletal maturity (8.5 [8.1]° vs. 4.5 [11.6]°, p = 0.217).
Nine patients underwent a leg length correction procedure at a mean age of 11.8 (± 1.5) years. In all patients these patients the DDH leg was longer and a contralateral epiphysiodesis of the distal femur was performed to reduce LLD. Mean LLD before epiphysiodesis was 19.3 (± 6.9) mm, reducing to 7.9 (± 8.4) mm at skeletal maturity (p = 0.003). At early FU, the LLD in the epiphysiodesis group was 13.1 (± 6.4, range 6–22), compared to 7.7 (± 7.6, range − 5–21) in the non-epiphysiodesis group (p = 0.08).
The mean CE angle at early follow-up was 14.6° (± 9.8), this improved to 23.2° (± 8.2) at skeletal maturity (p = 0.003). A linear regression analysis on factors influencing improvement of the CE-angle up to skeletal maturity, showed a trend towards less acetabular improvement for more initial residual dysplasia and more initial LLD but the correlations were not significant (Table 3). Adjusted R2 for this analysis was 0.275.
Table 3.
Multivariate linear regression analysis on predictors for improvement in CE-angle between early- and final-FU
| B | 95% CI B | Beta | p value | |
|---|---|---|---|---|
| LLD at early-FU | − 0.34 | − 0.80 to 0.10 | − 0.28 | 0.10 |
| CE-angle at early-FU | − 0.43 | − 0.87 to − 0.01 | − 0.40 | 0.05 |
| AVN grade | − 2.88 | − 9.32 to 3.57 | − 0.18 | 0.36 |
B unstandardised regression coefficient, Beta standardised regression coefficient, LLD leg-length-difference, FU follow-up, AVN avascular necrosis, CE-angle lateral center-edge-angle of Wiberg, SE standard error
Discussion
The present study found that in DDH patients, LLD at skeletal maturity is highly correlated to LLD found at early follow-up between the age of 4 and 8 years. Despite the observation that most LLDs can be identified early, considerable individual changes in LLD were observed during the rest of growth. Furthermore, we observed a trend towards impaired acetabular improvement in patients with more initial LLD.
We found that both at early follow-up and at skeletal maturity the DDH leg was on average longer than the contralateral leg [1–3]. Yoon et al. describe that overgrowth of the affected limb is common in DDH patients, with 44% having at least 1 cm LLD. In the patients with a LLD in their cohort, the vast majority had a longer DDH leg, which is in line with our results [1]. We hypothesised that the development of a LLD in DDH patients would follow a Shapiro type III pattern [8]. Surgical treatment for DDH often includes femoral osteotomies, which theoretically leads to a temporary increase in rate of growth on the affected side due to increased periosteal blood flow as observed following paediatric femoral shaft fractures [10, 15, 16]. In a typical Shapiro type III pattern after the initial overgrowth period, the LLD remains stable until skeletal maturity (Fig. 3) [8]. This is at least partly reflected by our results with no significant change noted in LLD between early follow-up and skeletal maturity. Furthermore, all patients that underwent surgical epiphysiodesis to equalise leg length had a LLD that was identifiable at early FU (> 5 mm difference). Nevertheless, other factors than temporary proximal femoral overgrowth must play a role in the development of the LLD, because after the initial long leg radiographic assessment both considerable increase as well as considerable decrease in individual patients LLD was observed (Figs. 1, 2). The presence/development of AVN may play a role in some patients; leading to growth inhibition or early proximal femoral physeal closure resulting in a relatively shorter DDH leg at skeletal maturity, resembling a Shapiro type 4 pattern [2, 8]. In some patients on the other hand, the DDH leg continued to grow relatively faster than the contralateral side. This suggest that sustained overgrowth extending beyond the initial FU period can occur as well.
Fig. 3.
Shapiro type 3 developmental pattern, the leg length discrepancy first increases with time, but then stabilizes and remains unchanged throughout the remaining period of growth
It has been suggested that a long leg on the DDH side may have a negative influence on acetabular development [6, 7]. A term described as ‘long leg dysplasia’ [6, 7]. The development of the acetabulum is driven by two areas of growth; interstitial growth at the triradiate cartilage responsible for acetabular expansion and cartilage under the perichondrium responsible for appositional growth [17]. As the final shape of the acetabulum is closely related to that of the proximal femur [17], in theory eccentric acetabular loading due to a LLD induced pelvic tilt can impact the appositional growth at the perichondrium. In our cohort, we noted an overall significant improvement in the mean CE angle from early-FU to skeletal maturity. We noted that patients with more LLD at early follow-up had a more modest improvement in CEA, although this trend was not statistically significant (Figs. 4, 5). This might be influenced by the relatively small number of patients in this study, and the departmental policy of treating LLD aggressively with appropriate monitoring, epiphysiodesis and shoe raises during growth, perhaps resulting in a diminished effect of LLD on acetabular development in our cohort.
