Abstract
Trauma is often viewed as an individual or interpersonal issue. This paper expands the definition of trauma to include the impact collective and structural elements on health and well-being. The need for a trauma-informed response is demonstrated, with instruction as to how to implement this type of care in order to resist re-traumatization. Three examples from healthcare settings across the nation are provided, to demonstrate the ways in which organizations are bringing forward this patient-centered, trauma-informed approach to care.
Keywords: stress disorders, post-traumatic, patient-centered care, vulnerable populations
Introduction
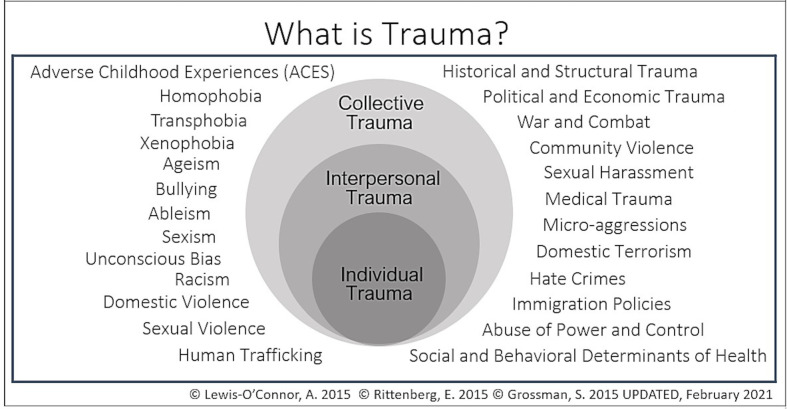
Trauma, whether physical or psychosocial, has profound effects on health, and influences how people engage with their healthcare services. Healthcare providers and anchor systems are beginning to explore trauma through a more inclusive lens. However, traditional definitions of trauma as a purely physical phenomenon are still prevalent, such as in the case of the Coalition for National Trauma Research website that defines trauma as: “traumatic injury includes that from vehicular collisions, falls from heights, gunshot wounds and burns…”.1 If healthcare providers and healthcare systems are to break down the structural barriers that negatively impact and promote the under-resourcing and marginalization of populations and communities, trauma must be considered in a broader, more multi-layered definition. To account for this, “trauma” in this manuscript is defined as both individual and interpersonal as well as collective and structural (See figure 1). A glossary of definitions of trauma is shown in box 1.
Figure 1.
This image describes the many levels on which trauma is experienced. Traumatic experiences can occur on individual, interpersonal, and/or collective levels; these levels do not necessarily occur in isolation, but rather as intersectional and dynamic layers.
Box 1. Glossary of definitions of trauma.
Individual trauma—an event, series of events, or set of circumstances, that is experienced by an individual as physically or emotionally harmful or life threatening and has lasting adverse effects on the individual’s functioning and mental, physical, social, emotional, or spiritual well-being.10
Interpersonal trauma—adverse childhood events, child maltreatment, domestic and sexual violence, human trafficking, elder abuse, etc.
Collective trauma—cultural, historical, social, political, and structural traumas (ie, racism, bias, stigma, oppression, genocide) that impact individuals and communities across generations.
