Abstract
Background:
Baseball and softball are popular sports in the United States and are responsible for a large number of youth sports injuries each year.
Purpose:
To investigate recent differences in youth baseball and softball injuries evaluated in nationwide emergency departments.
Study Design:
Descriptive epidemiology study.
Methods:
The National Electronic Injury Surveillance System (NEISS) database was examined for softball and baseball injuries in pediatric patients (age, 7-21 years) from 2010 through 2019. Patients were classified as children (age, 7-13 years), adolescents (age, 14-18 years), or young adults (age, 19-21 years). Case narratives were used to categorize injuries as contact injuries (hit by bat or ball), field injuries (sliding into base, collision with another player, catching, or running), throwing injuries, or other.
Results:
An unweighted total of 24,717 baseball injuries and 13,162 softball injuries were recorded. A nationwide estimate of 861,456 baseball injuries and 511,117 softball injuries were sustained during the studied time period, with estimated respective injury rates of 86,146 and 51,112 per year. Injured softball players were most commonly adolescent (47%) and female (92%), while injured baseball players were most commonly children (54%) and male (90%). There was a greater proportion of baseball-related injuries involving the head/neck (41%) as compared with softball-related injuries (30%) (P < .01). Conversely, a greater proportion of softball-related injuries involved the lower extremity (32%) as compared with baseball-related injuries (19%) (P < .01). When comparing diagnosis, softball injuries were more often sprains/strains (28%) than baseball injuries (18%) (P < .01). When comparing mechanisms of injury, baseball athletes were more likely to be evaluated with contact injuries than were softball athletes (49% vs 40%, P < .01).
Conclusion:
Youth baseball athletes were more likely to be injured through contact mechanisms and had a higher proportion of injuries related to the head/neck/face, whereas softball injuries more frequently involved the lower extremity and resulted in a sprain/strain. League guidelines should focus on reducing contact injuries within youth baseball, and injury-prevention programs should focus on reducing lower extremity injuries in youth softball.
Keywords: pediatric, athlete, emergency department, baseball, softball, sports
Baseball and softball are a large source of youth sports injuries every year, with studies estimating an injury rate of 0.61 to 1.47 per 1000 athlete-exposures (AEs) and 0.61 to 1.42 per 1000 AEs for youth participating in baseball and softball, respectively. 7 Youth athletes are particularly susceptible to injury because of the vulnerability of growing cartilage, differences in body proportions, and ongoing development of musculoskeletal strength and coordination. 1,39 Moreover, the annual cost of pediatric baseball and softball injuries in the United States is estimated to be between $1 billion and $4 billion when accounting for psychosocial impact, presenting a significant burden on health care expenditures. 6 More than 120,000 baseball and softball injuries are seen in hospital emergency departments (EDs) annually within the United States. 4,20 It is important to assess, characterize, and compare the types of youth baseball and softball injuries evaluated in the ED to reduce avoidable health care expenses and prevent injuries with long-lasting effects on pediatric athletes.
Youth baseball and softball injuries can be broadly categorized as acute or overuse injuries. Overuse injuries are due to repetitive muscle use and can result in tendonitis, strains, and sprains. 19,33,41 Overuse injuries are most often caused by noncontact mechanisms of injury. For example, repetitive throwing without rest can result in proximal humeral epiphysiolysis, otherwise known as Little League shoulder. 11 In contrast, acute injuries are due to a sudden force or change in direction of motion and can result in concussions, fractures, and dislocations. 10,30,35 Contact mechanisms of injury, such as being hit by a bat or ball, are most likely to result in an acute injury. 13,22,23,40
Although baseball and softball share several similarities, there are important differences that lead to distinct rates and types of injury. For example, the underarm technique of softball pitching places more load on the shoulder than the elbow, 14 resulting in a higher rate of pitching-related shoulder injuries in youth softball and a higher rate of pitching-related elbow injuries among youth baseball. 29,41 As a result, baseball-specific and softball-specific pitch count limits and regulations were established across Little League Baseball and Softball. 31
However, the impact of other differences between baseball and softball, such as athlete characteristics and playing techniques, is not as well understood. Softball players are mostly female and may be at risk for different injuries than baseball players are, who are mostly male. For example, previous studies have shown that female youth athletes are at greater risk for severe injuries that often require surgery. 5,37 Other important differences include field size, frequency of Little League games, and ball design, which may all contribute to specific patterns of injury for softball and baseball. It is important to characterize these injury differences in order to establish more sport-specific safety guidelines and guide the development of sport-specific injury prevention programs.