Fig. 4.
Radiographs of patient with right hip dysplasia with symmetrical leg lengths demonstrating improved CEA from 7° (age 5 years) to CEA 29° (age 13 years)
Fig. 5.
Radiographs of patient with right hip dysplasia with LLD of 17 mm (age 6 years) and persistent LLD of 10 mm at skeletal maturity following femoral varus shortening osteotomy (aged 11 years) demonstrating continued dysplasia with CEA of 13° (at skeletal maturity, aged 14 years)
The findings that a LLD can often be diagnosed early and the potential influence of a LLD on persistent acetabular dysplasia, emphasise the need for thorough assessment of leg length early in the follow-up and at set intervals until skeletal maturity. This is in concordance with the Stanmore DDH surveillance protocol [11]. Given the potential negative influence on acetabular development in DDH, treatment of LLD should be considered even below the traditional treatment threshold of 2 cm [5, 18]. In general, a contralateral heel raise for younger patients and an epiphysiodesis on the longer side for patients nearing skeletal maturity, will be sufficient [18]. As smaller differences might be missed on clinical assessment, we suggest obtaining long leg films to assess both hip development and leg length [11, 19]. The appropriate age to assess length differences and hip development are at 5 years to identify an initial LLD, at 8 years to identify patients with sustained/increasing femoral overgrowth, and around 2 years prior to predicted skeletal maturity (12 years for girls and 14 years for boys) to plan surgical leg length correction procedures for selected cases [11].
A limitation of the present study is the relatively small sample size, resulting from the strict inclusion and exclusion criteria we used. This allowed us to look at the development of LLD without other confounding factors such as overgrowth from recent surgery and surgical interventions changing leg length after radiographs at early follow-up. We can conclude that it is possible to identify a LLD early in the FU period. Unfortunately, the small number of patients prevented us from performing a more in-depth analysis of the influence of treatment and patient characteristics leading to LLD and change in LLD after early-FU in patients treated for DDH.
Another potential limitation is that the cohort presented does not reflect an average DDH follow-up population.
Of the included patients, a relatively high percentage of patients had femoral and/or pelvic osteotomies; one in five had multiple procedures and the included patients presented relatively late. These characteristics are a reflection of the complex case mix treated in the tertiary referral centre where this study was conducted. Both the relatively high incidence of LLD, and relatively high incidence of residual dysplasia reported for our cohort can to a large extent be explained by the complexity of DDH in our population. When generalising these results to a setting with less complex affected individuals, it should be recognised that the overall incidence of LLD and residual dysplasia is likely to be lower.
Conclusion
Most LLD in patients treated for DDH can be identified early in the follow-up period. Nevertheless, considerable individual changes in LLD can be observed between early follow-up measurements and skeletal maturity. A trend was observed towards impaired acetabular improvement in patients with more initial LLD. These findings emphasise the need for thorough assessment of leg length early in the follow-up and at set intervals during follow-up until skeletal maturity for DDH patients.
Supplementary Information
Below is the link to the electronic supplementary material.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard statement
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed consent
For this type of study informed consent is not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Jaap J. Tolk, Email: J.Tolk@erasmusmc.nl
Rajiv Merchant, Email: R.Merchant@NHS.net.
Deborah M. Eastwood, Email: DeborahEastwood1@NHS.net
Pranai Buddhdev, Email: Pranai.buddhdev@nhs.net.
Aresh Hashemi-Nejad, Email: Aresh.Nejad@NHS.net.