Individual and interpersonal trauma
Negative experiences in childhood are highly prevalent, including abuse and neglect, witnessing domestic abuse, parental mental illness, and parental imprisonment yet continue to be considered taboo subjects in society, and often, in medical encounters during a trauma evaluation. Seminal work by Felitti et al demonstrated the impact of adverse childhood experiences (ACEs) in adult health outcomes, in which more than half of 17,000 adult patients surveyed reported having an experience in childhood of at least one ACE, with one-fourth reporting two or more ACEs.2 The greater the number of ACES reported, the more prevalent were adult diseases including ischemic heart disease, cancer, chronic lung disease, skeletal fractures, and liver disease.2 Further large-scale replication, including a CDC review of Behavioral Risk Factor Surveillance System data from 2011 to 2014, shows the same prevalence and dose response effect.3 4
Collective/structural trauma
Healthcare services themselves can unintentionally traumatize or re-traumatize people. This is especially true in communities that have been hurt by histories of, as well as current medical institutional practices that propagate and maintain collective traumas. In order to respond effectively to trauma of all types, healthcare providers need to understand trauma as beyond the personal and include community and societal trauma. As pointed out by Kelly-Irving and Delpierre, when one makes ACES/trauma an individual problem, there is risk of placing the onus of responsibility on individuals solely to act to rectify their trauma, instead of on the cause or source of the trauma.5 Collective trauma is, therefore, a collective responsibility. The collective impacts of trauma can be traced in ACEs data as well: Merrick et al found that women, Native American and Black people, and the category “other racial/ethnic group” were more likely to experience four or more ACEs than males and whites. Higher ACE scores were reported by Black, Latinx, and LGBTQIA+ communities, with the highest ACEs in multiracial (2.5) and bisexual respondents (3.1).3
A collective approach to understanding trauma gives the ability to look upstream at the root causes of ACEs, to see trauma as embedded in collective and structural elements of history, systemic oppressions, and racism. The Philadelphia Urban ACE Study, the first to address the intersection of ACEs and social determinants of health, attended to this by including the addition of collective traumas such as seeing or hearing someone being beaten, stabbed, or shot; bullying; and racism and discrimination, finding that 40.5% of Philadelphia adult respondents, coming from diverse race and class backgrounds, reported these types of ACEs.6 Ellis and Dietz also called for examining the root causes of toxic stress and childhood adversity and sought to address this by creating a model for building community resilience.7
In the patient care setting, particularly in trauma or other disciplines that care for individuals from oppressed populations, it is common to encounter patients who carry histories of individual, interpersonal, and/or collective trauma. These experiences impact both patient health and the ways in which they engage with their healthcare. Given that there is neither time nor precedent to understand ACE and trauma history before trauma evaluation, it is imperative that care providers recognize the impact of the unspoken traumas that are brought to the clinical encounter. Box 2 shows a short exemplary list of experiences patients may find difficult due to ACE or trauma histories:
Box 2. Patient experiences as related to ACE/trauma histories.
Individual: Lack of privacy, removal of clothing, overall vulnerability including physical positions, fear of waking during surgery, loss of control inherent in surgical procedure/s.
Interpersonal: Physical touch, procedures of all kinds are not routine for patients, being unsure what is said about them or done to them during surgery, fear of surgical mistakes, confirmation of a poor diagnosis or outcome.
Collective: Care provider and/or institutional bias, discrimination or racism, stigma leading to worse outcomes, neglectful care.
Using trauma-informed care in a universal precaution method can address these concerns. One practical solution is to ask patients broad trauma inquiry such as “Have you had any life experiences that you feel have impacted your health and well-being?”8 Questions like these allow surgical teams and providers to understand not only acute traumas present, the potential causal interpersonal aspects of this trauma, but also the effects of collective/structural trauma.9 The Substance Abuse and Mental Health Administration (SAMHSA) summarizes this type of trauma-informed proactive approach as the “4 R’s” wherein providers seek to Realize how trauma affects the individuals and communities they serve in their practice, Recognize the symptoms of trauma in their patients, Respond to patients in a trauma-informed way, and Resist Re-traumatization of patients.10 This stance allows care providers to move beyond the conception of “what’s wrong with you” when assessing patients, to the broader question “what happened to you and how has what happened affected you?” This advances providers’ ability to pro-actively address trauma histories by asking patients what would be helpful before healthcare encounters, and to collaborate with healthcare teams to offer referrals or resources as needed.11 This universal trauma approach allows providers to address “hidden” traumas (undisclosed or unaccounted), as well as those that are rooted in collective and structural trauma.12
