Abstract
Background
High-intensity interval training (HIIT) or moderate-intensity continuous training (MICT) alone has been shown to improve metabolic health, but the effects of alternating the two training approaches as often practiced in real life remained unclear.
Purpose
To examine the effects of HIIT or MICT alone or alternating HIIT-MICT on cardiometabolic responses in inactive obese middle-aged men.
Methods
Forty-two participants (age: 42 ± 5 y; BMI: 26.3 ± 2.1 kg m−2) were randomly assigned to four groups: HIIT (12 x 1-min running bouts at 80–90% HRmax interspersed with 1-min active recovery at 50% HRmax), MICT (40-min brisk walk at 65–70% HRmax), alternating HIIT-MICT or a non-exercise control group (CON). Exercise sessions were conducted three times per week for 16 weeks. Maximal oxygen uptake (VO2max), body composition (by bioelectrical impedance analysis), blood pressure, fasting blood glucose, insulin resistance (HOMA-IR) and lipid profile were assessed at baseline and after the 16-week intervention. Enjoyment and self-efficacy were also assessed at the end of intervention.
Results
All exercise groups showed a similar VO2max increase of ∼15% (HIIT: 34.3 ± 4.4 vs 39.1 ± 5.4; MICT: 34.9 ± 5.0 vs 39.4 ± 7.2; and alternating HIIT-MICT: 34.4 ± 5.0 vs 40.3 ± 4.6 mL kg−1min−1) compared to baseline and CON (all p < 0.05). Weight, BMI, % fat and waist circumference also showed similar reductions in all exercise groups compared to baseline and CON (all p < 0.05). No significant group difference was observed for all blood markers. Compared to baseline, total cholesterol decreased after HIIT-MICT, while HIIT significantly decreased fasting insulin level and improved insulin resistance (p < 0.05). Enjoyment, self-efficacy and adherence were similar among all exercise groups.
Conclusion
HIIT or MICT alone or alternating HIIT-MICT similarly improve cardiovascular fitness and body composition in obese middle-aged men despite differences in total training volume and time commitment.
Keywords: HIIT, Interval exercise, Continuous training, Weight management, Public health
1. Introduction
Physical inactivity is a leading cause of global mortality and increases the risk of non-communicable diseases (NCDs) including cardiovascular diseases (CVD), obesity, type 2 diabetes (T2D), certain cancers, and premature mortality.1 Current physical activity (PA) guidelines typically recommend a minimum of 150 min of weekly moderate-intensity aerobic PA to enhance health.2,3 However, compliance with these guidelines around the world is low1 and a frequently cited barrier to is “lack of time.“.4 Therefore, an effective, time-efficient and enjoyable exercise protocol would hold great potential for mitigating the detrimental health consequences of physical inactivity and obesity.
Recent public health promotions have highlighted high-intensity interval training (HIIT) as an efficacious exercise strategy that may offer some time savings.5 HIIT is generally defined as repeated bouts of vigorous but submaximal exercise that elicits ≥80% maximum heart rate [HRmax]), interspersed with short periods of recovery.6 In particular, many HIIT protocols are classified as “low-volume” in nature, which only lasted ≤30 min per session.7 Despite the reduced training volume and lower time commitment relative to moderate-intensity continuous training (MICT), HIIT has generally been shown to improve cardiovascular fitness,8 cardio-metabolic health,9,10 weight management11 and cardiovascular function.12 For instance, a recent study showed that a HIIT protocol involving 10 × 1min bouts at 80–90% HRmax with 1-min recovery can elicit a similar improvement of cardiovascular fitness as traditional higher-volume MICT in overweight/obese middle-aged men.13 Other recent work also revealed that HIIT and continuous exercise yield comparable results on insulin sensitivity and various cardiovascular disease risk factors under work-matched14,15 and non-matched conditions.16
Despite the supporting health benefits of HIIT, its contribution to existing PA recommendations, which focuses on continuous exercise remains unclear. The latest Physical Activity Guideline Advisory Committee Scientific Report17 highlighted that most HIIT interventions are < 12 weeks, which are insufficient to detect clinically meaningful changes. In addition, most studies have compared HIIT versus MICT alone but have not evaluated the effects of alternating type training (HIIT-MICT) that many individuals might do in real life. Furthermore, intervention studies evaluating adherence related psycho-perceptual responses (i.e., enjoyment and self-efficacy) to HIIT are limited, particularly in physically inactive adults. While it has been shown that middle-aged men had both a lower self-efficacy and preference to an acute HIIT session,18 such responses over a longer period of time merit investigation.
Most HIIT protocols have been performed in well-supervised and controlled-laboratory or gym conditions using specialized equipment but these do not reflect the “real-world” practice of many individuals that often involves mixed training protocols that alternates HIIT and MICT.19 Research is needed that compares the efficacy of HIIT, MICT and alternating HIIT and MICT under free-living conditions.19, 20, 21 Recent evidence suggests that an unsupervised HIIT program was well-accepted by overweight/obese adults over 12 months.22 Yet, further studies conducted in unsupervised settings are needed to determine if incorporating HIIT in the real world is more effective in improving clinically relevant cardiometabolic outcomes and eliciting positive psychological responses than performing MICT alone.
This study therefore aimed to evaluate the effects of 16-week alternating HIIT-MICT on cardiometabolic health and adherence-related psycho-perceptual responses in physically inactive and obese middle-aged adults in a free-living condition. It was hypothesized that alternating HIIT-MICT would elicit favorable cardiometabolic health and adherence-related psycho-perceptual responses as performing HIIT or MICT alone.
2. Methods
2.1. Participants
This study was a randomized controlled trial (RCT) consisting of three intervention groups and one control group. A total of 48 inactive and obese Asian men aged 40–59 years were recruited through advertisements in the university, partner institutions, community centers, and online This particular cohort was chosen purposefully for the study, since men are typically associated with 4–5 times higher coronary heart disease (CHD) mortality risk than women in middle age.23 The recruitment advertisement only mentioned that the study was a 16-week intervention for improving cardiometabolic health in inactive obese middle-aged men, without specifying the exercise protocols (i.e. to prevent selection bias). Participants were considered as obese if their body mass index (BMI) > 25.0 kg m−2 according to the World Health Organization (WHO) standard for the Asian population1 and as physically inactive if they reported less than 150 min of moderate or 75 min of vigorous PA per week, as assessed via the International Physical Activity Questionnaire (IPAQ).24 Exclusion criteria included 1) severe high blood pressure (≥180/100 mm Hg); 2) taking prescribed medication for chronic health and medical conditions, including but not limited myocardial infarction, uncompensated heart failure, or unstable angina pectoris and; 3) any pre-existing medical or physical issue that could affect training and experimental tests, as outlined by current exercise prescription guidelines.2 The screening procedure was conducted by a certified exercise physiologist in which participants were asked to complete written consents and a health history questionnaire with a specific focus on cardiometabolic diseases that may preclude participation in the study.25,26 We estimated that a sample size of 12 participants per group would be required to detect an effect size of f = 0.5 between exercise groups and control group,27 with a power of 0.85 at an alpha level of 0.05 (G∗Power version 3.0.10). This effect size was deemed reasonable based on determinations made in G∗Power using our hypothesized clinically meaningful maximal oxygen uptake (VO2max) improvement of 10%27 and typical means, standard deviations and correlations determined in our laboratory13 and reported in the literature for VO2max in adults.28,29 Ethical approval was obtained from the Clinical Research Ethical Committee, CUHK (Chinese Clinical Trial Registry: ChiCTR1900022132).
