Abstract
Patient: Male, 57-year-old
Final Diagnosis: Diabetic foot
Symptoms: Chronic ulcer • osteomyelitis • polymicrobial infection
Medication: —
Clinical Procedure: Bone scan • intravenous antibiotic • oral antibiotic • PET-CT • telemedicine
Specialty: Dermatology • Infectious Diseases • Podiatry
Objective:
Unusual setting of medical care
Background:
Wounds affect millions of people world-wide, with care being costly and difficult to deliver remotely. The ongoing COVID-19 pandemic highlights the urgent need for telehealth solutions to play a larger role as part of remote care strategies for patient monitoring and care. We describe our findings on the use of a patient-facing wound care app (Swift Patient Connect App, Swift Medical, Canada) as an innovative solution in remote wound assessment and management of a diabetic patient’s wound.
Case Report:
In February 2020, a 57-year-old man with type I diabetes and peripheral arterial disease presented with osteomyelitis in the left foot at the fifth metatarsal, arising from a chronic ulcer. The wound was deep, with purulent discharge and polymicrobial growth. A 6-week course of intravenous antibiotics was administered, with slow improvement of the wound. At a follow-up appointment in June 2020, The Patient Connect app was recommended to the patient to securely share calibrated images of his wound as well to communicate with his doctor. Between June 2020 and January 2021, wound closure was accurately monitored as part of the management of this diabetic foot infection. The app was also used in the management of 2 subsequent wounds and infection episodes.
Conclusions:
Use of the Swift Patient Connect App designed to monitor and manage wounds by a patient with diabetes and foot ulcer as part of a remote care strategy resulted in numerous benefits expressed by the patient. After initial adoption, 3 successive wounds were managed with a combination of in-person and telehealth visits complemented by the app. Incorporation of this technology as part of a novel telemedicine strategy promises to have an extensive impact on remote care delivery during the current COVID-19 pandemic and beyond.
Keywords: Artificial Intelligence, Diabetic Foot, Telemedicine, Wounds and Injuries
Background
Wounds affect millions of people world-wide, with care being costly and difficult to deliver remotely [1]. A major limitation in the delivery of telemedicine remains the difficulty that many doctors and care providers experience with being able to conduct adequate visual assessments of patient wounds remotely [2]. Currently, standard telehealth practice involves patients using their smartphones to transmit photographs of their wounds through direct messaging services to their care provider; such images are often poorly calibrated for size, color, and lighting, not to mention the lack of security using such an approach. Wound-related information is either communicated over telephone or through text messages, which suffers from a lack of standardization of descriptors for issues such as pain and presence of exudate. Therefore, for remote care delivery to match the level received through in-person appointments, there is an urgent need for patients to be able to easily capture high-quality images of their wounds, that also contains high-quality information content which can be securely shared.
Healthcare apps are specially designed applications for smart-phones with health-oriented functionality [2]. By one estimate, over 318 000 health-related apps are available for download [3]. The US Food and Drug Administration (FDA) defines software functions such as those found in mobile medical apps as “device software functions” (https://www.fda.gov/media/80958/download). In addition, to assist with adhering to relevant design, best practices, and usage considerations, the World Health Organization (WHO) has published guidelines on digital health interventions (https://www.ncbi.nlm.nih.gov/books/NBK541905/). Evidence from 2020 during the COVID-19 pandemic suggests it played a pivotal role in the widespread implementation of digital technologies in healthcare [4]. We previously developed a mobile app and dashboard (Swift™ Skin and Wound) specifically designed to accurately and reliably measure and document many aspects of wounds [5] (Figure 1A–1D). The system, which is registered as a clinical device with Health Canada (https://health-products.canada. ca/mdall-limh/dispatch-repartition.do?type=active) and the US FDA (https://fda.report/Company/Swift-Medical-Inc), uses machine-vision technology to automatically focus and calculate wound dimensions from images acquired by a smartphone’s camera, allowing users to obtain precise and consistent measurements. These capabilities have been demonstrated to reduce the time needed for and increase accuracy of patient wound assessments compared with the traditional paper-and-ruler method [6].