Toxic stress, historical trauma, and epigenetics
Toxic stress can come from trauma at all levels, and stress can come from all levels of trauma. For example, a person can experience relative resiliency in their personal lives, while still experiencing intergenerational trauma due to historical occurrences such as slavery or genocide. The stress response is understood as both psychological and physiologic. When the body’s fight or flight, or adrenergic, response is activated, stress hormones like epinephrine and cortisol are released. Over time, when the stressful stimulus is removed, individuals return to homeostasis and the stress response subsides. However, for individuals who live in situations of chronic stress, it can become difficult to return to homeostasis. This experience of living with chronic stress and constant, low level activation of the adrenergic system creates changes in the brain, learning, and responses, and creates altered reactions to stress in the future. Known as toxic stress, this response has been linked to poor health outcomes, increased incidence of psychiatric and substance abuse disorders, and decreased immune responses.13
It is relatively easy for physicians to imagine that toxic stress can lead to altered physiology later in life. It is less intuitive to understand how toxic stress, which is an experience, is passed through to the next generation. A relatively new field of study, epigenetics, seeks to identify how experiences and stress shape the way DNA is transcribed over generations.14 The same stress hormones that cause individual toxic stress also affect DNA methylation and the formation of histones, so although the genetic code itself is not changed, its transcription is.15 When an individual experiences toxic stress, these responses can be passed on through generations.16 Although the specific genes affected and how stress affects gene transcription is still largely not understood, the downstream clinical effects of epigenetic changes are apparent in a number of clinical settings, particularly in behavioral health.17
Trauma-informed practices in the provider–patient relationship
Traumatic stress happens when individuals are unable to recover or feel safe after the body’s autonomic system is activated. As described previously, patients may arrive with complaints related to the physiologic effects of toxic stress, and/or to traumas of individual, interpersonal, or communal origins. It is critical then, that provider–patient interactions do not re-traumatize individuals who have likely just had an autonomic response from their injury or illness. Providers should seek to understand what types of trauma are present—individual, interpersonal and/or communal. It is important that providers know the traumas that are prevalent in their patient’s community and the historical trauma that this community may have faced, such as a history of poverty and violence, or for populations, impacts of slavery, racism, genocide, or displacement.
As a provider continues to evolve in their understanding of the community they serve, they can learn to recognize trauma in the patients they care for. Trauma may come in the form of anxiety, lack of eye contact, or hesitancy to participate in the healthcare encounter. It can also come in less obvious ways, like poor compliance with the medical care plan or pain out of proportion to injury or examination. As trauma-informed providers, we understand that these reactions are the result of previous trauma. To reduce re-traumatization in the provider–patient relationship, one must build trust and mutual respect, responding to patients in a trauma-informed way. One can protect privacy in the physical examination, and in the medical record by asking consent throughout the process; asking or telling a patient when you need to touch them and why, remaining at eye level with the patient, and explaining and asking input on the plan of care. While much of this may seem intuitive, these practices have been shown to be lacking in many healthcare interactions.18
Building a trauma-informed organization
Understanding trauma-informed principles and the effects of ACEs on the provider–patient relationship is not enough; it is critical to implement trauma-informed practices throughout the institution. Physicians are in a position within hospitals, educational institutions, and medical systems to build an entire system that is trauma-informed.19 This can be accomplished through formal teaching and training, mentoring, and through the establishment of trauma-informed institutional structures. Nursing literature has informed the field on trauma-informed care for decades.20–22 A synthesis of the nursing literature on TIC revealed the following themes: trauma screening and patient disclosure, provider–patient relationships, minimizing distress and maximizing autonomy, multidisciplinary collaboration and referrals, and advancement of TIC in diverse settings.
The Substance Abuse and Mental Health Administration (SAMHSHA) has outlined 10 domains of trauma-informed organizational leadership to assist with this.10 It is critical when considering these domains that this is considered a process that organizations are constantly striving to improve, rather than a “one-and-done” checklist. In the next section, we highlight how three institutions have promoted trauma-informed care to improve and transform services at interpersonal and structural levels.
