Abstract
Background/objective
Low physical activity is a risk factor for cardiovascular disease (CVD) and all-cause morbidity and mortality. CVD alters heart rate variability (HRV). Interestingly, HRV can improve after exercise training. Therefore, this study aimed to examine the effect of whole-body high-intensity interval training (whole-body HIIT) on HRV in low physical activity adults.
Methods
Twenty-one low physical activity young adults were randomly assigned into two groups: whole-body HIIT (n = 10, females = 2/males = 8, age 22 ± 0.8 years, BMI 19.5 ± 1.0 kg/m2) and control (n = 11, females = 4/males = 7, age 21.7 ± 0.8 years, BMI 19.8 ± 0.9 kg/m2). A 6-week exercise program (3 days per week) consisting of 10 min of whole-body HIIT (burpees, mountain climbers, jumping jacks, and squats) at their maximal effort was administered. Baseline and post-training HRV (time domain: SDNN and RMSSD, frequency domain: LF, HF, and LF/HF ratio) and resting heart rate (HRrest) were recorded.
Results
The time domain parameter increased significantly in the whole-body HIIT group (SDNN; 50.95 ± 37.17 vs. 73.40 ± 40.70 ms, p < 0.05, RMSSD; 54.45 ± 56.04 vs. 81.26 ± 60.14 ms, p < 0.05). HRrest decreased significantly following training (73.94 ± 13.2 vs. 66.1 ± 10.8 bpm, p < 0.05). However, there were no significant differences in all frequency-domain parameters.
Conclusion
Six weeks of whole-body HIIT improved cardiovascular autonomic function in insufficiently active adults. Thus, whole-body HIIT might be considered an alternative exercise for reducing the risk of CVD.
Keywords: Cardiovascular disease, High-intensity interval training, Physical activity
1. Introduction
The global prevalence of physical inactivity is high and increasing.1 Insufficient physical activity is associated with non-communicable diseases (NCDs) and other adverse effects on health, such as depression, osteoporosis, and sarcopenia.2,3 Moreover, NCDs have become the leading cause of death worldwide.4 Consequently, to reduce the risk of morbidity and mortality caused by NCDs, the physical activity recommendations guideline has been announced by the World Health Organization.5 Adults should achieve at least 150–300 min of moderate-intensity aerobic physical activity per week or vigorous-intensity aerobic physical activity for at least 75–150 min per week and perform muscle-strengthening activities at least 2 days per week.5 However, almost 30% of the worldwide population have been reported to be physically inactive.1 The major barrier is the lack of time.6 High-intensity interval training (HIIT) is a time-efficient exercise which consists of repeated, short, and intense periods of exercise interspersed by periods of rest or low-intensity exercise.7 Several studies have confirmed that HIIT provides similar or superior benefits to moderate-intensity continuous training (MICT).8, 9, 10 Furthermore, it helps to improve cardiovascular fitness,8, 9, 10 which is a predictor of cardiovascular health.11
One of the physiological parameters that could assess the risk of cardiovascular disease using a non-invasive method is heart rate variability (HRV).12 HRV is the variation in the time interval between consecutive heartbeats.13 It is considered as a marker of neurocardiac function14 and reflects the balance between sympathetic and parasympathetic nervous system.15 Interestingly, there is a relationship between CVD mortality and HRV, with CVD mortality being lower when HRV is increases.16 Moreover, there is an evidence demonstrated that autonomic dysfunction (sympathetic activation and vagal withdrawal) can be found in patients with CVD.17 It is well known that exercise training associated with a reduction in cardiovascular mortality and the risk of developing cardiovascular disease.18 Importantly, HRV can improve following exercise training.19 HRV, including time domain (LF and HF, LH/HF)20,21 and frequency domain (RMSSD), improves following HIIT.20 It could be assumed that HIT improved cardiac vagal activity after HIIT.22
However, HIIT protocols have some important limitations. The majority of these are laboratory or gym-based, which require specific equipment such as treadmills and cycle ergometers. These may not be easily available for general population.23 Additionally, the HIIT protocol may be impractical and too hard to adopt as a regular exercise by individuals with insufficient physical activity. As the HIIT protocol requires more time exercise per week than the exercise recommendations for vigorous-intensity aerobic exercise. Whole-body HIIT is a HIIT protocol that does not require any equipment and uses the bodyweight as resistance.24 Previous studies have demonstrated various health benefits following whole-body HIIT, including improved muscular endurance, muscular strength, and maximal oxygen consumption (VO2max).25, 26, 27 However, there has been no evidence indicating the changes in HRV following whole-body HIIT. Therefore, the main purpose of this study was to determine the effect of whole-body HIIT on HRV in low physical activity people. We hypothesized that whole-body HIIT would lead to an improvement in HRV in insufficiently active adults.