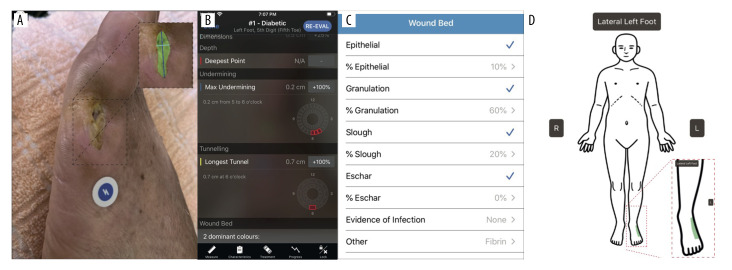
Figure 1.
Patient wound imaging, measurements, and progression tracking using the Swift Medical™ Skin and Wound App and Dashboard. (A) Example image of patient wound, taken using the Skin and Wound app. The app uses an adhesive fiducial marker (HealX™ calibrant), a Health Insurance Portability and Accountability Act, 1996 (HIPAA)-compliant, FDA and Health Canada certified Class I medical device placed next to the wound to automatically focus and acquire high-quality images, calibrate for color, lighting, and distancing when imaging. Note the image’s color calibration and focus. AI is used to automatically define the wound’s surface area (expanded box with wound area artificially shaded in green). All images are encrypted and stored in secure, cloud-based servers. (B) Screen shot showing wound-related metrics calculated by Skin and Wound app’s AI. (C) Image of wound-bed-related information taken from the dashboard. The app enables remote monitoring of high-risk individuals, offering insights into the healing process, including the tissue type present and its area. Patient identifiers (eg, name and unit number) are also accessible through the app’s dashboard, and treatment advice and care-related communications can be provided directly to the patient. (D) Human silhouette accessible through the HIPAA-compliant Skin and Wound healthcare provider dashboard showing the anatomical location of the wound, imaged by the patient.
In response to the increased reliance on remote appointments brought about by the COVID-19 pandemic [7], we have recently developed a stream-lined, patient-facing version of the app (Patient Connect, Figure 2A, 2B), designed for use by patients and/or their care providers using their own personal smartphones. In addition to being able to view a wound’s image series over time, additional information such as healing-associated metrics, wound-bed information, anatomical location, and patient identifiers can be viewed. We report the case of a patient with diabetes and multiple episodes of foot infections who was successfully managed using this app during the COVID-19 pandemic in 2020-2021. As well as reporting on their experiences, we present evidence demonstrating the app’s effectiveness in both remote care management and delivery.
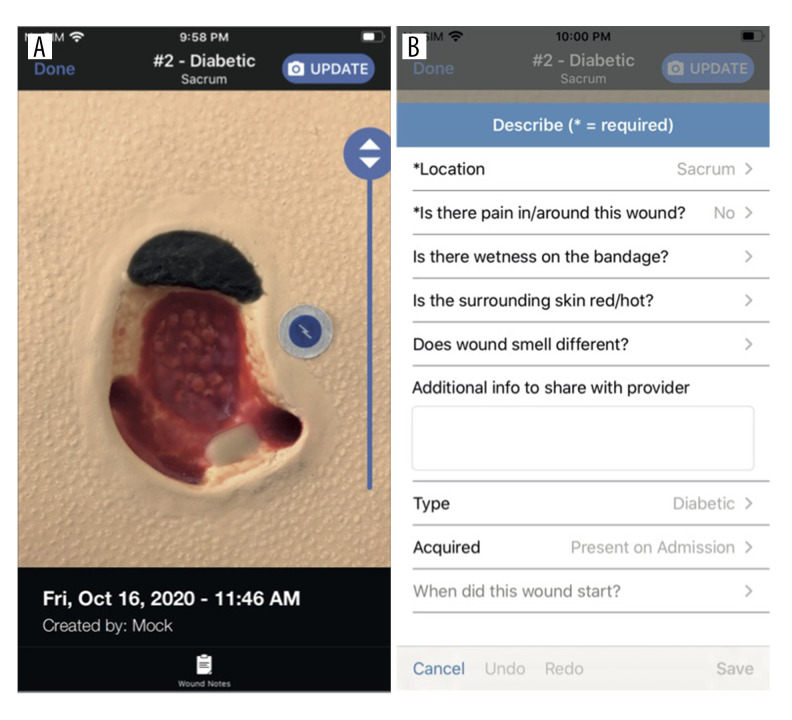
Figure 2.