2.2. Exercise intervention
The 48 screened participants were randomly assigned to one of three exercise groups or a control group after baseline assessments. Block randomization (in blocks of 4) using a counter-balanced design was performed by a research assistant who was independent of the data collection process. All intervention groups performed a standardized 3-min warm-up and 3-min cool-down at 50% HRmax.
-
(i)
HIIT: Twelve 1-min bouts of running at 80–90% HRmax, with 1-min walking at 50% HRmax in between bouts.
-
(ii)
MICT: 40-min of brisk-walking at 65–70% HRmax for each session.
-
(iii)
Alternating group (HIIT-MICT): Alternate between the abovementioned HIIT and MICT protocols for each consecutive session.
-
(iv)
Control (CON): No specific exercise intervention was given.
The total energy expenditure of each exercise session was matched for all of the experimental groups based on oxygen uptake data previously collected in our laboratory18 and confirmed by subsequent HR regression analysis. Participants were required to exercise three times per week on non-consecutive days for 16 weeks (i.e., 48 sessions in total).
Running, jogging or brisk walking could be performed on a treadmill or outdoors based on participants’ preference, as long as the prescribed HR intensities were achieved. The first 2 sessions included one-on-one supervised training, specific to the exercise intervention prescribed to participants in a laboratory setting. From the third session onwards, participants were instructed to perform their prescribed exercise in an unsupervised free-living condition. This methodological approach has been employed in previous research30,31 to address adherence to HIIT under unsupervised conditions.
As most physically inactive participants in the current study had a relatively low fitness level, a progressive approach was adopted in the intervention, which has been commonly employed.13,32,33 For the first two weeks, participants performed 50% of the duration of the designated exercise protocol. Therefore, the HIIT protocol was 6 x 1-min interval (instead of 12 repetitions) while the MICT protocol comprised 20-min of continuous exercise. In the third and fourth week, the volume progressed to 75% of the total duration of the protocols. Finally, the participants performed the full duration of the prescribed exercise in the remaining sessions. The total time commitment of each protocol, therefore, ranged from ∼17–29 min for HIIT and ∼26–46 min for MICT (including warm-up and cool-down). Notably, the MICT alone group was designated to accumulate approximately ∼150-min of moderate-intensity exercise per week, in accordance with the current PA guidelines.2,3 Each participant wore a heart rate (HR) monitor (H10, Polar Electro, Finland) for every exercise session to monitor exercise intensity. The HR monitors collated all exercise session data (including HR and energy expenditure) and were used to confirm the target intensity and session adherence (i.e., % of prescribed sessions attended). No specific behavioral counseling sessions were given to the participants. As fitness levels were likely to increase as the intervention progresses, a research assistant (unaware of the study purpose) informed the participants to adjust the running/walking speed accordingly to ensure individuals always exercise at their assigned HR on a monthly basis. Other than that, the researchers and the assistant avoided contact with participants during the intervention to let them follow the protocol based on their own choice and checked the overall session adherence at the end of the intervention. Similar monitoring approaches have been used in previous intervention studies.30,34 All participants were asked to maintain their usual daily PA outside the lab throughout the study period.
2.3. Cardiometabolic and cardiovascular markers
All cardiovascular and metabolic indices (shown in Table 1) were measured at: (i) baseline and (ii) at least 48 h (within 5 days) after the final session of the 16-week intervention at the Exercise Physiology Laboratory, Department of Sports Science and Physical Education, CUHK. Participants were instructed to avoid strenuous exercise for at least 24 h and caffeine consumption for at least 12 h, prior to each visit for testing. Each test took place at the same time of the day (i.e., 8a.m.–10a.m.). In the 24 h before the baseline test, participants were also required to record their food intake, and were instructed to replicate the same diet on the day before the post-test.
Table 1.
Anthropometric, cardiometabolic and dietary outcomes in all groups at baseline and post-intervention (mean ± SD).
| HIIT-MICT (n = 11) |
HIIT (n = 11) |
MICT (n = 10) |
CON (n = 10) |
ANCOVA |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | Pre | Post | Pre | Post | P-value | η2p | |
