Abstract
Objectives
This study aims to explore the attenuated impact of reported avoidance behaviours adherence on the transmission of COVID-19 through cross-sectional surveys in Hong Kong, in order to make up for the lack of research on avoidance behaviours fatigue.
Design
40 cross-sectional telephone surveys.
Setting
All districts in Hong Kong.
Participants
31 332 Cantonese or English-speaking participants at age of 18 years or above.
Methods
We collected data on behaviours and estimated the average effective reproduction number () among the Hong Kong adult population during the COVID-19 epidemic wave in November–December 2020 and compared with the preceding epidemic in June–July 2020.
Results
We observed a reduction in adherence to voluntary avoidance behaviours due to pandemic fatigue, but continued adherence to regulated avoidance behaviours. The average during the post-work from home period was higher in November–December wave with estimated of 0.81 (95% CI: 0.75 to 0.87) compared with the June–July wave with an of 0.67 (95% CI: 0.60 to 0.75).
Conclusions
The declined effectiveness of social distancing interventions in reducing COVID-19 transmission was associated with fatigue with voluntary avoidance behaviours in Hong Kong population, implying a need for the government to reinvigorate the public to maintain effective pandemic control.
Keywords: COVID-19, epidemiology, public health
Strengths and limitations of this study.
Multiple population-based cross-sectional surveys were conducted on participants selected with random digital dialling across multiple epidemic waves of COVID-19.
Similar public health and social measures were implemented in response to COVID-19 in two epidemic waves.
Preventive behaviours studied in the survey allowed for investigation of pandemic fatigue with avoidance behaviours in the population.
The association was demonstrated between transmission of COVID-19 and the pandemic fatigue.
Self-reporting preventive behaviours in the surveys might bias the findings of the study.
Introduction
On 31 December 2019, a cluster of atypical pneumonia was identified to the WHO Regional Office in Wuhan, China, which was identified as the novel SARS-CoV-2.1 To mitigate the COVID-19 pandemic, countries worldwide have enacted unprecedented public health and social measures (PHSMs).2 The WHO has recommended protective measures in response to the COVID-19 pandemic, such as maintaining physical distance at least 1 m away from each other, wearing a face mask, avoiding crowded or poorly ventilated areas and frequent handwashing.3 The extension of social/physical distancing measures and the use of masks could greatly reduce the risk of infection.4 Studies estimated that closing and restricting high-exposure business places and schools perhaps were the most effective public health interventions against COVID-19.2 5 6 Practising physical distancing has been a part of daily life for most people in the world although the compliance to the measures might not always be optimal.7–9
Pandemic fatigue with the PHSMs refers to a waning motivation to follow some recommended protective behaviours against infection, which can be driven by various underlying psychosocial and practical factors.10 Intense PHSMs applied during the pandemic resulted in high social and economic costs and posed a serious threat to the control of SARS-CoV-2 transmission due to the reduced compliance to the measures in the public. Modelling studies suggested that population compliance to social distancing measures might substantially affect the effectiveness in control of the spread of COVID-19,11 and the fatigue with interventions was likely to drive the second wave of COVID-19 in Europe.12
In Hong Kong, after the first confirmed case appeared in January 2020, a smaller second wave followed during March–April 2020.13 From July through August, COVID-19 cases rose sharply following identification of imported cases. The biggest epidemic wave starting from late November 2020 in Hong Kong was originated from clusters of cases linked to several dance clubs.14 Similar intense PHSMs were implemented over the epidemic waves alternating with periods of relaxation. We have been conducting population-based surveys to investigate the psycho-behaviour patterns in Hong Kong population in response to the COVID-19 pandemic. It provided us with an opportunity to investigate the phenomenon of pandemic fatigue and its potential association with COVID-19 transmission with the data collected from the two consecutive outbreaks in June–July and November–December 2020.
Methods
The survey
We conducted 40 cross-sectional telephone surveys throughout 2020 and in early 2021 in all districts in Hong Kong, initially at monthly intervals and then at weekly intervals from 5 May 2020 onwards to measure population responses to COVID-19 and recommended protective behaviours. Respondents who were Cantonese or English speakers at age of 18 years or older and had access to a landline or mobile telephone were eligible and invited for the survey, while visitors who travelled to Hong Kong would be excluded. In each household, we only invited one family member whose birthday was the closest to the survey date. A sample size of around 500 (n) was indicated to be sufficient to estimate population characteristics (p=0.5) with a margin of error 0.05 (m) and 95% CI (t=1.96) according to the following formula.15 16
Each survey included either 1000 or 500 respondents contacted via a computer-assisted random digit dialling of landlines and mobile phones. The survey items included basic demographic information, attitudes and risk perception towards COVID-19 and behavioural measures adopted in response to COVID-19 (eg, personal hygiene, mask wearing and reducing social contact). Verbal informed consent was obtained from all participants.
