Abstract
Background:
the optimal treatment of acute type III-V acromioclavicular (A-C) Rockwood dislocations is still a matter of discussion in orthopaedic surgery.
Aim of the work:
retrospective and comparative evaluation of the clinical and radiographic results of three different surgical techniques for stabilization of A-C joint using tension band wiring, hook plate and TightRope.
Methods:
a consecutive series of patients, treated from January 2014 and November 2019, were divided into three groups according to the surgical method used. They were clinically and radiographically assessed and the results were compared with those present in the literature.
Results:
66 patients, with a mean age of 44.7 years, were enrolled with a mean follow-up of 37.7 months (range 6-58 months). All patients, regardless of the group, had satisfactory outcome. According to the DASH score, statistically significant difference favours the TightRope Group (TRG) fixation (p<0.005). The TRG showed the highest mean Constant score (96,1); there are no significative differences between the clinical scores of Hook Plate Group (HPG) and Tension Band Wiring Group (TBWG). However, these two methods showed numerous complications, especially metal-work mobilization and stiffness respectively.
Conclusions:
good results can be overall achieved with primary fixation by the three different surgical methods under investigation. The TightRope system exhibited some advantages such as higher clinical scores, early recovery of range of movements, longitudinal surgical incision with non-keloid scar, no need for a second surgery and lower rate of complications.
Keywords: acromioclavicular dislocation, acromioclavicular surgical treatment, acromioclavicular joint, coracoclavicular ligaments, shoulder surgery, dislocation, TightRope, hookplate
Introduction
The acromioclavicular (AC) joint is a diarthrosis situated between the lateral end of the clavicle and the medial part of the acromion. It has a tough articular capsule reinforced by a strong system of ligaments, and a fibrocartilaginous disc between the bony surfaces. The horizontal stability of the joint is secured by acromioclavicular anterior and superior ligaments, whereas the responsible for vertical stability are coracoclavicular (CC) ligaments (conoid and trapezoid ligament) (1). The AC joint dislocation (ACD) with a prevalence of 9-12% is a common shoulder girdle injury in active young adults (2,3). In most cases, these are caused by a direct fall on the ipsilateral shoulder tip, with the upper limb in adduction (4). The indirect mechanism of injury with an extended arm is rare (5). ACD may be classified either according to the degree of ligamentous or capsular damage, or on the basis of the direction of the dislocating force impressed onto the clavicle with respect to the scapula (6). Historically, the most widely used classification is the one proposed by Almann and Tossy (7), modified later by Rockwood (8,9), which divides AC dislocations into six types depending on several criteria. Type I is a sprain of the AC ligaments; Type II is a rupture of the AC ligaments with a sprain of the CC ligaments and a minor dislocation of the lateral end of the clavicle in a vertical direction with a subsequent enlargement of the coracoclavicular distance less than 25% compared with the other side; Type III involves tear of both AC and CC ligaments as well as the deltotrapezoid fascia, with a coracoclavicular distance increased from 25% to 100% compared with the other side; Type IV is a tear of both the AC and CC ligaments and a posterior displacement of the distal clavicle into the trapezoid muscle; in Type V there is a tear of both AC and CC ligaments and of the origin of the deltoid and insertion of the trapezius, with a superior dislocation of the lateral end of the clavicle and an increase of the coracoclavicular distance from 100% to 300% compared with the other side; Type VI injuries are the result of inferior displacement of the distal clavicle into the subcoracoid position. Optimal treatment of AC dislocations is still a matter of discussion (10). However, there is agreement about conservative treatment by using either a harness or a sling for types I and II ACD (11,12), whereas surgical treatments have been generally accepted as the gold standard for Rockwood IV-VI lesions (13,14). There is an ongoing debate on what constitutes the best treatment for grade III lesions (15-18). On the basis of available literature, surgical and conservative treatment might have a similar impact on functional recovery. The high functional demands of a younger patient and the request for shorter recovery times without deformity or cosmetic concerns have oriented many orthopaedic surgeons (19-21), including the Authors, towards a preferential surgical approach in these selected cases (Figure 1). Many operative techniques have been developed over the years and the optimal operative treatment is still a matter of discussion (22). In recent years, our institutions have introduced a relatively new method of non-rigid fixation with Kevlar threads (TightRope®, Arthrex) for the stabilisation of acromioclavicular dislocations. This study compares this technique with the two most commonly performed alternatives: tension band wiring and hook plate.
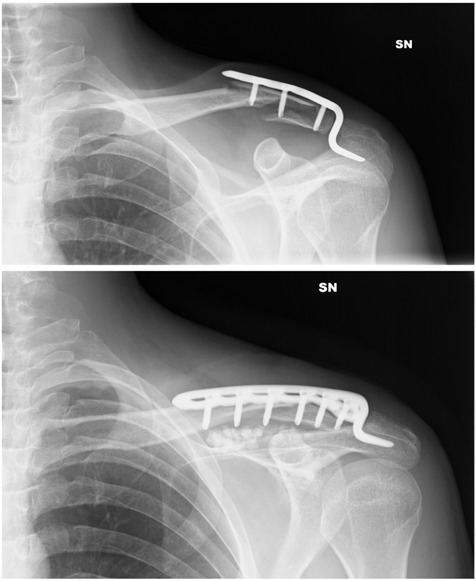
Figure 1.
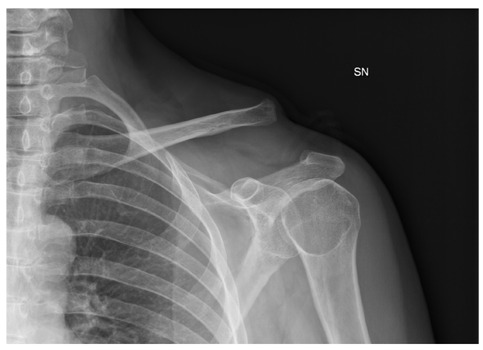
A case of left side acromioclavicular joint dislocation (Rockwood type V injury)
The aim of this study was to evaluate long-term clinical and radiological results of a consecutive series of patients diagnosed with acute ACD graded from III to V according to Rockwood classification treated by employing three different surgical methods of stabilization. Tension band wiring, hook plate and TightRope® groups are evaluated here, and the clinical and radiological results are compared between them and with those present in the literature in order to determine which surgical technique has a better outcome and to clarify the most adequate method of treatment
Materials and Methods
Here is reported a clinical retrospective and comparative study of a consecutive series of Caucasian patients with a diagnosis of type III, IV and V Rockwood ACD, hospitalized and surgically treated by one of the three techniques under investigation between January 2014 and November 2019 at our institutions.
All subjects participating in this study received a thorough explanation of the analysis and gave their oral and written informed consent to publish the data. The study was performed in accordance with the ethical standards (23).
Inclusion criteria were complete, acute, mono-lateral, isolated (mono-trauma) and painful ACD of type from III to V according to Rockwood et al. classification (7,8); patients between 18 and 70 years of age. Exclusion criteria were other traumas in the same arm, previous AC joint trauma, chronic AC joint dislocations, cerebral trauma, systemic disease (neuromuscular, rheumatic, psychiatric or metabolic disorders) and any other medical condition linked to range of movement reduction such as arthritis, rotator cuff tears and shoulder instability. All patients gave their written consent to undergo surgery.
According to the surgical treatment received, the patients were divided into 3 groups:
Tension-Band Wiring Group (TBWG);
Hook-Plate Group (HPG);
TightRope® Group (TRG).