| Age (yr) | 40.2 ± 5.3 | 40.5 ± 7.1 | 40.1 ± 3.6 | 44.8 ± 6.5 | ||||||
| VO2max (mL/min/kg) | 34.4 ± 5.0 | 40.3 ± 4.6∗∗# | 34.3 ± 4.4 | 39.1 ± 5.4∗∗# | 34.9 ± 5.0 | 39.4 ± 7.2∗∗# | 36.4 ± 7.2 | 36.1 ± 7.0 | 0.009 | 0.16 |
| HRmax (bpm) | 183 ± 10 | 181 ± 9 | 181 ± 17 | 179 ± 17 | 183 ± 8 | 181 ± 6 | 180 ± 8 | 177 ± 6 | 0.875 | 0.02 |
| Exhaustion Time (min) | 10.9 ± 0.8 | 11.7 ± 0.9∗∗# | 10.7 ± 1.3 | 11.4 ± 1.0∗∗# | 10.7 ± 1.1 | 11.4 ± 1.2∗∗# | 10.3 ± 1.4 | 10.0 ± 1.3 | 0.001 | 0.17 |
| Maximal speed (mph) | 4.3 ± 0.2 | 4.6 ± 0.4∗∗# | 4.3 ± 0.4 | 4.5 ± 0.4∗∗# | 4.4 ± 0.4 | 4.5 ± 0.4∗∗# | 4.2 ± 0.4 | 4.2 ± 0.4 | 0.001 | 0.15 |
| Maximal inclination (%) | 16.2 ± 0.6 | 16.9 ± 1.0∗∗# | 16.2 ± 1.1 | 16.8 ± 1.0∗∗# | 16.5 ± 1.0 | 16.8 ± 1.0∗# | 16.0 ± 1.1 | 16.0 ± 1.1 | 0.001 | 0.14 |
| Weight (kg) | 77.3 ± 7.4 | 76.5 ± 7.6∗# | 78.3 ± 8.6 | 77.0 ± 8.2∗# | 77.7 ± 11.2 | 76.5 ± 11.7∗# | 80.9 ± 7.2 | 81.7 ± 7.4 | 0.025 | 0.07 |
| BMI (kg·m−2) | 26.1 ± 2.2 | 25.8 ± 2.2∗# | 26.3 ± 2.4 | 25.9 ± 2.3∗# | 26.7 ± 2.6 | 26.3 ± 2.7∗# | 26.7 ± 1.6 | 26.9 ± 1.7 | 0.025 | 0.07 |
| Fat (%) | 24.0 ± 3.1 | 23.0 ± 3.4∗∗# | 23.9 ± 3.4 | 22.5 ± 2.9∗∗# | 23.9 ± 3.3 | 22.3 ± 3.7∗∗# | 22.7 ± 2.3 | 22.9 ± 2.6 | 0.001 | 0.09 |
| Waist Circumference (cm) | 87.5 ± 6.4 | 85.8 ± 6.2∗∗# | 87.0 ± 5.9 | 85.3 ± 6.0∗∗# | 86.8 ± 5.0 | 84.6 ± 5.1∗∗# | 91.4 ± 6.3 | 91.4 ± 6.2 | 0.046 | 0.07 |
| Systolic BP (mm Hg) | 123.2 ± 9.6 | 123.1 ± 11.6 | 126.1 ± 13.3 | 121.4 ± 10.1 | 115.3 ± 10.0 | 115.0 ± 10.7 | 127.8 ± 7.0 | 119.9 ± 8.0 | 0.074 | 0.03 |
| Diastolic BP (mm Hg) | 79.3 ± 9.6 | 77.6 ± 8.4 | 80.1 ± 6.2 | 76.8 ± 6.8 | 72.1 ± 6.5 | 71.4 ± 5.8 | 80.9 ± 5.3 | 80.1 ± 7.2 | 0.837 | 0.02 |
| Total Cholesterol (mmol/L) | 6.02 ± 0.54 | 5.43 ± 0.53∗ | 5.99 ± 0.62 | 5.73 ± 0.66 | 5.78 ± 0.58 | 5.53 ± 0.79 | 5.60 ± 0.95 | 5.38 ± 0.59 | 0.512 | 0.02 |
| HDL (mmol/L) | 1.40 ± 0.36 | 1.33 ± 0.45 | 1.31 ± 0.42 | 1.26 ± 0.35 | 1.07 ± 0.15 | 1.10 ± 0.28 | 1.31 ± 0.45 | 1.16 ± 0.33 | 0.450 | 0.03 |
| Triglyceride (mmol/L) | 1.50 ± 0.71 | 1.40 ± 0.61 | 1.85 ± 0.76 | 1.70 ± 0.54 | 1.77 ± 0.57 | 1.55 ± 0.60 | 1.40 ± 0.55 | 1.53 ± 0.89 | 0.304 | 0.02 |
| LDL (mmol/L) | 3.93 ± 0.42 | 3.46 ± 0.68∗ | 3.84 ± 0.36 | 3.69 ± 0.63 | 3.89 ± 0.56 | 3.72 ± 0.63 | 3.47 ± 0.85 | 3.51 ± 0.69 | 0.410 | 0.03 |
| Fasting Glucose (mmol/L) | 5.53 ± 0.46 | 5.65 ± 0.28 | 5.62 ± 0.56 | 5.55 ± 0.35 | 5.32 ± 0.25 | 5.45 ± 0.24 | 5.48 ± 0.62 | 5.39 ± 0.41 | 0.267 | 0.03 |
| Fasting insulin (pmol/L) | 59.4 ± 29.6 | 56.4 ± 20.2 | 54.2 ± 27.0 | 43.0 ± 8.3∗ | 58.7 ± 30.1 | 60.8 ± 35.7 | 65.7 ± 29.5 | 63.7 ± 23.1 | 0.107 | 0.06 |
| Insulin resistance (HOMA-IR) | 1.14 ± 0.56 | 1.09 ± 0.38 | 1.23 ± 0.50 | 0.83 ± 0.16∗ | 1.11 ± 0.55 | 1.16 ± 0.67 | 1.25 ± 0.56 | 1.21 ± 0.43 | 0.096 | 0.05 |
| Energy Intake (kcal) | 1913 ± 131 | 1946 ± 123 | 1878 ± 121 | 1901 ± 143 | 1891 ± 135 | 1924 ± 143 | 1913 ± 128 | 1936 ± 130 | 0.454 | 0.02 |
| Carbohydrates (g) | 253 ± 56 | 241 ± 52 | 242 ± 51 | 237 ± 54 | 234 ± 56 | 244 ± 54 | 248 ± 52 | 241 ± 57 | 0.346 | 0.02 |
| Protein (g) | 94 ± 20 | 101 ± 25 | 90 ± 20 | 95 ± 27 | 96 ± 22 | 93 ± 22 | 93 ± 24 | 101 ± 21 | 0.746 | 0.02 |
| Fat (g) | 56 ± 18 | 59 ± 16 | 61 ± 18 | 64 ± 13 | 63 ± 15 | 64 ± 12 | 56 ± 12 | 59 ± 19 | 0.356 | 0.03 |
Note: BMI, body mass index, BP, blood pressure, HDL, high-density lipoprotein cholesterol; HOMA-IR, homeostasis assessment model for insulin resistance; HRmax, maximal heart rate; LDL, low-density lipoprotein cholesterol; VO2max, maximal oxygen uptake.
∗pre vs post (p < 0.05). ∗∗ pre vs post (p < 0.01). # indicates significant group difference compared to CON upon pairwise comparison (p < 0.05).
2.4. Cardiovascular fitness
Participants performed a standardized Bruce Protocol ramp treadmill test to assess their cardiovascular fitness (i.e. VO2max) and HRmax. The detailed procedure of this test has been described elsewhere.35 Briefly, participants started exercising at 1.7 miles per hour (mph) on a 10% grade. The speed and incline of the treadmill increased every 3 min. The test was conducted until volition exhaustion. Achievement of VO2max was evaluated based on the following criteria as recommended36: (1) a respiratory exchange ratio of greater than or equal to 1.10; (2) failure of heart rate to increase with increases in workload; (3) post-exercise blood lactate ≥8.0 mmol/L. All participants were able to achieve VO2max based on these criteria. Blood lactate was measured via capillary blood samples from the fingertips with a portable analyser (Lactate Plus, Nova Biomedical, Waltham, Massachusetts). HR was recorded continuously during the test using HR telemetry (H10 Sensor, Polar, Finland) and HRmax was determined as the highest value recorded at the end of test. Individual HR data collected from the VO2max test were used to prescribe the intensity for the subsequent training sessions.