2. Methods
2.1. Participants
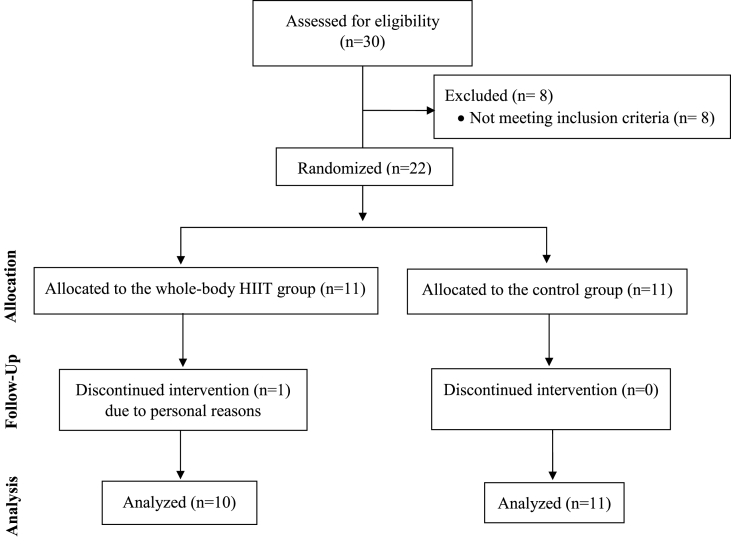
Twenty-two healthy, insufficiently active adults (aged 18–40 years and physical activity levels <600 MET minutes/week) were recruited via advertisements in the university. The participants were randomized into whole-body HIIT and control groups (Fig. 1). The research assistant performed randomization by using sealed envelopes to generate the list, which was concealed by the principal investigator. The sample size for each group was calculated based on the findings of a previous study.20 A minimum of 11 participants were required in each group in order to detect differences in the change in HRV between the groups with a power of 95%, α = 0.05, and effect size of ƒ = 0.48. One participant from the whole-body HIIT group dropped out of the study because of personal reasons (see Table 1 for participant demographic characteristics). Exclusion criteria were classification as moderate- or high physical activity according to the International Physical Activity Questionnaire (IPAQ),28 contraindications to exercise as determined using a physical activity readiness questionnaire (PAR-Q) (Thai version),29 any musculoskeletal disorders in the 6 months prior to the study or other serious underlying diseases. All participants were asked not to change their physical activity patterns and to record their activities (type and duration) in a log, everyday throughout the study. The aim, protocol, and potential risks from the study were explained to the participants, both verbally and in writing, before they provided informed consent. The study received university ethics approval (COA No.076/2563).
Fig. 1.
Study flow diagram.
Table 1.
Participants’ characteristics.
| Whole-body HIIT (n = 10) | Control (n = 11) | |
|---|---|---|
| Sex (male/female) | 8/2 | 7/4 |
| Age (y) | 22.0 ± 0.8 | 21.7 ± 0.8 |
| Height (cm) | 164.0 ± 6.8 | 161.4 ± 7.5 |
| Weight (kg) | 52.7 ± 5.9 | 51.6 ± 5.9 |
| BMI (kg·m2) | 19.5 ± 1.0 | 19.8 ± 0.9 |
| Physical activity level (MET-min·week-1) | 313.6 ± 117.8 | 345.2 ± 137.5 |
Values are presented as mean ± SD. Physical activity level was estimated using the IPAQ.
BMI: body mass index, HIIT: high-intensity interval training, IPAQ: International Physical Activity Questionnaire, MET: Metabolic equivalent.