Swift Medical Patient Connect App Interface. (A) Screen shot of an artificial wound captured using the Patient Connect App, which has more limited functionality compared to the Skin and Wound app: for example, wound measurements cannot be accessed by the patient/user of the Patient Connect app. (B) Screen shot of the Patient Connect app dashboard, indicating qualitative information fields that can be populated by the patient/user.
Case Report
In February 2020, a 57-year-old man with type I diabetes, coronary artery disease, chronic kidney disease, peripheral arterial disease, and prior toe amputation for infection presented with osteomyelitis in the left foot at the fifth metatarsal, arising from a chronic ulcer. The patient did not smoke, drink alcohol, or use recreational drugs. The wound was deep, with purulent discharge and polymicrobial growth, which included Pseudomonas aeruginosa. A 6-week course of intravenous ertapenem 500 mg (once daily) and oral ciprofloxacin 250 mg (twice daily) was administered, with slow improvement in the wound.
Between the patient’s first visit in February 2020 and early June 2020, he was followed via telephone at regular intervals.
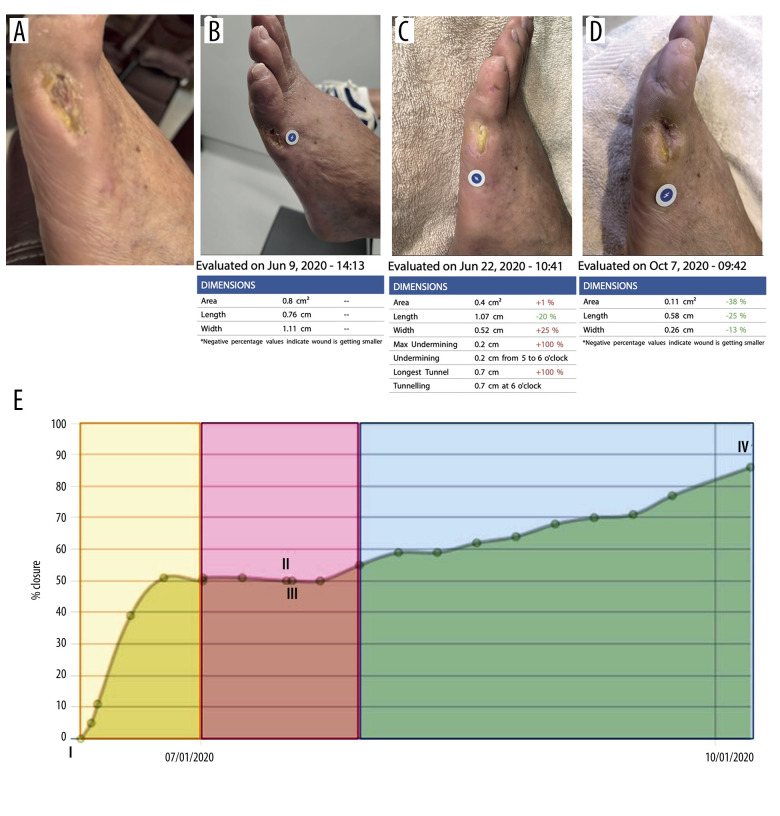
The attending physician and patient mutually agreed that the patient would provide photos via direct communication (text message or email) to allow wound assessment: despite ethical concerns regarding the sharing of the physician’s personal contact information, this was deemed crucial given the patient’s need for close follow-up and their reluctance to present for in-person follow-up in the pandemic context. During this 3-month period of remote follow-up, the patient shared 2 photographs of the wound: an example is shown in Figure 3A.
Figure 3.
