Abstract
The outbreak of coronavirus disease 19 (COVID-19) has dramatically imposed healthcare systems to reorganize their departments, including neurological wards. We aimed to describe the rearrangements made by stroke units (SU) and neurological intensive care units (ICU) in several German community and university hospitals facing the pandemic. This cross-sectional, survey-based, nationwide study collected data of 15 university and 4 community hospitals in Germany, being part of IGNITE Study Group, from April 1 to April 6, 2020. The rearrangements and implementation of safety measures in SUs, intermediate care units (IMC), and neurological ICUs were compared. 84.2% of hospitals implemented a separated area for patients awaiting their COVID-19 test results and 94.7% had a dedicated zone for their management. Outpatient treatment was reduced in 63.2% and even suspended in 36.8% of the hospitals. A global reduction of bed capacity was observed. Hospitals reported compromised stroke treatment (52.6%) and reduction of thrombolysis and thrombectomy rates (36.8%). All hospitals proposed special training for COVID-19 management, recurrent meetings and all undertook measures improving safety for healthcare workers. In an unprecedented global healthcare crisis, knowledge of the initial reorganization and response of German hospitals to COVID-19 may help finding effective strategies to face the ongoing pandemic. (www.actabiomedica.it)
Keywords: COVID-19, neuro-ICU, healthcare reorganization and repurposing
Introduction
The spread of the novel coronavirus responsible for the infection termed as ‘Coronavirus disease’ (COVID-19) is overwhelming and straining the healthcare systems globally. The steadily increasing number of infected patients is flooding the bed capacity of hospitals, resulting in shortage of personal protection equipment and the need for additional workforce in healthcare. Unprecedented reorganization measures within the wards still take place to increase the admission of COVID-19 patients, in particular in emergency departments and the intensive care setting (1).
Symptoms are predominantly respiratory but a neurotropism of the pathogen seems possible as well (2,3). The virus has been found in CSF and in brain tissue on autopsy (4) and various neurological conditions associated have been described. As an effect of the COVID-19 pandemic, neurological departments have been rearranged, particularly the stroke and neuro-intensive care units (2,5-7).
Similar to other European countries, Germany has implemented drastic restrictions on everyday life. Together with the patients’ epidemiological characteristics (such as distribution of age groups), the effects of the containment measures and the reorganization of the departments may have been crucial in determining the relatively low death rate recorded for the population of Germany (8). Being different from most other countries, most neurological departments in Germany do not only consist of stroke (SU) and intermediate care units (IMC), but also of neurological intensive care units (ICU). In order to assess the different approaches concerning neurological treatment in hospitals affected by COVID-19, we designed a survey aimed at evaluating the rearrangements applied by SUs and neurological ICUs in community and university hospitals.
Material and Methods
This survey was designed as a nationwide cross-sectional study. The existence of a SU and/or a neurological ICU in the hospital was the sole inclusion criteria for being enrolled in the study. Both university and community hospitals, which are members in the Initiative of the German Neuro-Intensive Trial Engagement (IGNITE) Study Group, were asked to complete the survey questionnaires (Supplemental Material) by a consulting neurologist for each center. The survey was conducted from April 1 to April 6 in 2020. Responses beyond this time limit were excluded to ensure the comparability of results considering the highly evolving and dynamic situation. The questionnaire consisted of 15 questions, with 13 of them requiring a binary and 2 of them a short open answer. Depending on the replies, additional items were available, forming other 15 dichotomous/numeral answers. Items were conceived to understand how the hospitals had been affected by the COVID-19 pandemic and which measures had already been taken to manage the ongoing outbreak. Some of the questions involved a subjective interpretation on how the pandemic has been impacting patient care as well as the medical staff.
Statistical analysis
Continuous and categorical variables were expressed as frequency with according percentages, respectively. The reliability of the questionnaire was evaluated by means of the Cronbach’s alpha coefficient. Chi-squared or Fisher’s exact test were performed to analyse categorical variables. Figures with p-values lower than 0.05 were considered as statistically significant. All statistical analyses were conducted by means of the commercial software SPSS (version 24.0, IBM Corporation, Armonk, NY, USA).
Results
The questionnaire proved to be reliable, with an acceptable alpha coefficient of 0.74. Nineteen (63.3%) out of 30 hospitals replied on time and were included, consisting of 14 university and 5 community hospitals (Table 1).
Table 1.
