Abstract
Background
Although pet removal has been recommended in guidelines on the management of allergic asthma, pet ownership remains high in families where one or more members have an allergy to pet dander. Allergen control measures such as air filtration units placed in the homes of pet‐allergic asthmatics have been used as a means of reducing allergen exposure.
Objectives
To determine the clinical efficacy of pet allergen control measures in the homes of people with pet‐allergic asthma.
Search methods
We carried out an electronic search of the Cochrane Airways Group Specialised Register of Trials. No restriction was placed on language of publication. Searches are current as of September 2008.
Selection criteria
Randomised controlled trials comparing an active allergen reduction measure with control were considered for analysis. Participants had stable pet‐allergic asthma.
Data collection and analysis
Two reviewers extracted data independently. Only a limited amount of data could be analysed and no meta‐analysis was possible.
Main results
Two studies met the inclusion criteria for the analysis. Both examined the effectiveness of air filtration units. Both trials were small (n = 22 and n = 35). No significant differences were detected between active intervention and control on the primary and secondary outcome measures reported in the studies. Data on absence from school or work were not reported in either study. No meta‐analysis could be performed due to lack of common outcomes. An update search conducted in September 2006 did not identify any further trials.
Authors' conclusions
The available trials are too small to provide evidence for or against the use of air filtration units to reduce allergen levels in the management of pet‐allergic asthma. Adequately powered trials are needed. There are no trials of other allergen reduction measures, such as pet washing or possibly pet removal.
Plain language summary
Pet allergen control measures for allergic asthma in children and adults
Some people with asthma who own pets can be allergic to the dander that accumulates in and around the home. Certain guidelines recommend the removal of pets as the most effective way of reducing exposure to the allergens emanating from their hair and skin. Other measures have been proposed as an alternative to pet removal, such as pet washing, sprays and air filtration units. The aim of these interventions is to lower the amount of allergen in the air and on the floor of the home, and so limit the risk of asthma symptoms worsening. Very little research of a high quality has been published on this topic, and the current evidence is not sufficiently reliable to draw firm conclusions. Further research should consider the effectiveness of pet washing, sprays and possibly pet removal from the home.
Background
Asthma can be defined by its major clinical symptoms, variable airflow obstruction and reversibility (BTS 1997). The etiology of the disease is complex and is attributable to both genetic and environmental influences. It is widely recognised that in Western countries atopy is associated with asthma with just over 50% of asthmatic adults and children having at least one positive skin prick test to a common allergen (Balfour Lynn 1999). There is evidence that atopy is a predictor of asthma in children (ATS 1962), but its role has yet to be fully elucidated (Pearce 1999; von Mutius 2001).
In Western countries up to 40% of adults or children (two to four years) with atopy and asthma may be sensitised to cat (ATS 1962; Eriksson 1996). Inhalation challenge studies in the laboratory setting demonstrate that contact with cat allergen can induce respiratory symptoms in those with cat allergy and asthma (Wanger 1999).
It would appear that the allergenic components of cat dander are relatively stable in house dust and are difficult to remove with regular cleaning (ATS 1962). Cat allergen is also found in unexpected places such as dust in schools (ATS 1962). It would seem that cat allergen is ubiquitous in societies where cat ownership is common, and indeed the community prevalence of cat shows a correlation with the community prevalence of respiratory symptoms and sensitisation prevalence (Roost 1999). However, the contribution that the real life 'challenge' of pet ownership has on respiratory symptoms compared to what is present in the community, is unclear.
Some guidelines for asthma indicate that pets especially cats should be removed from the homes of those with specific allergies and asthma (BTS 1997), but others do not (SIGN 1998; Prodigy). Anecdotally compliance with pet removal is reported to be poor. "Rather than dictatorial, it is best for the families to come to decisions about removing pets themselves. This may be helped by providing objective evidence." (Balfour Lynn 1999).
In those families that choose to keep the pet some techniques aimed at reducing indoor allergen load are available. Methods focused on the source include washing or wiping the pet with and without chemical agents and those focused on airborne and dust allergen reservoirs include air filtration and chemical cleaning agents (Avner 1997; Custovic 1998; Wood 1998; Hodson 1999).
This review attempts to summarise the evidence for the effectiveness of any measures to reduce pet allergen exposure on reducing the symptoms of asthma associated with pet allergy.
Objectives
To assess whether measures to reduce pet allergen are effective in the treatment of people with pet‐allergic asthma.
Methods
Criteria for considering studies for this review
Types of studies
All randomised trials or quasi‐ randomised trials comparing measures to reduce pet allergen in the home with placebo whenever practical. Controls with no placebo were acceptable only if it was not possible to use a placebo, such as removal of the family pet from the home.
Types of participants
The participants were diagnosed as having bronchial asthma by an appropriately qualified physician. Allergy to pet was demonstrated by positive skin prick test greater or equal to histamine control, or positive pet specific RAST or ELISA, or positive bronchial challenge to pet allergen. The relevant pet was in the home at the start of study. Participants included children or adults of any age and either gender.
Types of interventions
The types of allergen reduction measures considered were:
Removal of pet from the home with or without cleaning of the house compared to keeping the pet
Keeping the pet & High Efficiency Particulate Air (HEPA) filter compared to keeping the pet and placebo filtration unit
Keeping the pet & any air filter compared to keeping the pet & placebo filtration unit
Keeping the pet & chemical cleaning agents (of home or pet) compared to keeping the pet & placebo chemical cleaning agents
Types of outcome measures
Primary outcomes
Lung function
Secondary outcomes
Night time &/or day time coughing
Changes in asthma medication use (both reliever and preventer therapy)
School/work absenteeism
Quality of life score
Symptom scores.
