Abstract
Background and Purpose:
The impact of arterial ischemic events after intracerebral hemorrhage (ICH) on outcomes is unclear. This study aimed to evaluate the risk of death among ICH survivors with and without an incident arterial ischemic event.
Methods:
We performed a retrospective cohort study using claims data from Medicare beneficiaries with a non-traumatic ICH from January 2008 to October 2015. Our exposure was an arterial ischemic event, a composite of acute ischemic stroke or myocardial infarction (MI), identified using validated ICD-9-CM diagnosis codes. The outcome was mortality. We used marginal structural models to analyze the risk of death among ICH patients with and without an arterial ischemic event, after adjusting for confounders as time-varying covariates.
Results:
Among 8,804 Medicare beneficiaries with ICH, 2,371 (26.9%) had an arterial ischemic event. During a median follow-up time of 1.9 years (interquartile range, 0.7-3.9), ICH patients with an arterial ischemic event had a mortality rate of 21.7 (95% confidence interval [CI], 20.4-23.0) per 100 person-years compared to a rate of 15.0 (95% CI, 14.4-15.6) per 100 person-years in those without. In the marginal structural model, an arterial ischemic event was associated with an increased risk of death (hazard ratio [HR], 1.8; 95% confidence interval [CI], 1.6-1.9). In secondary analyses, the mortality risk was elevated after an ischemic stroke (HR, 1.7; 95% CI, 1.5-1.8), and MI (HR, 3.0; 95% CI, 2.4-3.8).
Conclusions:
We found that elderly patients who survived an ICH had an increased risk of death after a subsequent ischemic stroke or MI.
Keywords: intracerebral hemorrhage, ischemic stroke, myocardial infarction, death
Intracerebral hemorrhage (ICH) has high morbidity and mortality. 1 While nearly a third of patients die during the acute hospitalization of ICH, those who survive often make a substantial recovery years after the event. 2 Among ICH survivors, the risk of death in the first year is about 9.5%. 3 We and others have shown that ICH is associated with a 3 to 6-fold heightened risk of an ischemic stroke or myocardial infarction (MI), with the cumulative incidence of a major arterial event as high as 5.9% at the end of 1 year after ICH.4,5 In fact, acute vascular events are the second most common reason for readmissions after ICH.6,7 Whether these ischemic events influence outcomes among ICH survivors is poorly understood. Emerging data suggest that ischemic stroke or ischemic cardiovascular disease account for nearly 15% of deaths after ICH. 8 A better understanding of the prognostic significance of these ischemic events would support the need for better secondary stroke prevention strategies such as antiplatelet therapy, which are often contraindicated in the setting of an ICH. We therefore sought to explore the relationship between an arterial ischemic event and mortality among patients surviving hospitalization for acute ICH, in a large, heterogeneous, nationally representative cohort of Medicare beneficiaries.
Methods
Study Design
We performed a retrospective cohort study using inpatient and outpatient claims data on a 5% sample of Medicare beneficiaries, a dataset made available by the U.S. Centers for Medicare and Medicaid Services (CMS) which provides health insurance to a large majority of U.S. citizens 65 years of age and above. These de-identified data include up to 25 International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) diagnosis codes. 9 A unique and anonymous identifier code links multiple claims for a given patient, thus allowing for a comprehensive longitudinal analysis of each beneficiary’s care over time. Since a de-identified dataset was provided by CMS, individual patient consent did not apply to this study. The Weill Cornell Medicine institutional review board approved this study.
Data Sharing
The claims data used in this analysis are restricted per the terms of Medicare’s data use agreement and therefore cannot be shared directly with other investigators. However, investigators can obtain access to these data by application to the CMS.
Patient Population
We obtained data from inpatient and outpatient claims of Medicare beneficiaries between January 1, 2008 and September 30, 2015. We limited our cohort to beneficiaries with continuous coverage in traditional fee-for-service Medicare (both Parts A and B) for at least 1 year or until death, if applicable. 9 Although Medicare eligibility generally begins at 65 years of age, we included only patients 66 years or older in order to allow time for beneficiaries to enter medical care and for their providers to document any pre-existing medical comorbidities.