2.2. Experimental protocols
2.2.1. HRV measurement
Baseline HRV was recorded 24–48 h before starting the training program. Participants were instructed not to perform strenuous exercise or drink caffeine or alcohol the day prior to HRV measurement. The Polar V800 heart rate monitor (Polar Electro Oy Inc., Kempele, Finland) was used to measure RR intervals. The device has been validated for HRV studies previously.30,31 For each training session, HRV measurement was taken in the morning (8:00 to 9:00 a.m.) for 20 min in the supine position, with controlled breathing at 12 breaths/min using a metronome in a quiet room with limited visual stimulation. Participants were asked to maintain silence and stillness throughout the test. Post-training HRV was evaluated 24 h after the last training session. RR interval data were downloaded to a computer through the Polar Flow web service, and HRV analysis (time domain: SDNN and RMSSD; and frequency domain: LF, HF, and LF/HF ratio) was performed using Kubios HRV software version 3.4.1 (Biosignal Analysis and Medical Imaging Group, University of Eastern Finland, Kuopio, Finland). RR intervals were visually identified, and adjacent beats were corrected when necessary. The first 5 min of the 20 min were cut off to avoid noisy data due to the change in the body position (from standing to supine position), and the subsequent artifact-free 5-min recording was selected according to the standards of HRV.13
2.2.2. Whole-body HIIT program
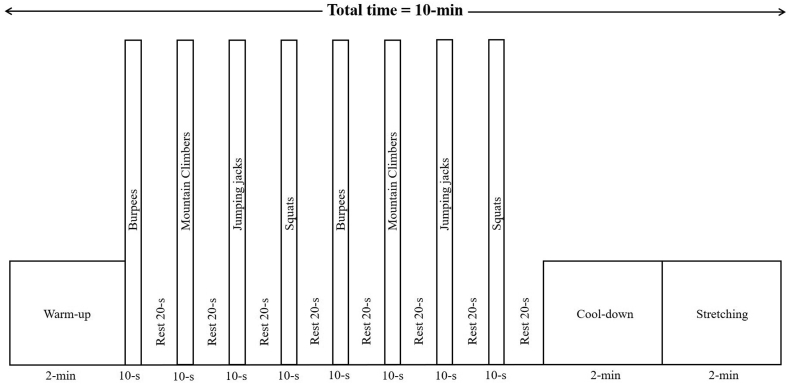
Participants in the training group completed 18 sessions (exercise 3 days per week for 6 weeks with one-on-one training) using the protocol modified from McRae et al.25 The whole-body HIIT program consisted of four exercises: burpees, mountain climbers, jumping jacks, and squats. Participants were requested to perform these exercises in this order and on all-out intensity for 10 s, interspersed by 20 s of jogging at low intensity (self-paced). All exercises were repeated twice (Fig. 2). In addition, 2 min of warm-up, cool-down with jogging at low intensity (self-paced), and leg stretching were performed. During all sessions, participants were supervised by the researchers and received strong verbal encouragement to ensure that they performed with their maximal effort. Moreover, the number of repetitions on the 1st, 8th, and 16th sessions were recorded to guarantee that the participants engaged in an all-out effort in which the number of repetitions did not reduce throughout the study. The heart rate during exercise was recorded using the Polar H10 heart rate sensor (Polar Electro Oy Inc., Kempele, Finland). Age-predicted maximal heart rate was calculated using Tanaka's equation (208 - 0.7 x age).32 The rating of perceived exertion (RPE) using the Borg scale (Thai version)33 and the affective response to exercise34 were recorded pre-and immediately post-exercise at every session. Additionally, all training sessions were performed at the exercise physiology laboratory and all participants performed the training sessions at the same time of the day (3:00 to 6:00 p.m.).
Fig. 2.
Whole-body HIIT program plan.
2.2.3. Statistical analysis
All results are presented as mean ± SD. An independent sample t-test was used to determine the differences between baseline characteristics of the two groups. Two-way repeated-measures ANOVA was used to examine differences between the groups for changes in HRV (time × group), affective response, and RPE (time × session). In case of significant results, post-hoc comparisons were performed using Fisher's least significant difference (LSD) test. Cohen's d calculation for effect sizes were reported. The significance level was set at p < 0.05.
3. Results
3.1. Training characteristics
The mean adherence to whole-body HIIT sessions was 100%. All training sessions were well-tolerated by participants, and there were no adverse events during the training sessions. The average RPE for whole-body HIIT are shown in Table 2. The highest RPE was found in the 1st session (16.0 ± 1.9, corresponding to “hard to very hard”). Thereafter, RPE reduced significantly in the 3rd, 9th, and 18th session (p < 0.001). Additionally, the RPE over 18 training sessions corresponded to somewhat hard (13.1 ± 2.4). Moreover, there was no significant difference in the affective response between pre- and post-training in the 1st, 3rd, 9th, and 18th session.
Table 2.
RPE and the affective response after the 1st, 3rd, 9th, and 18th session.
| RPE |
Affect response |
|||||||
|---|---|---|---|---|---|---|---|---|
| 1 | 3 | 9 | 18 | 1 | 3 | 9 | 18 | |
| Pre-training | 7.6 ± 1.5 | 7.2 ± 1.1 | 7.6 ± 1.4 | 6.8 ± 0.8 | 0.5 ± 1.1 | 1.1 ± 1.1 | 0.2 ± 0.4 | 0.2 ± 0.8 |
| Post-training | 16.0 ± 1.9∗ | 13.8 ± 2.6∗† | 12.9 ± 2.7∗†‡ | 11.5 ± 2.2∗†‡§ | −0.3 ± 1.3 | −0.2 ± 1.5 | 0.2 ± 0.6 | 0.7 ± 0.9 |
Values are presented as mean ± S D. RPE: rating of perceived exertion.