Statistical analysis
We identified the time periods when the government recommended civil servants to work from home (WFH), a measure often adopted by many private businesses as well during the two epidemic waves in June–July and November–December 2020 (online supplemental appendix table S1). We analysed behavioural responses of participants in the surveys conducted in the 3 weeks before the WFH announcement (pre-intervention) and 4 weeks after the WFH (post-intervention). Response frequencies were weighted to the adult population in Hong Kong by age, sex, educational attainment and occupation.17 Linear regression models were used to explore the relationship between the reported avoidance behaviours in the survey respondents and the weekly numbers of COVID-19 cases notified during the pre-intervention and post-intervention periods in each wave. In the surveys included in the analysis, participants (≤1%) who answered ‘don’t know’ or ‘refuse to answer’ in the questions about their behaviour in response to COVID-19 were included into the denominator for calculation of the adherence percentages (online supplemental appendix table S2).
bmjopen-2021-055909supp001.pdf (256.8KB, pdf)
We evaluated the transmissibility of COVID-19 over time with the effective reproduction number (), using the methods by Tsang et al.18 The change in COVID-19 transmission after the WFH policy was used to assess the impact of public health interventions (online supplemental appendix table S1) implemented during the two epidemic waves. We estimated the Rt for the pre-intervention period, that is, 2 weeks before the WFH announcement, and for the post-intervention period, 2–3 weeks after the WFH announcement, allowing for a 7-day delay from the date of implementing the interventions to the time for assessment of the transmission (approximately one serial interval), which were then used to quantify the effect of the interventions in reducing COVID-19 transmission.19 All analyses were done with R V.4.1.0.
Patient and public involvement
No patients and public involved.
Results
As of 10 January 2021, Hong Kong has reported 9243 laboratory-confirmed COVID-19 cases in a series of local epidemic waves (figure 1A). In response to the surges of cases, the government introduced a package of PHSMs which seemed to have suppressed the transmission of COVID-19 with broadly similar physical distancing interventions across the epidemic waves (online supplemental appendix table S1). The PHSMs applied in Hong Kong included suspending schools, restricting public gathering, requiring restaurants to operate at reduced capacity and for shorter hours, closing bars, nightclubs and karaoke centres, allowing civil servants to WFH, mandating mask-wearing in public areas and so on. The daily reported case numbers had returned to a low level within 2–3 months since the earliest surge of cases in each epidemic wave (figure 1A). In Hong Kong, all laboratory-confirmed cases were isolated until recovery (defined by two consecutive negative PCR tests and/or positive IgG antibody titre), and their close contacts were traced and placed in designated quarantine facilities for 14 days after their last exposure to the confirmed case.17
Figure 1.
(A) Laboratory-confirmed COVID-19 cases in Hong Kong by date of reporting as of 10 January 2021. The shaded areas in yellow indicate the implementation of work-from-home policy for civil servants. The pink area indicates the time periods adopting the mandatory masks policy in public places. The red and blue lines represent the closure of bars and the closure of schools, respectively. (B) Measures of personal hygiene practices against COVID-19 among Hong Kong adults overlaid on the daily numbers of confirmed COVID-19 cases by date of reporting. (C) Measures of physical distancing behaviours against COVID-19 among Hong Kong adults overlaid on the daily numbers of confirmed COVID-19 cases by date of reporting. Percentages indicate weighted proportions of respondents who adopted the specific behaviour to prevent contracting COVID-19 in the past week. Starting from May, questions about hand hygiene practice were specifically asked for immediate actions after certain behaviours, such as going outside and touching common objects. The shaded areas in Panels B and C indicate the time periods selected for analysis of the survey data in the June–July wave (blue) and the November–December wave (red).