Biochemical markers of inflammation such as change in eosinophilic peroxidase (EPO) and eosinophil protein X (EPX) (Bjornsson 1996; Lonnkvist 1999) and of allergen contact such as reduction in serum IgG or IgE specific for cat proteins were also recorded. Changes in allergen levels within the home such as airborne or dust concentration of Fel d 1 (cat dander) or other cat allergen and dust concentration of Fel d 1 or other cat allergen were also recorded.
We considered studies provided they reported the primary outcome.
Search methods for identification of studies
Electronic searches
Trials were identified using the Cochrane Airways Group Specialised Register of trials, which is derived from systematic searches of bibliographic databases including the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, EMBASE and CINAHL, and handsearching of respiratory journals and meeting abstracts. All records in the Specialised Register coded as 'asthma' were searched using the following terms:
(cat* or "fel d 1" or feline* or dog* or canine* or pet* or animal*) and (((air*) and filt* or cleaner*) or hepa* or wash* or chemical* or (allergen* and (avoid* or reduc*)))
We did not impose any restrictions on the language of publication. The searches were up to date as of September 2008.
Searching other resources
We checked the bibliography of each paper and other published reviews for further references. We also contacted the primary authors of each study, together with experts in the field, and the manufacturers of allergen reduction materials/appliances in order to identify additional trials, whether published or unpublished.
Data collection and analysis
Selection of studies
Two independent reviewers (SK and TL) assessed all reports of studies identified as potentially eligible. SK and TL extracted data following the Airways Group procedure.
Data extraction and management
Data were entered into RevMan software package for analysis.
Assessment of risk of bias in included studies
We assessed the risk of bias for each study in terms of allocation, blinding and other sources of bias relating to treatment or population recruited. The domains we used as the basis for this assessment (allocation generation, allocation concealment, blinding and other sources of bias) were judged to be at low, high or unclear risk of bias.
Data synthesis
Data will be combined with WMD (weighted mean difference) for continuous outcomes measured on the same metric, or SMD for continuous outcomes measured on different metrics. Fixed Effect modelling will be used to combine data unless heterogeneity is identified (P =/< .01) in which case a Random Effects model will be used to determine the extent to which variation in the data affect the pooled treatment effect estimate.
For dichotomous variables, event rate data will be pooled using a Peto Odds Ratio (POR).
In the event of further randomised trials being identified, there will be a sensitivity analysis of high‐ and low‐quality trials, and subgroups planned in the following way:
Adults or children with asthma with a clinical history and positive skin prick test (SPT) or elevated serum specific IgE to cat allergen.
Children will be analysed as a sub group as this population is most at risk of allergen induced symptoms.
Patients who are mono‐allergic or have a seasonal allergy and are studied out of that season will be analysed as a sub group.
Results
Description of studies
Results of the search
From searches run from all years to September 2008 we have identified a total of 227 references. A total of 16 of these have been retrieved as full‐text articles. Thirteen studies were excluded, one is ongoing (Rolfsjord 2005), and two met the eligibility criteria of the review.
An archive of previous search results is given in Appendix 1.
Included studies
Two studies met the eligibility criteria of the review.
Study design
Both van der Heide 1999 and Wood 1998 were randomised, double blind placebo controlled studies. Wood 1998 was a parallel designed study and van der Heide 1999 was designed as a cross‐over study. However, in the van der Heide 1999 study parallel group data from the first arm of the study were presented due to uneven distribution. The study duration in the Wood 1998 study was four months in total. Following a one‐month run in, patients were treated with active or placebo filters for three months with no follow‐up. van der Heide 1999 had a one week run in and a treatment period of six months with cross‐over at three months. No follow‐up or washout was apparent. The duration of the Wood 1998 study was four months in total. Following a one‐ month run in, patients were treated with active or placebo filters for three months with no follow‐up. van der Heide 1999 had a one week run in and a treatment period of six months with cross‐over at three months. No follow‐up or washout periods were reported.
Populations
Wood 1998 recruited 38 adult patients with allergic asthma and/or rhinitis associated with cats. Thirty five patients were randomised to the two treatment groups, three having been excluded during the one month run‐in. Asthma was defined as respiratory symptoms (either asthma or rhinitis) requiring regular medication use on more than 50% days. Severe asthmatics were excluded but no definition of severe was cited as these data were obtained by questionnaire. Sensitisation to pet allergen was established by cat specific skin prick test and a history of developing symptoms on exposure to cat. A skin prick test was undertaken which consisted of several allergens (dust mite, cat, dog, cockroach, molds, grass, tree and ragweed pollen), and this was used to determine other coexistent allergies. Participants were enrolled outside of the pollen season for which they had had an allergic reaction, or were not enrolled if part of the study period included part of the pollen season. Participants who planned to be away from their domicile for more than one week during the study period were excluded. A subgroup of asthmatics were defined as methacholine reactive (N = 23). Participants were recruited from the community via a newspaper advertisement.
van der Heide 1999 recruited 22 children with mild asthma (mean FEV1 90.2 +/‐11.2 % predicted) who were allergic to cat or dog. There were two drop outs, both due to changes in inhaled steroid medication. Asthma was defined as 'moderate' although participants had minimal symptoms on inhaled steroids and all participants were responsive to adenosine monophosphate. Particpants were enrolled provided they were sensitised to cat or dog allergen (RAST class > or = two units). The study period was out of the pollen season (September to April), and this study also included participants with perennial allergies. Participants were excluded from the study if they changed their medication. No patients had viral upper respiratory tract infections during the study period, but it is unclear if this was an inclusion criterion. Participants were recruited from an outpatient paediatric chest clinic.