2.5. Body composition and anthropometry
A Bioelectrical Impedance Analysis (BIA) scale (MC-780MA, Tanita, Japan) was used to measure body weight, body mass index (BMI), whole body and regional fat mass, and lean body mass (LBM). Participants were measured wearing light clothing and bare feet after being asked to void their bladders. Individual data were input into the BIA scale following the manufacturer's instruction. Waist circumference was measured with an anthropometric tape to indicate central obesity based on WHO classification for Asian adults.37
2.6. Blood biomarkers
Twelve-hour fasted venous blood sampling (20 mL) was performed by a qualified nurse. Glucose was measured using the enzymatic-amperometric method (Biosen-C; EKF Diagnostics, Germany) with an intra-assay coefficient of variation (CV) of 0.5%. Lipid profile was measured via commercially available kits (RX Monza; Randox Biosciences, UK). Total cholesterol was measured via cholesterol oxidase, esterase, and peroxidase colorimetric method and had an intra-assay CV of 1.3%. High-density lipoprotein (HDL) cholesterol was measured by the polyethylene glycol direct method while low-density lipoprotein (LDL) cholesterol was assessed using the direct method with an intra-assay CV of 0.7% and 1.3%, respectively. Triglyceride was measured using the enzymatic method without glycerol blanking with an intra-assay CV of 1.3%. Insulin was measured using an enzyme-linked immunosorbent assay (ELISA) (Insulin ELISA; Mercodia AB, Sweden). The average of duplicate measures for each marker was reported. A homeostasis assessment model for insulin resistance (HOMA-IR) was used to estimate overall insulin resistance.38 It was calculated according to the formula: [glucose] (mmol/L) × [insulin] (μU/mL)/22.5.38
2.7. Blood pressure
Blood pressure was measured at the brachial artery using a clinical automatic blood pressure monitor (M7, Omron, Japan) and cuff following 10 min of supine rest in a quiet place. Two readings (with 1-min interval) of systolic blood pressure (SBP) and diastolic blood pressure (DBP) were averaged.
2.8. Psychological responses
Exercise enjoyment and self-efficacy were assessed at the end of the 16-week exercise intervention. Perceived enjoyment of the three protocols was assessed using the original English version of Physical Activity Enjoyment Scale (PACES). This validated instrument39 is suitable for use as a mediator variable for devising interventions for promoting PA.40,41 Participants were asked to complete the scale determine which protocol they perceived as being more enjoyable.
Self-efficacy is the perception of confidence in performing certain actions. Feeling of competence and confidence are suggested as the key psychological drivers of exercise compliance.42,43 Three factors (task, scheduling, and coping) related to exercise self-efficacy were assessed by a 5-item questionnaire.44 Each item was rated between 1 (no confidence) to 10 (complete confidence). The scores for each factor were then combined for subsequent analysis. Participants' self-efficacy was assessed via a 5-item questionnaire45 designed to determine participants' confidence to repeat their exercise task. All questions included the same stem, “How confident are you that you can …” and the 5-items were: “perform (one to five) session(s) of exercise per week for the next 4 weeks that is just like the one you completed throughout the intervention?” Responses were scored as a percentage of 0% (Not at all) to 100% (Extremely confident) in 10% increments, and then averaged for the five items. Participants were asked to complete the scale at the end of the 16-week intervention. The self-efficacy scale demonstrated good internal consistency (α′s = 0.9) in the present study.
2.9. Dietary intake
Participants were instructed to maintain their usual diet throughout the exercise intervention, in accordance with existing intervention studies on HIIT.34,46 A validated three-day food diary assessment (on two weekdays and one weekend day) were conducted before and after the intervention47 to control for dietary influence, ensuring all observed post-test changes are due to the exercise intervention. Completed dietary records were analyzed using the online database of the Centre for Food Safety, Hong Kong by a registered dietician. The total amount of calories and macronutrients (i.e. carbohydrate, fat and protein) were assessed.
2.10. Statistical analysis
Data were analyzed using SPSS (Version 22.0). All continuous variables were presented as means and standard deviation. Mean differences among groups (HIIT, MICT, HIIT-MICT and CON) for each cardio-metabolic variable were tested by analysis of covariance (ANCOVA), while controlling for baseline values. This statistical approach was chosen as it has shown to be generally more powerful than a two-way repeated-measures ANOVA (group main effect and time by group interaction) when interest lies in group differences in change from pre-test to post-test.48 Additional paired-sample t-tests were used to examine within-group time effect. Psychological variables were tested by one-way analysis of covariance (ANOVA). When a significant F-ratio was obtained, Bonferroni post hoc analysis was performed for pairwise comparisons. The threshold for statistical significance was set at the 0.05 level (2-sided).
To estimate practical relevance of the ANCOVA between group effects, effect sizes (partial eta squared, η2p) were calculated. An η2p ≥ 0.01 indicates a small, ≥ 0.06 a medium and ≥ 0.14 a large effect.49 Additionally, effect sizes comparing pre-post changes within each group were calculated using Cohen's d to indicate the magnitude of standardized mean difference (SMD) where appropriate.50 Scores of 0.2, 0.5 and > 0.8 were considered small, moderate and large effect sizes, respectively.
3. Results
3.1. Training characteristics
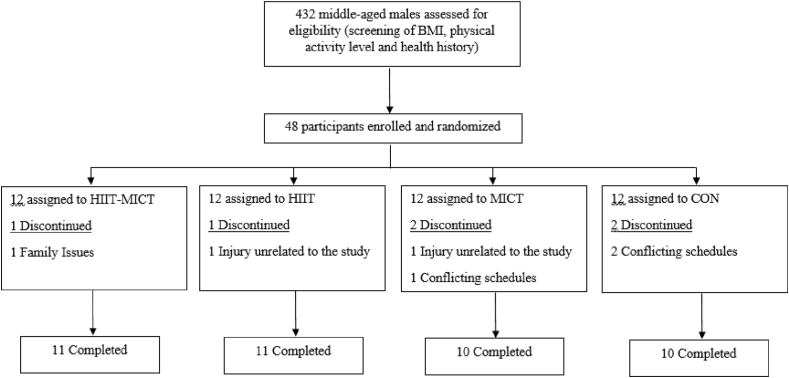
Six participants withdrew from the study unexpectedly owing to scheduling conflicts (n = 3), injuries unrelated to the study (n = 2) and family issues (n = 1). Thus, 42 participants completed all required testing and their data were included in the subsequent analysis (see Fig. 1). Their baseline PA level was 60 ± 23 min/week for moderate-intensity PA and 23 ± 13 min/week for vigorous-intensity PA, according to pre-intervention IPAQ analysis. The average energy expenditure of the HIIT, MICT and alternating group was 311 ± 22 kcal, 325 ± 28 kcal and 319 ± 26 kcal per exercise session. The average intensity was 86 ± 6% and 68 ± 5% of HRmax for each session of HIIT and MICT respectively, indicating that the participants were able to comply with the prescribed exercise intensity throughout the intervention.
Fig. 1.
CONSORT flow diagram of Study.
