Abstract
Introduction and importance
Chyle leak is the leakage of milk-like triglyceride-rich lymphatic fluid from the lymphatic system to the peritoneal cavity. The incidence of chyle leak after radical gastrectomy is very low.
Case presentation
A 77-year-old female presented with complaints of decreased appetite and weight loss for six months. Upper gastrointestinal endoscopy showed a polypoidal growth along the greater curvature and the histopathological report of the biopsy taken showed high-grade tubular adenoma with high-grade dysplasia. The patient underwent pylorus-preserving gastrectomy with D1 lymphadenectomy. Postoperatively, after initiation of the oral diet, the abdominal drain started draining milky white fluid, which was rich in triglyceride. The patient was managed conservatively with nil per oral, total parenteral nutrition, and somatostatin analogue.
Clinical discussion
The appearance of milky, nonpurulent fluid in abdominal drain concurrent with the initiation of oral feeding is characteristic of postoperative chyle leak. In our case, we managed the case successfully over a few days with total parenteral nutrition, nil per oral status, and somatostatin analogue.
Conclusion
The incidence of chyle leak after gastrectomy is low, if it occurs it prolongs the hospital stay. Higher age, female gender, and early enteral feeding have been seen as the risk factors for chyle leak. Conservative treatment is effective and is the treatment of choice.
Keywords: Chyle leak, Pylorus preserving gastrectomy, D1 lymphadenectomy, Total parenteral nutrition, Case report
Highlights
-
•
Chyloperitoneum is the leakage of milk-like triglyceride-rich lymphatic fluid from lymphatic system to the peritoneal cavity.
-
•
Post-operative chyle leak increases with extensive intraoperative dissection
-
•
Higher age, female gender and early enteral feeding have been seen as risk factor for chylous ascites.
-
•
Total parenteral nutrition, somatostatin analogues, paracentesis along with low fat diet are curable in most of the cases.
1. Introduction
Chyle leak is defined as the leakage of milk-like triglyceride-rich lymphatic fluid from the lymphatic system to the peritoneal cavity [1]. The incidence of chyle leak after oncological surgery is approximately 7.4% [2]. The incidence of chyle leak after gastrectomy with D1–2 dissection is reported as 1.99%, however, D3–4 lymphadenectomy is associated with a higher incidence of lymphorrhea ranging up to 6.3% [3], indicating that extensive lymph node dissection leads to a higher incidence of chylous leak. There have been few cases associated with D1 dissection [4]. In most patients, conservative treatment is recommended that includes paracentesis, total parenteral nutrition (TPN), a medium-chain triglyceride (MCT) based diet, and somatostatin analogue. Surgery is the last treatment option only when the conservative treatment fails. Here, we present a case of chyle leak after pylorus-preserving gastrectomy with D1+ lymph node dissection successfully managed with total parenteral nutrition, somatostatin analogue and medium-chain triglyceride (MCT) based low-fat diet. This is the first reported case of chyle leak amongst 26 gastrectomies performed in the last two years at our center. This case report has been reported in line with the SCARE Criteria [5].
2. Presentation of the case
A 77-year-old female presented with complaints of decreased appetite and significant weight loss for 6 months. She also complained of abdominal pain for a similar duration in the epigastric region, on and off with no aggravating or relieving factors. She was hypertensive and under medications for the past 6 years. She had undergone an open appendectomy and bilateral tubal ligation 14 years back. On general examination, she was of average built with body mass index (BMI) of 21 kg/m2 and Eastern Cooperative Oncology Group (ECOG) performance status of 2.