Neither study gave data for the total eligible population or the number that declined to consent.
Interventions
Wood 1998 used a Honeywell envirocare HEPA filter used in the bedroom alone, with the capacity for 15 changes of air per hour in an average bedroom (350 cubic feet per minute). In both treatment groups, participants' pillow and mattress were encased with impervious covers, and they were instructed to wash bedding once a week and keep the cats from entering the bedroom at all times by keeping the door shut. Compliance was closely monitored, with a timing device inserted into the HEPA filter and a regular visit by a study investigator to ensure that the device was used. Participants were excluded from the trial if they failed to comply with any of the environmental allergen control measures. The control intervention consisted of an identical HEPA unit with the filter removed. This sounded and looked identical to the active HEPA unit.
van der Heide 1999 used a Phillips air cleaner in the living room and the bedroom and no additional control measures were used. Active and placebo units were identical, other than the absence of the active filter in the placebo unit.
Outcomes
Wood 1998 reported lung function (peak flow and monthly spirometry), bronchial hyperresponsiveness, medication change (rescue and maintenance), symptom scores, sleep disturbance, airborne and settled dust Fel d 1 concentration.
van der Heide 1999 reported lung function (peak flow, peak flow variability, FEV1), bronchial hyperresponsiveness, symptom scores, and settled dust Fel d 1 and Can f 1 (dog dander) and EDN (eosinophil‐derived neurotoxin).
Excluded studies
We have retrieved the following studies from searches conducted to September 2008 that have not met the inclusion criteria of the review: Francis 2003 (randomised study comparing HEPA filter with vacuum cleaner); De Blay 2003 (randomised study comparing mite allergen exposure reduction advice ‐ multiple intervention study); Carter 2001(pet ownership not stipulated and interventions not covered by this review); Bjornsdottir 2003 (participants had allergic rhinitis); Gore 2003 (before and after study of air filtration units in the home); Karlsson 2004 (school‐based study).
Risk of bias in included studies
The overall quality of reporting in the studies was high. Our judgements for each of the four domains are detailed in Figure 1. We were able to establish that allocation procedures were adequate for both studies. We did not have sufficient information to determine how adequately concealed allocation was performed in the studies.
1.
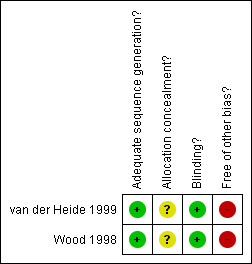
Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
Placebo filter units were used in both studies, stated to be indistinguishable from active in van der Heide 1999. It was not stated that the units were prepared by an independent party or how they were dispensed to participants.
Both studies were at risk of bias in terms of either the intervention offered to study participants (Wood 1998), or the characteristic of the population studied (van der Heide 1999). Wood 1998 offered participants additional mattress covers to intervention and control groups, potentially confounding treatment effect. van der Heide 1999 recruited participants with particularly mild asthma, therefore limiting the potential for improving symptoms and lung function.
Effects of interventions
The published data did not enable us to conduct a meta‐analysis. This was due in part to one study population including rhinitics and asthmatics (Wood 1998), and limited data being provided as means and standard deviations in the van der Heide 1999 study. Following correspondence with Dr Robert Wood, unpublished means have been reported in this review. No distributional data were made available to us. There were 14 asthma sufferers in the placebo group, and nine asthma sufferers in the active treatment group. Unless otherwise stated, the values reported here for Wood 1998 refer to unpublished data.
Lung function
Wood 1998 reported peak flow as litres/min and adjusted for baseline, comparing the treatment group means. Measurements were taken for both morning and evening flow rates. No statistically significant change between control and active therapy was detected (p = 0.173 for am PEFR and p = 0.409 for pm PEFR).
van der Heide 1999 reported no change in peak flow values. No data were supplied as means, and no p values were reported for change scores.
van der Heide 1999 reported no effect on FEV1. Peak flow amplitude was presented in graphical format, and values were imputed by SK and TL independently. Means and standard deviations were then entered into MetaView, but the confidence intervals generated by these data should be regarded with caution. van der Heide 1999 reported a significant change from baseline in the group treated with the active filter (p = 0.045). However, this was not compared with the change in the control group.
Bronchial Hyperresponsiveness (BHR)
Wood 1998 found no significant difference between the active and control arms of the study after adjusting for baseline.
van der Heide 1999 reported that BHR was significantly decreased after intervention but not after control. Direct comparison between active and control groups was not calculated. Change from baseline may have been a fairer comparison for such a small heterogeneous population, but such data were not reported. Data were log transformed due to uneven distribution.
Symptom Scores
Wood 1998 reported no significant changes in symptom scores in either the placebo or active groups. Mean values were provided by Dr Wood for chest and nasal symptom scores in the asthmatic participants. The p values provided with these data did not reach significance.
Sleeping difficulty data were also provided for asthmatic participants. Twelve and four asthma sufferers in the placebo and active group respectively, reported difficulty with sleeping during the study.
van der Heide 1999 did not present numerical values for changes in symptom scores in either treatment group. In the narrative of the published study, no effects on wheezing or shortness of breath were reported for active and placebo therapies. A baseline median symptom score revealed that most participants had few or no symptoms at all at the beginning of the trial.
Medication usage
Wood 1998 did not detect any significant difference in either maintenance or as‐needed medication usage in the active or placebo groups. Maintenance and as‐needed therapies generated non‐significant p values (p = 0.228 and p = 0.552 respectively).
van der Heide 1999 withdrew the data contributed by participants who embarked new therapies or who came off existing therapies during the study. No medication usage scores were reported in the study.