3.2. Cardiovascular fitness
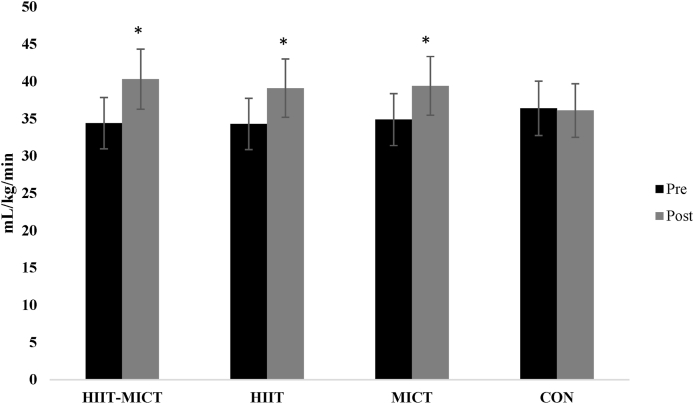
All exercise groups showed a similar VO2max increase of ∼15% (SMD = 0.7–1.2). Taken baseline values into account, ANCOVA revealed a large and significant between group effect for VO2max (p < 0.01, η2p = 0.15). Post-hoc analysis showed that VO2max in all exercise groups were higher compared to CON after the 16-week intervention (all p < 0.05, Table 1 and Fig. 2). Exhaustion time, maximal speed and inclination attained in Bruce treadmill test showed large and significant between group effect (p < 0.01, η2p = 0.14–0.17), while pairwise comparisons showed significant improvements of these variables in all exercise groups compared to CON (all p < 0.05, Table 1). There is no significant time or group difference in HRmax (all p > 0.05, Table 1).
Fig. 2.
VO2max before and after the 16-week intervention. Values are mean ± SD. ∗indicates significant post-training group difference compared to CON (p < 0.05).
3.3. Body composition and anthropometry
Weight, BMI, % fat and waist circumference showed similar reductions in all exercise groups (SMD = 0.2–0.5). ANCOVA, again taken baseline values into account, revealed a moderate and significant between group effect for weight, BMI, % fat and waist circumference (p < 0.05, η2p = 0.06–0.09). Post-hoc analysis showed that these body composition and anthropometric variables in all exercise groups were lower at post-intervention compared to CON (all p < 0.05, Table 1).
3.4. Cardiometabolic blood markers
ANCOVA did not reveal significant group differences for all blood markers at post-intervention (p > 0.05, η2p = 0.02–0.06; Table 1). Compared to baseline, total cholesterol and LDL decreased after HIIT-MICT (p < 0.05, SMD = 0.8), while HIIT showed significant decrease in fasting insulin (p < 0.05, SMD = 0.5) and improved insulin resistance (p < 0.05, SMD = 0.9) after the 16-week intervention.
3.5. Dietary intake
Energy and macronutrient did not show significant time or group difference for all groups (all p > 0.05), suggesting that participants did not change their diet throughout the 16-week intervention (Table 1).
3.6. Psychological responses and exercise adherence
No significant differences for enjoyment (p = 0.789) and self-efficacy score for the three groups (p = 0.345). Meanwhile exercise adherence was satisfactory and similar in both groups (>80% attendance rate, p = 0.576) (Table 2). One minor injury incident (knee pain) was reported in the HIIT group but the participant could resume training normally after a short period of rest (i.e. a few days). No other incidence of adverse events related to training was reported.
Table 2.
Psychological outcomes in all exercise groups after the 16-week intervention (mean ± SD).
| HIIT-MICT (n = 11) | HIIT (n = 11) | MICT (n = 10) | Group Difference (P Value) | |
|---|---|---|---|---|
| Enjoyment (score out of 126) | 102.5 ± 8.0 | 109.1 ± 11.1 | 109.1 ± 9.5 | 0.789 |
| Self-Efficacy (score out of 100) | 66.3 ± 14.3 | 61.2 ± 13.9 | 60.3 ± 17.2 | 0.345 |
| Exercise Adherence (% of prescribed sessions completed) | 85.8 ± 4.2 | 84.0 ± 8.4 | 83.8 ± 4.3 | 0.576 |
4. Discussion
The major finding of the current study was that 16 weeks of training using HIIT or MICT alone or an alternating model of HIIT-MICT was similarly efficacious for improving cardiorespiratory fitness and other health-related markers in previously inactive and obese middle-aged men. This study also extends the previous literature by using a real-world approach to compare the efficacy of HIIT or MICT alone or alternating HIIT-MICT under an unsupervised free-living setting.
Low cardiovascular fitness, indicated as maximal oxygen uptake (VO2max), is a consequence of physically inactive lifestyle and a powerful predictor of premature cardiovascular mortality.51 The majority of literature has suggested that both HIIT and MICT can elicit large improvements in the VO2max of healthy, young to middle-aged adults.8,52 Most of these studies, however, only separately compare the efficacy of single interventions such as MICT alone or HIIT alone. To date, limited research has investigated the potential benefits of alternating HIIT-MICT on cardiovascular and cardio-metabolic health. Recently, 2 years of supervised combined HIIT-MICT consisting of 30 min of exercise 4–5 days per week including at least 1 HIIT session (4 x 4-min at 90–95% HRmax with 3-min active recovery) was effective in reducing cardiac stiffness, decreasing resting HR and improving cardiovascular fitness in previously sedentary middle-aged adults.53
To the best of our knowledge, however, only one study has compared the combined effect HIIT-MICT and MICT alone.54 Roxburgh et al. investigated the effectiveness of MICT alone (5 days per week) versus MICT (4 days per week) combined with a single weekly bout of HIIT on cardiovascular fitness over 12 weeks. Both protocols elicited clinically meaningful improvements in cardiovascular fitness but no significant group difference was found. Our current study add novelties to the existing body of evidence by revealing that alternating HIIT-MICT can elicit comparable improvements in cardiovascular fitness as performing HIIT and MICT alone. All exercise groups induced a similar and substantial VO2max increase (approximately 5–6 mL kg−1·min−1). Of note, such magnitude of improvement likely has significant clinical relevance. Given that cardiovascular function decreases with primary aging and that each 1- metabolic equivalent increase in cardiovascular fitness is associated with a 13% and 15% reduction in all-cause and CVD mortality respectively,27 our study suggested both alternating or single type training could also be a feasible approach to enhance cardiovascular function in physically inactive and obese middle-aged adults.
Another highlighted aspect of the present study was the significant and similar reduction of weight, BMI, % fat and waist circumference in all exercise groups over the 16-week intervention. This result was in accordance with recent systematic evidence which suggested both HIIT and MICT could induce modest body composition improvements.55 While some studies suggested that HIIT may induce fat loss more effectively than MICT by several proposed mechanisms, including increased excess post-exercise oxygen consumption (EPOC), decreased post-exercise appetite and catecholamine release that elevate tissue lipolysis,56 our result did not reveal significant difference between all exercise groups. It is worth noting that the energy expenditure of each exercise session was matched for all exercise groups. Participants also did not change their diet throughout the intervention according to our dietary analysis. From a weight management point of view, it is thus possible that the lack of caloric expenditure and intake difference among the three exercise groups may make the group difference in body weight and composition change not clinically relevant over the 16-week intervention.