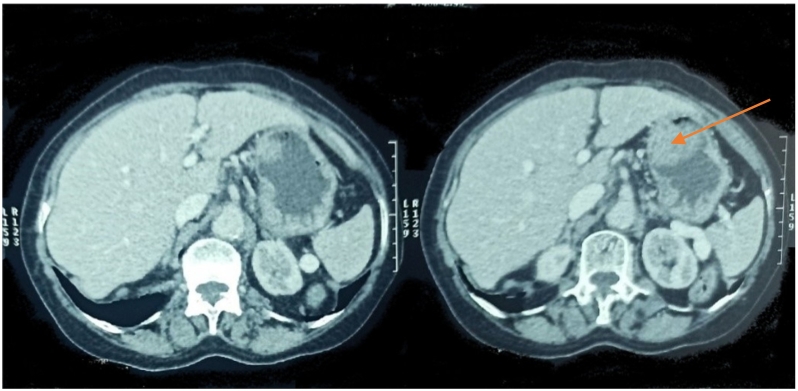
The transabdominal ultrasound done at the other center showed a heterogeneously echogenic lesion along the lesser curvature of the stomach protruding into the lumen. Upper gastrointestinal endoscopy showed pedunculated mass arising from the lesser curvature of the stomach. Endoscopic biopsy report of the mass showed tubular adenoma with high-grade dysplasia. Contrast-enhanced computer tomography (CECT) abdomen and pelvis showed a large (5.4 × 4.2 cm) moderately enhancing intraluminal pedunculated polypoidal lesion in the lesser curvature in the mid-body region with no surrounding fat strandings and enlarged perigastric lymph nodes. The patient was optimized for surgery and later underwent pylorus-preserving gastrectomy with D1 lymphadenectomy and gastrojejunostomy (Fig. 1).
Fig. 1.
CECT showing pedunculated polypoidal lesion arising from the lesser curvature (red arrow). (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
Intraoperatively, there was a firm, pedunculated, polypoidal intraluminal growth approximately 6 × 5 × 5 cm size arising from the lesser curvature of the stomach with no adhesions, ascites, or omental deposits. A twenty-eight French (Fr) drain was kept near the gastrojejunostomy site. The histopathological examination (HPE) report of the surgical specimen revealed mixed carcinoma (tubulopapillary), well-differentiated extending up to muscular mucosae with no perineural and lymphovascular invasion, harvested 23 lymph nodes all were free of tumor and TNM staging pT1aN0(AJCC8th edition 2020) (Fig. 2, Fig. 3).
Fig. 2.
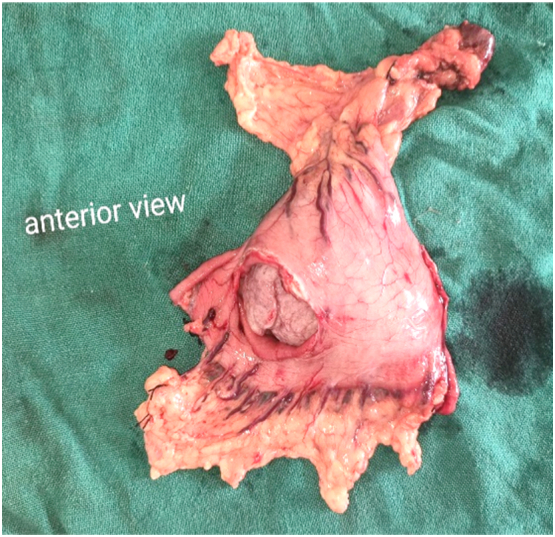
Surgical specimen of pylorus preserving gastrectomy with tumor mass within it.
Fig. 3.