Measurements
We restricted our cohort to only those with a diagnosis of ICH, identified by the ICD-9-CM code 431.x in any diagnostic position, which has a sensitivity of 82% and a specificity of 93% as compared to medical record review.10,11 We excluded patients with any diagnosis codes for trauma, and those with a diagnosis of cerebrovascular disease (using the ICD-9-CM codes 430, 433.x1, 434.x1, and 436) or MI (using the ICD-9-CM code 410.x1) preceding the index hospitalization for ICH to prevent misclassification of chronic events. Patients were entered into the study after discharge from the index ICH hospitalization. Using previously used ICD-9-CM code algorithms, we also measured the following cardiovascular risk factors and relevant comorbidities: hypertension, diabetes, atrial fibrillation, congestive heart failure, valvular heart disease, peripheral vascular disease, chronic kidney disease, chronic obstructive pulmonary disease, alcohol abuse, and tobacco use. The burden of comorbidities was quantified using the Charlson comorbidity index,12,13 used extensively in previous studies of ICH to adjust for illness burden.14,15
The exposure was an arterial ischemic event, defined as a composite of acute ischemic stroke or MI, identified through ICD-9-CM diagnosis codes. The sensitivity and specificity of diagnosis codes for acute ischemic stroke are 86% and 95%, respectively,11,16 while codes for MI have a sensitivity and specificity > 85% with a positive predictive value of over 93%.18 The main outcome was mortality. Since our study focused on ICH survivors, entry time in the study started with hospital discharge, and therefore, in-hospital mortality was not considered. Additionally, we conservatively excluded ischemic events in the first 30 days after discharge from ICH hospitalization. This was done to ensure that ischemic events directly related to the index hospitalization were not carried forward in our analysis.
Statistical Analysis
We used Kaplan-Meier survival analysis to calculate the incidence rate of death among patients with and without an arterial ischemic event. To analyze the effect of an arterial ischemic event on time to death among ICH patients, we used a marginal structural model to account for possible confounding by baseline and time-dependent risk factors and the ischemic event. Age, hypertension, diabetes mellitus, atrial fibrillation, chronic kidney disease, and valvular heart disease were used as time varying covariates and serially updated, while sex and race were treated as fixed covariates. Confidence intervals (CI) were computed using the nonparametric bootstrap method. In secondary analyses, we evaluated the relationship between ischemic stroke and mortality, and MI and mortality, using marginal structural models similar to those in the primary analysis. Statistical analyses were performed using Stata (version 15.0, StataCorp) and R (version, 3.6.3). All tests were 2-tailed, with the threshold for statistical significance set at p < 0.05.
Results
Study Population
Among 1.7 million Medicare beneficiaries analyzed in this study, 27,616 were diagnosed with ICH (Figure 1). Of these patients, 18,812 had a stroke or MI prior to ICH or in the first 30 days after ICH, and were excluded. Among 8,804 Medicare beneficiaries with an ICH, 2,371 (27.2%) had an arterial ischemic event. Patients with an arterial ischemic event were older and they more often had hypertension, coronary artery disease, atrial fibrillation and valvular heart disease (Table 1).
Figure 1.
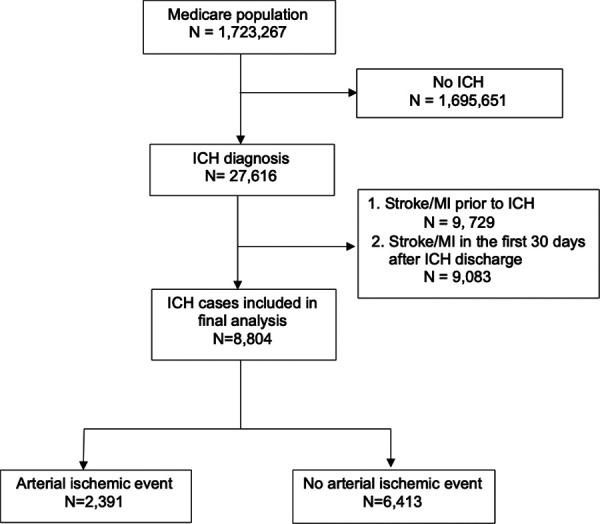
Flowchart showing patient inclusion criteria.
Table 1.