Surgical procedures and treatment
All surgical treatments were performed by surgeons with expertise in trauma, prosthetics and arthroscopy of the shoulder joint (A.C. and M.F.), who chose one of the three different methods of fixation according to his personal preference and experience (Figure 2).
Figure 2.
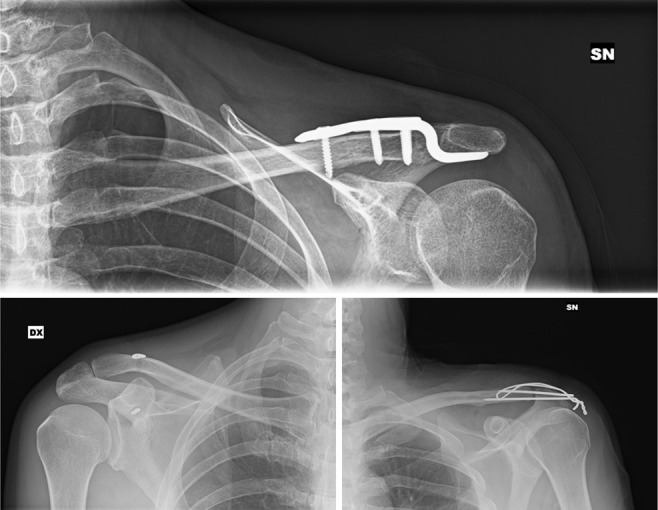
Pic collage of the three techniques under investigation
The operations were performed with the patients in the beach-chair position and using inter-scalene anaesthesia. Antibiotic prophylaxis was performed intraoperatively with 1g of Cefazolin and continued postoperatively at the dosage of 1g every 6h in the following 24 hours. No antithrombotic prophylaxis was used during the entire treatment.
-
Tension-Band Wiring Group
An anterior approach to the AC joint is created with a transverse incision starting from the clavicle to just above the AC joint and further up to the apex of the acromion. The dislocation is reduced with pointed forceps and stabilised with two k-wires inserted onto the lateral aspect of the clavicle, down to the cortex, in order to increase stability of the apical mechanical block avoiding loss of reduction. A hole is drilled along the sagittal plane of the clavicle and a Mittelmeier wire is inserted (24). The wire is then tied and trimmed, as are the k-wires at their ends, to be then buried in the bony cortex. Soft tissues are approximated in layers in order to cover the metalwork and minimise any further soft tissue injury.
-
Hook-Plate Group
An anterior approach, as above, was performed. The capsule was partially removed, together with the articular surface and the ligaments interposed in the intra-articular space, in order to create a space for the hook of the clavicular plate in the subacromial space. The dislocation was reduced and the plate end was then laid on the defect and secured with either compression or locking screws (25). The wound was then sutured in layers, taking care to reconstruct the muscular plane and particularly to repair the platysma at its clavicular insertion in order to avoid suboptimal cosmetic results.
-
TightRope® Group
An anterior approach to the shoulder with a 4-5 cm incision is made in a cranio-caudal direction starting from the lateral third of the clavicle down to the coracoid apophysis (Figure 3). After proceeding by blunt dissection down to the superior aspect of the coracoid, two blunt retractors are placed below of the apophysis. The centre of the superior surface of the coracoid is palpated and a 4.0mm hole is drilled in a cranio-caudal direction to allow for the passage of the TightRope® thread (Figure 4). Progressing up to the anterior margin of the clavicle, the deltoid and trapezium are sharply dissected, the centre of the superior surface of the clavicle is palpated and a 4.0mm hole is drilled in a precise cranio-caudal direction to ensure excellent tensioning of the construct. The TightRope® clip is now inserted through the two 4.0mm holes, from the clavicle to the coracoid, deep to the muscle belly of Pectoralis Major (Figure 5). The clip is flipped into a horizontal position just below the coracoid, the threads are drawn under tension and the button brought close to the superior surface of the clavicle (26). The dislocation should be reduced manually with controlled external manoeuvres and should be checked with an X-ray for the acromioclavicular space. When reduction is achieved, the implant is locked with a knot. The myo-tendinous flap raised during the approach will be useful at this point to cover the anchorage button and its safety knot on the superior surface of the clavicle.
Figure 3.
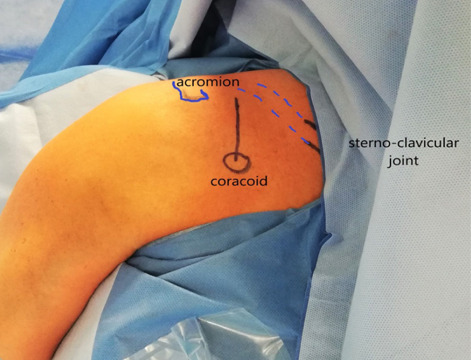
Shoulder region and line of incision.
Figure 4.
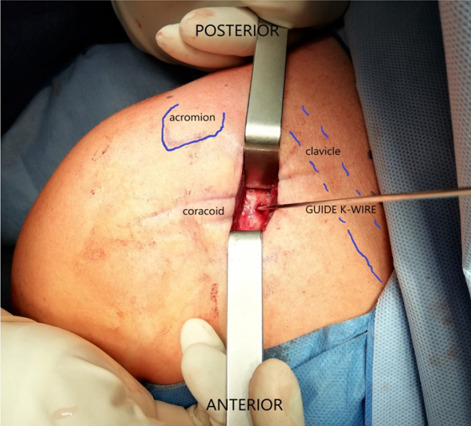
Coracoid, K wire used as guidewire prior to 4.5mm hole drilling.
Figure 5.
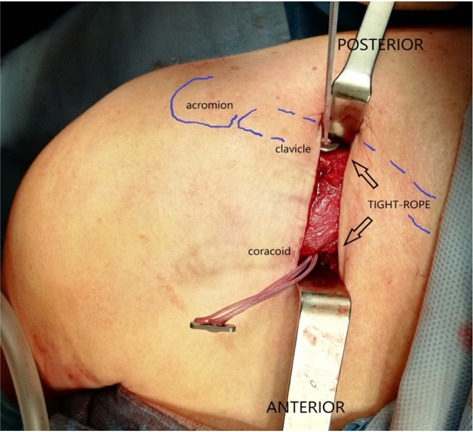
TightRope® clip is inserted
Post-operative care
Immediately after the operation, in all groups, the arm was immobilized with a Velpeau-type brace. The final X-ray was then carried out and the patient discharged within 24 hours. Follow-ups were then organised at day 7 for wound check and at day 15 for suture removal. The brace was kept in place for 21 days at the end of which it was removed, and an X-rays carried out. Further follow-ups and X-rays were then scheduled at 2- and 6-months post-op. Physiotherapy was started 3 weeks postoperatively with gradual return to normal daily activities.
The metalwork was removed at the time established by the personal indications of the treating surgeons. After the removal of the metalwork, the patients were sent for further physiatric evaluation and subsequent physiotherapy in different centres agreed upon with the hospital.
Clinical assessment
Both clinical and radiological analyses were carried out by the Authors.
Patients were examined for AC joint pain on palpation or during passive mobilization, instability during active mobilization or lifting weights, and the presence of deformity and keloids. Clinical function was assessed based on Constant score and a final score between 0 (no functionality) and 100 (full functionality) was obtained (27). Finally, patients were asked to fill the Disabilities of the Arm, Shoulder and Hand (DASH) self-assessing questionnaire (28). Rating 30 different symptoms and disabilities in the daily living, a final score between 100 (no disability) and 0 (full disability) was obtained. When required, patients who had undergone hook plate fixation or tension band wiring were followed up further and removal of metalwork was programmed. These cases were then followed up according to the same schedule as above.