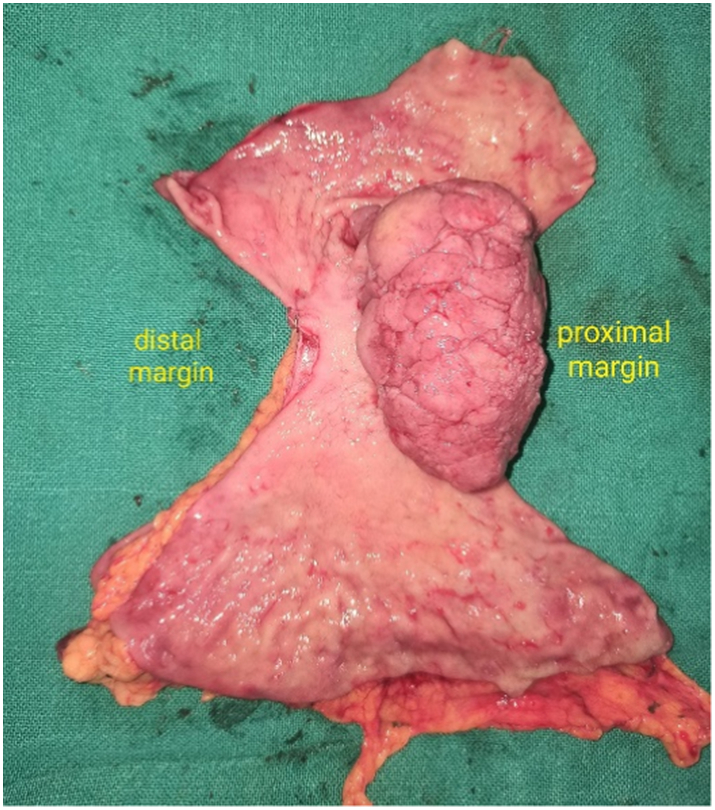
Pedunculated exophytic mass seen arising from the lesser curvature with adequate proximal and distal resection margins.
Postoperatively, the nasogastric (NG) tube was removed on the 3rd postoperative day (POD 3) and the patient was given sips followed by clear liquids. The abdominal drain output was 100 ml, serosanguinous on the first post-operative day and later it became serous and the amount was in decreasing trend till 4th POD. However, on the 5th POD, after the soft diet was started, the drain color changed to milky white, and the amount increased to 300 ml over twenty-four hours. The triglyceride level of the drain content was found to be 229 mg/dl. The patient was discharged with the abdominal drain and kept on a low-fat diet.
On follow-up after a week, the abdominal drain was draining about 400-500 ml of chyle with some discharge from the midline wound. The patient gradually developed generalized weakness and anorexia for which she was re-admitted to the surgical ward. She was kept nil per os (NPO) and total parenteral nutrition (TPN) was started via central venous route, along with subcutaneous injection octreotide 100 μg thrice daily. After five days, the drain amount decreased gradually and was nil for over twenty-four hours (Fig. 4), and hence fat-free oral liquid diet was restarted. TPN was stopped once the oral intake was adequate. Ultrasound of the abdomen repeated on the seventh day showed no intraabdominal collection and the patient was discharged with advice for a very low-fat diet. On follow-up after 2 weeks, she recovered well and was symptom-free.
Fig. 4.
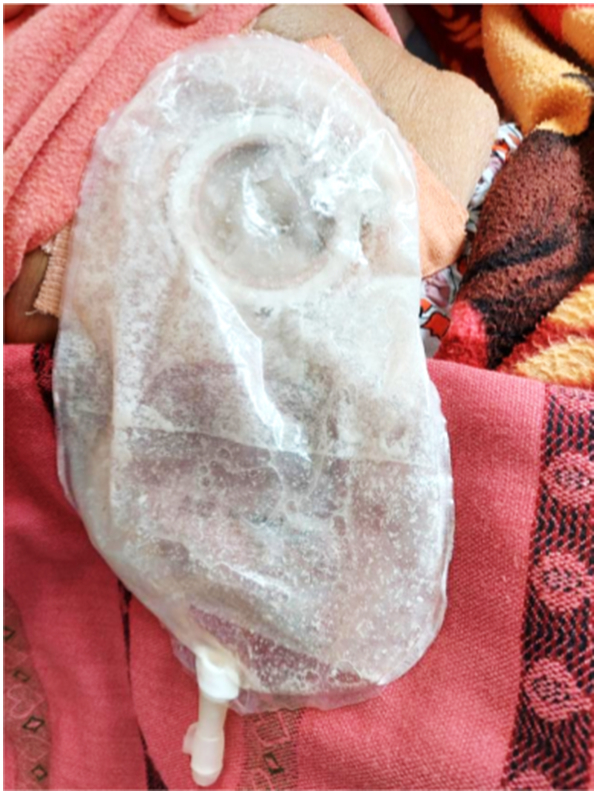
Drain bag containing a minimal amount of chylous content following five days of treatment.