We found no group difference in all measured blood markers and blood pressure. This similarity in response is consistent with existing literature, which suggests that HIIT promotes similar cardiometabolic blood marker improvement in comparison to MICT.57 A possible explanation for our finding could be that most participants already presented blood markers and blood pressure within standard-range at baseline, and thus reducing the likelihood of observing notable group difference. Yet, total cholesterol and LDL decreased after HIIT-MICT, while HIIT significantly decreased fasting insulin level and improved insulin resistance when compared to baseline, although these variables did not differ significantly upon group comparison at post-intervention. Further research investigating the cardiometabolic health benefits of HIIT/MICT or their combination could be carried out in different clinical populations (e.g. hypertensive, diabetic and metabolic syndrome patients).
As for the psychological responses, no significant group difference for enjoyment and self-efficacy were found. While the physiological benefits of HIIT have been demonstrated in this study and others,6 a typical public health concern is how the general population, particularly inactive and less fit middle-aged individuals, perceive HIIT and whether they can adhere to it in the long term.58 Findings to date have been conflicting with some studies reporting positive affect and/or enjoyment in response to a single bout of HIIT compared to MICT,59, 60, 61 while others reported contradictory findings.62 Such mixed results towards psychological responses to HIIT is likely explained by the heterogeneity of protocol used (e.g., relative intensity, duration and total number of work bouts completed) and participants’ background (e.g., age, activity level and obesity level etc.). Nevertheless, both the HIIT group and alternating group in the present study showed satisfactory attendance rate (>80%) and high level of enjoyment, and reported no adverse events, suggesting that it is a practical and well-tolerated exercise option for inactive middle-aged obese adults when performed in an unsupervised free-living setting.
This study has several strengths including investigating cardiometabolic changes and psychological outcomes under a randomized control research design that mainly performed in free-living conditions which provide more real-life implications. In addition, this study also used accurate and reliable measures of cardiorespiratory fitness and blood sampling, monitoring participant's diet before and after the intervention and a satisfactory adherence in all exercise groups. Despite these strengths, it is acknowledged that only middle-aged male participants were recruited and hence caution should be taken when generalizing to younger and elderly men, as well as women. Another limitation is that this study tested only fasted samples and did not utilize more direct measurements such as glucose clamp technique or oral glucose tolerance test to depict insulin sensitivity. Furthermore, the relatively small sample size in this study may limit the ability to draw some conclusion about the relative potency of each exercise group, especially on some secondary outcomes. Future studies are needed that are adequately powered to detect potential differences between interventions, although sample size needed might likely be very large. We do believe, however, that our findings provide valuable insights regarding the real-world application of HIIT, MICT and their combination in an unsupervised free-living setting. While the incorporation of HIIT into traditional continuous-based exercise program might not necessarily offer superior health benefits, it could be a time-efficient and efficacious approach considered by healthcare professionals, when designing individualized programmes that target cardiometabolic health benefits in physically inactive obese middle-aged men.
5. Conclusion
In summary, our findings suggest that HIIT or MICT alone or alternating HIIT-MICT similarly improved cardiovascular fitness in obese middle-aged men despite differences in total training volume and time commitment. Alternating training also shows a similar enjoyment level as HIIT or MICT alone and all three approached showed high adherence in a free-living environment. Further research in different populations with more exercise protocol combinations is required to determine how HIIT can contribute to the current PA guideline in terms of overall cardiometabolic health and weight management benefits.
Author statement
E.T. Poon: Conceptualization, Investigation, Formal analysis, Writing - original draft. P.M. Siu: Investigation, Writing - review & editing. W. Wongpipit: Investigation, Formal analysis, Writing - review & editing. M. Gibala: Formal analysis, Writing - review & editing. S.H. Wong: Writing - review & editing, Supervision.
Acknowledgement
The work described in this paper was partially supported by a fellowship award from the Research Grants Council of the Hong Kong Special Administrative Region, China (Project No. CUHKPDFS2021-4S11).
Contributor Information
Eric Tsz-Chun Poon, Email: eric.poon@cuhk.edu.hk.
Parco Ming-Fai Siu, Email: pmsiu@hku.hk.
Waris Wongpipit, Email: waris.w@chula.ac.th.
Martin Gibala, Email: gibalam@mcmaster.ca.
Stephen Heung-Sang Wong, Email: hsswong@cuhk.edu.hk.
References
- 1.WHO. World Health Organization Physical Activity Fact Sheet2016.
- 2.ACSM . tenth ed. Wolters Kluwer; Philadelphia, PA: 2017. ACSM's Guidelines for Exercise Testing and Prescription. [Google Scholar]
- 3.WHO . World Health Organization; Geneva: 2010. Global Recommendations on Physical Activity for Health. [PubMed] [Google Scholar]
- 4.Stutts W.C. Physical activity determinants in adults. Perceived benefits, barriers, and self efficacy. AAOHN J. 2002;50:499–507. [PubMed] [Google Scholar]
- 5.Kilpatrick M.W., Jung M.E., Little J.P. HIGH-INTENSITY interval training A review of physiological and psychological responses. ACSM's Health & Fit J. 2014;18:11–16. [Google Scholar]
- 6.MacInnis M.J., Gibala M.J. Physiological adaptations to interval training and the role of exercise intensity. J Physiol. 2017;595:2915–2930. doi: 10.1113/JP273196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gillen J.B., Gibala M.J. Is high-intensity interval training a time-efficient exercise strategy to improve health and fitness? Appl Physiol Nutr Metabol. 2014;39:409–412. doi: 10.1139/apnm-2013-0187. [DOI] [PubMed] [Google Scholar]
- 8.Poon ET, Wongpipit W, Ho RS, Wong SH. Interval training versus moderate-intensity continuous training for cardiorespiratory fitness improvements in middle-aged and older adults: a systematic review and meta-analysis. J Sports Sci. 2021:1-10. [DOI] [PubMed]