Radiographic assessment
For the radiographic follow-up, the alignment of the AC joint was evaluated in the AP projection, in projection of Zanca (29) and also in comparative radiographs of both clavicles in the antero-posterior view. The aim was to assess recurrence of AC joint instability, defined as subluxation or clear re-dislocation. The outcome was dichotomized (yes or no) according to the presence of a complete anatomical reduction of the AC joint in both the coronal and the axial plane and compared to the controlateral side. Any mechanical and methodological failures of the metalwork, including migration, loosening and material breakage have been reported.
Statistical analysis
The data are summarized as arithmetic mean (range) for DASH-score and Constant-score. For the statistical analysis of the clinical scores obtained with the DASH and Constant questionnaires at the final follow-up, Kruskall-Wallis test and multiple comparation Dwass-Steel-Critchlow-Fligner test were applied. The DASH and Constant scores were analysed and compared to elucidate a statistically significant difference between the cohorts. All 3 groups were compared simultaneously and pairwise, to highlight the group with significantly different values. The two-tailed p-value was considered to be significative when <0.005.
Results
Patients’ data
A total of 66 patients, 55 males and 11 females were included in the study cohort with a mean age was 44.7 years (range 21-70). Concerning the degree of acromioclavicular dislocation, there were 48 cases grade III, 3 cases grade IV and 15 cases grade V. In 32 cases the right side was involved, while in 34 the left. The mean follow-up lasted 37.7 months (range 6-58).
-
Tension-Band Wiring Group
The TBWG included 19 men and 3 women with a mean age of 45.3 years (22-64). There were 20 cases grade III and 2 were grade V. The right side was involved in 11 cases and left in 11. All patients underwent removal of metalwork and the mean follow-up was 39.9 months (6-54 months). At the last follow-up, the mean DASH score was 95.8 (88.3-99.2) and the mean Constant score was 92.8 (81-100). In most cases, range of movement was complete, or at least very good, with full return to usual activities. Return to recreational and sports activities was once again partially limited by residual stiffness, the sensation of a somewhat ‘different’ arm, surgical wound paraesthesia and difficulty falling asleep on the operated side (Table 1). At the radiographic follow-up, displacement of k-wires with subsequent loss of reduction was reported in 8 cases (36,4%).
-
Hook-Plate Group
It included 16 men and 6 women with mean age of 48.2 years (22-70 years). 14 cases had a grade III dislocation, 2 had a grade IV and 6 had a grade V. The dislocation was on the right side in 9 cases, and on the left in 13 cases. 21 patients underwent removal of metalwork. Only one refused the procedure, due to satisfaction with own function. The mean follow-up lasted 41.3 months (6-58 months). At the last follow-up, the mean DASH and Constant scores were respectively 95.7 (91.7-98.3) and 92.7 (80-100). In many cases range of movement was complete, or very good, pain free and without mechanical blocks of notice. All cases fully returned to their activities of daily living. Minimal loss of internal rotation, strength and joint stiffness were common to all cases, with subsequent impact on recreational and sports activities. The sensation of the operated limb as somewhat ‘different’ from the contralateral, difficulty sleeping on such side, and mild paraesthesia on the surgical wounds were common to all cases. None of the patients suffered recurrence or loss of reduction at the radiographic follow-up.
-
TightRope® Group
This group included 20 men and 2 women with a mean age of 40.5 years (range 21-63). The degree of dislocation was: III for 14 cases, IV for just one, V for 7 cases. In 12 cases the right side was involved, the left in 10 cases. All patients have undergone only one procedure, and their follow-up was for a mean of 32.2 months (6-46 months). At the last clinical evaluation, the mean DASH score was 97.7 (87.5-100) while the mean Constant score was 96.1 (72-100). In many cases ROM was found to be complete, pain free, with return to activities of daily living without limitation. Some patients reported minimal abduction and internal rotation deficits limiting those sports activities requiring the highest degrees of mobility (such as volleyball, tennis and frisbee), minimum deficits in strength or the sensation of an arm somewhat ‘different’ from the other. In only one case suboptimal outcome was observed, with partial recovery of strength and function. From the radiographic point of view, only one patient (4,5%) suffered a recurrence diagnosed at 6 months, probably caused by breakage of the ropes or failure of safety knot
Table 1.
Data, clinical scores and complications
| Complications | |||||||||||||||
| Sex, Age (yr) | Side | Rockwood type | follow-up (mo) | Constant score (points) | DASH score (points) | n. of surgeries | implant pullout | loss of reduction | recurrence | loss of strenght | stiffness | keloid, scar imperfection | paresthesia | Implanted object discomfort | |
| TIGHT-ROPE | |||||||||||||||
| 1 | M, 48 | R | 5 | 46 | 100 | 98,3 | 1 | + | |||||||
| 2 | M, 35 | L | 3 | 45 | 95 | 97,5 | 1 | ||||||||
| 3 | F, 45 | R | 5 | 42 | 95 | 97,5 | 1 | ||||||||
| 4 | M, 63 | L | 3 | 42 | 100 | 98,3 | 1 | ||||||||
| 5 | F, 23 | L | 3 | 42 | 94 | 99,2 | 1 | ||||||||
| 6 | M, 35 | R | 3 | 41 | 72 | 87,5 | 1 | + | + | + | |||||