Allergen Concentrations
Concentration of settled allergens captured by the units were reported in the original studies.
No change was reported in allergen concentration for settled dust at any stage during the Wood 1998 study (p = 0.407).
van der Heide 1999 reported allergen in settled dust for both active and sham filters. No change in allergen concentration was reported. No numerical data were presented.
Wood 1998 compared airborne allergen levels between the two types of filter. Original published data for this outcome showed a statistically significant difference in the levels of airborne Fel d 1 allergen in the actively treated group after three months (1.7+/‐1.7ng per m3 in the active filter group and 2.8+/‐1.8ng per m3 in the sham filter group p = 0.045). However, these results exclude data contributed by non‐compliant participants, and when all homes were included in the analysis mean levels of allergen were not significantly different (2 ng per m3 and 2.7 ng per m3 for the active and sham filters respectively). These data include levels of allergen captured from non‐asthmatic participants, and as such cannot be correlated with any treatment effect detected in the participants with asthma.
Biochemical Markers
van der Heide 1999 reported that urinary EDN did not alter after intervention with either active or placebo filter for either group.
Discussion
This review has not found sufficient objective evidence to support or refute the use of measures for allergen control, which aim to benefit patients with pet allergic asthma. The studies had some methodological limitations but extensive efforts were made in both instances to blind the patients to whether the treatment they received was active or placebo.
The studies were small with no sample size calculations shown, and as such they may have been underpowered. The authors were unable to conduct a meta‐analysis with the two studies included, and so any overall treatment effect may not be detected until further studies are conducted with similar outcomes to those measured in these studies. In the Cochrane review on house dust mite reduction (Gotzsche 2008), one subgroup analysis detected a significant effect (asthma symptom scores ‐ parallel group trials) and whilst this significant effect may have occurred by chance, meta‐analysis can overcome inadequately powered trials by combining data from more than one trial (Jones 2003). This is possible with regard to the interventions analysed in this review, but impossible to prove without further adequately powered studies.
The presence of co‐interventions aimed at reducing contact with allergens in the Wood 1998 study may also have compromised the detection of a clear treatment effect in favour of the filter. Further research in the area of allergen avoidance measures should take into account the possibility that concomitant 'active' measures may confound the overall efficacy of the intervention in question. The design of the excluded van der Heide 1999 study did account for this to a certain degree, with three groups allocated to: active filter, impermeable mattress covers plus placebo filter; and active filters plus impermeable mattress covers. In that study participants with an allergic reaction to house dust mite allergen were included, among whom there were several pet allergic participants. Pet ownership was not a specified entry criteria, and it is difficult to conclude whether air filter and mattress covers used in that study would improve symptoms of pet allergic asthmatics where pets were present. Four cat‐owning pet‐allergic participants whose PC 20 improved following the introduction of the filter and mattress covers were also highly sensitised to house dust mite and grass pollen. Reducing exposure to any of these allergens may therefore induce a positive response.
The populations chosen for van der Heide 1999 were mild and stable on current medication, the baseline symptom scores were minimal and the FEV% predicted averaged at 90.2% at baseline. The implications for a clear demonstration of treatment efficacy may be more difficult in this population of asthmatics, given their relatively healthy status at the start of the trial. In Wood 1998 the population was considered to be symptomatic, and subgroup analysis was performed groups on for high and low maintenance therapy groups. In Wood 1998 changes in medication use were based on outcome measure but there is no indication that patient medication was regularly reviewed in a systematic manner. In the van der Heide 1999 study, patients whose medication altered over the course of the study were withdrawn from the final analysis, and so the effect on medication usage could not be measured in this review.
This review does not attempt to summarise the evidence on the effectiveness of control measures to reduce allergen concentrations in the air or dust of homes housing pets. Indeed as little is known about what allergen concentration would be 'safe' for a typical asthmatic that aim would be futile. The included studies did compare settled dust concentration of Fel d 1, but found no significant difference between homes with placebo or active filters. Even airborne allergen concentrations were not significantly different in placebo or active filter groups.
Non‐compliance with treatment protocol was taken into account by Wood 1998 and a subgroup analysis for compliant participants was subsequently conducted. Even in this group the reduction in mean allergen concentration only just reaches significance. Compliance was assessed by a home visit to determine if cats were excluded from the bedrooms and mattress and pillow covers maintained. Timer devices were also installed in the filters to determine for how long they had been left to run. This population had been screened for poor compliance during the one month baseline period and had consented to participate in the study. Consequently, compliance would be expected to be higher than in the normal clinical setting. Further studies of adequate sample size may give a clearer answer to this question. In Gotzsche 2008, one study (Huss 1992) examined the additional benefit of a computer assisted education programme to instruct the participants in the study on allergen avoidance. However, this was not found to improve asthma symptoms at all timepoints. In this review the possible role of an education programme has not been evaluated, but could be considered by future studies.
Other interventions that were represented in the literature that we reviewed included pet washing. Pre‐ and post‐treatment comparisons of washing cats (Avner 1997) or dogs (Hodson 1999) by immersion in water or shampooing showed a reduction in the shedding of allergen in the short term, but this is not maintained and would need repeating twice weekly (Hodson 1999). Chemical wipes are perhaps even less effective (Perzanowski 1997), although presumably easier to use. The impact upon asthma needs to be measured in future studies.