In total we interviewed 31 332 participants in the 40 surveys (online supplemental appendix table S3) after excluding individuals due to invalid/non-residential phone numbers, unreachable/busy line/blocking/answering device/language problem, refusal/interruption/inability to participate (online supplemental appendix table S3). Here we focused on behavioural changes among participants in response to the surge of COVID-19 cases in June–July and November–December 2020 (figure 1). While a high coverage of face mask use and optimal hand hygiene practices remained throughout (figure 1B, online supplemental appendix table S4), several types of physical distancing behaviour in the respondents changed following the reported case numbers of COVID-19 in Hong Kong over the two epidemic waves (figure 1C, online supplemental appendix table S4).
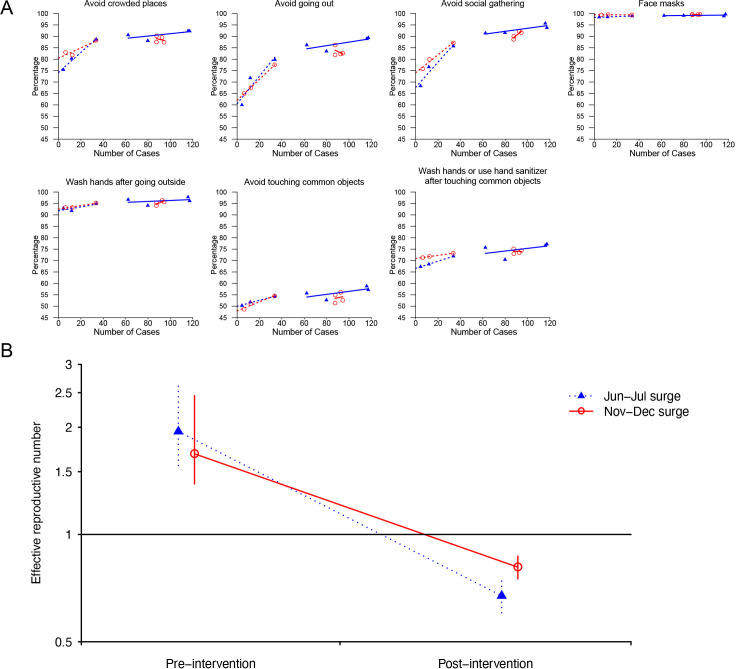
We observed that the reported percentages of voluntary avoidance behaviours, that is, avoiding crowded places or going out, among the survey respondents increased with the notified COVID-19 cases numbers before implementation of the PHSMs during the two consecutive waves. However, a negative correlation was indicated between the reported voluntary avoidance behaviours and the weekly COVID-19 cases and during the post-intervention period in the November–December wave, in comparison with the positive association shown in the June–July wave (figure 2A). Compliance with avoiding social gathering (a regulated avoidance behaviour) was found to increase consistently with the reported case numbers both before and after the PHSMs. We estimated that the average was 1.95 (95% CI: 1.56 to 2.62) and 0.67 (95% CI: 0.60 to 0.75) for the pre-intervention and post-intervention periods, respectively, in the June–July wave, while the estimates were 1.68 (95% CI: 1.39 to 2.45) and 0.81 (95% CI: 0.75 to 0.87) during the November–December wave (figure 2B).
Figure 2.
(A) Seven reported avoidance behaviours in the surveys plotted against the number of confirmed cases reported. Percentages indicate the weighted proportions of survey respondents who adopted the specific behaviour in the past week to prevent contracting COVID-19. The triangles and blue line represent the June–July wave, and the circles and red line represent the November–December wave. Dotted lines represent pre-intervention and solid lines represent post-intervention. (B) The average effective reproduction number estimated for 2 weeks before the work-from-home announcement and the second and third weeks after the work-from-home announcement during the June–July and November–December waves, excluding the 7 days immediately after the work-from-home announcement. The triangles and blue dotted line represent the June–July wave, and the circles and red solid line represent the November–December wave.
Discussion
From the population-based surveys, we observed a declined adherence to voluntary avoidance behaviours but not regulated avoidance behaviours following the implementation of the PHSMs in response to the increased COVID-19 case numbers in Hong Kong population over two consecutive COVID-19 epidemic waves.
Our study illustrated the issue of pandemic fatigue in a place implementing intense PHSMs over multiple epidemic waves of COVID-19. The population-based longitudinal questionnaire surveys involved more than 30 000 participants showed the behavioural characteristics of the adult population in Hong Kong. The random digital-dialling sampling approaches in the surveys minimised the selection bias from the surveyors. The weekly surveys well covered the periods when the PHSMs were implemented and the evolution of the COVID-19 epidemics.