Example 1: The Center for Health Resilience of MetroHealth in Cleveland, Ohio
The Center for Health Resilience at MetroHealth in Cleveland, Ohio expands the understanding of how trauma intersects and impacts the health of communities, systems and people. The Center uses Resilience in Action, which promotes connection through an innovative and proprietary Recovery Coaching model.
This model comprised three main elements: needs assessment, resource navigation, and care coordination. Recovery Coaches are trained in building rapport, empowering and providing ongoing support, education, and resources to the patients and families they serve. Peer support has been shown to benefit the patient receiving support and also the peer supporter.23
The Center’s training and education efforts have focused on embedding trauma-competent programming into multiple specialties. By focusing training and education on physicians, nursing, and administrative staff, they have successfully identified champions who believe in the intrinsic value of recovery services. The team identifies areas of importance and relevance to specific departments and has demonstrated impact on patient outcomes based on interaction with services.24
Published findings have shown exposure to these recovery focused services is associated with higher overall patient-reported care ratings (modeled after the Hospital Consumer Assessment of Healthcare Providers and Systems survey), lower rates of emergency department misuse, higher rates of patient-perceived ability to recover, and higher rates of patient perception of physician competence and responsiveness.25 26 These findings have earned recognition throughout this health system and nationally.
Example 2: Oregon Health Science University (OHSU) in Portland, Oregon
Oregon Health and Science University (OHSU), in Portland, Oregon recognizes the impact of trauma on patients and to surgical residents. Surgical residents are exposed to traumatic experiences and stressors throughout their residency.27 One study of surgical residents found that 22% screened positive for PTSD and another 35% screened in the “at-risk” range suggesting that residents as well as patients may benefit from a systematic response to the high prevalence of trauma.27 Despite evidence that trauma-informed care (TIC) can benefit patients and providers, the integration of TIC training into the residency curricula has been slow.28
OHSU used a novel, interdisciplinary, peer-to-peer training model to address to the prevalence of these types of trauma in medicine. The objective of the training was to improve surgical resident physician understanding of the effects of trauma and introduce TIC principles and practices with the ultimate goal of improving patient care by increasing the awareness of the trauma that shows up in patients and providers. A cohort of four surgical and one psychiatry residents participated in a series of trainings addressing the principles of TIC and TIC curriculum development based on the text Training for Change: Transforming Systems to be Trauma-Informed, Culturally Responsive and Neuroscientifically Focused.29 This group then developed a TIC curriculum for surgical interns using a peer-to-peer teaching model culminating in three 30 min sessions delivered during protected surgery didactic time. The surgery TIC curriculum uses case-based learning, reflection, and collaborative small group work to describe the neurobiology of trauma and fear, discuss provider experiences of vicarious trauma, and identify trauma-informed patient care practices.
Surgical residents’ learning was assessed with pre-training and post-training surveys. Results quantified by post-training assessments showed marked improvement in skills in TIC after the trainings. This training has impacted day-to-day care from a bottom-up approach, as the newly trained interns report feeling empowered to broach difficult situations and generate discussion with their seniors and team members using a TIC lens. The training is ongoing and the curriculum continues to adapt and improve since its inception 3 years ago.
Example 3: Rutgers New Jersey Medical School
At Rutgers New Jersey Medical School in New Jersey providers and residents were trained in depth in TIC, with follow-up provided for residents in the form of TIC-informed peer support. The TIC program was brought to this school as part of the launch of a hospital-based violence intervention program (HVIP). The trauma service elected to train physicians, advanced practice providers, and HVIP staff together in a trauma-informed care course. This three-part course was offered by a local TIC training program being employed in pediatric settings at regional medical centers as part of a SAMSHA-funded program to train providers in TIC principles.