Characteristics of Patients Stratified by Presence of a Stroke or Myocardial Infarction After Intracerebral Hemorrhage.
| Characteristicsa | Stroke/MI (N = 2,371) | No Stroke/MI (N = 6,433) |
|---|---|---|
| Age, mean (SD), y | 78.7 (7.7) | 78.7 (8.3) |
| Female | 1,338 (56) | 3,550 (55) |
| Race | ||
| White | 2,012 (85) | 5,585 (87) |
| Black | 201 (8) | 416 (6) |
| Other | 158 (7) | 432 (7) |
| Hypertension | 2,239 (94) | 5,956 (93) |
| Diabetes | 1,331 (56) | 3,539 (55) |
| Congestive heart failure | 85 (4) | 231 (4) |
| Peripheral vascular disease | 54 (2) | 145 (2) |
| Chronic obstructive pulmonary disease | 73 (3) | 203 (3) |
| Chronic kidney disease | 621 (26) | 1,668 (26) |
| Atrial fibrillation | 861 (36) | 2,144 (33) |
| Valvular disease | 1,027 (43) | 2,802 (44) |
| Tobacco use | 425 (18) | 1,521 (24) |
| Alcohol use | 337 (14) | 1,051 (16) |
Abbreviations: MI, myocardial infarction; SD, standard deviation.
a Data are presented as number (%) unless otherwise specified.
Primary Outcome
During a median follow up time of 1.9 years (interquartile range, 0.7-3.9), the mortality rate was 21.7 (95% confidence interval [CI], 20.4-23.0) per 100 person-years in patients with an arterial ischemic event and 15.0 (95% CI, 14.4-15.6) per 100 person-years in patients without an arterial ischemic event. In the unadjusted marginal structural model, the occurrence of an arterial ischemic event was associated with an increased risk of death (hazard ratio [HR], 2.0; 95% confidence interval [CI], 1.8-2.1) (Figure 2). This risk was increased after incrementally adjusting for age, sex, and race in model 2 (HR, 1.9; 95% CI, 1.7-2.1), and after controlling for demographics and comorbidities (hypertension, diabetes mellitus, valvular heart disease, atrial fibrillation, congestive heart failure) in model 3 (HR, 1.8; 95% 1.6-1.9) (Table 2). There was no effect medication by age (p value for interaction = 0.40) or sex (p value for interaction 0.52).
Figure 2.
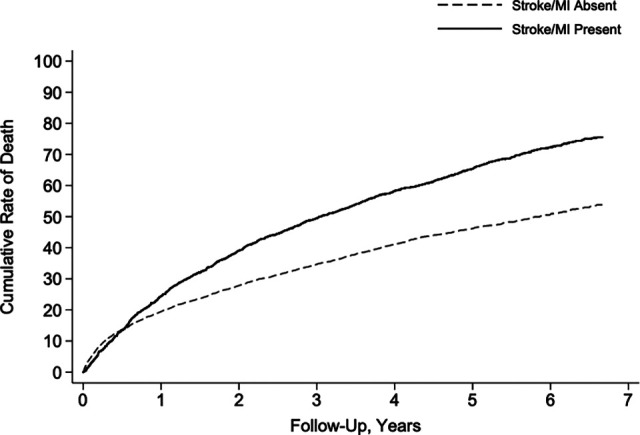
Risk of death after arterial ischemic event among patients with intracerebral hemorrhage.
Table 2.
Hazard Ratios Showing the Relationship Between an Arterial Ischemic Event and Mortality After Intracerebral Hemorrhage.
| Characteristica | HR (95% CI) | P value |
|---|---|---|
| Model 1: | 2.0 (1.8-2.1) | <0.001 |
| Unadjusted | ||
| Model 2: | 1.9 (1.7-2.1) | <0.001 |
| Age, sex, race | ||
| Model 3: | 1.8 (1.6-1.9) | <0.001 |
| Model 1 + hypertension, diabetes mellitus, valvular heart disease, atrial fibrillation, congestive heart failure | ||
| Model 4: | 1.3 (1.2-2.3) | <0.001 |
| Model 3 +including events in the first 30 days | ||
| Model 5: | 1.6 (1.5-1.7) | <0.001 |
| Model 3 + including patients with prior stroke and MI |
Abbreviations: CI, confidence interval; HR, hazard ratio; MI, myocardial infarction.
Secondary Analysis
In secondary analyses, we evaluated the risk of mortality after ischemic stroke and MI separately. After adjustment of confounders, the mortality risk was similarly elevated after an ischemic stroke (HR, 1.7; 95% CI, 1.5-1.8), and a MI (HR, 3.0; 95% CI, 2.4-3.8).