- 9.Batacan R.B., Duncan M.J., Dalbo V.J., Tucker P.S., Fenning A.S. Effects of high-intensity interval training on cardiometabolic health: a systematic review and meta-analysis of intervention studies. Br J Sports Med. 2017;51 doi: 10.1136/bjsports-2015-095841. [DOI] [PubMed] [Google Scholar]
- 10.Batacan R.B., Duncan M.J., Dalbo V.J., Tucker P.S., Fenning A.S. Effects of high-intensity interval training on cardiometabolic health: a systematic review and meta-analysis of intervention studies. Br J Sports Med. 2017:51. doi: 10.1136/bjsports-2015-095841. [DOI] [PubMed] [Google Scholar]
- 11.Wewege M., van den Berg R., Ward R.E., Keech A. The effects of high-intensity interval training vs. moderate-intensity continuous training on body composition in overweight and obese adults: a systematic review and meta-analysis. Obes Rev. 2017;18:635–646. doi: 10.1111/obr.12532. [DOI] [PubMed] [Google Scholar]
- 12.Heydari M., Boutcher Y.N., Boutcher S.H. The effects of high-intensity intermittent exercise training on cardiovascular response to mental and physical challenge. Int J Psychophysiol. 2013;87:141–146. doi: 10.1016/j.ijpsycho.2012.11.013. [DOI] [PubMed] [Google Scholar]
- 13.Poon E.T., Little J.P., Sit C.H., Wong S.H. The effect of low-volume high-intensity interval training on cardiometabolic health and psychological responses in overweight/obese middle-aged men. J Sports Sci. 2020:1–8. doi: 10.1080/02640414.2020.1766178. [DOI] [PubMed] [Google Scholar]
- 14.Malin S.K., Francois M.E., Eichner N.Z.M., et al. Impact of short-term exercise training intensity on beta-cell function in older obese adults with prediabetes. J Appl Physiol. 2018;125:1979–1986. doi: 10.1152/japplphysiol.00680.2018. 1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heiston E.M., Eichner N.Z., Gilbertson N.M., Malin S.K. Exercise improves adiposopathy, insulin sensitivity and metabolic syndrome severity independent of intensity. Exp Physiol. 2020;105:632–640. doi: 10.1113/EP088158. [DOI] [PubMed] [Google Scholar]
- 16.Ryan B.J., Schleh M.W., Ahn C., et al. Moderate-intensity exercise and high-intensity interval training affect insulin sensitivity similarly in obese adults. J Clin Endocrinol Metab. 2020;105 doi: 10.1210/clinem/dgaa345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.PAG Advisory Committee . U.S.: U.S. Department of Health and Human Services; Washington, DC: 2018. Physical Activity Guideline Advisory Committee Scientific Report. [Google Scholar]
- 18.Poon E.T., Sun F.H., Chung A.P., Wong S.H. Post-exercise appetite and ad libitum energy intake in response to high-intensity interval training versus moderate- or vigorous-intensity continuous training among physically inactive middle-aged adults. Nutrients. 2018;10 doi: 10.3390/nu10101408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gray S.R., Ferguson C., Birch K., Forrest L.J., Gill J.M.R. High-intensity interval training: key data needed to bridge the gap from laboratory to public health policy. Br J Sports Med. 2016;50 doi: 10.1136/bjsports-2015-095705. 1231-U1219. [DOI] [PubMed] [Google Scholar]
- 20.Stork M.J., Banfield L.E., Gibala M.J., Martin Ginis K.A. A scoping review of the psychological responses to interval exercise: is interval exercise a viable alternative to traditional exercise? Health Psychol Rev. 2017:1–21. doi: 10.1080/17437199.2017.1326011. [DOI] [PubMed] [Google Scholar]
- 21.Gray S.R., Ferguson C., Birch K., Forrest L.J., Gill J.M.R. High-intensity interval training: key data needed to bridge the gap from laboratory to public health policy. Br J Sports Med. 2016;50 doi: 10.1136/bjsports-2015-095705. 1231-U1219. [DOI] [PubMed] [Google Scholar]
- 22.Roy M., Williams S.M., Brown R.C., et al. High-intensity interval training in the real world: outcomes from a 12-month intervention in overweight Adults. Med Sci Sports Exerc. 2018;50:1818–1826. doi: 10.1249/MSS.0000000000001642. [DOI] [PubMed] [Google Scholar]
- 23.Bots S.H., Peters S.A.E., Woodward M. Sex differences in coronary heart disease and stroke mortality: a global assessment of the effect of ageing between 1980 and 2010. Bmj Glob Health. 2017;2 doi: 10.1136/bmjgh-2017-000298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Craig C.L., Marshall A.L., Sjostrom M., et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 25.Riebe D., Franklin B.A., Thompson P.D. Updating ACSM's recommendations for exercise preparticipation health screening: corrigendum. Med Sci Sports Exerc. 2016;48 doi: 10.1249/MSS.0000000000000664. 579-579. [DOI] [PubMed] [Google Scholar]
- 26.Riebe D., Franklin B.A., Thompson P.D., et al. Updating ACSM's recommendations for exercise preparticipation health screening. Med Sci Sports Exerc. 2015;47:2473–2479. doi: 10.1249/MSS.0000000000000664. [DOI] [PubMed] [Google Scholar]
- 27.Kodama S., Saito K., Tanaka S., et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women A meta-analysis. JAMA, J Am Med Assoc. 2009;301:2024–2035. doi: 10.1001/jama.2009.681. [DOI] [PubMed] [Google Scholar]
- 28.Ciolac E.G., Bocchi E.A., Bortolotto L.A., Carvalho V.O., Greve J.M.D., Guimaraes G.V. Effects of high-intensity aerobic interval training vs. moderate exercise on hemodynamic, metabolic and neuro-humoral abnormalities of young normotensive women at high familial risk for hypertension. Hypertens Res. 2010;33:836–843. doi: 10.1038/hr.2010.72. [DOI] [PubMed] [Google Scholar]
- 29.Maldonado-Martin S., Jurio-Iriarte B., Labayen I., et al. Effects of high-intensity aerobic interval training Vs. Moderate exercise on body mass, blood pressure and cardiorespiratory condition in hypertensive patients with diet Vs. No diet. J Hypertens. 2015;33 E276-E276. [Google Scholar]
- 30.Vella C.A., Taylor K., Drummer D. High-intensity interval and moderate-intensity continuous training elicit similar enjoyment and adherence levels in overweight and obese adults. Eur J Sport Sci. 2017;17:1203–1211. doi: 10.1080/17461391.2017.1359679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vella C.A., Taylor K., Drummer D. High-intensity interval and moderate-intensity continuous training elicit similar enjoyment and adherence levels in overweight and obese adults. Eur J Sport Sci. 2017;17:1203–1211. doi: 10.1080/17461391.2017.1359679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Racil G., Ben Ounis O., Hammouda O., et al. Effects of high vs. moderate exercise intensity during interval training on lipids and adiponectin levels in obese young females. Eur J Appl Physiol. 2013;113:2531–2540. doi: 10.1007/s00421-013-2689-5. [DOI] [PubMed] [Google Scholar]