| 7 | M, 28 | L | 4 | 41 | 100 | 100,0 | 1 | ||||||||
| 8 | M, 58 | R | 5 | 41 | 100 | 98,3 | 1 | ||||||||
| 9 | M, 24 | R | 5 | 39 | 99 | 97,5 | 1 | ||||||||
| 10 | M, 44 | L | 5 | 37 | 95 | 98,3 | 1 | ||||||||
| 11 | M, 38 | R | 3 | 37 | 94 | 95,8 | 1 | + | + | ||||||
| 12 | M, 46 | R | 3 | 32 | 100 | 98,3 | 1 | + | |||||||
| 13 | M, 26 | R | 3 | 28 | 95 | 98,3 | 1 | ||||||||
| 14 | M, 29 | R | 3 | 28 | 90 | 98,3 | 1 | ||||||||
| 15 | M, 27 | L | 3 | 27 | 100 | 100,0 | 1 | ||||||||
| 16 | M, 55 | R | 5 | 27 | 100 | 97,5 | 1 | ||||||||
| 17 | M, 56 | L | 3 | 26 | 93 | 97,5 | 1 | ||||||||
| 18 | M, 52 | R | 3 | 21 | 95 | 99,2 | 1 | + | |||||||
| 19 | M, 63 | R | 3 | 20 | 98 | 99,2 | 1 | ||||||||
| 20 | M, 21 | L | 5 | 19 | 99 | 99,2 | 1 | + | + | ||||||
| 21 | M, 48 | L | 3 | 16 | 100 | 97,5 | 1 | ||||||||
| 22 | M, 28 | L | 3 | 6 | 100 | 96,7 | 1 | + | |||||||
| HOOK-PLATE | |||||||||||||||
| 1 | M, 70 | R | 3 | 57 | 97 | 98,3 | 2 | ||||||||
| 2 | M, 46 | L | 3 | 52 | 95 | 96,2 | 2 | + | + | ||||||
| 3 | M, 60 | R | 5 | 53 | 92 | 98,3 | 2 | + | |||||||
| 4 | M, 68 | L | 3 | 56 | 100 | 98,3 | 2 | + | |||||||
| 5 | M, 56 | L | 5 | 51 | 83 | 95,8 | 2 | + | + | ||||||
| 6 | M, 44 | L | 3 | 58 | 80 | 91,7 | 3 | + | + | + | + | ||||
| 7 | M, 43 | R | 3 | 49 | 94 | 96,7 | 2 | + | + | ||||||
| 8 | F, 32 | R | 4 | 45 | 91 | 95,5 | 2 | + | + | ||||||
| 9 | F, 24 | L | 3 | 46 | 100 | 96,7 | 2 | ||||||||
| 10 | F, 57 | L | 5 | 44 | 91 | 92,5 | 2 | + | + | + | + | ||||
| 11 | F, 22 | L | 5 | 42 | 100 | 98,3 | 2 | + | |||||||
| 12 | M, 44 | R | 3 | 37 | 93 | 95,8 | 1 | + | + | ||||||
| 13 | M, 51 | L | 3 | 46 | 91 | 94,3 | 2 | + | + | ||||||
| 14 | M, 69 | R | 3 | 39 | 95 | 93,3 | 2 | + | + | ||||||
| 15 | M, 47 | L | 3 | 38 | 95 | 98,2 | 2 | ||||||||
| 16 | M, 59 | R | 5 | 33 | 92 | 98,3 | 2 | + | |||||||
| 17 | M, 62 | L | 3 | 35 | 98 | 98,3 | 2 | + | |||||||
| 18 | M, 58 | L | 5 | 41 | 87 | 91,8 | 2 | + | + | + | |||||
| 19 | M, 42 | L | 3 | 28 | 92 | 95,7 | 2 | + | + | ||||||
| 20 | M, 43 | R | 3 | 27 | 94 | 96,7 | 2 | + | |||||||
| 21 | F, 35 | R | 4 | 10 | 90 | 92,5 | 2 | + | + | ||||||
| 22 | F, 28 | L | 3 | 6 | 89 | 91,7 | 2 | + | + | ||||||
| K-WIRES | |||||||||||||||
| 1 | M, 54 | L | 3 | 54 | 94 | 97,5 | 2 | + | |||||||
| 2 | M, 62 | L | 3 | 53 | 100 | 99,2 | 2 | + | |||||||
| 3 | M, 51 | R | 3 | 52 | 81 | 88,3 | 3 | + | + | + | + | + | |||
| 4 | M, 31 | R | 3 | 54 | 97 | 95,8 | 2 | + | |||||||
| 5 | F, 54 | R | 3 | 50 | 95 | 97,5 | 2 | + | + | + | + | + | |||
| 6 | M, 51 | L | 3 | 45 | 81 | 94,2 | 2 | + | |||||||
| 7 | M, 46 | L | 3 | 43 | 95 | 95,8 | 2 | + | + | + | + | ||||
| 8 | M, 42 | R | 3 | 47 | 97 | 98,3 | 2 | + | |||||||
| 9 | M, 36 | L | 3 | 43 | 94 | 96,7 | 2 | + | |||||||
| 10 | M, 22 | R | 3 | 50 | 95 | 97,5 | 2 | + | |||||||
| 11 | M, 35 | R | 5 | 38 | 92 | 92,5 | 2 | + | + | ||||||
| 12 | F, 64 | L | 5 | 41 | 92 | 92,5 | 2 | + | + | ||||||
| 13 | M, 59 | L | 3 | 34 | 94 | 97,5 | 2 | ||||||||
| 14 | M, 62 | L | 3 | 36 | 90 | 89,2 | 3 | + | + | + | + | + | + | ||
| 15 | M, 57 | R | 3 | 39 | 91 | 98,3 | 2 | + | + | + | |||||
| 16 | M, 29 | R | 3 | 43 | 97 | 96,8 | 2 | + | |||||||
| 17 | F, 42 | R | 3 | 41 | 95 | 97,5 | 2 | + | |||||||
| 18 | M, 53 | L | 3 | 32 | 83 | 94,2 | 2 | + | + | + | + | ||||
| 19 | M, 49 | L | 3 | 34 | 93 | 95,3 | 2 | + | |||||||
| 20 | M, 45 | R | 3 | 26 | 95 | 96,3 | 2 | + | + | ||||||
| 21 | M, 36 | L | 3 | 17 | 94 | 97,2 | 2 | + | + | ||||||
| 22 | M, 27 | R | 3 | 6 | 97 | 98,5 | 2 | + | |||||||
Comparison between groups
All 3 groups were compared simultaneously and one by one, to highlight the group with significantly different values (Table 2). From the DASH and CONSTANT score analysis, there are no significative differences between the hook-plate and tension band wiring groups. In comparison with the two groups mentioned above, the TightRope® fixation group reports better DASH questionnaire scores for questions 27, 28 and 30. Such questions probe specifically for residual weakness, stiffness and the sensation of a difference with the contralateral side. The scores for other questions are similar or better in comparison to the hook-plate and tension band wiring groups. In the comparison among two or three groups, a statistically significant difference favours the cases who underwent TightRope® fixation (Figure 6). From the analysis of Constant scores (Figure 7), TightRope®cases reported the highest results for full recovery of movement, particularly flexion and external rotation. The scores obtained for other parameters are uniformly equal or superior to those of the other two groups. The difference in scores obtained with this questionnaire is weakly significant when analysed across the three groups, and non-significant when two groups are compared. In this case, there is just a tendency to improved scores in the TightRope® subgroup.
Table 2.
Statistical analysis
| Constant Score | |||
| Comparison | p-value KW* test | p-value DSCF° test | Diff. medians (95% CI) |
| TIGHT vs. HOOK | 0.005 | 0.013 | 4.000 (1.000, 7.000) |
| TIGHT vs. KWIRES | 0.014 | 3.000 (1.000, 5.000) | |
| HOOK vs. KWIRES | 0.850 | 1.000 (-2.000, 3.000) | |
| Dash Score | |||
| Comparison | p-value KW* test | p-value DSCF° test | Diff. medians (95% CI) |
| TIGHT vs. HOOK | 0.001 | 0.003 | 1.800 (0.900, 3.400) |
| TIGHT vs. KWIRES | 0.005 | 1.700 (0.800, 2.800) | |
| HOOK vs. KWIRES | 0.910 | 0.100 (-0.900, 1.700) | |
| * Kruskal-Wallis test; ° Dwass, Steel, Critchlow-Fligner method for multiple comparisons | |||
Figure 6.
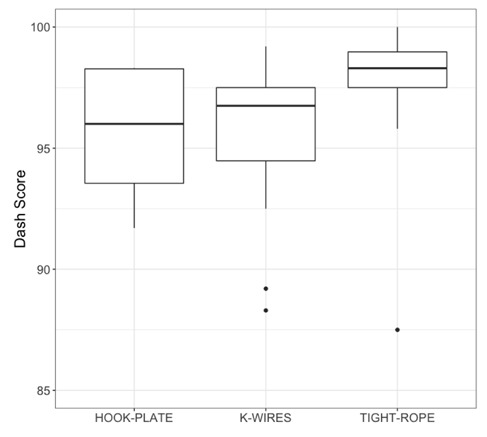
DASH score
Figure 7.