Post Hoc Analyses
We performed several post hoc analyses. An arterial ischemic event was associated with an increased risk of death after ICH when counting events in the first 30 days (HR, 1.3; 95% 1.2-2.3), and when including patients with a prior stroke and MI (HR, 1.6; 95% CI, 1.5-1.7). We also performed subgroup analyses stratified by age (mean as cut-off) and sex. An incident stroke or MI after ICH was associated with a higher risk of death when stratified by the mean age of the cohort (76 years) and by sex (Supplemental Table 1).
Discussion
In a large cohort of Medicare beneficiaries who survived an ICH, we observed a heightened risk of death after an arterial ischemic event compared to patients without, particularly within the first 3 years after ICH. The increased mortality risk was observed after an ischemic stroke and acute MI.
Prior studies have mostly evaluated trends and incidence of all-cause mortality after ICH. A recent population-based study in a Chinese community reported a 1- and 5-year cumulative incidence of vascular mortality of 9% and 23%, respectively after ICH. 3 A U.S population study found similar trends of ICH mortality across various study periods. 17 However, the risk of death after an acute vascular event was not estimated in these studies. Furthermore, an analysis of the Framingham heart study showed an age-specific increasing trend in the incidence of ICH, particularly after 75 years of age. 18 In the context of the aging population in the U.S. and the increased risk of an arterial ischemic event after ICH, our study provides important prognostic findings that indicate more than a 1.5-fold higher risk of mortality after a stroke or MI among ICH survivors.
Current guidelines equivocate about the use of antithrombotic medications after ICH due to concerns about ICH recurrence, and therefore, the ideal secondary cardiovascular prevention strategy in these patients is not established. In the REstart or STop Antithrombotics Randomised Trial (RESTART), restarting antiplatelet therapy after ICH, showed a significant reduction in major vascular occlusive events, and a trend toward decreased ICH recurrence, compared to discontinuing antiplatelet therapy. 19 A multi-center retrospective cohort study showed a significant reduction in mortality after initiation of oral anticoagulant therapy among ICH survivors with atrial fibrillation, compared to those not started on antithrombotic therapy. 20 In fact, the ongoing Anticoagulation in ICH Survivors for Stroke Prevention and Recovery (ASPIRE) trial that seeks to randomize patients with atrial fibrillation and a recent ICH to receive either apixaban or aspirin, also includes mortality in the composite primary outcome. 21 Collectively, given emerging data on the arterial ischemic risk after ICH,4,5 and our findings of an elevated mortality risk, careful exploration of possible antithrombotic strategies is warranted to prevent cardiovascular disease and vascular death in these vulnerable patients.
Our study has several important limitations. First, the Medicare data lacked information on ICH etiology and severity factors such as hematoma volume or location, presence of intraventricular hemorrhage, and Glasgow Coma Scale score. We lacked information on antithrombotic medication use and interruption. Second, our study is subject to selection bias due to inclusion of patients older than 66 years, which limits the generalizability of our results; however, this age group accurately reflects the median age of ICH patients in the general population. 22 Third, errors in misclassification resulting from our use of ICD-9-CM codes are also possible. For instance, the ICH primary diagnosis code may have been replaced with a more generic stroke diagnosis code for subsequent readmissions after ICH for non-cardiovascular complications, which may have resulted in the overestimation of the ischemic stroke risk in our study. The ICD-9-CM codes for ICH, stroke and MI however, have been previously validated to have high specificity and positive predictive value.10,23 Moreover, ICD-9-CM codes for major diagnoses in these types of administrative datasets have generally been shown to be reliable, 24 and any miscoding is likely to bias the results toward the null, which would support the results of our analyses. Lastly, our study did not have information on stroke severity, stroke subtype, or specific interventions performed for acute stroke.
Conclusions
There appears to be a heightened risk of death among ICH survivors, after an arterial ischemic event compared to those without, in the first 2 years after ICH. Better cardiovascular and cerebrovascular prevention strategies may aid in improving long-term recovery after ICH.