Replies to the questionnaire broken for community and university hospitals.
| Item | Community hospital | University hospital | ||
| No | Yes | No | Yes | |
| Does your hospital have a stroke unit? | 0 (0.0%) | 5 (100.0%) | 0 (0.0%) | 14 (100.0%) |
| Did you already treat SARS-CoV-2 infected patients at your stroke unit? | 4 (80.0%) | 1 (20.0%) | 12 (85.7%) | 2 (14.3%) |
| Does your stroke unit have a dedicated team of medical staff (physicians, nurses) for the management of COVID-19 patients? | 5 (100.0%) | 0 (0.0%) | 9 (64.3%) | 5 (35.7%) |
| Are all admitted patients tested for SARS-CoV-2? | 4 (80.0%) | 1 (20.0%) | 7 (50.0%) | 7 (50.0%) |
| Does your hospital have a neurological IMC unit? | 2 (40.0%) | 3 (60.0%) | 7 (50.0%) | 7 (50.0%) |
| Did you already treat SARS-CoV-2 infected patients at your IMC unit? | 1 (33.3%) | 2 (66.7%) | 6 (85.7%) | 1 (14.3%) |
| Does your IMC unit have a dedicated team of medical staff (physicians, nurses) for COVID-19 patients? | 1 (33.3%) | 2 (66.7%) | 2 (28.6%) | 5 (71.4%) |
| Are all admitted patients tested for SARS-CoV-2? | 1 (33.3%) | 2 (66.7%) | 4 (57.1%) | 3 (42.9%) |
| Does your hospital have a neurological ICU? | 2 (40.0%) | 3 (60.0%) | 1 (7.1%) | 13 (92.9%) |
| Did you already treat SARS-CoV-2 infected patients at your ICU? | 3 (100.0%) | 0 (0.0%) | 12 (92.3%) | 1 (7.7%) |
| Does your ICU have a dedicated team of medical staff (physicians, nurses) for COVID-19 patients? | 3 (100.0%) | 0 (0.0%) | 9 (69.2%) | 4 (30.8%) |
| Are all admitted patients tested for SARS-CoV-2? | 2 (66.7%) | 1 (33.3%) | 6 (46.2%) | 7 (53.8%) |
| Have you already executed rearrangements regarding bed capacity during the COVID-19 pandemic? | 0 (0.0%) | 5 (100.0%) | 2 (14.3%) | 12 (85.7%) |
| Does your hospital/department have a separated area for patients with unknown SARS-CoV-2-status, waiting for the test result (e.g. floating area)? | 1 (20.0%) | 4 (80.0%) | 2 (14.3%) | 12 (85.7%) |
| Did your hospital/department create a dedicated ward for COVID-19-patients? | 0 (0.0%) | 5 (100.0%) | 1 (7.1%) | 13 (92.9%) |
| Did your hospital/department take any measures in order to enable higher security distances between patients or medical staff? | 0 (0.0%) | 5 (100.0%) | 0 (0.0%) | 14 (100.0%) |
| Did your hospital/your department reduce neurological outpatient treatment? | 0 (0.0%) | 2 (reduced; 40.0%); 3 (suspended; 60.0%) | 0 (0.0%) | 10 (reduced; 71.4%); 4 (suspended; 28.6%) |
| Do you believe that the COVID-19-pandemic has compromised treatment of stroke patients? | 2 (40.0%) | 3 (60.0%) | 7 (50.0%) | 7 (50.0%) |
| Did you observe a decrease of cases of thrombolysis / thrombectomy at your hospital during the ongoing COVID-19 pandemic? | 4 (80.0%) | 1 (20.0%) | 8 (57.1%) | 6 (42.9%) |
| Did your hospital/department train nurses and physicians regarding a safe approach towards COVID-19 patients (i.e. correct use of protective equipment) | 0 (0.0%) | 5 (100.0%) | 0 (0.0%) | 14 (100.0%) |
| Did your hospital/department schedule frequent staff meetings regarding COVID-19? | 0 (0.0%) | 5 (100.0%) | 0 (0.0%) | 14 (100.0%) |
| Does your hospital/department offer psychotherapeutic assistance for the medical staff regarding COVID-19 cases? | 1 (20.0%) | 4 (80.0%) | 8 (57.1%) | 6 (42.9%) |
SARS-CoV-2 = Severe Acute Respiratory Syndrome – CoronaVirus – 2; COVID-19 = Coronavirus Disease 2019; ICU = Intensive Care Unit; IMC = Intermediate Care
The majority of hospitals (84.2%) had implemented a separated area for patients awaiting testing and measures were undertaken by all hospitals in order to ensure higher safety and security distances. 94.7% of hospitals had implemented a dedicated COVID-19 area (Figure 1).