Until a rigorous study of successful allergen concentration reduction has been conducted, the impact of such devices as a HEPA filtration unit on health status remain unclear. Pollution may also have an affect on asthma in patients who experience exacerbations or a worsening of symptoms when exposed to environmental triggers. Some research on the impact of traffic pollution on the respiratory system, has described a hypothesis that diesel particles may have an impact on allergic respiratory reactions (Sabbah 2000). This may in turn have a bearing on people with allergic asthma living in large urbanised areas. However, this hypothesis has not been proven in the published literature considered in this review.
There is little objective evidence of the benefit of pet removal on asthma symptoms. It is impossible to determine whether such a strategy may be more effective than using a HEPA filter, or other pet allergen avoidance measures such as washing or chemical sprays.
Authors' conclusions
Implications for practice.
On the strength of the current body of evidence, HEPA filtration units have not been shown to reduce asthma symptoms significantly in people with pet allergic asthma. This may be due to the small number and size of the studies to date. If a pet is kept in the same residence as a pet allergic asthmatic, there seems to be no evidence to support or refute the effectiveness of allergen avoidance measures in the management of symptoms.
Implications for research.
The impact of pet removal on patients with pet allergic asthma should be evaluated, using patient centered outcomes such as quality of life symptom scales, medication reduction in addition to lung function tests. Clinical trials with sample size calculations, rigorous methodology and appropriate patient populations are required to determine what role allergen reduction measures may play in the treatment of asthma.
Feedback
Incorrect Quotation
Summary
Note: This comment was based on the previous version of the review which has since been amended as a consequence.
The authors suggest that we should have found a treatment effect in our review of house dust mite control measures for asthma (1). We did not. We reported two significant subgroup results and noted that because of the large number of significance tests we performed, two significant results would be expected to occur by chance.
The authors furthermore refer to a study by Huss et al. (2) which was included in our review and claim that the intervention was found to improve asthma symptoms. This is not correct. As we have reported, there was no significant improvement in asthma symptoms. The study ran for 12 weeks but Huss et al inappropriately did multiple analyses and found a significant difference after 9‐10 weeks, but not after 12 weeks (or after 1 week, 3 weeks, 5 weeks or 7 weeks), and reported only the significant result in the abstract.
Peter C. Gotzsche
Helle Krogh Johansen
Michael Burr
1. Gotzsche PC, Johansen HK, Burr ML, Hammarquist C. House dust mite control measures for asthma (Cochrane Review). In: The Cochrane Library, Issue 1, 2003. Oxford: Update Software.
2. Huss K, Squire EN, Carpenter GB, Smith LJ, Huss RW, Salata K, Salerno M, Agostinelli D, Hershey J. Effective education of adults with asthma who are allergic to dust mites. J Allergy Clin Immunol 1992;89:836‐43.
I certify that I have no affiliations with or involvement in any organisation or entity with a direct financial interest in the subject matter of my criticisms
Reply
We thank Gotzsche et al for their useful comments about our review and for drawing attention to some important methodological issues we raise in the Discussion section. The Discussion section of our review refers to the fact that individually some studies are under‐powered to detect a significant treatment effect, and that in combination a significant effect can be detected, and not in fact as Gotzsche et al believe, that they should have found a significant treatment effect. Indeed, combining data from studies in a meta‐analysis is useful in deriving global assessments of treatment efficacy1. Our review may not have explained that the outcome measure to which we referred from the House‐dust mite review was 'asthma symptom scores' and that the subgroup analysis referred to was 'physical interventions' (parallel group trials). We have amended the Discussion to indicate this explicitly. We felt that it would be inappropriate to take the summary statistic for the pooled analysis for this outcome measure as it combined the results not only from different types of interventions (chemical and physical) but this was pooled data from parallel and crossover studies.
We accept the comment regarding the study by Huss et al and the Discussion section has been amended accordingly.
1. Jones PW. An introduction to systematic reviews in respiratory medicine. Respiratory Medicine vol 97 (2003) 97‐103
Contributors
Gotzsche PC, Johansen HK, Burr M.
What's new
| Date | Event | Description |
|---|---|---|
| 26 September 2008 | New search has been performed | Literature search re‐run; no new studies identified. |
History
Protocol first published: Issue 1, 2001 Review first published: Issue 1, 2003
| Date | Event | Description |
|---|---|---|
| 15 August 2008 | Amended | Converted to new review format. |
| 3 September 2007 | New search has been performed | Literature search re‐run; no new studies identified. |
| 1 September 2006 | New search has been performed | Literature searches re‐run; no new studies found |
| 24 October 2000 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
We are very grateful to the editorial base of the Cochrane Airways Group for obtaining papers. We thank Bettina Reuben, Karen Blackhall and Steve Milan for extensive clerical, technical and methodological support. We thank Makiko Meguro for looking at the Spanish paper. We would also like to extend our gratitude to Dr Robert Wood and Dr Sicco van der Heide for providing us with unpublished data on their trials.
Appendices
Appendix 1. Archive of search results
Electronic searches yielded a total of 34 references. Of these, two met the inclusion criteria for the review (Wood 1998; van der Heide 1999). One further randomised study did not meet the inclusion criteria, because pet ownership was not stipulated at study entry (van der Heide 1997 ‐ see Excluded Studies). Upon searching the bibliography of these studies, five further reports were identified and retrieved for possible inclusion in this review. None met the inclusion criteria (see Excluded Studies). The principal reason for exclusion was no randomisation (Villaveces 1977; Reisman 1990; Boquete 1997). Two other references identified were a review article (Sabbah 2000) and a randomised study which recruited participants sensitive to house dust mites (Antonicelli 1991).