Patient wound monitoring using the Skin and Wound platform. (A) Baseline photograph of patient’s wound associated with underlying osteomyelitis. Image was taken using the standard iPhone Camera App on an iPhone11 running iOS 14.0.1 and is representative of the 2 photographs shared by the patient between February and June 2020. Note the image’s lack of focus. The patient shared 2 images using the Camera App. (B) Image of the dashboard showing wound image and healing process-associated metrics, acquired on the date and at the time indicated. (C) Same as B except at the later date indicated. (D) Same as C, except at the later date indicated. (E) Closure graph viewed through the dashboard, automatically calculated from aggregated images of the wound over time. I, II, and IV indicate the dates when the images shown in B–D were captured. The timeframe highlighted in yellow indicates when the patient received antibiotics, which corresponded to enhanced healing of the wound. After the healing stalled (highlighted in pink), a tunnel wound was detected (III), resulting in wound debridement and the insertion of a mesh. This was followed by further closure of the wound (highlighted in blue). At IV, wound closure was calculated at 86%.
In June 2020, the patient reported pain and new discharge from the wound, which prompted an in-person visit on June 9, 2020. A bone and PET scan showed resolution of osteomyelitis, with soft-tissue inflammation. He was treated with another course of oral antibiotics (amoxicillin-clavulanate and ciprofloxacin). At this point, the patient agreed to download and use the Swift Medical Patient Connect App to capture and share images of the wound (Figure 3B–3D). As of January 2021, the patient had 7 additional telemedicine appointments and submitted a total of 39 images through the app, an almost 20-fold increase in sharing wound-related data compared to the situation before using the app. The wound gradually improved over this time, with objective decrease in size as measured by the app (Figure 3E). The patient subsequently developed 2 additional wounds in different locations and was followed again via the app, with ongoing use as of September 2021. Throughout a 1-year period as part of telehealth care, the app permitted the longitudinal monitoring and successful management of 3 infection episodes in a high-risk patient.
As wound assessment via the app occurred weekly, formal monitoring increased self-examination and engagement in preventive behavior such as monitoring for trauma and early signs of infection and off-loading wound pressure using orthotics. Owing to the patient’s comorbidities and the pandemic, he was reluctant to attend in-person appointments. Use of the app therefore reduced anxiety through reduced healthcare contact and surrounding risk of hospital-associated COVID-19 exposure. From the physician’s perspective, the increased frequency of images provided by the patient for review allowed real-time assessment of the wound, increasing physician confidence in remote wound monitoring.
Use of the Patient Connect App also helped realize time and cost savings. Total time and financial commitment from the patient per appointment averaged 3 hours and approximately $50 CAD, respectively: remote appointments eliminated both of these costs. For the physician, use of the Patient Connect App as part of the remote care strategy deployed resulted in a substantial time saving: the standard workflow ordinarily required to visually assess the wound, including positioning, dressing removal, and cleansing, was eliminated. The physician estimated that this reduced the time required from 30 to 15 minutes: if this modality were widely adopted, this would potentially allow twice the number of patients to be seen. In addition, the patient captured photos during visits by a local community service centre nurse who performed his routine dressing changes. As regular dressing changes remain an essential part of wound care, whether delivered in-person or remotely, the ease of imaging the wound as part of routine wound care in a standardized manner represented another time-saving factor.
Discussion
The COVID-19 pandemic has placed great importance on the use of novel strategies for remote care of patients [4]. Regular use of the Patient Connect App by the patient in this case report allowed remote monitoring of the wound and could potentially promote higher rates of adherence to treatment through engagement in preventive care and early wound detection. Access to the Patient Connect App is provided through a health care provider that has access to the Swift Medical solution through a licensing agreement; the Patient Connect App itself is free and there is no charge to the patient or caregiver using the app. The virtual appointments had no upfront cost for the patient, and the physician was remunerated for virtual visits via the healthcare system, similar to in-person visits, through a separate billing code.
Factors that would help the widespread adoption of this innovation include more evidence-based research from larger patient populations to demonstrate the app’s effectiveness and benefits in helping deliver remote care; patient education on the use of apps and general improvements in the familiarity of certain population groups (eg, the elderly) with technology; and access to high-speed internet, especially for rural/indigenous populations.