- 33.Shepherd S.O., Wilson O.J., Taylor A.S., et al. Low-volume high-intensity interval training in a gym setting improves cardio-metabolic and psychological health. PLoS One. 2015;10 doi: 10.1371/journal.pone.0139056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tjonna A.E., Lee S.J., Rognmo O., et al. Aerobic interval training versus continuous moderate exercise as a treatment for the metabolic syndrome - a pilot study. Circulation. 2008;118:346–354. doi: 10.1161/CIRCULATIONAHA.108.772822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bruce R.A., Kusumi F., Hosmer D. Maximal oxygen intake and nomographic assessment of functional aerobic impairment in cardiovascular disease. Am Heart J. 1973;85:546–562. doi: 10.1016/0002-8703(73)90502-4. [DOI] [PubMed] [Google Scholar]
- 36.Edvardsen E., Hem E., Anderssen S.A. End criteria for reaching maximal oxygen uptake must Be strict and adjusted to sex and age: a cross-sectional study. PLoS One. 2014;9 doi: 10.1371/journal.pone.0085276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.WHO . World Health Organization; Geneva: 2011. Waist Circumference and Waist-Hip Ratio : Report of a WHO Expert Consultation. [Google Scholar]
- 38.Matthews D.R., Hosker J.P., Rudenski A.S., Naylor B.A., Treacher D.F., Turner R.C. Homeostasis model assessment - insulin resistance and beta-cell function from fasting plasma-glucose and insulin concentrations in man. Diabetologia. 1985;28:412–419. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- 39.Kendzierski D., Decarlo K.J. Physical-activity enjoyment scale - 2 validation studies. J Sport Exerc Psychol. 1991;13:50–64. [Google Scholar]
- 40.Motl R.W., Dishman R.K., Saunders R., Dowda M., Felton G., Pate R.R. Measuring enjoyment of physical activity in adolescent girls. Am J Prev Med. 2001;21:110–117. doi: 10.1016/s0749-3797(01)00326-9. [DOI] [PubMed] [Google Scholar]
- 41.Motl R.W., Dishman R.K. Measuring enjoyment of physical activity in adolescent girls (vol 21, pg 110, 2001) Am J Prev Med. 2001;21 doi: 10.1016/s0749-3797(01)00326-9. 332-332. [DOI] [PubMed] [Google Scholar]
- 42.Martin M.K., Sharpe T.L. Analysis of three exercise adherence interventions on self-efficacy and goal orientation. Res Q Exerc Sport. 2006;77 A81-A81. [Google Scholar]
- 43.Martin M.K., Sharpe T.L. Analysis of three exercise adherence interventions on self-efficacy and goal orientation. Res Q Exerc Sport. 2006;77 A81-A81. [Google Scholar]
- 44.Rodgers W.M., Sullivan M.J.L. Task, coping, and scheduling self-efficacy in relation to frequency of physical activity. J Appl Soc Psychol. 2001;31:741–753. [Google Scholar]
- 45.McAuley E., Blissmer B., Katula J., Duncan T.E. Exercise environment, self-efficacy, and affective responses to acute exercise in older adults. Psychol Health. 2000;15:341–355. [Google Scholar]
- 46.Stensvold D., Tjonna A.E., Skaug E.A., et al. Strength training versus aerobic interval training to modify risk factors of metabolic syndrome. J Appl Physiol. 2010;108:804–810. doi: 10.1152/japplphysiol.00996.2009. 1985. [DOI] [PubMed] [Google Scholar]
- 47.Chinnock A. Validation of an estimated food record. Publ Health Nutr. 2006;9:934–941. doi: 10.1017/phn2005922. [DOI] [PubMed] [Google Scholar]
- 48.Rausch J.R., Maxwell S.E., Kelley K. Analytic methods for questions pertaining to a randomized pretest, posttest, follow-up design. J Clin Child Adolesc. 2003;32:467–486. doi: 10.1207/S15374424JCCP3203_15. [DOI] [PubMed] [Google Scholar]
- 49.Cohen J., Cohen P., West S.G., Aiken L.S. Routledge; Mahwah, NJ: 2013. Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences. [Google Scholar]
- 50.Cohen J. A power primer. Psychol Bull. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- 51.Myers J., Prakash M., Froelicher V., Do D., Partington S., Atwood J.E. Exercise capacity and mortality among men referred for exercise testing. N Engl J Med. 2002;346:793–801. doi: 10.1056/NEJMoa011858. [DOI] [PubMed] [Google Scholar]
- 52.Milanovic Z., Sporis G., Weston M. Effectiveness of high-intensity interval training (HIT) and continuous endurance training for VO2max improvements: a systematic review and meta-analysis of controlled trials. Sports Med. 2015;45:1469–1481. doi: 10.1007/s40279-015-0365-0. [DOI] [PubMed] [Google Scholar]
- 53.Howden E.J., Sarma S., Lawley J.S., et al. Reversing the cardiac effects of sedentary aging in middle age-A randomized controlled trial implications for heart failure prevention. Circulation. 2018;137:1549. doi: 10.1161/CIRCULATIONAHA.117.030617. -+ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Roxburgh B.H., Nolan P.B., Weatherwax R.M., Dalleck L.C. Is moderate intensity exercise training combined with high intensity interval training more effective at improving cardiorespiratory fitness than moderate intensity exercise training alone? J Sports Sci Med. 2014;13:702–707. [PMC free article] [PubMed] [Google Scholar]
- 55.Keating S.E., Johnson N.A., Mielke G.I., Coombes J.S. A systematic review and meta-analysis of interval training versus moderate-intensity continuous training on body adiposity. Obes Rev. 2017;18:943–964. doi: 10.1111/obr.12536. [DOI] [PubMed] [Google Scholar]
- 56.Irving B.A., Davis C.K., Brock D.W., et al. Effect of exercise training intensity on abdominal Visceral fat and body composition. Med Sci Sports Exerc. 2008;40:1863–1872. doi: 10.1249/MSS.0b013e3181801d40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kessler H.S., Sisson S.B., Short K.R. The potential for high-intensity interval training to reduce cardiometabolic disease risk. Sports Med. 2012;42:489–509. doi: 10.2165/11630910-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 58.Biddle S.J.H., Batterham A.M. High-intensity interval exercise training for public health: a big HIT or shall we HIT it on the head? Int J Behav Nutr Phy. 2015;12 doi: 10.1186/s12966-015-0254-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Thum J.S., Parsons G., Whittle T., Astorino T.A. High-intensity interval training elicits higher enjoyment than moderate intensity continuous exercise. PLoS One. 2017;12 doi: 10.1371/journal.pone.0166299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Jung M.E., Bourne J.E., Little J.P. Where does HIT fit? An examination of the affective response to high-intensity intervals in comparison to continuous moderate- and continuous vigorous-intensity exercise in the exercise intensity-affect continuum. PLoS One. 2014;9 doi: 10.1371/journal.pone.0114541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bartlett J.D., Close G.L., MacLaren D.P.M., Gregson W., Drust B., Morton J.P. High-intensity interval running is perceived to be more enjoyable than moderate-intensity continuous exercise: implications for exercise adherence. J Sports Sci. 2011;29:547–553. doi: 10.1080/02640414.2010.545427. [DOI] [PubMed] [Google Scholar]
- 62.Oliveira B.R.R., Slama F.A., Deslandes A.C., Furtado E.S., Santos T.M. Continuous and high-intensity interval training: which promotes higher pleasure? PLoS One. 2013;8 doi: 10.1371/journal.pone.0079965. [DOI] [PMC free article] [PubMed] [Google Scholar]