Figure 1.
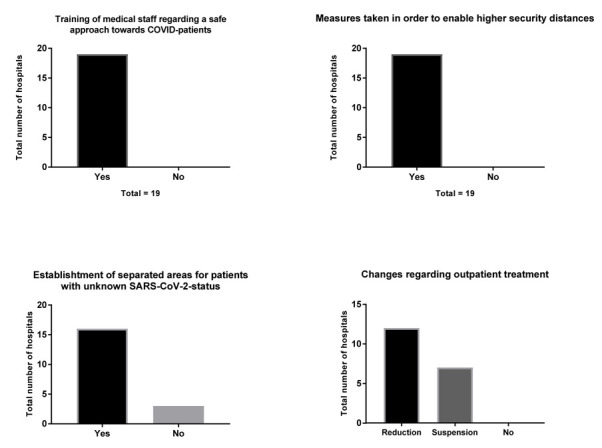
Main rearrangements during the COVID-19 pandemic
A reorganization was carried out with rearrangements of bed capacity, reduced outpatient treatment and a little decrease in neurological ICUs (from 170 to 166 beds) as well as SUs (from 242 to 226 beds) and IMC beds (from 68 to 66 beds). Outpatient treatment was reduced in 63.2% and completely suspended in 36.8% of hospitals. Stroke treatment was compromised in 52.6% of hospitals and a reduction of treatments was reported by 36.8% of them (Figure 2).
Figure 2.
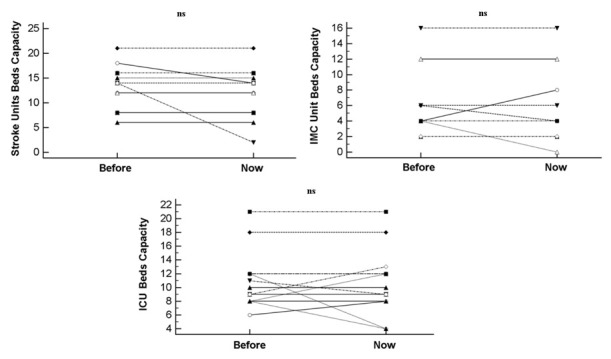
Bed Capacity rearrangement before and during the COVID-19 pandemic.
All hospitals had implemented special training for medical staff regarding a safe approach to the management of the COVID-19 patients, with frequent staff meetings focusing on new information about COVD-19. Noteworthy, 56.2% of hospitals provided psychotherapeutic assistance for the medical staff.
No differences between community and university hospitals could be detected for any variable (Table 1). Earlier treatment of infected patients in the hospitals’ SUs or neurological IMCs was associated with a lower probability that the hospital/department had created a dedicated COVID-19 ward (p=0.0209) and had reduced or suspended neurological outpatient treatment (p=0.0162). In SUs and neurological IMCs with a dedicated COVID-19 team fewer stroke treatments were performed (p=0.0233 and p=0.0202, respectively).
Discussion
Being the first, this work provides detailed information how the ongoing COVID-19 pandemic has affected operational processes in SUs and neurological ICUs in hospitals in Germany.
All hospitals implemented measures to prevent the spread of the virus among healthcare staff and hospitalized patients such as separated areas for patients with unknown COVID-19 status, dedicated wards for COVID-19 patients, frequent meetings, and special training for medical staff regarding a safer approach towards patients, and enabling larger security distances. Results are in line with the literature (9). Furthermore, we observed a slight, but not significant decrease in bed capacity because of the attempt to isolate and manage COVID-19 patients and to stop the spread of infections. Bed reorganization, mostly in neurological ICUs, was possible because of the quantity of semi-intensive and intensive care beds in Germany, being higher than in the rest of the world (10). Another important aspect is the reduction of outpatient treatments to secure the treatment of critically ill patients, and to implement social distancing. Currently, this remains acceptable, but a persistently protracted pandemic could result in an inadequate treatment of neurological chronic diseases.
Regarding acute stroke treatment, about one third of hospitals reported reduced IV thrombolysis/endovascular treatments, in line with other studies suggesting a decreased number of patients with TIA in emergency rooms (1). Despite the possibility of a temporary reduction of admission of acute strokes to emergency departments, it is extremely relevant to implement stroke pathways by creating protected code algorithm for patients with hyperacute stroke requiring urgent treatments (6,7).