In the case reported, the patient explained that he shared an increased number of images because he felt comfortable using a formal, specially designed portal through which the physician was able to access images at their convenience. The patient found the app “educational and empowering”, consistent with an earlier study on patient wound-perception [8]. This observation is also consistent with a recent study describing the use of an mHealth tool facilitating remote assessment of digital ulcers, resulting in high levels of patient satisfaction [9]. Possession of and familiarity with a smartphone is an obvious pre-requisite for using this technology, but given their ubiquity, we do not envision this being a significant limitation. Presently, the Patient Connect App is being used in addition to other care practices, including telephone calls and in-person visits, which remain essential in the care of patients with wounds. If the app were to completely substitute for in-person visits, a major concern remains whether complications might be missed or wounds mis-diagnosed, resulting in administration of inappropriate treatments. Therefore, more research is required to determine if this innovation can provide a level of patient care comparable to standard care/ in-person appointments.
Telemedicine strategies have increasingly been used to monitor and treat diabetic foot ulcers (DFUs) [10]. A recent systematic review showed that photographic imaging of wounds is a valid, reliable, and feasible method for telehealth purposes [11]. At-distance photographic imaging of wounds is associated with good levels of patient adherence and timely referrals based on photographic assessments, thus leading to a favorable perception of usability [12]. However, the lack of consistent imaging regarding scale, focus, and lightning conditions has been tied to relatively low inter- and intra-observer reliability in the diagnosis of DFU complications based on mobile phone imaging [13]. Another systematic review [14] found that the use of mobile applications for monitoring DFUs led to increased community support and wound care knowledge, and helped empower patients. The study also concluded that a lack of technological savviness, non-user-friendly or non-intuitive apps, and lack of patient dexterity were significant hurdles to the widespread adoption of wound-care mobile applications.
A common concern over the use of smartphones as part of remote care strategies remains the security of patient data [15]. Prior to using the app, despite being able to directly contact the physician, the present patient considered sending images a potential imposition on the physician. The patient also felt uncomfortable that images would be sent via standard messaging and stored on the physician’s smartphone. In contrast, by storing images captured using the app on secure cloud-based servers, this reduced the patient’s anxiety about sharing images and facilitated the physician’s ability to rapidly and securely receive images. In addition, patient identifiers (eg, name and unit number) are accessible through the secure dashboard, and treatment advice and care-related communications can be provided directly to the patient using the app.
The Patient Connect App can be used by any patient treated for any condition involving a wound or skin condition that requires monitoring. Underscoring this point, the app is being used not only where we are based at McGill University Health Centre by colleagues and collaborators in the Division of Orthopedic Surgery and Diabetic Clinic, but has also been implemented at other hospitals such as the Jewish General Hospital, where this patient was treated, and in ambulatory settings (Ostomy care and pressure ulcer prevention, Centenary Hospital; Scarborough Health Network; Saint Elizabeth Health, Home and Community Care Support Services Central East; The Michener Institute; University Health Network) throughout Quebec and Ontario. In addition, the Patient Connect App has recently been licensed to a national health care system in the US, with the contract able to support up to 10 000 patients, which will ensure its impact in the short-to-medium term. Studies are underway to more rigorously determine the extent of time savings made through use of the app (eg, average number of days lost due to unplanned hospital admissions) and to investigate whether use of the app as part of a remote wound care strategy can deliver care comparable to or better than standard care/in-person appointments.
Conclusions
Here, we present the case of a 57-year-old man with type 1 diabetes mellitus and a chronic foot ulcer who was successfully managed with a remote patient-facing wound care smart-phone application. The use of an innovative patient-facing smart phone app designed to monitor and manage wounds by a patient with diabetes and foot ulcer resulted in numerous benefits. After initial adoption, 3 successive wounds were managed with a combination of in-person and telehealth visits complemented by the app. Incorporation of this technology as part of a novel telemedicine strategy promises to have an extensive impact on remote care delivery, during the current COVID-19 pandemic and beyond.
Footnotes
Department and Institution Where Work Was Done
Division of Infectious Diseases, Jewish General Hospital, Montreal, QC, Canada.