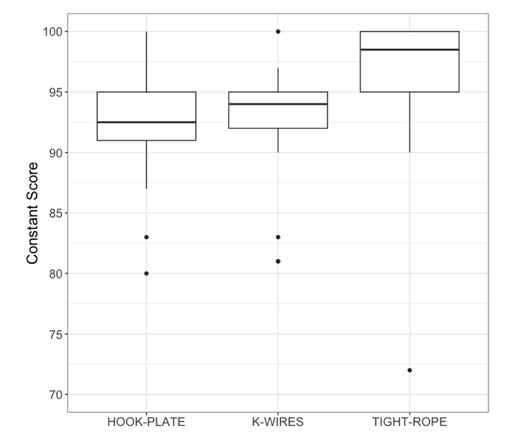
Constant score
Complications
From an anesthesiological point of view there were no reported complications. No cases of neurovascular injury, pneumothorax or iatrogenic fracture were reported. There were no cases of infections.
In the TBWG all patients required a second procedure for the removal of metalwork. Among the total 8 cases (36,4%) of loss of reduction, in 2 (9,1%) of them, k-wire breakage was observed 30 days post-op, with subsequent loss of reduction (Figure 8). In 3 cases (13,6%) early failure of k wires and dehiscence of the surgical wound were observed just a few days post-op. Such early loss of reduction required further tension band repositioning. Further to this, 4 cases (18,2%) suffered a loss of reduction after removal of metalwork. Once again, paraesthesia around the surgical wound was common, reported in 10 cases (45,5%). Deficit in strength were also common, reported in 9 cases (40,9%), the majority of which were those who suffered a loss of reduction or dissociation recurrence. Many patients (50%) complained of metalwork prominence, joint stiffness at the extremes of movement, limitations in recreational and sports activities and night time discomfort on the affected side.
Figure 8.
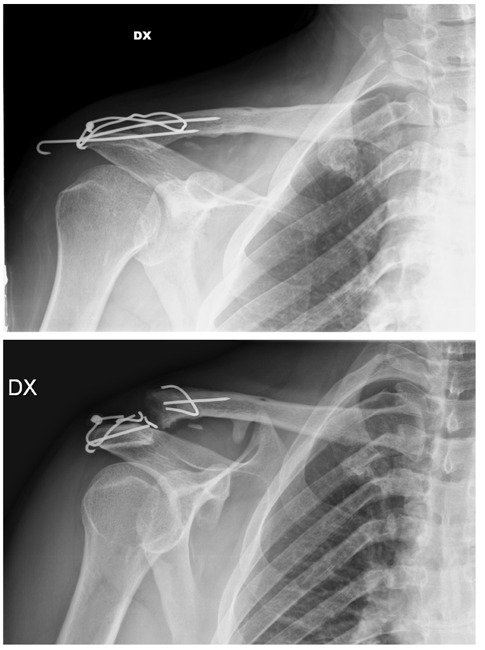
Displacement of K-wire, subsequently breakage of metalwork and loss of reduction
In the HPG the majority of patients (95,5%) required a further procedure for the removal of metalwork. Only one patient refused, still has the metalwork in place, but complains of discomfort during recreational activities or when carrying backpacks or heavy weights. One patient required metalwork revision due to a perioperative fracture and an undersized plate (Figure 9). None of the patients suffered recurrence or loss of reduction. Paraesthesia around the surgical wound were common and reported in 10 cases (45,5%). Strength deficits in comparison to the contralateral side were reported in 8 cases (36,4%). Most patients (54,5%) reported mechanical blocks caused by the plate, stiffness at the maximum degrees of movement, limitations in recreational and sports activities and discomfort lying on the operated side.
Figure 9.
2nd surgery, remove the short plate and put a longer one
In the TRG no one of the cases needed further surgery. Only one patient suffered a recurrence diagnosed at 6 months, probably caused by breakage of the ropes or failure of safety knot. On follow-up X-rays all metalwork appeared correctly placed. In one case (4,5%) loss of reduction and significant deficit in strength was observed. Isolated strength deficit was observed in 3 cases (13,6%). The most common complaint after TightRope® stabilisation was tactile awareness of button and safety knot. In 5 cases (22,7%) limitation in sports activities that require to carry weight (such as heavy backpacks) was reported. Only one patient (4,5%) complained of paraesthesia around the surgical wound.
Finally, the evaluation of surgical incision must be taken into great account. A surgical wound was deemed cosmetically suboptimal in the presence of a keloid or patient dissatisfaction. The short, longitudinal wound in TightRope®procedures was accepted by all patients, with no cases of keloid scar recorded. On the opposite, long transverse scars were found to be unacceptable in 9 (40,2%) of the cases treated with hook-plate and 7 (31,8%) of those treated with tension band wiring.
Discussion
Since the first procedure for AC joint repair proposed by Cooper in 1861 (30), more than 100 surgical methods have so far been described for acute injuries, but the ideal procedure remains controversial (10,31). We conceived this study in order to report our experience and to evaluate clinical, functional and radiological outcome of three different surgical techniques of stabilization using tension band wiring, hook plate and TightRope®. The main finding of the present report is that, despite the complications observed, good results can be overall achieved with primary fixation by the three different surgical methods under investigation (Table 2). Further, the statistical analyses of the DASH and Constant score do not reveal a significant difference (p > 0.05) between the hook-plate and tension band wiring groups, showing that these two methods are equally effective to restore the clinical function of the affected shoulder. A statistically significant difference in DASH score, conversely, favours the cases who underwent TightRope® fixation in the comparison among two or three groups. Moreover, from the analysis of Constant scores (Figure 7), all the parameters of TightRope® group are uniformly equal or superior to those of the other two groups, although the difference in overall score is weakly significant when analysed across the three groups, and non-significant when two groups are compared. In this case, there is just a tendency to improved scores in the TightRope® subgroup.
Our results are in agreement with previous reports, which compared different methods. Horst et al. (32) compared two groups of patients with a Rockwood III Type dislocation, one group treated with the TightRope® system and the other with K-wire fixation combined with additional ligament augmentation with sutures. Both groups (a total of 42 patients) achieved comparable functional, radiographic and pain severity-related outcomes. The Authors emphasized that the TightRope® system avoids the need to remove the material and involves shorter hospital stays, which is an advantage. We agree with their considerations and in the present study we obtained similar clinical data. Andreani et al. (33) carried out a retrospective study on 33 patients with AC dislocation treated with two different methodologies: the hook-plate and the TightRope® system, obtaining encouraging results, especially with the latter method; the mean Costant score was 90 (range 74–99) for the TightRope® group while for the hook-plate group was 75 (range 65–85). In our study we had a better Constant score for both groups, 96.1 (72-100) and 92.7 (80-100) respectively. This difference could be partly explained by the different sample size (66 of our study vs 33) and mean follow-up duration (37,7 months vs 24). Functional score similar to the one displayed by our HPG was described by Von Heideken et al. (34), which showed that the median Constant score of 37 patients treated with hook-plate was 91points, and by Kumar et al. (35), which obtained an average Constant score of 90.3 at 1 year follow-up in 33 male serving soldiers.