3. Discussion
Postoperative chyle leak is a common phenomenon in abdominal surgery that causes significant prolongation of hospital length of stay and thus increases healthcare costs. Incidence of chylous ascites is 11.7% after gastrectomy with D3 lymph node dissection [6], while it was as low as 0.3% to 0.7% [6], [7] after laparoscopic gastrectomy with D1 or D2 lymph node dissection indication that extensive lymph node dissection was associated with a higher incidence of postoperative chylous ascites.
The postoperative chyle leak is commonly believed to be the result of direct trauma to the cisterna chyli or one of its branches with subsequent lymphatic leakage into the peritoneal cavity. [8] Extent of lymph node dissection [8], higher age [9], female gender [10], number of lymph nodes removed [11], early enteral feeding [10], and poor performance status are a few established risk factors for postoperative chyle leak.
Diagnosis is based mainly on clinical parameters. The appearance of milky, nonpurulent fluid in drains concurrent with initiation of oral feeding is characteristic of postoperative chylous ascites. A culture-negative chylomicron-rich fluid with triglyceride levels of 110 mg/dl or 1.2 mmol/L is suggestive of chylous ascites. In patients where drains are removed, the presence of abdominal pain, distention, fever, and leukocytosis should warn the attending surgeon about the probability of intraabdominal collection. Lymphangiography and lymphoscintigraphy are the modalities that can detect fistulas or leakage from lymphatic channels and can also determine the patency of the thoracic duct [12].
Conservative treatment is successful in the majority of cases of postoperative chylous ascites and it has a good prognosis. However, it may cause significant morbidity including malnutrition, dehydration, immunosuppression, or septic complications due to superinfection [8]. Once diagnosed, total parenteral nutrition and nil per oral status provided a high efficacy in resolving chylous ascites. The total parenteral nutrition can reduce the accumulation of intra-abdominal lymph fluid and can simultaneously supply the necessary nutrition. The addition of somatostatin analogue example octreotide may be an option to shorten leakage time. [8]. Paracentesis can also be done however there is loss of albumin and other nutrients causing electrolyte imbalance and hypoproteinemia. If conservative treatment fails the patient may be considered for open surgery. Laparotomy may be performed for fistula closure, bowel resection, or insertion of a peritoneovenous shunt [12].
In our case, we managed the case successfully with total parenteral nutrition, nil per oral status, and somatostatin analogue for postoperative chylous ascites following pylorus-preserving gastrectomy with D1 dissection. The patient recovered well within a week and was discharged in good health.
4. Conclusion
Postoperative chyle leak is a rare complication following radical gastrectomy and its incidence increases with extensive lymphatic dissection. Higher age, female gender, early enteral nutrition, and poor performance status are other risk factors associated with it. Conservative treatment in the form of total parenteral nutrition, somatostatin analogues, paracentesis along a low-fat diet is curable in most cases.
Ethical approval
Not required.
Funding
None.
Guarantor
Aliza Hamal.
Registration of research studies
Not applicable.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
CRediT authorship contribution statement
Aliza Hamal, Sushil Gyawali, Ramesh Singh Bhandari: Study concept, Data collection, and surgical therapy for the patient.
Aliza Hamal, Sushil Gyawali: Writing- original draft preparation.
Aliza Hamal, Deepak Sharma, Romi Dahal: Editing and writing.
Ramesh Singh Bhandari and Sumita Pradhan: senior author and manuscript reviewer.
All the authors read and approved the final manuscript.
Declaration of competing interest
None.
Acknowledgment
None.