Data and analyses
Comparison 1. HEPA air filter versus sham filter.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Bronchial hyperresponsiveness (PC20) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Morning peak flow | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Evening peak flow | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 Peak flow variability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5 Sleeping difficulty at 3 months | 1 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Totals not selected |
1.1. Analysis.
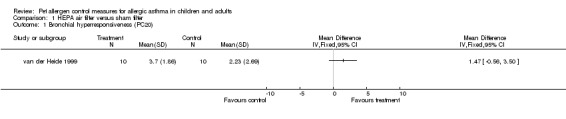
Comparison 1 HEPA air filter versus sham filter, Outcome 1 Bronchial hyperresponsiveness (PC20).
1.2. Analysis.
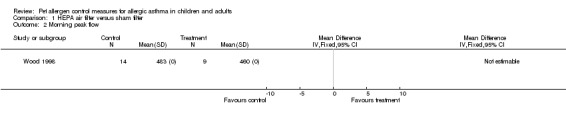
Comparison 1 HEPA air filter versus sham filter, Outcome 2 Morning peak flow.
1.3. Analysis.
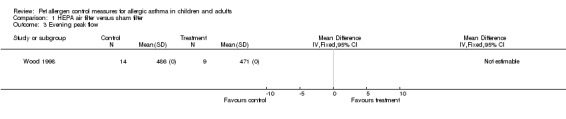
Comparison 1 HEPA air filter versus sham filter, Outcome 3 Evening peak flow.
1.4. Analysis.
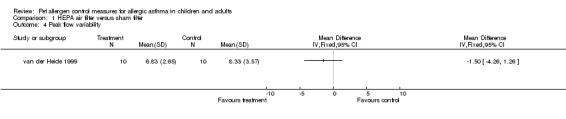
Comparison 1 HEPA air filter versus sham filter, Outcome 4 Peak flow variability.
1.5. Analysis.
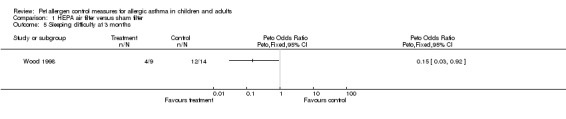
Comparison 1 HEPA air filter versus sham filter, Outcome 5 Sleeping difficulty at 3 months.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
van der Heide 1999.
| Methods | Randomised, cross‐over double blind placebo controlled trial. Participants recruited from pulmonology outpatient clinic in Groningen. | |
| Participants | Children (N = 22, M = 8) were recruited but two withdrew from the study. Moderate asthmatics with a cat or dog at home, all were responsive to adenosine monophosphate, no URTIs during the course of the study. | |
| Interventions | Active versus sham (placebo) air filtration units. Phillips air cleaner in the living room and bedroom, over a 6 month period (3 month treatment arm, no wash out period). | |
| Outcomes | Airways hyperresponsiveness to adenosine, FEV1 % predicted value, peak flow, medication and symptoms. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Minimisation method |
| Allocation concealment? | Unclear risk | Information not available |
| Blinding? All outcomes | Low risk | Sham filter unit used. |
| Free of other bias? | High risk | The participants were described as having minimal symptoms when using inhaled steroids, and a high an FEV1, implying that they were well controlled and suffering from only very mild asthma. It was felt that this may inhibit the demonstration of a clear treatment effect. The exclusion of participants who changed medication during the study also made it impossible to detect an effect on medication usage. |
Wood 1998.
| Methods | Randomised, double‐blind, placebo controlled trial. Participants were recruited following an advertising campaign. | |
| Participants | Adults, 7 rhinitic and 28 asthmatic rhinitics. Inclusion criteria: adult (16 to 60yrs); clinical history of symptoms of asthma or rhinitis on contact with cats; sharing a home with one or more cats; IgE sensitised to cat. 35 (age range 23 to 60, 10 M). | |
| Interventions | Active: Envirocare HEPA filter plus environmental control. Placebo: filter unit with no filter plus environmental control | |
| Outcomes | Symptoms (morning and night), peak flow (morning and night), sleep disturbance, medication usage and Fel d 1 in air and dust. | |
| Notes | Asthma: 5 by clinical history alone and 23 also methacholine reactive. Compliance: monitored by home visits and timers in units | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Computer‐generated randomised schedule. |
| Allocation concealment? | Unclear risk | Information not available |
| Blinding? All outcomes | Low risk | Placebo unit identical in appearance to active. |
| Free of other bias? | High risk | Participants were given additional measures to control allergen levels, namely pillow covers and mattresses. Because both groups received these interventions, any reduction in house dust mite levels could conceivably have confounded the effect of active air filtration units from reducing cat allergen levels. |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Antonicelli 1991 | Randomised study examining air filter in patients sensitive to house dust mite. |
| Bjornsdottir 2003 | Study conducted in participants with rhinitis |
| Boquete 1997 | Non‐randomised study. |
| Carter 2001 | Randomised study on allergen avoidance. Excluded as pet ownership not specified as criterion for study entry. No skin prick tests were undertaken until completion of the study. |
| De Blay 2003 | Randomised study assessing the effects of advice on mite allergen exposure reduction. This was excluded as it was a multiple treatment intervention. |
| Francis 2003 | Randomised study assessing the effects of HEPA filter when compared with vacuum cleaner. This study was excluded as no placebo HEPA filter was included in the study. |
| Gore 2003 | Before and after study. |
| Karlsson 2004 | Scholl‐based study. |
| Reisman 1990 | This randomised trial was conducted with patients who had an allergy to house dust mite. |
| Sabbah 2000 | Review article. |
| van der Heide 1997 | This randomised double‐blind study focused on participants with an allergic reaction to house dust mite allergen. Pet ownership was not an inclusion criteria, although in one third of the homes of participants, pets were resident. Pet allergic participants were included but only if they had an allergic reaction to house dust mite allergen. |
| Villaveces 1977 | Double‐blind non‐randomised crossover study. |
Characteristics of ongoing studies [ordered by study ID]
Rolfsjord 2005.