During the study period, 42.1% of SUs tested every admitted patient, whereas 57.9% tested only symptomatic patients. This demonstrates that hospitals followed different approaches, rather than a unique global guideline. Finally, significantly decreased numbers of thrombolysis and endovascular treatment for acute stroke have been observed in hospitals with a dedicated COVID-19 team. Some patients with stroke, indeed, could have been referred to centers already prepared to manage the COVID-19 pandemic. In summary, German SUs, IMCs, and neurological ICUs have undergone important changes regarding daily operational processes. As the ending of the pandemic is not yet foreseeable, it is too early to evaluate the preventive effects of these rearrangements, as well as the impact on the usual clinical routine.
The major limitation of the study is that the survey captures a specific organizational phenomenon performed in a significant number of semi-intensive and intensive neurological settings, but it is not comprehensive enough to assess the reorganization of the entire German healthcare system. Additionally, this cross-sectional study offers an initial and static snapshot of the situation, which develops constantly and dynamically. Finally, this scenario is specific for Germany and might not be suitable for other countries with different healthcare organizations and bed capacities.
In conclusion, we showed that the COVID-19 pandemic has imposed great changes on health care systems, in particular for the management of critically ill patients in neurological stroke and intensive care units. Our findings suggest that stroke treatment has been compromised in neurological departments, associated with reported decreasing numbers of thrombolysis/thrombectomy. Despite some limitations, we believe that our findings offers an overview on the initial reorganization and response of German hospitals to COVID-19.
Acknowledgements:
We would like to express our gratitude towards all participating centers (Klinikum Großhadern of the Ludwig Maximilian University of Munich, University Hospital Cologne, Charité University Hospital Berlin, University Hospital Bonn, University Hospital Frankfurt, University Hospital Leipzig, Saarland University Medical Center, University Hospital Würzburg, University Hospital Augsburg, University Hospital Regensburg, University Hospital Erlangen, University Hospital Rostock, University Hospital Jena, University Hospital Göttingen, Klinikum Kassel, Maria-Hilf-Klinikum Mönchengladbach, Klinikum Ingolstadt, Klinikum Ludwigshafen, Klinikum Darmstadt).
The study was performed at the Department of Neurology at Saarland University Medical Center in Homburg, Germany.
Appendix
Supplementary Material: Survey Preparation of German Stroke-Units and neurological ICUs during the COVID-19 pandemic
The spread of COVID-19, caused by the novel coronavirus (SARS-CoV-2) is associated with great challenges regarding capacity and equipment of hospitals, as well as it leads to demanding tasks for medical staff.
While COVID-19 patients usually present respiratory symptoms, there have been reports suggesting a possible neurotropism of the novel coronavirus. While it is too early to evaluate the impact of possible neurological manifestations directly caused by the virus, it seems obvious that the ongoing pandemic is affecting the treatment of neurological patients, especially the critically ill.
In order to evaluate different approaches concerning the management of neurological patients affected by COVID-19 in the future, we created the following survey and kindly ask you to answer to the questions. Altogether it takes less than five minutes to answer and most of the questions can be answered with ‘yes’ or ‘no’.
1. Which hospital do you work at?
2. Does your hospital have a stroke unit?
yes ○ no ○
If answered ‘yes’, please specify
- Usual bed capacity of your stroke-unit ____
- Current bed capacity of your stroke unit ____
- Did you already treat SARS-CoV-2 infected patients at your stroke unit?
yes ○ no ○
- Does your stroke unit have a dedicated team of medical staff (physicians, nurses) for the management of COVID-19 patients?
yes ○ no ○
- Are all admitted patients tested for SARS-CoV-2?
yes ○ no, only patients with corresponding symptoms ○
3. Does your hospital have a neurological IMC unit?
yes ○ no ○
If answered ‘yes’, please specify
- Usual bed capacity of your IMC unit ____
- Current bed capacity of your IMC unit ____
- Did you already treat SARS-CoV-2 infected patients at your IMC unit?
yes ○ no ○
- Does your IMC unit have a dedicated team of medical staff (physicians, nurses) for COVID-19 patients?
yes ○ no ○
- Are all admitted patients tested for SARS-CoV-2?
yes ○ no, only patients with corresponding symptoms ○
4. Does your hospital have a neurological ICU?
yes ○ no ○
If answered ‘yes’, please specify
- Usual bed capacity of your ICU ____
- Current bed capacity of your ICU ____
- Did you already treat SARS-CoV-2 infected patients at your ICU?
yes ○ no ○
- Does your ICU have a dedicated team of medical staff (physicians, nurses) for COVID-19 patients?
yes ○ no ○
- Are all admitted patients tested for SARS-CoV-2?