Trauma-informed care principles, adverse childhood experiences, and the science of epigenetics and toxic stress were introduced via didactic teaching. Follow-up sessions focused on building provider team trust, sharing ideas for how to implement trauma-informed practices as a team, and discussing what trauma-informed patient interactions would look like in clinical settings. In the third session, a trainer accompanied the team on rounds, observed interactions with patients, and gave immediate feedback about how to make the interaction more trauma informed.
Providers feedback reported that training helped them better care for patients, better manage their own life stress and trauma, and practice better self-care. The main feedback was that training should be provided to all who manage trauma patients, most particularly the nursing and residency staff.
To implement this, ongoing trauma-informed care teaching was applied to the residency program. In this model, residents attend a department-wide grand rounds presentation on trauma-informed care at the beginning of the academic year. At the onset of their trauma rotation, the second interactive lecture is given as part of the curriculum. Finally, a trainer attends rounds with the trauma team and provides specific feedback to residents on their patient interactions in the week following the second didactic lecture.
The program implementation has been well received and was easy to integrate into the trauma rotations. The interactions observed by attending staff between patients and residents has been improved. As medical providers seek to further implement this programming hospital-wide, we are eager to understand if these programs can translate to improved patient outcomes.
Conclusion
As we constantly seek to improve the care of our patients, it is important to realize that trauma impacts all individuals, patients and providers alike, across the lifespan and across generations. Awareness of the breadth and depth of trauma and its impact on healthcare outcomes is critical to improving the health of all patients, as well as those providing care. Using the framework above, we can improve ourselves and our provider practices, and we can also advocate for and build organizations that account for trauma. As SAMHSA notes, “everyone has a role to play in a trauma-informed approach (p.15).”10 This will improve outcomes and create healthier communities in which we and our patients will live, work, and play.
Acknowledgments
SG acknowledges Eve Rittenberg, MD for editorial assistance for this manuscript, as well as for collaboration in bringing trauma-informed care forward, along with AL-O'C, NP, and Nomi Levy-Carrick, MD, MPhil. She has no competing interests. SH acknowledges Dr. Heather Vallier, MD, founder of Trauma Recovery Services, at the MetroHealth System; as well as Katie Kurtz, LISW-S and Mary Breslin, MPH for support with organizational collaboration and research. She has no competing interests.
Footnotes
Contributors: SG assumed the primary writing responsibility for the manuscript content, references, tables and figures, final formatting and references and review overall and wrote the introduction, and individual/interpersonal and collective/structural trauma sections of the manuscript. SB wrote the sections on toxic stress, historical trauma, and epigenetics; trauma-informed practices in the provider–patient relationship; and building a trauma-informed organization and the section entitled: Rutgers New Jersey Medical School. SH wrote the section entitled: The Center for Health Resilience of MetroHealth in Cleveland, Ohio. HB, JS, and L-YW wrote the section entitled: Oregon Health Science University (OHSU) in Portland, Oregon. AL-O'C provided overall comments on the manuscript and relevant information on nursing literature. SB served as the senior author and advised SG throughout the entire process, contributing to the content in the manuscript. All authors reviewed and contributed to the final manuscript.
Funding: HB was awarded a $7000 educational mini grant through OHSU to fund projects related to trauma informed care. Grant award number: none.
Disclaimer: The study sponsor(s) had no role in the study design; in the collection, analysis, and interpretation of the data; in the writing of the report; and in the decision to submit the paper for publication.
Competing interests: The curriculum used in the OHSU study included text from the book Training for Change: Transforming Systems to be Trauma-Informed, Culturally Responsive, and Neuroscientifically Focused written by Dr Alisha Moreland. This is the only related disclosure.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study does not involve human participants.
References
- 1.CNTR . Coalition for National Trauma Research. 2021. https://www.east.org/content/documents/cntr_infopiece.pdf.