| Trial name or title | Air cleaners for children and adolescents with asthma and dog allergy |
| Methods | |
| Participants | Children/adolescents |
| Interventions | Air cleaners |
| Outcomes | Not reported |
| Starting date | |
| Contact information | |
| Notes | www.clinicaltrials.gov |
Contributions of authors
SK conceived and wrote the protocol. Abstracts were read by SK and TL. Data were extracted independently by SK and TL and data were entered by TL and SK. TL and SK developed the results and discussion sections. TL wrote the abstract and synopsis. TL translated papers from French and German.
Sources of support
Internal sources
School of Postgraduate Medicine, University of Portsmouth, UK.
External sources
Garfield Weston Foundation, UK.
Declarations of interest
None known.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
van der Heide 1999 {published data only}
- Heide S, Aaldsen WMC, KauffmanHF, Dubois AEJ, Monchy JGR. Clinical effects of air cleaners in homes of asthmatic children sensitized to pet allergen. Journal of Allergy and Clinical Immunology 1999;104(2):447‐51. [DOI] [PubMed] [Google Scholar]
Wood 1998 {published data only}
- Wood RA, Johnson EF, Natta ML, Hua Chen P, Eggleston PA. A placebo‐controlled trial of a HEPA air cleaner in the treatment of cat allergy. American Journal of Respiratory and Critical Care Medicine 1998;158:115‐20. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Antonicelli 1991 {published data only}
- Antonicelli L, Bilo MB, Pucci S, Schou C, Bonifazi F. Efficacy of an air‐cleaning device equipped with a high efficiency particulate air filter in house dust mite respiratory allergy. Allergy 1991;46:594‐600. [DOI] [PubMed] [Google Scholar]
Bjornsdottir 2003 {published data only}
- Bjornsdottir US, Jakobinudottir S, Runarsdottir V, Juliusson S. The effect of reducing levels of cat allergen (Fel d 1) on clinical symptoms in patients with cat allergy. Annals of Allergy, Asthma, & Immunology 2003;91(2):189‐94. [DOI] [PubMed] [Google Scholar]
Boquete 1997 {published data only}
- Boquete M, Cortada Macias JM, Gonzalez JJG, Ibero M, Cocera CM. Effectiveness of air purification with HEPA filter in domestic environmental control [Eficacia de un purificador de aire con filtro HEPA en el control ambinetal domiciliario]. Revista Espanola de Alergologia e Immunologia Clinica 1997;12(4):258‐64. [Google Scholar]
Carter 2001 {published data only}
- Carter MC, Perzanowski MS, Raymond A, Platts‐Mills TA. Home intervention in the treatment of asthma among inner‐city children. Journal of Allergy & Clinical Immunology 2001;108(5):732‐7. [DOI] [PubMed] [Google Scholar]
De Blay 2003 {published data only}
- Blay F, Fourgaut G, Hedelin G, Vervloet D, Michel FB, Godard P, et al. Medical indoor environment counselor (MIEC): role in compliance with advice on mite allergen avoidance and on mite allergen exposure. Allergy: European Journal of Allergy and Clinical Immunology 2003;58(1):27‐33. [DOI] [PubMed] [Google Scholar]
Francis 2003 {published data only}
- Francis H, Fletcher G, Anthony C, Pickering C, Oldham L, Hadley E, et al. Clinical effects of air filters in homes of asthmatic adults sensitized and exposed to pet allergens. Clinical & Experimental Allergy 2003;33:101‐5. [DOI] [PubMed] [Google Scholar]
Gore 2003 {published data only}
- Gore RB, Bishop S, Durrell B, Curbishley L, Woodcock A, Custovic A. Air filtration units in homes with cats: can they reduce personal exposure to cat allergen?. Clinical & Experimental Allergy 2003;33(6):765‐9. [DOI] [PubMed] [Google Scholar]
Karlsson 2004 {published data only}
- Karlsson AS, Andersson B, Renstrom A, Svedmyr J, Larsson K, Borres MP. Airborne cat allergen reduction in classrooms that use special school clothing or ban pet ownership. Journal of Allergy & Clinical Immunology 2004;113(6):1172‐7. [DOI] [PubMed] [Google Scholar]
- Karlsson AS, Benstrom A, Hedren M, Larsson K. Allergen avoidance does not alter airborne cat allergen levels in classrooms. Allergy 2004;59(6):661‐7. [DOI] [PubMed] [Google Scholar]
Reisman 1990 {published data only}
- Reisman RE, Mauriello PM, Davis GB, Georgitis JW, DeMasi JM. A double‐blind study of the effectiveness of a high‐efficiency particulate air(HEPA) filter in the treatment of patients with perennial allergic rhinitis and asthma. Journal of Allergy and Clinical Immunology 1990;85:1050‐9. [DOI] [PubMed] [Google Scholar]
Sabbah 2000 {published data only}
- Sabbah A. The role of air purifiers in the prevention of respiratory allergy [L'intérêt des purificateurs d'air dans la prévention de l'allergie respiratoire]. Allergie et Immunologie 2000;32(6):242‐5. [PubMed] [Google Scholar]
van der Heide 1997 {published data only}
- Heide S, Kauffman HF, Dubois AE, Monchy JG. Allergen reduction measures in houses of allergic asthmatic patients: effects of air‐cleaners and allergen‐impermeable mattress covers. European Respiratory Journal 1997;10:1217‐23. [DOI] [PubMed] [Google Scholar]
Villaveces 1977 {published data only}
- Villaveces JW, Rosengren H, Evans J. Use of laminar air flown portable filter in asthmatic children. Annals of allergy 1977;38(6):400‐4. [PubMed] [Google Scholar]
References to ongoing studies
Rolfsjord 2005 {unpublished data only}
- Air cleaners for children and adolescents with asthma and dog allergy. Ongoing study Starting date of trial not provided. Contact author for more information.