References
- 1.Lv S., Wang Q., Zhao W., Han L., Wang Q., Batchu N., et al. A review of the postoperative lymphatic leakage. Oncotarget [Internet] 2017 Apr 20;8(40):69062–69075. doi: 10.18632/oncotarget.17297. https://www.oncotarget.com/article/17297/text/ Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kaas R., Rustman L.D., Zoetmulder F.A.N. Chylous ascites after oncological abdominal surgery: incidence and treatment. Eur. J Surg Oncol [Internet] 2001 Mar 1;27(2):187–189. doi: 10.1053/ejso.2000.1088. https://www.ejso.com/article/S0748-7983(00)91088-6/abstract Available from. [DOI] [PubMed] [Google Scholar]
- 3.Surgical Case Reports | Full Text [Internet] 2021 Nov 21. Successful treatment of hepatic lymphorrhea by percutaneous transhepatic lymphangiography followed by sclerotherapy using OK-432.https://surgicalcasereports.springeropen.com/articles/10.1186/s40792-019-0761-z Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.SpringerLink [Internet] 2021 Nov 21. Treatment and prevention of lymphorrhea after radical gastrectomy of gastric cancer.https://link.springer.com/article/10.1007%2Fs00432-008-0495-y Available from. [DOI] [PubMed] [Google Scholar]
- 5.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., Thoma A., et al. The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int J Surg [Internet] 2020 Dec 1;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. https://www.sciencedirect.com/science/article/pii/S1743919120307718 Available from. [DOI] [PubMed] [Google Scholar]
- 6.Yol S., Bostanci E.B., Ozogul Y., Ulas M., Akoglu M. A rare complication of D3 dissection for gastric carcinoma: chyloperitoneum. Gastric Cancer [Internet] 2005 Feb 1;8(1):35–38. doi: 10.1007/s10120-004-0312-5. cited 2021 Nov 21. Available from. [DOI] [PubMed] [Google Scholar]
- 7.Bo T., Zhihong P., Peiwu Y., Feng Q., Ziqiang W., Yan S., et al. General complications following laparoscopic-assisted gastrectomy and analysis of techniques to manage them. Surg Endosc [Internet] 2009 Aug 1;23(8):1860–1865. doi: 10.1007/s00464-008-0312-3. cited 2021 Nov 21. Available from. [DOI] [PubMed] [Google Scholar]
- 8.Weniger M., D’Haese J.G., Angele M.K., Kleespies A., Werner J., Hartwig W. Treatment options for chylous ascites after major abdominal surgery: a systematic review. Am J Surg [Internet] 2016 Jan 1;211(1):206–213. doi: 10.1016/j.amjsurg.2015.04.012. https://www.americanjournalofsurgery.com/article/S0002-9610(15)00327-X/fulltext#relatedArticles Available from. [DOI] [PubMed] [Google Scholar]
- 9.Baek S.-J., et al. Incidence and risk factors of chylous ascites after colorectal cancer surgery. Am. J. Surg. 2013 Oct 1;206(4):555–559. doi: 10.1016/j.amjsurg.2013.01.033. https://www.americanjournalofsurgery.com/article/S0002-9610(13)00229-8/fulltext Available from. [DOI] [PubMed] [Google Scholar]
- 10.Gaag NA van der, et al. Chylous ascites after pancreaticoduodenectomy: introduction of a grading system. J. Am. Coll. Surg. 2008 Nov 1;207(5):751–757. doi: 10.1016/j.jamcollsurg.2008.07.007. https://www.journalacs.org/article/S1072-7515(08)01004-1/fulltext Available from. [DOI] [PubMed] [Google Scholar]
- 11.Assumpcao L., Cameron J.L., Wolfgang C.L., Edil B., Choti M.A., Herman J.M., et al. Incidence and management of chyle leaks following pancreatic resection: a high volume single-center institutional experience. J. Gastrointest. Surg. [Internet] 2008 Nov 1;12(11):1915–1923. doi: 10.1007/s11605-008-0619-3. cited 2021 Nov 21. Available from. [DOI] [PubMed] [Google Scholar]
- 12.Bhardwaj R., Vaziri H., Gautam A., Ballesteros E., Karimeddini D., Wu G.Y. Chylous ascites: a review of pathogenesis, diagnosis and treatment. J. Clin. Transl. Hepatol. [Internet] 2017 Dec 4;6(1):105–113. doi: 10.14218/JCTH.2017.00035. http://www.xiahepublishing.com/ArticleFullText.aspx?sid=2&jid=1&id=10.14218%2fJCTH.2017.00035 Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]