References
- 1.Yoon C, Shin CH, Kim DO, Park MS, Yoo WJ, Chung CY, et al. Overgrowth of the lower limb after treatment of developmental dysplasia of the hip: incidence and risk factors in 101 children with a mean follow-up of 15 years. Acta Orthopaedica. 2020;91(2):197–202. doi: 10.1080/17453674.2019.1688485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Merchant R, Tolk JJ, Ayub A, Hashemi-Nejad A, Eastwood DM, Tennant S, et al. The importance of leg length monitoring in developmental dysplasia of the hip. Orthopaedic Proceedings. 2021;103-B(supplement 6):52. [Google Scholar]
- 3.Metcalfe JE, Banaszkiewicz P, Kapoor B, Richardson J, Jones CW, Kuiper J. Unexpected long femur in adults with acetabular dysplasia. Acta Orthopaedica Belgica. 2005;71(4):424–428. [PubMed] [Google Scholar]
- 4.Song KM, Halliday SE, Little DG. The effect of limb-length discrepancy on gait. Journal of Bone and Joint Surgery American Volume. 1997;79(11):1690–1698. doi: 10.2106/00004623-199711000-00011. [DOI] [PubMed] [Google Scholar]
- 5.Gordon JE, Davis LE. Leg length discrepancy: the natural history (and what do we really know) Journal of Pediatric Orthopedics. 2019;39(6):S10–S13. doi: 10.1097/BPO.0000000000001396. [DOI] [PubMed] [Google Scholar]
- 6.Zadeh H, Catterall A, Hashemi-Nejad A, Perry R. Test of stability as an aid to decide the need for osteotomy in association with open reduction in developmental dysplasia of the hip. The Bone & Joint Journal. 2000;82(1):17–27. doi: 10.1302/0301-620x.82b1.9618. [DOI] [PubMed] [Google Scholar]
- 7.Ponseti I. Growth and development of the acetabulum in the normal child: anatomical, histological, and roentgenographic studies. Journal of Bone and Joint Surgery American Volume. 1978;60(5):757–585. [PubMed] [Google Scholar]
- 8.Shapiro F. Developmental patterns in lower-extremity length discrepancies. The Journal of Bone and Joint - Series A. 1982;64(5):639–651. [PubMed] [Google Scholar]
- 9.Segaren N, Abdul-Jabar HB, Hashemi-Nejad A. The influence of the choice of closing wedge angle on leg length discrepancy after proximal femoral varus osteotomy. The Bone & Joint Journal. 2014;96 B(8):1124–1129. doi: 10.1302/0301-620X.96B8.33322. [DOI] [PubMed] [Google Scholar]
- 10.Shapiro F. Fractures of the femoral shaft in children: the overgrowth phenomenon. Acta Orthopaedica. 1981;52(6):649–655. doi: 10.3109/17453678108992162. [DOI] [PubMed] [Google Scholar]
- 11.Wright J, Tudor F, Luff T, Hashemi-Nejad A. Surveillance after treatment of children with developmental dysplasia of the hip: current UK practice and the proposed Stanmore protocol. Journal of Pediatric Orthopedics. Part B. 2013;22(6):509–515. doi: 10.1097/BPB.0b013e3283636feb. [DOI] [PubMed] [Google Scholar]
- 12.Segev E, Hemo Y, Wientroub S, Ovadia D, Fishkin M, Steinberg DM, et al. Intra- and interobserver reliability analysis of digital radiographic measurements for pediatric orthopedic parameters using a novel PACS integrated computer software program. Journal of Children’s Orthopaedics. 2010;4(4):331–341. doi: 10.1007/s11832-010-0259-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint. Acta Chirurgica Scandinavica. 1939;58:1–130. [Google Scholar]
- 14.Kalamchi A, MacEwen G. Avascular necrosis following treatment of hip dislocation avascular necrosis following treatment of congenital dislocation of the hip. Journal of Bone and Joint Surgery American Volume. 1980;62:876–888. doi: 10.2106/00004623-198062060-00002. [DOI] [PubMed] [Google Scholar]
- 15.Irani RN, Nicholson JT, Chung SM. Long-term results in the treatment of femoral-shaft fractures in young children by immediate spica immobilization. Journal of Bone and Joint Surgery American Volume. 1976;58(7):945–951. doi: 10.2106/00004623-197658070-00009. [DOI] [PubMed] [Google Scholar]
- 16.Nascimento FP, Santili C, Akkari M, Waisberg G, Braga SR, Fucs PMMB. Flexible intramedullary nails with traction versus plaster cast for treating femoral shaft fractures in children: comparative retrospective study. Sao Paulo Medical Journal. 2013;131(1):5–12. doi: 10.1590/S1516-31802013000100002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weinstein SL, Dolan LA. Proximal femoral growth disturbance in developmental dysplasia of the hip: What do we know? Journal of Children’s Orthopaedics. 2018;12(4):331–341. doi: 10.1302/1863-2548.12.180070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Inan M, Chan G, Bowen JR. The correction of leg-length discrepancy after treatment in developmental dysplasia of the hip by using a percutaneous epiphysiodesis. Journal of Pediatric Orthopaedics Part B. 2008;17(1):43–46. doi: 10.1097/BPB.0b013e3282e61af7. [DOI] [PubMed] [Google Scholar]
- 19.Sabharwal S, Kumar A. Methods for assessing leg length discrepancy. Clinical Orthopaedics and Related Research. 2008;466(12):2910–2922. doi: 10.1007/s11999-008-0524-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.