∗p < 0.001 from pre-training, †p < 0.001 from the 1st session, ‡p < 0.05 from the 3rd session, §p < 0.05 from the 9th session.
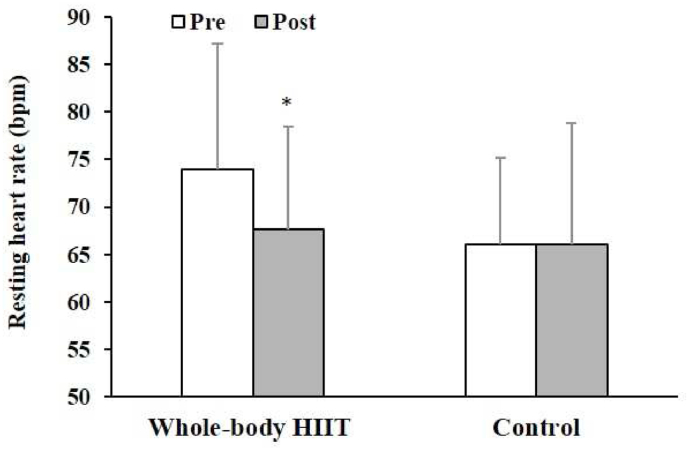
There was a significant decrease in the resting heart rate in the whole-body HIIT group, which is shown in Fig. 3 (pre-training 73.9 ± 13.2 bpm, post-training 66.1 ± 10.8 bpm, p = 0.046). In addition, the peak heart rate during whole-body HIIT intervention reached on average ∼84–95% of maximal heart rate.
Fig. 3.
Resting heart rate in the whole-body HIIT and control groups. Data are represented as mean ± SD (n = 10 in the whole-body HIIT group, n = 11 in the control group). ∗p < 0.05 for the group × time interaction effect.
3.2. HRV
There was a greater increase in SDNN in the whole-body HIIT group (50.95 ± 37.17 vs. 73.40 ± 40.70 ms) compared to the control group (55.07 ± 25.14 vs. 54.43 ± 25.96 ms; group × time interaction effect: p = 0.001, d = 0.43). RMSSD also increased in the former after training (54.45 ± 56.04 vs. 81.26 ± 60.14 ms) compared to the control group (57.62 ± 30.61 vs. 59.59 ± 31.63 ms; group × time interaction effect: p = 0.019, d = 0.26) (Table 3). However, no significant changes were observed in any frequency domain parameters from pre-to post-training.
Table 3.
HRV variables in the time and frequency domains.
| Variables | Whole-body HIIT (n = 10) |
Control (n = 11) |
||
|---|---|---|---|---|
| Pre | Post | Pre | Post | |
| Time domain | ||||
| SDNN (ms) | 50.95 ± 37.17 | 73.40 ± 40.70∗∗ | 55.07 ± 25.14 | 54.43 ± 25.96 |
| RMSSD (ms) | 54.45 ± 56.04 | 81.26 ± 60.14∗ | 57.62 ± 30.61 | 59.59 ± 31.63 |
| Frequency domain | ||||
| LF (ms2) | 662.43 ± 459.25 | 1318.59 ± 1666.54 | 954.94 ± 1067.34 | 819.33 ± 829.23 |
| LF (n.u.) | 37.95 ± 27.54 | 32.94 ± 24.35 | 33.08 ± 24.91 | 28.95 ± 19.71 |
| HF (ms2) | 2767.93 ± 5028.54 | 4051.48 ± 4984.48 | 2404.96 ± 2820.61 | 2449.66 ± 2398.32 |
| HF (n.u.) | 61.67 ± 27.64 | 66.59 ± 24.23 | 66.77 ± 24.81 | 70.82 ± 19.60 |
| LF/HF ratio | 2.20 ± 4.93 | 1.38 ± 3.08 | 1.02 ± 1.44 | 0.65 ± 0.82 |
Values are presented as mean ± SD.
HF: high-frequency band (0.15–0.4 Hz), HRV: heart rate variability, LF: low-frequency band (0.04–0.15 Hz), LF/HF: ratio of LF to HF power, RMSSD: root mean square of successive RR interval difference, SDNN: standard deviation of NN interval.
∗∗p = 0.001 for the time × group interaction effect.
∗p = 0.019 for the time × group interaction effect.
4. Discussion
To the best of our knowledge, this is the first study investigating the effect of whole-body HIIT on HRV in adults participating in low levels of physical activity. The main findings were that 6 weeks of whole-body HIIT significantly increased the time domain variables of HRV (SDNN and RMSSD) and significantly decreased the resting heart rate. However, there was no significant difference in the frequency domain.
