Over the last decade, drug overdoses across Canada have skyrocketed, resulting in a tidal wave of preventable deaths. In 2017, the province of Alberta—as well as other Canadian provinces—funded supervised consumption services (SCS) as part of a multifaceted public health approach to mitigate the incidences of rising drug overdose deaths. SCS are facilities where adults can use preobtained illicit drugs under the supervision of trained staff. A key objective of SCS is to prevent overdose deaths. 1 Less recognized in the public media but notably, SCS objectives also include (i) facilitating referrals to health and social services (e.g., primary care, addiction treatment programs, housing, and income support services), (ii) providing naloxone training and substance use education, (iii) providing sterile injection equipment, and (iv) facilitating social interaction for marginalized populations. Authors of peer-reviewed literature tend to be generally supportive of SCS; however, most data on SCS have been collected from sites operating outside of Alberta. For example, authors of a systematic review of 75 studies conducted in Vancouver, Canada, and Sydney, Australia, suggested SCS typically: (i) reduce overdose deaths, (ii) increase access to health and social services, (iii) reduce the incidence of HIV and hepatitis C, (iv) a reduce improperly discarded syringes, and (v) are not associated with detrimental socioeconomic impacts to the adjacent community. 2
Despite this wealth of encouraging evidence, the utility of Alberta’s SCS has met skepticism from policymakers, with consequent fears among harm reduction advocates of SCS funding cuts or program cancelation. Alberta currently has seven SCS in four cities, the first opened in 2017. A 2020 Provincial government-led gray literature review 3 suggested that SCS in Alberta may not meet their aims in reducing overdose deaths, stating the following:
In many cases, “adverse events” (even if non-life threating or minor) are reported as overdoses, and the term “reversal” is used even when the response was a simple administration of oxygen. This leaves the public with an inference that without these sites thousands of people would fatally overdose or no longer be alive. Comparatively rare cases resulted in the use of naloxone. As a result, the committee became concerned with issues of transparency and accountability with the regards to the way overdose reversals are tracked and reported. The committee finds this misleading and the ambiguity and faulty reporting cannot responsibly make such a determination. 3
After reviewing the literature, we developed an a priori hypothesis that an increase of SCS visits in Alberta would be associated with a decrease in fentanyl-related overdose deaths. We then reviewed the publicly available opioid response reports from the Province of Alberta website (https://open.alberta.ca/publications/alberta-opioid-response-surveillance-report). In this quarterly reported data set, confirmed fentanyl-related deaths were determined by medical examiner’s reports, and SCS visits were recorded as number of total visits at each of the provincial SCS locations. In 2020, according to these data, opioids were involved in over 80% of all drug-related deaths, and fentanyl was involved in 94% of all opioid-related deaths. 4
Using a Pearson correlation, we found a statistically significant association between the number of total quarterly SCS visits and fentanyl-related overdose deaths (r = −0.643, df = 1, P = 0.028, two-tailed; Figure 1). Based on the basic data available, we were unable to control for effects of other public health initiatives that took place simultaneously such as: (i) take-home naloxone programs, (ii) changes in black market carfentanil availability, and (iii) increased access to addiction treatment and medications such as opioid agonist therapy. Nevertheless, data from the provincial report suggest that SCS have facilitated over 10,000 referrals to addiction treatment programs and account for 12.2% of all provincial naloxone kit dispensing. Further, SCS visits decreased by 64.3% during Q2 2020 in comparison with Q1 2020, while fentanyl-related overdoses increased by 118.4%. 4,5 This outlier may reflect a plethora of other complications associated with the COVID-19 pandemic such as poorer mental health, increased unemployment, and so on. Despite these limitations, the association is consistent with the findings from the systematic review although the review was based on data from other jurisdictions.
Figure 1.