Despite the good clinical results, the principal criticisms of the K-wire and hook plate fixation methods regard the number of early and late complications, often due to the metalwork dislocation, ruptures or intolerance and the required removal of the implant before the patient can return to normal activities. These aspects were encountered also in the current study. For what concernsthe tension-band wiring, this technique is highly vulnerable to K-wire failure due to migration (13,6%) and breakage (9,1%). This is significant, as it leads to loss of reduction and recurrence of dislocation (36,4%). Further to this, loss of strength (40,9%), paresthesia (45,5%), cosmetically suboptimal wounds (31,8%) and discomfort for metalwork prominence are common with this approach. Due to these complications, the role of Kirschner wires for fixation of AC dislocation has been partially abandoned (36-38). Hook-plate fixation is associated with limitation of movement, as component design and positioning result in a mechanical block of the acromioclavicular joint (Figure 10). On the one hand, such technique of fixation has the advantage of achieving reduction in both the vertical and horizontal planes (39)and ensures adequate stabilisation brought about by fibrous tissue formation, as shown by the absence of loss of reduction cases before and after removal of metalwork displayed by our study. On the other hand, it may cause stiffness leading to loss of range of movement (54,5%). Such stiffness often improves with intensive physiotherapy once the metalwork is removed. Paraesthesia (45,5%) and poor cosmetic results (40,2%) are reported in almost half of cases. These findings are consistent with the literature. The hook-plate is described as a simple and reliable technique of fixation; however, there are several concerns: the plate may crowd and violate the subacromial space and produce impingement syndrome with rotator cuff injury, subacromial osteolysis, osteoarthritis of the AC joint, implant failure, wound infection and coraco-clavicular ossification (40-43). Usually removal of the plate improves the shoulder functional scores(40,44), but a second surgical intervention is a big disadvantages, in terms of inconvenience for the patients and economical burden. The TightRope® technique instead, allows for early, almost complete recovery of joint mobility and function. Consequently, there is less social and psychological strain on the patient able to return to his usual activities. In our report only one patient (4,5%) suffered a recurrence diagnosed at 6 months, probably caused by breakage of the ropes or failure of safety knot. As further advantage to this, TightRope® it requires only one surgical procedure. This is its strong point, considering the option of only one general anaesthetic, shorter surgical time, minimal blood loss, lower complications. In our study an isolated deficit of strength was observed in just 3 cases (13,6%), and only one patient complained of paraesthesia around the surgical wound (4,5%). These rates are remarkable lower than TBWG and HPG. In addition, the cosmetic part plays a strong role; there is also less social and psychological strain on the patient able to return to his usual activities. The vertical incision, only a few cm long, is more acceptable, particularly to women as they can conceal it under bra straps. In our experience there were no cases of keloid scar. The single downside of the TightRope® technique is the prominence of the button on the bony salience of the clavicle (22,7%). In lean patients with suboptimal tissue coverage, this tactile feedback might be an issue, as it may cause pressure discomfort in those activities involving lifting and carrying heavy weights. Finally, all the clinical scores of TightRope® group are uniformly equal or superior to those of the other two groups. Several studies have reported good to excellent results with this method. In a systematic review and meta-analysis, Arirachakaran et al. (45) compared the clinical outcomes and complications of the loop suspensory fixation devices, including tightrope, with hook plate fixation for the treatment of acute AC joint injury. They found that in a short-term period, loop suspensory fixation had higher postoperative Constant score and lower postoperative pain level. The TightRope® technique may be preferential to hook-plate according to a review by Qi et al. (46). The authors claim that TightRope® appears to be associated with better functional recovery and less pain and in addition, it does not increase the risk of reduction loss, coraco-clavicular distance, or operation time. Conversely, in a prospective randomized study carried out by Cai et al. (47), there was no significant difference between Constant scores of the TightRope® and hook-plate groups, but both achieved reasonable and satisfactory clinical and radiological outcomes. Moreover, patients with TightRope® fixations had complete AC joint re-dislocations in 10% of cases. The problem of early loss of reduction, despite the advantages of this technique, is prominent in the literaure. Mottaet al. (48) reported 20% of cases with loss of reduction at the follow-up due to rupture of the sutures running and a systematic review of Woodmass et al. (49) displayed a dislocation rate in the literature of 8.0% using the fixation technique and it is closer to the one showed by our paper (4,5%). In addition, TightRope® technique requires bicortical holes in the clavicle and the coracoid, which may in some rare case produce fracture, as reported by Gerhardt andWalz (50,51). Anyhow, in our study we have not found any fractures. Recently, arthroscopic TightRope® techniques have been described and different studies have reported good clinical and radiological outcomes (52,53). However, this procedure is not free of complications (49,52,53) and requires a long learning curve, therefore it is restricted to experienced shoulder arthroscopists (54). One of the strenghts of this study is that the analyzed procedures were always performed by the same two surgeons (A.C, M.F). Follow-up was adequately prolonged even after the removal of metalwork (plate and tension band wiring). This allows for a truly accurate evaluation of shoulder function. Some points of weakness should be acknowledged:the number of patients in the sample is limited. Patients assigned to conservative treatment were not included, although it would have been interesting to analyse these alongside the available data. It should be pointed out that the operator were also in charge of the data analysis, which is undeniably a potential source of bias.
Figure 10.
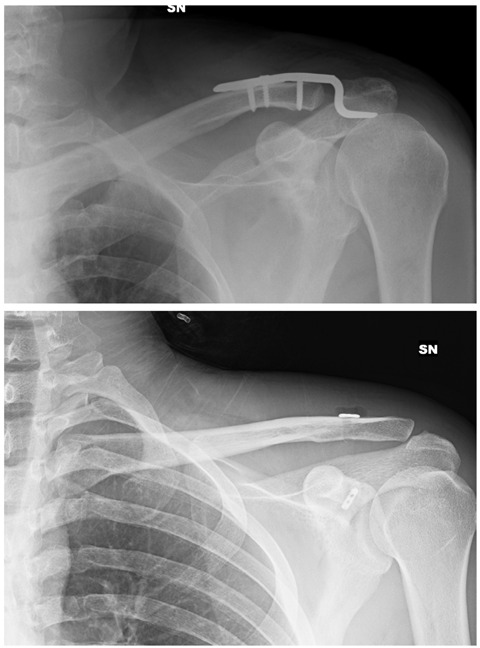
Hook plate and TightRope ®, a radiographic example of what mechanic block means
Conclusions
All three techniques under evaluation for the treatment of Rockwood grade III, IV and V acromioclavicular dislocation have scored highly on clinical tests. Therefore, all three techniques are adequate for surgical management in the acute setting. From the results of our study, the TightRope® technique has some advantages over the other two. It requires a single procedure, a smaller and cosmetically acceptable wound, less local complications (such as metalwork failure, surgical wound dehiscence and recurrence of dissociation) leading to rapid mobilisation which in turn favours early range of movement recovery. Based on an adequate learning curve, a wider dissemination and utilisation of such technique is desirable.
Ethics approval and consent to participate:
This study was performed in accordance with the ethical standards of the 1964 Declaration of Helsinki as revised in 2001. The patients received a thorough explanation of this study and gave their oral and written informed consent to be included in this analysis.
Consent for publication:
The patients gave their oral and written informed consent for the publication of their anonymous and clustered data and anonymous pictures.
Conflicts of interest:
Each author declares that he has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article.
Research materials:
Any research materials of this study are available at our institution and can be accessed.