These findings are consistent with previous HIIT studies despite the differences in type and duration of exercise protocols. Heydari et al. demonstrated that RMSSD improved following 12 weeks of cycle HIIT (20 min of 8 s sprints and 12 s recovery, 3 times per week) in physically inactive males (d = 0.14).20 Moreover, Piras et al. showed that 3 months training of cycle HIIT (20 min of 1 min sprints and 2 min recovery, 3 times per week) increased SDNN and RMSSD in healthy individuals (d = 0.34 and d = 0.30, respectively).35 It suggests that cycle HIIT and whole-body HIIT can improve SDNN and RMSSD in healthy and physically inactive individuals with a small to medium effect size. However, whole-body HIIT might be time-efficient because the training duration is short, making it more suitable to people who mentioned lack of time as their exercise barrier.
Importantly, SDNN and RMSSD reduction is associated with an increased risk of cardiac mortality and morbidity.36,37 RMSSD is an index that represents vagal tone.38 Previous evidence confirmed that exercise training is effective in improving HRV by reducing the sympathetic activity and increasing the parasympathetic activity,39 which suggests that whole-body HIIT can improve vagal modulation. Moreover, the present study demonstrated a significant reduction in resting heart rate after training. Similar findings were found in numerous exercise training studies.40,41 O'Driscoll et al. also demonstrated that the resting heart rate was reduced significantly after HIIT in physically inactive young adults.42 The mechanisms responsible for decreasing resting heart rate might include the reduction of the intrinsic heart rate and sympathetic tone and an increase in the vagal tone.20 Importantly, increasing the vagal tone might be a potential mechanism of cardioprotection.43
However, this study did not find a significant difference in the frequency domain. This finding is supported by Alansare et al. that reported that the frequency domain did not improve after 2 weeks of cycle HIIT (20 min of 10 s sprints and 50 s recovery, 4 times per week).44 On the other hand, Heydari et al. and Piras et al. have reported a significant improvement in the frequency domain following 12 weeks of cycle HIIT.20,35 Accordingly, Hottenrott et al. suggested that HRV could also be improved after at least 3 months of regular training of moderate intensity and volume.45 The training duration might play an important role in improving the frequency domain of HRV.
Despite the high intensity of whole-body HIIT, a low negative affective response was found after training in the first and third sessions. Astorino et al. suggested that the negative affective response to HIIT can be found in low fitness individuals.46 In this study, the negative affective response to whole-body HIIT was found in the first week of training. In addition, RPE over 18 training sessions corresponds to somewhat hard (RPE 13). Parfitt et al. demonstrated that training at this particular subjective intensity (i.e. RPE 13) was related to long-term exercise adherence,47 thus supporting exercise adoption and adherence to whole-body HIIT in individuals with insufficient physical activity. Importantly, no serious adverse effects were noted during or after whole-body HIIT, indicating that whole-body HIIT is a feasible exercise which could be taken by low physical inactive adults or individuals who define lack of time as the main exercise barrier; however, further studies need to be explored in order to validate whether whole-body HIIT is acceptable in several populations such as inactive children, metabolic syndrome or obese/overweight individuals.
The limitations of this study need to be considered. First, all training sessions were laboratory-based. Thus, the adherence to exercise may not represent the exercise behavior in real life. Further studies are needed to confirm and validate the long-term adherence to whole-body HIIT in non-laboratory-based environment (home or gym). Second, the physical activity levels before and during training were not confirmed by objective measurements. However, all participants maintained their physical activity throughout the 6 weeks of training duration, which was confirmed by the physical activity log. Third, only one health parameter (HRV) has been investigated in the study. Future studies are required to confirm the effects of whole-body HIIT on other health parameters associated with cardiometabolic health, such as blood pressure, insulin sensitivity, VO2max, or muscle/fat mass. Additionally, further studies must be conducted in order to validate whether the benefit or disadvantage can be elicited following whole-body HIIT over more than 6 weeks.
5. Conclusion
This study demonstrated that 6 weeks of whole-body HIIT significantly improves HRV (SDNN, and RMSSD) and reduce the resting heart rate when comparing to a non-exercising control group in insufficiently active adults. Thus, whole-body HIIT provides an effective and manageable exercise alternative to improve cardiovascular autonomic function, which is associated with a reduction of cardiovascular morbidity and mortality.
Author statement
P. Songsorn: Conception and design of study, analysis and interpretation of data, Drafting the manuscript, revising the manuscript critically for important intellectual content. K. Somnarin, S. Jaitan and A. Kupradit: Acquisition of data, analysis and interpretation of data. All authors approved the final manuscript.