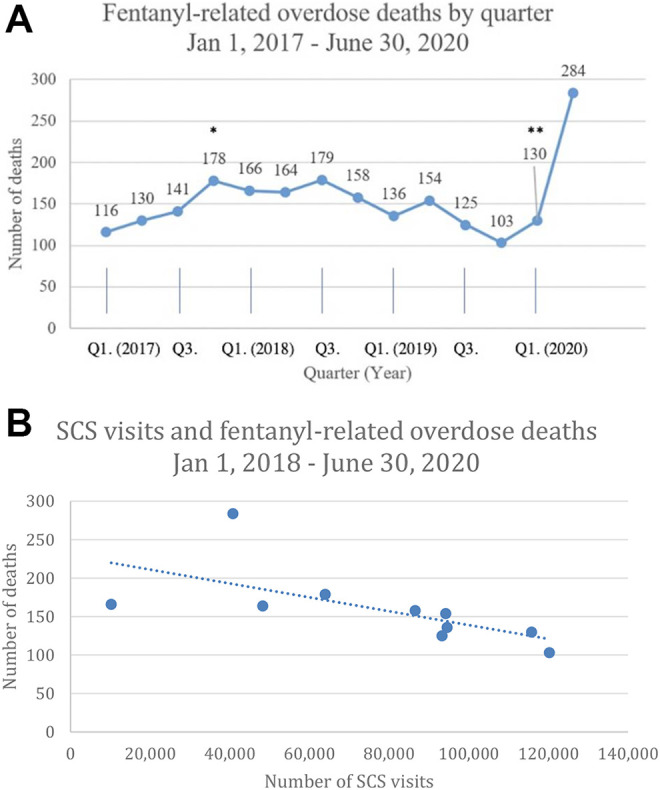
Fentanyl-related overdose deaths and SCS visits in Alberta: (A) Fentanyl-related overdose deaths 2017-2020 by quarter. * shows approximately when the first SCS opened in Alberta (around Q4 2017; however, the first SCS data became available Q1 2018). ** shows approximately when physical distancing policies associated with the COVID-19 pandemic began (around Q2 2020); (B) SCS visits and fentanyl-related overdose deaths by quarter after January 1, 2018. Please note that the x-axis is not in chronological order.
Based on our preliminary finding of a negative association of SCS visits in Alberta with decreased fentanyl-related overdose deaths, we call for more independent, peer-reviewed research to clarify the impact of SCS on overdose deaths in newly implemented SCS. Moreover, we suggest additional research to investigate novel ways in which SCS may further contribute to increased access and continuity of care for people who use drugs. We believe that future research in this area is urgent as the impact of two concurrent public health crises—the drug overdose crisis and the COVID-19 pandemic—continue to contribute to an overwhelming burden on the health care system.
Supplemental Material
Supplemental Material, sj-docx-1-cpa-10.1177_0706743721999571 for The Impact of Supervised Consumption Services on Fentanyl-related Deaths: Lessons Learned from Alberta’s Provincial Data by Tyler Marshall, Adam Abba-Aji, Robert Tanguay and Andrew J. Greenshaw in The Canadian Journal of Psychiatry
Acknowledgments
We would like to thank Dr. Sunita Vohra, Dr. Elaine Hyshka, and Jayelle Warken for their helpful comments on earlier versions of this manuscript.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Tyler Marshall, MPH https://orcid.org/0000-0002-7644-3639
Supplemental Material: The supplemental material for this article is available online.
References
- 1. Health Canada. Supervised consumption sites and services: explained. 2018. https://www.canada.ca/en/health-canada/services/substance-use/supervised-consumption-sites/explained.html
- 2. Potier C, Laprevote V, Dubois-Arber F, Cottencin O, Rolland B. Supervised injection services: what has been demonstrated? a systematic literature review. Drug Alcohol Depend. 2014;145:48–68. [DOI] [PubMed] [Google Scholar]
- 3. Health, Government of Alberta. Impact: a socio-economic review of supervised consumption sites in Alberta. 2020. https://open.alberta.ca/publications/9781460147054
- 4. Health, Government of Alberta. COVID-19 opioid response surveillance report: Q2 2020. Analytics and performance reporting. 2020. https://www.alberta.ca/substance-use-surveillance-data.aspx#toc-1
- 5. Health, Government of Alberta. Alberta opioid response surveillance report Q1 2020 analytics and performance reporting. 2020. https://www.alberta.ca/substance-use-surveillance-data.aspx#toc-1
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-docx-1-cpa-10.1177_0706743721999571 for The Impact of Supervised Consumption Services on Fentanyl-related Deaths: Lessons Learned from Alberta’s Provincial Data by Tyler Marshall, Adam Abba-Aji, Robert Tanguay and Andrew J. Greenshaw in The Canadian Journal of Psychiatry