The attenuated impact of PHSMs in suppressing COVID-19 transmission in November–December 2020 in Hong Kong might be related to the reduced motivation to follow the recommended physical distancing behaviours when the public was requested to maintain high compliance with the PHSMs over a prolonged period of time. Pandemic fatigue might be attributable to various underlying factors, such as negative psychological impact of the continuous strict PHSMs, prolonged financial stress caused by loss of working hours and weakening of government credibility and so on.20 21 Additional PHSMs or other pharmaceutical interventions may be needed to suppress future surges in cases, especially with increasing risk of introduction of the more transmissible SARS-CoV-2 variants (eg, B.1.1.7, B.1.351, P.1) into Hong Kong.
Balancing individual rights and social interests is the biggest challenge to implement population-based PHSMs over a long period given the need to reduce the health impact of COVID-19 and the need from the public to return to normal life.10 22 Clear, concise, respectful communication with the public together with a feasible execution plan might be helpful to reduce the pandemic fatigue.10 Further research should be carried out to identify the social, physical and psychological factors potentially associated with the protective behaviours against the pandemic and to assess the effectiveness of the measures targeting the individual factors.
A limitation of our study is that we did not allow for analysis of individual PHSMs (listed in online supplemental appendix table S1), or account for minor variations in the implementation of the measures in different time periods. However, the avoidance behaviours reported by survey respondents provided a general reflection of the fatigue with the largely similar PHSMs in Hong Kong population over the two epidemic waves studied. While the November–December wave occurred when the weather was slightly cooler than the June–July, environmental factors might not be major transmission drivers for COVID-19 transmission.23 A second limitation is that the self-reported behaviours in our surveys might be subject to various reporting biases. Nevertheless, the reduced impact of these same PHSMs on transmission appeared to be evident from our comparative analysis of the two surges in daily case numbers in the same population (figure 2B).
Conclusions
This study used the population-based cross-sectional survey data and the estimated effective reproduction number to highlight the pandemic fatigue with voluntary avoidance behaviours over two consecutive epidemic waves of COVID-19 in Hong Kong. The potential impact from population behavioural changes needs to be considered in implementing non-pharmaceutical interventions to control the COVID-19 pandemic.
Acknowledgments
No writing assistance was provided in the preparation of the manuscript. The authors thank Tiffany Ng and Julie Au for technical assistance.
Footnotes
GML and BJC contributed equally.
Contributors: All authors meet the ICMJE criteria for authorship. HG, ZD, SS, PW, GL and BJC designed the study. HG, ZD, TKT and PW contributed to conduct the data analysis. HG, ZD, PW, GL and BJC interpreted the results. JX, QL and BJC conceived the telephone surveys. HG drafted the manuscript. All authors reviewed and approved the manuscript. PW is responsible for the overall content as guarantor.
Funding: This project was supported by the Health and Medical Research Fund (grant no. COVID190118), Food and Health Bureau and the Theme-based Research Scheme (Project No. T11-712/19-N) of the Research Grants Council, the Government of the Hong Kong Special Administrative Region. The weekly telephone surveys were supported by the Government of the Hong Kong Special Administrative Region.
Competing interests: GL and BJC are supported by the AIR@innoHK program of the Innovation and Technology Commission of the Hong Kong SAR Government. BJC consults for Roche, Sanofi Pasteur, GSK and Moderna. The authors report no other potential conflicts of interest.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants. Our study has been approved by the Institutional Review Board of The University of Hong Kong/Hospital Authority Hong Kong West Cluster (HKU/HA HKW IRB) (UW 20-095). Participants gave informed consent to participate in the study before taking part.
References
- 1.Hu B, Guo H, Zhou P, et al. Characteristics of SARS-CoV-2 and COVID-19. Nat Rev Microbiol 2021;19:141–54. 10.1038/s41579-020-00459-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brauner JM, Mindermann S, Sharma M, et al. Inferring the effectiveness of government interventions against COVID-19. Science 2021;371 10.1126/science.abd9338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.The World Health Organization . Coronavirus disease (COVID-19): small public gatherings, 2020. Available: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/coronavirus-disease-covid-19-small-public-gatherings [Accessed 22 Oct 2021].