Funding/support statement
This study was supported by the Young investigator research grant of the Faculty of Allied Health Sciences, Thammasat University, Thailand (grant number 05/2563).
Declaration of competing interest
The authors have no conflicts of interest relevant to this article.
Acknowledgments
We would like to thank all participants for their time and effort. We acknowledge the Faculty of Allied Health Sciences, Thammasat University, Thailand for the grant.
Contributor Information
Preeyaphorn Songsorn, Email: preeyaphorn.s@allied.tu.ac.th.
Kawinpop Somnarin, Email: kawinpop.som@allied.tu.ac.th.
Supakij Jaitan, Email: supakij.jai@allied.tu.ac.th.
Atcharaphan Kupradit, Email: atcharaphan.kup@allied.tu.ac.th.
References
- 1.Guthold R., Stevens G.A., Riley L.M., Bull F.C. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob Health. 2018;6(10):e1077–e1086. doi: 10.1016/s2214-109x(18)30357-7. [DOI] [PubMed] [Google Scholar]
- 2.Booth F.W., Roberts C.K., Thyfault J.P., Ruegsegger G.N., Toedebusch R.G. Role of inactivity in chronic diseases: evolutionary insight and pathophysiological mechanisms. Physiol Rev. 2017;97(4):1351–1402. doi: 10.1152/physrev.00019.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee I.M., Shiroma E.J., Lobelo F., Puska P., Blair S.N., Katzmarzyk P.T. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012;380(9838):219–229. doi: 10.1016/s0140-6736(12)61031-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.GBD 2015 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1659–1724. doi: 10.1016/s0140-6736(16)31679-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization . World Health Organization; Geneva, Switzerland: 2020. WHO Guidelines on Physical Activity and Sedentary Behaviour. [Google Scholar]
- 6.Booth M.L., Bauman A., Owen N., Gore C.J. Physical activity preferences, preferred sources of assistance, and perceived barriers to increased activity among physically inactive Australians. Prev Med. 1997;26(1):131–137. doi: 10.1006/pmed.1996.9982. [DOI] [PubMed] [Google Scholar]
- 7.Gillen J.B., Gibala M.J. Is high-intensity interval training a time-efficient exercise strategy to improve health and fitness? Appl Physiol Nutr Metabol. 2014;39(3):409–412. doi: 10.1139/apnm-2013-0187. [DOI] [PubMed] [Google Scholar]
- 8.Su L., Fu J., Sun S., et al. Effects of HIIT and MICT on cardiovascular risk factors in adults with overweight and/or obesity: a meta-analysis. PLoS One. 2019;14(1) doi: 10.1371/journal.pone.0210644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sultana R.N., Sabag A., Keating S.E., Johnson N.A. The effect of low-volume high-intensity interval training on body composition and cardiorespiratory fitness: a systematic review and meta-analysis. Sports Med. 2019;49(11):1687–1721. doi: 10.1007/s40279-019-01167-w. [DOI] [PubMed] [Google Scholar]
- 10.Wewege M., van den Berg R., Ward R.E., Keech A. The effects of high-intensity interval training vs. moderate-intensity continuous training on body composition in overweight and obese adults: a systematic review and meta-analysis. Obes Rev. 2017;18(6):635–646. doi: 10.1111/obr.12532. [DOI] [PubMed] [Google Scholar]
- 11.Myers J., Prakash M., Froelicher V., Do D., Partington S., Atwood J.E. Exercise capacity and mortality among men referred for exercise testing. N Engl J Med. 2002;346(11):793–801. doi: 10.1056/NEJMoa011858. [DOI] [PubMed] [Google Scholar]
- 12.Goldenberg I., Goldkorn R., Shlomo N., et al. Heart rate variability for risk assessment of myocardial ischemia in patients without known coronary artery disease: the HRV-DETECT (heart rate variability for the detection of myocardial ischemia) study. J Am Heart Assoc. 2019;8(24) doi: 10.1161/jaha.119.014540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology Heart rate variability: standards of measurement, physiological interpretation and clinical use. Circulation. 1996;93(5):1043–1065. doi: 10.1161/01.CIR.93.5.1043. [DOI] [PubMed] [Google Scholar]