References
- Babhulkar A, Pawaskar A. Acromioclavicular joint dislocations. Curr Rev Musculoskelet Med. 2014;7:33–9. doi: 10.1007/s12178-013-9199-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teodoro RL, Nishimi AY, Pascarelli L, Bongiovanni RR, Velasco MA, Dobashi ET. Surgical treatment of acromioclavicular dislocation using the endobutton. Acta Ortop Bras. 2017;25(3):81–4. doi: 10.1590/1413-785220172503166657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb J, Bannister G. Acromioclavicular disruption in first class rugby players. Br J Sports Med. 1992;26:247–248. doi: 10.1136/bjsm.26.4.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rockwood CA., Jr . Injuries to the acromioclavicular joint. In: Rockwood CA Jr, Williams GR, Young DC, editors. Rockwood & Green’s fractures in adults. 4th ed. Philadelphia: Lippincott-Raven Publishers; 1996. [Google Scholar]
- Luis GE, Yong CK, Singh DA, Sengupta S, Choon DS. Acromioclavicular joint dislocation: a comparative biomechanical study of the palmaris-longus tendon graft reconstruction with other augmentative methods in cadaveric models. J Orthop surg Res. 2007;2:22. doi: 10.1186/1749-799X-2-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bannister GC, Wallace WA, Stableforth PG, et al. A classification of acute acromioclavicular dislocation: a clinical, radiological and anatomical study. Injury. 1992;23:194–6. doi: 10.1016/s0020-1383(05)80044-0. [DOI] [PubMed] [Google Scholar]
- Tossy JD, Mead NC, Sigmond HM. Acromioclavicular separations: useful andpractical classification for treatment. Clin Orthop Relat Res. 1963;28:111–119. [PubMed] [Google Scholar]
- Rockwood C. Injuries to the acromioclavicular joint. In: Ca R, Green D, editors. Fractures in adults. 2nd ed. Philadelphia, PA: JB Lippincott; 1984. pp. 860–910. [Google Scholar]
- Rockwood CA, Williams G, Young D. Disorders of the acromioclavicular joint. In: Rockwood CA, Matsen FA, editors. The shoulder. Fourth ed. Vol. 1. Philadelphia: WB Saunders; 2009. pp. 453–526. [Google Scholar]
- Modi C. S, Beazley J, Zywiel M. G, Lawrence T. M, Veillette C. J. H. Controversies relating to the management of acromioclavicular joint dislocations. Bone Joint J. 2013;95-B:1595–1602. doi: 10.1302/0301-620X.95B12.31802. [DOI] [PubMed] [Google Scholar]
- Larsen E, Bjerg-Nielsen A, Christensen P. Conservative or surgical treatment of acromioclavicular dislocation: a prospective, controlled, randomized study. J Bone Joint Surg [Am] 1986;68-A:552–555. [PubMed] [Google Scholar]
- Tamaoki MJ, Belloti JC, Lenza M, et al. Surgical versus conservative interventions for treating acromioclavicular dislocation of the shoulder in adults. Cochrane Database Syst Rev. 2010;8:CD007429. doi: 10.1002/14651858.CD007429.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein D, Day M, Rokito A. Current concepts in the surgical management of acromioclavicular joint injuries. Bull NYU Hosp Jt Dis. 2012;70:11–24. [PubMed] [Google Scholar]
- Costic RS, Labriola JE, Rodosky MW, Debski RE. Biomechanical rationale for development of anatomical reconstructions of coracoclavicular ligaments after complete acromioclavicular joint dislocations. Am J Sports Med. 2004;32:1929–36. doi: 10.1177/0363546504264637. [DOI] [PubMed] [Google Scholar]
- Smith TO, Chester R, Pearse EO, Hing CB. Operative versus non-operative management following Rockwood grade III acromioclavicular separation: a meta-analysis of the current evidence base. J Orthop Traumatol. 2011;12:19–27. doi: 10.1007/s10195-011-0127-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korsten K, Gunning AC, Leenen LPH. Operative or conservative treatment in patients with Rockwod type III acromionclavicular dislocation: a systematic review and update of current literature. Int Orthop. 2014;38:831–38. doi: 10.1007/s00264-013-2143-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang G, Zhang Y, Liu Y, Qin X, Hu J, Li X. Comparison of surgical and conservative treatment of Rockwood type-III acromioclavicular dislocation: A meta-analysis. Medicine (Baltimore) 2018;97(4):e9690. doi: 10.1097/MD.0000000000009690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gstettner C, Tauber M, Hitzl W, Resch H. Rockwood type III acromioclavicular dislocation: surgical versus conservative treatment. J Shoulder Elbow Surg. 2008;17:220–225. doi: 10.1016/j.jse.2007.07.017. [DOI] [PubMed] [Google Scholar]
- Ryhänen J, Niemelä E, Kaarela O, Raatikainen T. Stabilization of acute, complete acromioclavicular joint dislocations with a new C hook implant. J Shoulder Elbow Surg. 2003;12(5):442–5. doi: 10.1016/s1058-2746(03)00064-8. [DOI] [PubMed] [Google Scholar]
- Jerosch J, Filler T, Peuker E, Greig M, Siewering U. Which stabilization technique corrects anatomy best in patients with AC separation? An experimental study. Knee Surg Sports Traumatol Arthrosc. 1999;7:365–72. doi: 10.1007/s001670050182. [DOI] [PubMed] [Google Scholar]
- Lizaur A, Sanz-Reig J, Gonzalez-Parreño S. Long-term results of the surgical treatment of type III acromioclavicular dislocations: an update of a previous report. J Bone Joint Surg (Br) 2011;93(8):1088–92. doi: 10.1302/0301-620X.93B8.26775. [DOI] [PubMed] [Google Scholar]
- Johansen JA, Grutter PW, McFarland EG, Petersen SA. Acromioclavicular joint injuries: indications for treatment and treatment options. J Shoulder Elbow Surg. 2011;20(2 Suppl):70–82. doi: 10.1016/j.jse.2010.10.030. [DOI] [PubMed] [Google Scholar]
- World Medical Association. World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. Bulletin of the World Health Organization. 2001;79(4):373–374. [PMC free article] [PubMed] [Google Scholar]
- Ladermann A, Grosclaude M, Lubbeke A, Christofilopoulos P, Stern R, Rod T, et al. Acromioclavicular and coracoclavicular cerclage reconstruction for acute acromioclavicular joint dislocations. J Shoulder Elbow Surg. 2011;20:401–8. doi: 10.1016/j.jse.2010.08.007. [DOI] [PubMed] [Google Scholar]
- Ejam S, Lind T, Falkenberg B. Surgical treatment of acute and chronic acromioclavicular dislocation Tossy type III and V using the Hook plate. Acta Orthop Belg. 2008;74(4):441–445. [PubMed] [Google Scholar]
- Horst K, Dienstknecht T, Pishnamaz M, Sellei RM, Kobbe P, Pape HC. Operative treatment of acute acromioclavicular joint injuries graded Rockwood III and IV: risks and benefits in tight rope technique vs. k-wire fixation. Patient Saf Surg. 2013;7:18. doi: 10.1186/1754-9493-7-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987 Jan;214:160–4. [PubMed] [Google Scholar]
- Germann G, Wind G, Harth A. The DASH (Disability of Arm-Shoulder-Hand) Questionnaire--a new instrument for evaluating upper extremity treatment outcome. Handchir Mikrochir Plast Chir. 1999 May;31(3):149–52. doi: 10.1055/s-1999-13902. [DOI] [PubMed] [Google Scholar]