Additional references
ATS 1962
- American thoracic society committee on diagnostic standards. Definitions and classification of chronic bronchitis, asthma and pulmonary emphysema. American Review of Respiratory Disease 1962;85:762‐8. [Google Scholar]
Avner 1997
- Avner DB, Perzanowski MS, Platts‐Mills TA, Woodfolk JA. Evaluation of different techniques for washing cats: quantitation of allergen removed from the cat and the effect on airborne Fel d 1. Journal of Allergy & Clinical Immunology 1997;100(3):307‐12. [DOI] [PubMed] [Google Scholar]
Balfour Lynn 1999
- Balfour Lynn I. Difficult asthma: beyond the guidelines. Archives of Disease in Childhood 1999;80:201‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bjornsson 1996
- Bjornsson E, Janson C, Hakansson L, Enander I, Venge P, Boman G. Eosinophil peroxidase: a new serum marker of atopy and bronchial hyper‐responsiveness. Respiratory Medicine 1996;90(1):39‐46. [DOI] [PubMed] [Google Scholar]
BTS 1997
- British Thoracic Society. Asthma in adults and schoolchildren. Thorax 1997;52(Suppl 1):2‐8. [Google Scholar]
Custovic 1998
- Custovic A, Simpson A, Pahdi H, Green RM, Chapman MD, Woodcock A. Distribution, aerodynamic characteristics, and removal of the major cat allergen Fel d 1 in British homes. Thorax 1998;53(1):33‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Eriksson 1996
- Eriksson NE, Holmen A. Skin prick tests with standardized extracts of inhalant allergens in 7099 adult patients with asthma or rhinitis: cross‐sensitizations and relationships to age, sex, month of birth and year of testing. Journal of Investigational Allergology & Clinical Immunology 1996;6:36‐46. [PubMed] [Google Scholar]
Gotzsche 2008
- Gøtzsche PC, Johansen HK. House dust mite control measures for asthma. Cochrane Database of Systematic Reviews 2008, Issue 2. [DOI: 10.1002/14651858.CD001187.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hodson 1999
- Hodson T, Custovic A, Simpson A, Chapman M, Woodcock A, Green R. Washing the dog reduces dog allergen levels, but the dog needs to be washed twice a week. Journal of Allergy & Clinical Immunology 1999;103(4):581‐5. [DOI] [PubMed] [Google Scholar]
Huss 1992
- Huss K, Squire EN, Carpenter GB, Smith LJ, Huss RW, Salata K, et al. Effective education of adults with asthma who are allergic to dust mites. Journal of Allergy & Clinical Immunology 1992;89:836‐43. [DOI] [PubMed] [Google Scholar]
Jadad 1996
- Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds JM, Gavaghan DJ, et al. Assessing the quality of reports of randomized controlled trials: Is blinding necessary?. Controlled Clinical Trials 1996;134:1‐12. [DOI] [PubMed] [Google Scholar]
Jones 2003
- Jones PW. An introduction to systematic reviews in respiratory medicine. Respiratory Medicine 2003;97:97‐103. [DOI] [PubMed] [Google Scholar]
Lonnkvist 1999
- Lonnkvist K, Hallden G, Dahlen SE, Enander I, Hage‐Hamsten M, Kumlin M, et al. Markers of inflammation and bronchial reactivity in children with asthma, exposed to animal dander in school dust. Pediatric Allergy & Immunology 1999;10(1):45‐52. [DOI] [PubMed] [Google Scholar]
Pearce 1999
- Pearce N. How much asthma is really attributable to atopy?. Thorax 1999;54(3):268‐72. [DOI] [PMC free article] [PubMed] [Google Scholar]
Perzanowski 1997
- Perzanowski MS, Wheatley LM, Avner DB, Woodfolk JA, Platts‐Mills TA. The effectiveness of Allerpet/c in reducing the cat allergen Fel d 1. Journal of Allergy & Clinical Immunology 1997;100(3):428‐30. [DOI] [PubMed] [Google Scholar]
Prodigy
- Prodigy. http://www.prodigy.nhs.uk/.
Roost 1999
- Roost HP, Kunzli N, Schindler C, Jarvis D, Chinn S, Perruchoud AP, et al. Role of current and childhood exposure to cat and atopic sensitization. Journal of Allergy & Clinical Immunology 1999;104(5):941‐7. [DOI] [PubMed] [Google Scholar]
SIGN 1998
- The Scottish Intercollegiate Guidelines Network (SIGN). Primary Care Management of Asthma. http://www.sign.ac.uk/ 1998.
von Mutius 2001
- Mutius E. Is asthma really linked to atopy?. Clinical and Experimental Allergy 2001;31:1651‐2. [DOI] [PubMed] [Google Scholar]
Wanger 1999
- Wanger JS, Dockhorn RJ. Correlation of cat‐hair (Fel D1) prick skin test to airway response using a live‐cat‐room challenge model. Allergy & Asthma Proceedings 1999;20(6):371‐6. [DOI] [PubMed] [Google Scholar]