- 14.Shaffer F., McCraty R., Zerr C.L. A healthy heart is not a metronome: an integrative review of the heart's anatomy and heart rate variability. Front Psychol. 2014;5 doi: 10.3389/fpsyg.2014.01040. 1040-1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Singh N., Moneghetti K.J., Christle J.W., Hadley D., Froelicher V., Plews D. Heart rate variability: an old metric with new meaning in the era of using mHealth technologies for health and exercise training guidance. Part Two: prognosis and training. Arrhythmia Electrophysiol Rev. 2018;7(4):247–255. doi: 10.15420/aer.2018.30.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Prinsloo G.E., Rauch H.G., Derman W.E. A brief review and clinical application of heart rate variability biofeedback in sports, exercise, and rehabilitation medicine. Phys. Sportsmed. 2014;42(2):88–99. doi: 10.3810/psm.2014.05.2061. [DOI] [PubMed] [Google Scholar]
- 17.Besnier F., Labrunée M., Pathak A., et al. Exercise training-induced modification in autonomic nervous system: an update for cardiac patients. Ann Phys Rehabil Med. 2017;60(1):27–35. doi: 10.1016/j.rehab.2016.07.002. [DOI] [PubMed] [Google Scholar]
- 18.Nystoriak M.A., Bhatnagar A. Cardiovascular effects and benefits of exercise. Front Cardiovasc Med. 2018;5:135. doi: 10.3389/fcvm.2018.00135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Routledge F.S., Campbell T.S., McFetridge-Durdle J.A., Bacon S.L. Improvements in heart rate variability with exercise therapy. Can J Cardiol. 2010;26(6):303–312. doi: 10.1016/s0828-282x(10)70395-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Heydari M., Boutcher Y.N., Boutcher S.H. High-intensity intermittent exercise and cardiovascular and autonomic function. Clin Auton Res. 2013;23(1):57–65. doi: 10.1007/s10286-012-0179-1. [DOI] [PubMed] [Google Scholar]
- 21.Rakobowchuk M., Harris E., Taylor A., Cubbon R.M., Birch K.M. Moderate and heavy metabolic stress interval training improve arterial stiffness and heart rate dynamics in humans. Eur J Appl Physiol. 2013;113(4):839–849. doi: 10.1007/s00421-012-2486-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kiviniemi A.M., Tulppo M.P., Eskelinen J.J., et al. Autonomic function predicts fitness response to short-term high-intensity interval training. Int J Sports Med. 2015;36(11):915–921. doi: 10.1055/s-0035-1549854. [DOI] [PubMed] [Google Scholar]
- 23.Batacan R.B., Duncan M.J., Dalbo V.J., Tucker P.S., Fenning A.S. Effects of high-intensity interval training on cardiometabolic health: a systematic review and meta-analysis of intervention studies. Br J Sports Med. 2017;51(6):494–503. doi: 10.1136/bjsports-2015-095841. [DOI] [PubMed] [Google Scholar]
- 24.Machado A.F., Baker J.S., Figueira Junior A.J., Bocalini D.S. High-intensity interval training using whole-body exercises: training recommendations and methodological overview. Clin Physiol Funct Imag. 2019;39(6):378–383. doi: 10.1111/cpf.12433. [DOI] [PubMed] [Google Scholar]
- 25.McRae G., Payne A., Zelt J.G., et al. Extremely low volume, whole-body aerobic-resistance training improves aerobic fitness and muscular endurance in females. Appl Physiol Nutr Metabol. 2012;37(6):1124–1131. doi: 10.1139/h2012-093. [DOI] [PubMed] [Google Scholar]
- 26.Myers T.R., Schneider M.G., Schmale M.S., Hazell T.J. Whole-body aerobic resistance training circuit improves aerobic fitness and muscle strength in sedentary young females. J Strength Condit Res. 2015;29(6):1592–1600. doi: 10.1519/jsc.0000000000000790. [DOI] [PubMed] [Google Scholar]
- 27.Schaun G.Z., Pinto S.S., Silva M.R., Dolinski D.B., Alberton C.L. Whole-body high-intensity interval training induce similar cardiorespiratory adaptations compared with traditional high-intensity interval training and moderate-intensity continuous training in healthy men. J Strength Condit Res. 2018;32(10):2730–2742. doi: 10.1519/jsc.0000000000002594. [DOI] [PubMed] [Google Scholar]
- 28.IPAQ Research Committee . 2005. Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire (IPAQ)–short and Long Forms. [Google Scholar]
- 29.Thai Health Literacy Promotion Association . 18 August 2019. Physical Activity Readiness Questionnaire Plus 2019-PAR-Q+ (Thai)http://doh.hpc.go.th/bs/issueDisplay.php?id=186&category=A04&issue=Physical%20Activity [Google Scholar]
- 30.Giles D., Draper N., Neil W. Validity of the Polar V800 heart rate monitor to measure RR intervals at rest. Eur J Appl Physiol. 2016;116(3):563–571. doi: 10.1007/s00421-015-3303-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jinakote M., Pongpanit K. Correlations between change in neural respiratory drive and heart rate variability in patients submitted to open-heart surgery. J Exerc Rehabil. 2019;15(4):616–621. doi: 10.12965/jer.1938230.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tanaka H., Monahan K.D., Seals D.R. Age-predicted maximal heart rate revisited. J Am Coll Cardiol. 2001;37(1):153–156. doi: 10.1016/s0735-1097(00)01054-8. [DOI] [PubMed] [Google Scholar]