Supplemental Material
Supplemental Material, sj-docx-1-nho-10.1177_19418744211026709 for Risk of Mortality After an Arterial Ischemic Event Among Intracerebral Hemorrhage Survivors by Melvin Parasram, Neal S. Parikh, Alexander E. Merkler, Guido J. Falcone, Kevin N. Sheth, Babak B. Navi, Hooman Kamel, Cenai Zhang and Santosh B. Murthy in The Neurohospitalist
Declaration of Conflicting Interests: The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article. AM is supported by the NIH (grant KL2TR002385), the American Heart Association (18CDA34110419) and the Leon Levy Foundation. GJF is supported by the NIH (K76AG059992, R03NS112859), the American Heart Association (18IDDG34280056), the Yale Pepper Scholar Award (P30AG021342) and the Neurocritical Care Society Research Fellowship. KNS is supported by the NIH (U24NS107215, U24NS107136, RO1NR018335, and U01NS106513), Novartis, and Bard, and reports grants from Hyperfine, Biogen, and Astrocyte unrelated to this work. AB is supported by the NIH (K23NS100816). H.K serves as the co-PI for the NIH-funded ARCADIA trial which receives in-kind study drug from the BMS-Pfizer Alliance and in-kind study assays from Roche Diagnostics, serves as a steering committee member of Medtronic’s Stroke AF trial (uncompensated), serves on an endpoint adjudication committee for a trial of empagliflozin for Boehringer-Ingelheim, and has served on an advisory board for Roivant Sciences related to Factor XI inhibition. S.B.M is supported by the NIH (K23NS105948). All other authors report no conflict of interest for this study.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study is supported by the National Institutes of Health (NIH) (K23NS105948) to SBM. The funding entities had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the article; and decision to submit the article for publication.
Supplemental Material: Supplemental material for this article is available online.
ORCID iDs
Melvin S. Parasram, DO  https://orcid.org/0000-0002-2981-2307
https://orcid.org/0000-0002-2981-2307
Neal S. Parikh, MD  https://orcid.org/0000-0002-8802-2380
https://orcid.org/0000-0002-8802-2380
Hooman Kamel, MD  https://orcid.org/0000-0002-5745-0307
https://orcid.org/0000-0002-5745-0307
Santosh B. Murthy, MD, MPH  https://orcid.org/0000-0002-4950-0992
https://orcid.org/0000-0002-4950-0992
References
- 1.van Asch CJ, Luitse MJ, Rinkel GJ, van der Tweel I, Algra A, Klijn CJ. Incidence, case fatality, and functional outcome of intracerebral haemorrhage over time, according to age, sex, and ethnic origin: a systematic review and meta-analysis. Lancet Neurol. 2010;9(2):167–176. doi:10.1016/S1474-4422(09)70340-0 [DOI] [PubMed] [Google Scholar]
- 2.Hemphill JC, III, Farrant M, Neill TA, Jr. Prospective validation of the ICH score for 12-month functional outcome. Neurology. 2009;73(14):1088–1094. doi:10.1212/WNL.0b013e3181b8b332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen Y, Wright N, Guo Y, et al. Mortality and recurrent vascular events after first incident stroke: a 9-year community-based study of 0.5 million Chinese adults. Lancet Glob Health. 2020;8(4):e580–e590. doi:10.1016/S2214-109X(20)30069-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Casolla B, Moulin S, Kyheng M, et al. Five-year risk of major ischemic and hemorrhagic events after intracerebral hemorrhage. Stroke. 2019;50(5):1100–1107. doi:10.1161/STROKEAHA.118.024449 [DOI] [PubMed] [Google Scholar]
- 5.Murthy SB, Diaz I, Wu X, et al. Risk of arterial ischemic events after intracerebral hemorrhage. Stroke. 2020;51(1):137–142. doi:10.1161/STROKEAHA.119.026207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liotta EM, Singh M, Kosteva AR, et al. Predictors of 30-day readmission after intracerebral hemorrhage: a single-center approach for identifying potentially modifiable associations with readmission. Crit Care Med. 2013;41(12):2762–2769. doi:10.1097/CCM.0b013e318298a10 f [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wen T, Liu B, Wan X, et al. Risk factors associated with 31-day unplanned readmission in 50,912 discharged patients after stroke in China. BMC Neurol. 2018;18(1):218. doi:10.1186/s12883-018-1209-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kuohn LR, Leasure AC, Acosta JN, et al. Cause of death in spontaneous intracerebral hemorrhage survivors: multi-state longitudinal study. Neurology. 2020;95(20):e2736–e2745. doi:10.1212/WNL.0000000000010736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Medicare and Medicaid Services . Medicare limited dataset files. Accessed August 11, 2020. https://www.cms.gov/Research-Statistics-Data-and-Systems/Files-for-Order/LimitedDataSets/