- Zanca P. Shoulder pain: involvement of AC joint (analysis of 1000 cases) Am J Roentgenol Radium Ther Nucl Med. 1971;112(3):493–506. doi: 10.2214/ajr.112.3.493. [DOI] [PubMed] [Google Scholar]
- Cooper ES. New method of treating long standing dislocations of the scapula-clavicular articulation. Am J Med Sci. 1861;1:389–392. [Google Scholar]
- Helfen T, Siebenbürger G, Ockert B, Haasters F. Therapy of acute acromioclavicular joint instability. Meta-analysis of arthroscopic/minimally invasive versus open procedures. Unfallchirurg. 2015;118:415–426. doi: 10.1007/s00113-015-0005-z. [DOI] [PubMed] [Google Scholar]
- Horst K, Garving C, Thometzki T, et al. Comparative study on the treatment of Rockwood type III acute acromioclavicular dislocation: Clinical results from the TightRope((R)) technique vs. K-wire fixation. Orthop Traumatol Surg Res. 2017;103(2):171–6. doi: 10.1016/j.otsr.2016.11.009. [DOI] [PubMed] [Google Scholar]
- Andreani L, Bonicoli E, Parchi P, Piolanti N, Michele L. Acromioclavicular repair using two different techniques. Eur J Orthop Surg Traumatol. 2012 doi: 10.1007/s00590-013-1186-1. DOI 10.1007/s00590-013-1186-1. [DOI] [PubMed] [Google Scholar]
- von Heideken J, Bostrom Windhamre H, Une-Larsson V, et al. Acute surgical treatment of acromioclavicular dislocation type V with a hook plate: superiority to late reconstruction. J Shoulder Elbow Surg. 2013;22:9–17. doi: 10.1016/j.jse.2012.03.003. [DOI] [PubMed] [Google Scholar]
- Kumar N, Sharma V. Hook-plate fixation for acute acromioclavicular dislocations without coracoclavicular ligament reconstruction: a functional outcome study in military personnel. Strategies Trauma Limb Reconstr. 2015;10:79–85. doi: 10.1007/s11751-015-0228-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leidel BA, Braunstein V, Kirchhoff C, et al. Consistency of long-term outcome of acute Rockwood grade III acromioclavicular joint separations after K-wire transfixation. J Trauma. 2009;66:1666–1671. doi: 10.1097/TA.0b013e31818c1455. [DOI] [PubMed] [Google Scholar]
- Ejeskar A. Coracoclavicular wiring for acromioclavicular joint dislocation. A ten year follow-up study. Acta Orthop Scand. 1974;45:652–61. doi: 10.3109/17453677408989674. [DOI] [PubMed] [Google Scholar]
- Franssen BB, Schuurman AH, Van der Molen AM, Kon M. One century of Kirschner wires and Kirschner wire insertion techniques: a historical review. Acta Orthop Belg. 2010;76(1):1–6. [PubMed] [Google Scholar]
- Ladermann A, Gueorguiev B, Stimec B, Fasel J, Rothstock S, Hoffmeyer P. Acromioclavicular joint reconstruction: a comparative biomechanical study of three techniques. J Shoulder Elbow Surg. 2013;22:171–178. doi: 10.1016/j.jse.2012.01.020. [DOI] [PubMed] [Google Scholar]
- Chen CH, Dong QR, Zhou RK, Zhen HQ, Jiao YJ. Effects of hook plate on shoulder function after treatment of acromioclavicular joint dislocation. Int J Clin Exp Med. 2014;7(9):2564–70. [PMC free article] [PubMed] [Google Scholar]
- Lin HY, Wong PK, Ho WP, et al. Clavicular hook plate may induce subacromial shoulder impingement and rotator cuff lesion – dynamic sonographic evaluation. J Orthop Surg Res. 2014;9:6. doi: 10.1186/1749-799X-9-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sim E, Schwarz N, Hocker K, Berzlanovich A. Repair of complete acromioclavicular separations using the acromioclavicular-hook plate. Clin Orthop Relat Res. 1995;314:134–42. [PubMed] [Google Scholar]
- Kienast B, Thietje R, Queitsch C, et al. Mid-term results after operative treatment of Rockwood grade III-V acromioclavicular joint dislocations with an AC-hook-plate. Eur J Med Res. 2011;16:52–56. doi: 10.1186/2047-783X-16-2-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nadarajah R, Mahaluxmivala J, Amin A, Goodier DW. Clavicular hook-plate: complications of retaining the implant. Injury. 2005;36:681–3. doi: 10.1016/j.injury.2004.08.010. [DOI] [PubMed] [Google Scholar]
- Arirachakaran A, Boonard M, Piyapittayanun P, Kanchanatawan W, Chaijenkij K, Prommahachai A, et al. Post-operative outcomes and complications of suspensory loop fixation device versus hook plate in acute unstable acromioclavicular joint dislocation: a systematic review and meta-analysis. J Orthop Traumatol. 2017;18(4):293–304. doi: 10.1007/s10195-017-0451-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi W, Xu Y, Yan Z, Zhan J, et al. The Tight-Rope Technique versus Clavicular Hook Plate for Treatment of Acute Acromioclavicular Joint Dislocation: A Systematic Review and Meta-Analysis. J Invest Surg. 2019 May;14:1–10. doi: 10.1080/08941939.2019.1593558. [DOI] [PubMed] [Google Scholar]
- Cai L, Wang T, Lu D, Hu W, Hong J, Chen H. Comparison of the tight rope technique and clavicular hook plate for the treatment of Rockwood type III acromioclavicular Joint Dislocation. J Invest Surg. 2017;31(3):226–33. doi: 10.1080/08941939.2017.1305022. [DOI] [PubMed] [Google Scholar]
- Motta P, Maderni A, Bruno L, et al. Suture rupture in acromioclavicular joint dislocations treated with flip buttons. Arthroscopy. 2011;27:294–298. doi: 10.1016/j.arthro.2010.09.009. [DOI] [PubMed] [Google Scholar]
- Woodmass JM, Esposito JG, Ono Y, et al. Complications following arthroscopic fixation of acromioclavicular separations: a systematic review of the literature. Open Access JSports Med. 2015;6:97–107. doi: 10.2147/OAJSM.S73211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerhardt DC, VanDerWerf JD, Rylander LS, McCarty EC. Postoperative coracoid fracture after transcoracoid acromioclavicular joint reconstruction. J Shoulder Elbow Surg. 2011;20(5):e6–10. doi: 10.1016/j.jse.2011.01.017. [DOI] [PubMed] [Google Scholar]
- Walz L, Salzmann GM, Fabbro T, et al. The anatomic reconstruction of acromioclavicular joint dislocations using 2 TightRope devices: a biomechanical study. Am J SportsMed. 2008;36:2398–2406. doi: 10.1177/0363546508322524. [DOI] [PubMed] [Google Scholar]
- Natera-Cisneros L, Sarasquete-Reiriz J, Escolà-Benet A, Rodriguez-Miralles J. Acute high-grade acromioclavicular joint injuries treatment: arthroscopic non-rigid coracoclavicular fixation provides better quality of life outcomes than hook plate ORIF. Orthop Traumatol Surg Res. 2016;102:31–39. doi: 10.1016/j.otsr.2015.10.007. [DOI] [PubMed] [Google Scholar]
- Scheibel M, Dröschel S, Gerhardt C, Kraus N. Arthroscopically assisted stabilization of acute high-grade acromioclavicular joint separations. Am J Sports Med. 2011;39:1507–1516. doi: 10.1177/0363546511399379. [DOI] [PubMed] [Google Scholar]
- El Sallakh SA. Evaluation of arthroscopic stabilization of acute acromioclavicular joint dislocation using the TightRope system. Orthopedics. 2012;16:18–22. doi: 10.3928/01477447-20111122-13. [DOI] [PubMed] [Google Scholar]