- 33.Wongphaet Parit, Jitpraphai Chattaya, Kantaratanakul Visal, Chira-Adisai W. The study of correlation among rate of perceived exertion from translated Borg's scale, intensity of exercise and heart rate. J Thai Rehabil Med. 1998;7(3):121–125. [Google Scholar]
- 34.Hardy C.J., Rejeski W.J. Not what, but how one feels: the measurement of affect during exercise. J Sport Exerc Psychol. 1989;11(3):304. doi: 10.1123/jsep.11.3.304. [DOI] [Google Scholar]
- 35.Piras A., Persiani M., Damiani N., Perazzolo M., Raffi M. Peripheral heart action (PHA) training as a valid substitute to high intensity interval training to improve resting cardiovascular changes and autonomic adaptation. Eur J Appl Physiol. 2015;115(4):763–773. doi: 10.1007/s00421-014-3057-9. [DOI] [PubMed] [Google Scholar]
- 36.Jandackova V.K., Scholes S., Britton A., Steptoe A. Healthy lifestyle and cardiac vagal modulation over 10 years: whitehall II Cohort Study. J Am Heart Assoc. 2019;8(19) doi: 10.1161/JAHA.119.012420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shaffer F., Ginsberg J.P. An overview of heart rate variability metrics and norms. Front Public Health. 2017;5 doi: 10.3389/fpubh.2017.00258. 258-258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Laborde S., Mosley E., Thayer J.F. Heart rate variability and cardiac vagal tone in psychophysiological research - recommendations for experiment planning, data analysis, and data reporting. Front Psychol. 2017;8 doi: 10.3389/fpsyg.2017.00213. 213-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ramírez-Vélez R., Tordecilla-Sanders A., Téllez-T L.A., et al. Effect of moderate- versus high-intensity interval exercise training on heart rate variability parameters in inactive Latin-American adults: a randomized clinical trial. J Strength Condit Res. 2020;34(12):3403–3415. doi: 10.1519/JSC.0000000000001833. [DOI] [PubMed] [Google Scholar]
- 40.Reimers A.K., Knapp G., Reimers C.D. Effects of exercise on the resting heart rate: a systematic review and meta-analysis of interventional studies. J Clin Med. 2018;7(12):503. doi: 10.3390/jcm7120503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wilmore J.H., Stanforth P.R., Gagnon J., et al. Heart rate and blood pressure changes with endurance training: the HERITAGE Family Study. Med Sci Sports Exerc. 2001;33(1):107–116. doi: 10.1097/00005768-200101000-00017. [DOI] [PubMed] [Google Scholar]
- 42.O'Driscoll J.M., Wright S.M., Taylor K.A., Coleman D.A., Sharma R., Wiles J.D. Cardiac autonomic and left ventricular mechanics following high intensity interval training: a randomized crossover controlled study. J Appl Physiol. 2018;125(4):1030–1040. doi: 10.1152/japplphysiol.00056.2018. 1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gourine A., Gourine A.V. Neural mechanisms of cardioprotection. Physiology (Bethesda) 2014;29(2):133–140. doi: 10.1152/physiol.00037.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Alansare A., Alford K., Lee S., Church T., Jung H.C. The effects of high-intensity interval training vs. Moderate-intensity continuous training on heart rate variability in physically inactive adults. Int J Environ Res Publ Health. 2018;15(7) doi: 10.3390/ijerph15071508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hottenrott K., Hoos O., Esperer H.D. Herzfrequenzvariabilität und Sport. Herz. 2006;31(6):544–552. doi: 10.1007/s00059-006-2855-1. [DOI] [PubMed] [Google Scholar]
- 46.Astorino T.A., Clausen R., Marroquin J., Arthur B., Stiles K. Similar perceptual responses to reduced exertion high intensity interval training (REHIT) in adults differing in cardiorespiratory fitness. Physiol Behav. 2020;213:112687. doi: 10.1016/j.physbeh.2019.112687. [DOI] [PubMed] [Google Scholar]
- 47.Parfitt G., Olds T., Eston R. A hard/heavy intensity is too much: the physiological, affective, and motivational effects (immediately and 6 months post-training) of unsupervised perceptually regulated training. J Exerc Sci Fit. 2015;13(2):123–130. doi: 10.1016/j.jesf.2015.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]