Here, we compare the presentation of recent youth baseball and softball injuries evaluated in the ED and examine differences in site of injury, diagnoses, and mechanisms of injury. We hypothesized that baseball players would have more contact and upper extremity injuries, whereas softball players would have more noncontact and lower extremity injuries. These possible differences could lead to the implementation of more protective equipment or lower extremity injury-prevention programs within these sports.
Methods
The National Electronic Injury Surveillance System (NEISS) is a publicly available database managed by the US Consumer Product Safety Commission (CPSC) that contains data related to sports, recreational activities, and consumer products. 12 It pulls from 100 randomly selected EDs that represent a stratified probability sample of all US hospitals with a 24-hour ED and at least 6 beds. Each entry contains date of admission, disposition from the ED, patient age, race, ethnicity, sex, diagnosis, injured body part(s), activity involved, location where injury occurred, and a brief case narrative describing the circumstances of the injury.
The NEISS database was examined for all softball (activity code 5034) and baseball (activity code 5041) injuries involving patients aged 7 to 21 years from 2010 through 2019. This age range was chosen because many children begin engaging with softball and baseball at 7 years of age, which has been used as the lower age limit in other studies. 4 The upper limit was 21 years because it represents the final year of college for athletes who choose to compete at the collegiate level. Inclusion criteria included injuries received during competition, practice, or other practice-related activities, resulting in 40,256 unweighted cases. Exclusion criteria were cases that had unrelated diagnoses, unrelated injured body parts, and injuries that occurred at locations unrelated to practice or competition (n = 2337) (Appendix Table A1).
Patients were classified by age as children (age, 7-13 years), adolescents (age, 14-18 years), and young adults (age, 19-21 years). Cases were classified into 4 mechanisms of injury using the case narrative: (1) contact injuries: those received by being hit by the bat or ball; (2) field injuries: those received while sliding into base, from player-on-player collision, during catching, or during running; (3) throwing injuries: those received while throwing or pitching the ball; and (4) unknown/other. These categories were chosen because they represent distinct aspects of play that may differ between softball and baseball. An algorithm developed by one of the authors (A.L.) was used to search the case narrative of each injury to determine the mechanism of injury. The algorithm was compared with the manual classification of 1000 cases to verify accuracy. Details of the injury-mechanism analysis based on case narrative are found in Appendix Table A2. Injured body part was classified as head/neck/face, trunk, lower extremity, or upper extremity. In cases in which there was more than 1 injured body part, only the injured body part most relevant to the injury, as defined by the CPSC coding manual, was included for analysis. Diagnoses were grouped as fractures/dislocations, concussions, superficial injuries (contusion, laceration, puncture), internal injuries, sprains/strains, and other. Severe cases were defined as cases that required hospitalization, transfer, admission to the hospital for observation, or death. 16
Injury proportions were compared between baseball and softball with respect to the mechanism of injury, affected body part, diagnosis, and severity. Subsequently, injuries that occurred because of contact, field, or throwing were specifically compared with respect to affected body part, diagnosis, and severity. Data were analyzed using Stata Version 16 (StataCorp). Statistical weights provided by the CPSC were used to calculate national injury estimates. Results for all analyses were reported as overall national estimates, estimated percentages, and estimated 95% confidence intervals (CIs). Statistical comparisons included uncorrected Pearson χ2 tests with 95% CIs. The significance for all analyses was set at P <.05.
Results
Population Characteristics
A nationwide estimate of 1,372,573 injuries were sustained during the time period, with 861,456 injuries resulting from baseball and 511,117 injuries resulting from softball, with respective injury rates of 86,146 and 51,112 injuries per year (P < .01) (Table 1). The combined population had a mean age of 13.6 years (95% CI, 13.5-13.8 years), was 59.7% (95% CI, 57.4%-61.9%) male, and was 81.5% (95% CI, 74.7%-86.7%) White. A majority of baseball cases were children (53.7%; 95% CI, 51.5-56.0), as opposed to softball cases, which were most often adolescent (47.5%; 95% CI, 45.6-49.4) (P < .01). A vast majority of baseball cases were male (90.1%; 95% CI, 88.8-91.3), whereas softball cases were mostly female (91.5%; 95% CI, 89.9-92.9) (P < .01). There was no significant difference when evaluating race, and White patients made up the majority of baseball cases (80.2%; 95% CI, 72.8-85.9) and softball cases (83.6%; 95% CI, 77.3-88.4).