- 4.Chu DK, Akl EA, Duda S, et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet 2020;395:1973–87. 10.1016/S0140-6736(20)31142-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Haug N, Geyrhofer L, Londei A, et al. Ranking the effectiveness of worldwide COVID-19 government interventions. Nat Hum Behav 2020;4:1303–12. 10.1038/s41562-020-01009-0 [DOI] [PubMed] [Google Scholar]
- 6.Mendez-Brito A, El Bcheraoui C, Pozo-Martin F. Systematic review of empirical studies comparing the effectiveness of non-pharmaceutical interventions against COVID-19. J Infect 2021;83:281–93. 10.1016/j.jinf.2021.06.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aldarhami A, Bazaid AS, Althomali OW, et al. Public Perceptions and Commitment to Social Distancing "Staying-at-Home" During COVID-19 Pandemic: A National Survey in Saudi Arabia. Int J Gen Med 2020;13:677–86. 10.2147/IJGM.S269716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Park CL, Russell BS, Fendrich M, et al. Americans' COVID-19 stress, coping, and adherence to CDC guidelines. J Gen Intern Med 2020;35:2296–303. 10.1007/s11606-020-05898-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Expectations, reference points, and compliance with COVID-19 social distancing measures. Available: https://www.nber.org/papers/w26916 [Accessed 2 Feb 2021]. [DOI] [PMC free article] [PubMed]
- 10.The World Health Organization . Pandemic fatigue - Reinvigorating the public to prevent COVID-19. Available: https://apps.who.int/iris/bitstream/handle/10665/337574/WHO-EURO-2020-1573-41324-56242-eng.pdf?sequence=1&isAllowed=y [Accessed 13 Jan 2021].
- 11.Chang SL, Harding N, Zachreson C, et al. Modelling transmission and control of the COVID-19 pandemic in Australia. Nat Commun 2020;11:5710. 10.1038/s41467-020-19393-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rypdal K, Bianchi FM, Rypdal M. Intervention fatigue is the primary cause of strong secondary waves in the COVID-19 pandemic. Int J Environ Res Public Health 2020;17 10.3390/ijerph17249592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kan Z, Kwan M-P, Huang J, et al. Comparing the space-time patterns of high-risk areas in different waves of COVID-19 in Hong Kong. Trans GIS 2021 10.1111/tgis.12800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chan W-M, Ip JD, Chu AW-H, et al. Phylogenomic analysis of COVID-19 summer and winter outbreaks in Hong Kong: an observational study. Lancet Reg Health West Pac 2021;10:100130. 10.1016/j.lanwpc.2021.100130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Charan J, Biswas T. How to calculate sample size for different study designs in medical research? Indian J Psychol Med 2013;35:121–6. 10.4103/0253-7176.116232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kadam P, Bhalerao S. Sample size calculation. Int J Ayurveda Res 2010;1:55–7. 10.4103/0974-7788.59946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cowling BJ, Ali ST, Ng TWY, et al. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: an observational study. Lancet Public Health 2020;5:e279–88. 10.1016/S2468-2667(20)30090-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tsang TK, Wu P, Lau EHY, et al. Accounting for imported cases in estimating the time-varying reproductive number of coronavirus disease 2019 in Hong Kong. J Infect Dis 2021;224:783–7. 10.1093/infdis/jiab299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Islam N, Sharp SJ, Chowell G, et al. Physical distancing interventions and incidence of coronavirus disease 2019: natural experiment in 149 countries. BMJ 2020;370:m2743. 10.1136/bmj.m2743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hu Y. Intersecting ethnic and native-migrant inequalities in the economic impact of the COVID-19 pandemic in the UK. Res Soc Stratif Mobil 2020;68:100528. 10.1016/j.rssm.2020.100528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hartley K, Jarvis DSL. Policymaking in a low-trust state: legitimacy, state capacity, and responses to COVID-19 in Hong Kong. Policy and Society 2020;39:403–23. 10.1080/14494035.2020.1783791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Habersaat KB, Betsch C, Danchin M, et al. Ten considerations for effectively managing the COVID-19 transition. Nat Hum Behav 2020;4:677–87. 10.1038/s41562-020-0906-x [DOI] [PubMed] [Google Scholar]
- 23.Sehra ST, Salciccioli JD, Wiebe DJ, et al. Maximum daily temperature, precipitation, ultraviolet light, and rates of transmission of severe acute respiratory syndrome coronavirus 2 in the United States. Clin Infect Dis 2020;71:2482–7. 10.1093/cid/ciaa681 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-055909supp001.pdf (256.8KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.