- 2.Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med 1998;14:245–58. 10.1016/s0749-3797(98)00017-8 [DOI] [PubMed] [Google Scholar]
- 3.Merrick MT, Ford DC, Ports KA, Guinn AS. Prevalence of adverse childhood experiences from the 2011–2014 behavioral risk factor surveillance system in 23 states. JAMA Pediatr 2018;172:1038–44. 10.1001/jamapediatrics.2018.2537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Merrick MT, Ford DC, Ports KA, Guinn AS, Chen J, Klevens J, Metzler M, Jones CM, Simon TR, Daniel VM, et al. Vital Signs: Estimated Proportion of Adult Health Problems Attributable to Adverse Childhood Experiences and Implications for Prevention – 25 States, 2015–2017. MMWR Morb Mortal Wkly Rep 2019;68:999–1005. 10.15585/mmwr.mm6844e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kelly-Irving M, Delpierre C. A critique of the adverse childhood experiences framework in epidemiology and public health: uses and misuses. Social Policy and Society 2019;18:445–56. 10.1017/S1474746419000101 [DOI] [Google Scholar]
- 6.Cronholm PF, Forke CM, Wade R, Bair-Merritt MH, Davis M, Harkins-Schwarz M, Pachter LM, Fein JA. Adverse childhood experiences: expanding the concept of adversity. Am J Prev Med 2015;49:354–61. 10.1016/j.amepre.2015.02.001 [DOI] [PubMed] [Google Scholar]
- 7.Ellis WR, Dietz WH. A new framework for addressing adverse childhood and community experiences: the building community resilience model. Acad Pediatr 2017;17:S86–93. 10.1016/j.acap.2016.12.011 [DOI] [PubMed] [Google Scholar]
- 8.Lewis-O'Connor A, Warren A, Lee JV, Levy-Carrick N, Grossman S, Chadwick M, Stoklosa H, Rittenberg E. The state of the science on trauma inquiry. Womens Health 2019;15:174550651986123. 10.1177/1745506519861234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oral R, Ramirez M, Coohey C, Nakada S, Walz A, Kuntz A, Benoit J, Peek-Asa C. Adverse childhood experiences and trauma informed care: the future of health care. Pediatr Res 2016;79:227–33. 10.1038/pr.2015.197 [DOI] [PubMed] [Google Scholar]
- 10.Substance Abuse and Mental Health Services Administration . SAMHSA’s Concept of trauma and guidance for a trauma-informed approach. HHS Publication No. (SMA). Rockville, MD: Substance Abuse and Mental Health Services Administration, 2014:14–4884. [Google Scholar]
- 11.Fischer KR, Bakes KM, Corbin TJ, Fein JA, Harris EJ, James TL, Melzer-Lange MD. Trauma-informed care for violently injured patients in the emergency department. Ann Emerg Med 2019;73:193–202. 10.1016/j.annemergmed.2018.10.018 [DOI] [PubMed] [Google Scholar]
- 12.Racine N, Killam T, Madigan S. Trauma-informed care as a universal precaution: beyond the adverse childhood experiences questionnaire. JAMA Pediatr 2020;174. [DOI] [PubMed] [Google Scholar]
- 13.Shonkoff JP, Garner AS, Siegel BS, Dobbins MI, Earls MF, Garner AS, McGuinn L, Pascoe J. Committee on Psychosocial Aspects of Child and Family Health Committee on Early Childhood, Adoption, and Dependent Care Section on Developmental and Behavioral Pediatrics . The lifelong effects of early childhood adversity and toxic stress. Pediatrics 2012;129:e232–46. 10.1542/peds.2011-2663 [DOI] [PubMed] [Google Scholar]
- 14.Tammen SA, Friso S, Choi S-W. Epigenetics: the link between nature and nurture. Mol Aspects Med 2013;34:753–64. 10.1016/j.mam.2012.07.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ryan J, Chaudieu I, Ancelin M-L, Saffery R. Biological underpinnings of trauma and post-traumatic stress disorder: focusing on genetics and epigenetics. Epigenomics 2016;8:1553–69. 10.2217/epi-2016-0083 [DOI] [PubMed] [Google Scholar]