Table 1.
Sport-Specific Characteristics of Pediatric Athlete Injuries Evaluated in the ED, as Surveyed by NEISS a
| Characteristic | Baseball Injuries | Softball Injuries | P Value | ||
|---|---|---|---|---|---|
| National Estimate | Proportion (95% CI) | National Estimate | Proportion (95% CI) | ||
| Total cases | 861,456 | 62.76 (60.44-65.03) | 511,117 | 37.24 (34.97-39.56) | <.01 |
| Age Children, 7-13 y Adolescent, 14-18 y Young adult, 19-21 y |
462,759 308,603 90,093 |
53.72 (51.47-55.95) 35.82 (34.05-37.64) 10.46 (9.14-11.94) |
201,768 242,615 66,735 |
39.48 (37.17-41.83) 47.47 (45.58-49.36) 13.06 (11.50-14.78) |
<.01 |
| Sex Male Female |
776,111 85,345 |
90.09 (88.79-91.26) 9.91 (8.74-11.21) |
43,391 467,726 |
8.49 (7.10-10.12) 91.51 (89.88-92.90) |
<.01 |
| Ethnicity White Black Asian Other |
489,907 58,046 6965 56,318 |
80.15 (72.76-85.92) 9.50 (6.31-14.05) 1.14 (0.47-2.72) 9.21 (5.48-15.09) |
316,484 30,598 2354 29,229 |
83.58 (77.30-88.38) 8.08 (5.56-11.60) 0.62 (0.30-1.27) 7.72 (4.24-13.65) |
.11 |
a Values represent the national estimates derived from the National Electronic Injury Surveillance System (NEISS). Bolded P values indicate statistically significant differences between study cohorts (P < .05). ED, emergency department.
Overall Injuries
Table 2 details the injury characteristics by sport. When evaluating injury mechanisms, most baseball (49.2%) and softball (39.7%) cases were caused by contact. Other baseball cases included 25.3% field injuries, 3.0% throwing injuries, and 22.5% other injuries. In comparison, softball cases were 27.0% field injuries, 2.0% throwing injuries, and 31.3% other injuries (P < .01).
Table 2.
Characterization of Sport-Specific Injuries Evaluated in the ED, as Surveyed by NEISS a
| Characteristic | Overall Baseball Injuries | Overall Softball Injuries | P Value | ||
|---|---|---|---|---|---|
| National Estimate | Proportion (95% CI) | National Estimate | Proportion (95% CI) | ||
| Injury mechanism Contact b Field Throwing Other |
423,672 217,715 26,097 193,972 |
49.18 (47.43-50.93) 25.27 (23.53-27.10) 3.03 (2.66-3.45) 22.52 (20.56-24.60) |
202,819 138,090 10,178 160,030 |
39.68 (38.11-41.28) 27.02 (25.13-28.99) 1.99 (1.64-2.42) 31.31 (28.75-33.99) |
<.01 |
| Body part Head/neck/face b Trunk Lower extremity b Upper extremity |
351,077 59,722 165,423 284,370 |
40.80 (39.27-42.34) 6.94 (6.38-7.55) 19.22 (18.53-19.93) 33.04 (31.60-34.52) |
153,770 28,133 161,784 166,313 |
30.15 (28.16-32.22) 5.52 (5.00-6.09) 31.72 (30.29-33.19) 32.61 (30.70-34.58) |
<.01 |
| Diagnosis Fracture/dislocation b Concussion Superficial injury Internal injury Sprain/strain b Other |
185,259 35,255 290,173 76,639 156,340 117,790 |
21.51 (20.06-23.02) 4.09 (3.42-4.89) 33.68 (31.71-35.72) 8.90 (7.96-9.93) 18.15 (16.66-19.74) 13.67 (10.26-17.99) |
83,364 25,066 149,953 34,294 145,530 72,910 |
16.31 (15.01-17.70) 4.90 (4.18-5.74) 29.34 (27.13-31.65) 6.71 (5.48-8.19) 28.47 (25.74-31.38) 14.26 (10.10-19.76) |
<.01 |
| Disposition Treated/released Treated/admitted b Other |
836,030 16,997 8429 |
97.05 (96.45-97.55) 1.97 (1.66-2.35) 0.98 (0.66-1.44) |
502,250 6003 2864 |
98.27 (97.82-98.62) 1.17 (0.91-1.51) 0.56 (0.39-0.80) |
<.01 |
| Severity Severe b Not severe |
18,207 843,248 |
2.11 (1.77-2.52) 97.89 (97.48-98.23) |
6431 504,670 |
1.26 (0.98-1.62) 98.74 (98.38-99.02) |
<.01 |
a Values represent the national estimates derived from National Electronic Injury Surveillance System (NEISS) cases. ED, emergency department.
b Rows with important differences between baseball and softball.