- 10.Kokotailo RA, Hill MD. Coding of stroke and stroke risk factors using international classification of diseases, revisions 9 and 10. Stroke. 2005;36(8):1776–1781. doi:10.1161/01.STR.0000174293.17959.a1 [DOI] [PubMed] [Google Scholar]
- 11.Tirschwell DL, Longstreth WT, Jr. Validating administrative data in stroke research. Stroke. 2002;33(10):2465–2470. [DOI] [PubMed] [Google Scholar]
- 12.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. [DOI] [PubMed] [Google Scholar]
- 13.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–619. [DOI] [PubMed] [Google Scholar]
- 14.Bar B, Hemphill JC, III. Charlson comorbidity index adjustment in intracerebral hemorrhage. Stroke. 2011;42(10):2944–2946. doi:10.1161/STROKEAHA.111.617639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jiménez Caballero PE, López Espuela F, Portilla Cuenca JC, Ramírez Moreno JM, Pedrera Zamorano JD, Casado Naranjo I. Charlson comorbidity index in ischemic stroke and intracerebral hemorrhage as predictor of mortality and functional outcome after 6 months. J Stroke Cerebrovasc Dis. 2013;22(7):e214–e218. doi:10.1016/j.jstrokecerebrovasdis.2012.11.014 [DOI] [PubMed] [Google Scholar]
- 16.McCormick N, Bhole V, Lacaille D, Avina-Zubieta JA. Validity of diagnostic codes for acute stroke in administrative databases: a systematic review. PLoS One. 2015;10(8). doi:10.1371/journal.pone.0135834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Flaherty ML, Haverbusch M, Sekar P, et al. Long-term mortality after intracerebral hemorrhage. Neurology. 2006;66(8):1182–1186. doi:10.1212/01.wnl.0000208400.08722.7c [DOI] [PubMed] [Google Scholar]
- 18.Lioutas VA, Beiser AS, Aparicio HJ, et al. Assessment of incidence and risk factors of intracerebral hemorrhage among participants in the Framingham Heart Study between 1948 and 2016. JAMA Neurol. 2020;77(10):1252–1260. doi:10.1001/jamaneurol.2020.1512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Al-Shahi Salman R, Minks DP, Mitra D, et al. Effects of antiplatelet therapy on stroke risk by brain imaging features of intracerebral haemorrhage and cerebral small vessel diseases: subgroup analyses of the RESTART randomised, open-label trial. Lancet Neurol. 2019;18(7):643–652. doi:10.1016/S1474-4422(19)30184-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Biffi A, Kuramatsu JB, Leasure A, et al. Oral anticoagulation and functional outcome after intracerebral hemorrhage. Ann Neurol. 2017;82(5):755–765. doi:10.1002/ana.25079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Anticoagulation in ICH Survivors for Stroke Prevention and Recovery (ASPIRE) trial. Accessed June 25, 2020. https://clinicaltrials.gov/ct2/show/NCT03907046
- 22.Feigin VL, Lawes CM, Bennett DA, Anderson CS. Stroke epidemiology: a review of population-based studies of incidence, prevalence, and case-fatality in the late 20th century. Lancet Neurol. 2003;2(1):43–53. [DOI] [PubMed] [Google Scholar]
- 23.Williams GR, Jiang JG, Matchar DB, Samsa GP. Incidence and occurrence of total (first-ever and recurrent) stroke. Stroke. 1999;30(12):2523–2528. a journal of cerebral circulation. [DOI] [PubMed] [Google Scholar]
- 24.Quan H, Li B, Saunders LD, et al. Assessing validity of ICD-9-CM and ICD-10 administrative data in recording clinical conditions in a unique dually coded database. Health Serv Res. 2008;43(4):1424–1441. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-docx-1-nho-10.1177_19418744211026709 for Risk of Mortality After an Arterial Ischemic Event Among Intracerebral Hemorrhage Survivors by Melvin Parasram, Neal S. Parikh, Alexander E. Merkler, Guido J. Falcone, Kevin N. Sheth, Babak B. Navi, Hooman Kamel, Cenai Zhang and Santosh B. Murthy in The Neurohospitalist