- 16.Ridout KK, Khan M, Ridout SJ. Adverse childhood experiences run deep: toxic early life stress, telomeres, and mitochondrial DNA copy number, the biological markers of cumulative stress. Bioessays 2018;40:e1800077:1800077. 10.1002/bies.201800077 [DOI] [PubMed] [Google Scholar]
- 17.Daskalakis NP, Rijal CM, King C, Huckins LM, Ressler KJ. Recent genetics and epigenetics approaches to PTSD. Curr Psychiatry Rep 2018;20:30. 10.1007/s11920-018-0898-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stevens NR, Ziadni MS, Lillis TA, Gerhart J, Baker C, Hobfoll SE. Perceived lack of training moderates relationship between healthcare providers' personality and sense of efficacy in trauma-informed care. Anxiety Stress Coping 2019;32:679–93. 10.1080/10615806.2019.1645835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Clements AD, Haas B, Cyphers NA, Hoots V, Barnet J. Creating a communitywide system of trauma-informed care. Prog Community Health Partnersh 2020;14:499–507. 10.1353/cpr.2020.0055 [DOI] [PubMed] [Google Scholar]
- 20.Muskett C. Trauma-informed care. Int J Ment Health Nurs 2014;23:51–9. [DOI] [PubMed] [Google Scholar]
- 21.Stokes Y, Jacob J-D, Gifford W, Squires J, Vandyk A. Exploring nurses' knowledge and experiences related to trauma-informed care. Glob Qual Nurs Res 2017;4:233339361773451. 10.1177/2333393617734510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fleishman J, Kamsky H, Sundborg S. Trauma-informed nursing practice. Online J Issues Nurs 2019;24. 10.3912/OJIN.Vol24No02Man03 [DOI] [Google Scholar]
- 23.DeMario B, Kalina MJ, Truong E, Hendrickson S, Tseng ES, Claridge JA, Vallier H, Ho VP. Downstream hospital system effects of a comprehensive trauma recovery services program. J Trauma Acute Care Surg 2020;89:1177–82. 10.1097/TA.0000000000002872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Simske NM, Rivera T, Breslin MA, Hendrickson SB, Simpson M, Kalina M, Ho VP, Vallier HA. Implementing psychosocial programming at a level 1 trauma center: results from a 5-year period. Trauma Surg Acute Care Open 2020;5:e000363. 10.1136/tsaco-2019-000363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Simske NM, Benedick A, Rascoe AS, Hendrickson SB, Vallier HA. Patient satisfaction is improved with exposure to trauma recovery services. J Am Acad Orthop Surg 2020;28:597–605. 10.5435/JAAOS-D-19-00266 [DOI] [PubMed] [Google Scholar]
- 26.Simske NM, Breslin MA, Hendrickson SB, York KP, Vallier HA. Implementing recovery resources in trauma care: impact and implications. OTA Int 2019;2:e045. 10.1097/OI9.0000000000000045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jackson T, Provencio A, Bentley-Kumar K, Pearcy C, Cook T, McLean K, Morgan J, Haque Y, Agrawal V, Bankhead-Kendall B, et al. Discussion of: "PTSD and surgical residents: everybody hurts … sometimes". Am J Surg 2017;214:1125–6. 10.1016/j.amjsurg.2017.10.014 [DOI] [PubMed] [Google Scholar]
- 28.Green BL, Saunders PA, Power E, Dass-Brailsford P, Schelbert KB, Giller E, Wissow L, Hurtado-de-Mendoza A, Mete M. Trauma-informed medical care: CME communication training for primary care providers. Fam Med 2015;47:7-14. [PMC free article] [PubMed] [Google Scholar]
- 29.Moreland-Capuia A. Training for change: transforming systems to be trauma-informed, culturally responsive and neuroscientifically focused. 1 edn. Cham, Switzerland: Springer International Publishing, 2019. [Google Scholar]