Declaration of Figures’ Authenticity
All figures submitted have been created by the authors who confirm that the images are original with no duplication and have not been previously published in whole or in part.
References:
- 1.Guest J, Fuller GW, Vowden P, et al. Cohort study evaluating pressure ulcer management in clinical practice in the UK following initial presentation in the community: costs and outcomes. BMJ Open. 2018;8(7):e021769. doi: 10.1136/bmjopen-2018-021769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang SC, Au Y, Ramirez-GarciaLuna JL, et al. The promise of smartphone applications in the remote monitoring of postsurgical wounds: A literature review. Adv Skin Wound Care. 2020;33(9):489–96. doi: 10.1097/01.ASW.0000694136.29135.02. [DOI] [PubMed] [Google Scholar]
- 3.IQVIA The Growing Value of Digit al Health: Evidence Impact on Human Health the Healthcare System Institute Report. IQVIA; 2017. Available at: https://www.iqvia.com/insights/the-iqvia-institute/reports/the-growing-value-of-digital-health.
- 4.Golinelli D, Boetto E, Carullo G, et al. Adoption of digital technologies in health care during the COVID-19 pandemic: Systematic review of early scientific literature. J Med Internet Res. 2020;22(11):e22280. doi: 10.2196/22280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang SC, Anderson JAE, Evans R, et al. Point-of-care wound visioning technology: Reproducibility and accuracy of a wound measurement app. PLoS One. 2017;12(8):e0183139. doi: 10.1371/journal.pone.0183139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Au Y, Beland B, Anderson JAE, et al. Time-saving comparison of wound measurement between the ruler method and the swift skin and wound app. J Cutan Med Surg. 2019;23(2):226–28. doi: 10.1177/1203475418800942. [DOI] [PubMed] [Google Scholar]
- 7.Webster P. Virtual health care in the era of COVID-19. Lancet. 2020;395(10231):1180–81. doi: 10.1016/S0140-6736(20)30818-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang SC, Anderson JA, Jones DV, et al. Patient perception of wound photography. Int Wound J. 2016;13(3):326–30. doi: 10.1111/iwj.12293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang J, Mihai C, Tüshaus L, et al. Wound image quality from a mobile health tool for home-based chronic wound management with real-time quality feedback: Randomized feasibility study. JMIR Mhealth Uhealth. 2021;9(7):e26149. doi: 10.2196/26149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Najafi B, Reeves ND, Armstrong DG. Leveraging smart technologies to improve the management of diabetic foot ulcers and extend ulcer-free days in remission. Diabetes Metab Res Rev. 2020;36(Suppl. 1):e3239. doi: 10.1002/dmrr.3239. [DOI] [PubMed] [Google Scholar]
- 11.Hazenberg CEVB, Aan de Stegge WB, Van Baal SG, et al. Telehealth and tele-medicine applications for the diabetic foot: A systematic review. Diabetes Metab Res Rev. 2020;36(3):e3247. doi: 10.1002/dmrr.3247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hazenberg CE, Bus SA, Kottink AI, et al. Telemedical home-monitoring of diabetic foot disease using photographic foot imaging – a feasibility study. J Telemed Telecare. 2012;18(1):32–36. doi: 10.1258/jtt.2011.110504. [DOI] [PubMed] [Google Scholar]
- 13.van Netten JJ, Clark D, Lazzarini PA, et al. The validity and reliability of remote diabetic foot ulcer assessment using mobile phone images. Sci Rep. 2017;7(1):9480. doi: 10.1038/s41598-017-09828-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Foong HF, Kyaw BM, Upton Z, et al. Facilitators and barriers of using digital technology for the management of diabetic foot ulcers: A qualitative systematic review. Int Wound J. 2020;17(5):1266–81. doi: 10.1111/iwj.13396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gunter RL, Chouinard S, Fernandes-Taylor S, et al. Current use of telemedicine for post-discharge surgical care: A systematic review. J Am Coll Surg. 2016;222:915–27. doi: 10.1016/j.jamcollsurg.2016.01.062. [DOI] [PMC free article] [PubMed] [Google Scholar]