yes ○ no, only patients with corresponding symptoms ○
5. Have you already executed rearrangements regarding bed capacity during the COVID-19 pandemic? (If answered ‘yes’, please specify)
yes ○ ________________________________________________________________
no ○
6. Does your hospital/department have a separated area for patients with unknown SARS-CoV-2-status, waiting for the test result (e.g. floating area)?
yes ○ no ○
7. Did your hospital/department create a dedicated ward for COVID-19-patients?
yes ○ no ○
8. Did your hospital/department take any measures in order to enable higher security distances between patients or medical staff?
yes ○ no ○
9. Did your hospital/your department reduce neurological outpatient treatment?
yes, outpatient treatment was reduced ○
yes, outpatient treatment was suspended ○
no ○
10. Which ‘elective’ neurological services were preserved despite the ongoing pandemic?
11. Do you believe that the COVID-19-pandemic has compromised treatment of stroke patients?
Yes, treatment has been compromised moderately ○
Yes, treatment has been compromised severely ○
No, treatment has not been compromised ○
12. Did you observe a decrease of cases of thrombolysis / thrombectomy at your hospital during the ongoing COVID-19 pandemic?
yes ○ no ○
13. Did your hospital/department train nurses and physicians regarding a safe approach towards COVID-19 patients (i.e. correct use of protective equipment)
yes ○ no ○
14. Did your hospital/department schedule frequent staff meetings regarding COVID-19?
yes ○ no ○
15. Does your hospital/department offer psychotherapeutic assistance for the medical staff regarding COVID-19 cases?
yes ○ no ○
Conflicts of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article.
References
- Bersano A, Pantoni L. On being a neurologist in Italy at the time of the COVID-19 outbreak. Neurology Epub. 2020 Apr 3 doi: 10.1212/WNL.0000000000009508. doi: 10.1212/WNL.0000000000009508. [DOI] [PubMed] [Google Scholar]
- Helms J, Kremer S, Merdji H, et al. Neurologic Features in Severe SARS-CoV-2 Infection. N Engl J Med Epub. 2020 Apr 15 doi: 10.1056/NEJMc2008597. doi: 10.1056/NEJMc2008597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Y, Xu X, Chen Z, et al. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav Immun Epub. 2020 Mar 30 doi: 10.1016/j.bbi.2020.03.031. doi: 10.1016/j.bbi.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yashavantha Rao HC, Jayabaskaran C. The emergence of a novel coronavirus (SARS-CoV-2) disease and their neuroinvasive propensity may affect in COVID-19 patients. J Med Virol Epub. 2020 Apr 22 doi: 10.1002/jmv.25918. doi: 10.1002/jmv.25918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Majersik JJ, Reddy VK. Acute neurology during the COVID-19 pandemic: Supporting the front line. Neurology Epub. 2020 Apr 13 doi: 10.1212/WNL.0000000000009564. doi: 10.1212/WNL.0000000000009564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baracchini C, Pieroni A, Viaro F, et al. Acute stroke management pathway during Coronavirus-19 pandemic. Neurol Sci. 2020;41:1003–5. doi: 10.1007/s10072-020-04375-9. doi: 10.1007/s10072-020-04375-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khosravani H, Rajendram P, Notario L, Chapman MG, Menon BK. Protected Code Stroke: Hyperacute Stroke Management During the Coronavirus Disease 2019 (COVID-19) Pandemic. Stroke Epub. 2020 Apr 1 doi: 10.1161/STROKEAHA.120.029838. doi: 10.1161/STROKEAHA.120.029838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomson GA. COVID-19: Leaving Lockdown - Of Schrodinger, Cats, Testing and Masks. Int J Clin Pract Epub. 2020 Apr 21:e13519. doi: 10.1111/ijcp.13519. doi: 10.1111/ijcp.13519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung JC, Ho LT, Cheng JV, Cham EYK, Lam KN. Staff safety during emergency airway management for COVID-19 in Hong Kong. Lancet Respir Med. 2020;8:e19. doi: 10.1016/S2213-2600(20)30084-9. doi: 10.1016/S2213-2600(20)30084-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radtke JS, Götz J, Gielen S, et al. Bed capacity analysis for an intensive care unit: Retrospective analysis and projection for need of intensive care beds in over 65 year olds with selected cardiovascular diseases]. Article in German. Med Klin Intensivmed Notfmed Epub. 2020 Feb 18 doi: 10.1007/s00063-020-00663-6. doi: 10.1007/s00063-020-00663-6. [DOI] [PMC free article] [PubMed] [Google Scholar]