The distribution of the affected body region also differed significantly between baseball and softball (P < .01). The head/neck/face was the most commonly injured body part among baseball cases, representing 40.8% of injuries. In comparison, the upper extremity was the most commonly injured body part for softball cases, representing 32.6% of injuries. Baseball cases also had a much lower proportion of lower extremity injuries (19.2%) as compared with softball injuries (31.7%).
There was a significant difference with respect to diagnoses between baseball and softball injuries (P < .01). Superficial injury was most common among both baseball (33.7%) and softball (29.3%), and there was a similar prevalence of fracture/dislocation (21.5% and 16.3%), concussion (4.1% and 4.9%), and internal injury (8.9% and 6.7%) among both sports. However, sprain/strain was more prevalent among softball (28.5%) than baseball (18.2%). Baseball had more severe injuries (2.11%) than softball (1.26%) (P < .01), and similarly, baseball had more cases that were treated and admitted (1.97%) than softball (1.17%) (P < .01).
Contact Injuries
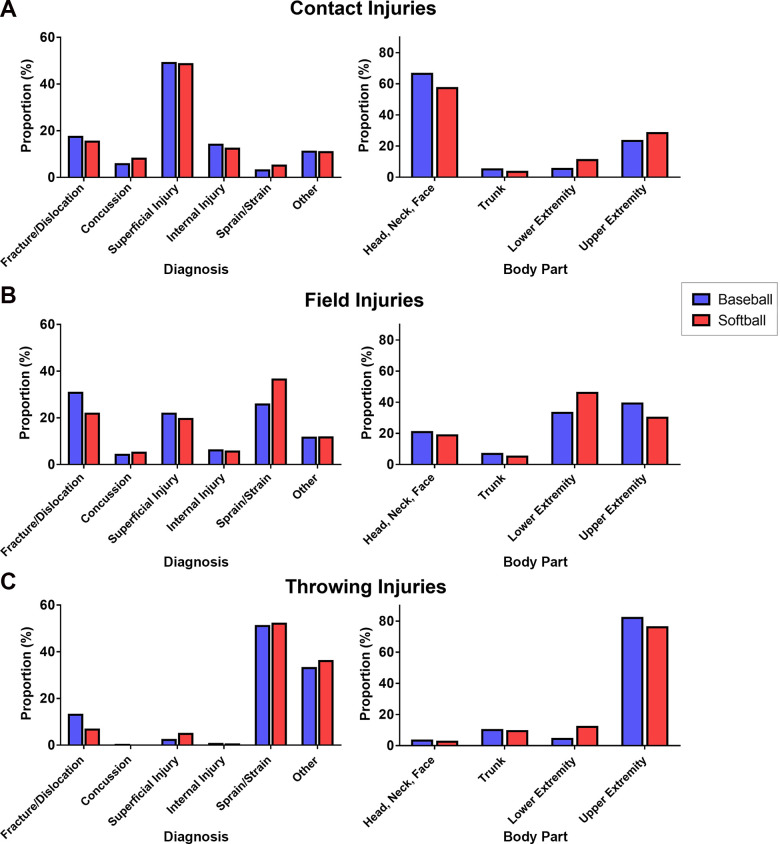
Comparisons of contact injuries according to sport are shown in Figures 1A and 2A. Contact injuries evaluated in the ED were most likely to affect the head/neck/face region in both baseball cases (66%) and softball cases (57%). However, contact injuries were more likely to affect the lower extremity in softball cases (11%) as compared with baseball cases (5.3%) (P < .01). Contact injuries were similarly likely to affect the trunk (5% and 3%) and upper extremity (23% and 28%) in baseball and softball cases. When considering diagnosis, contact injuries were most likely to result in superficial injury among both sports (49% and 48%). Contact injuries also resulted in similar proportions of internal injury (14% and 12%) and fracture/dislocation (17% and 15%). However, softball contact injuries were slightly more likely to result in sprain/strain (5% vs 3%) and concussion (8% vs 6%) as compared with baseball injuries (P < .01). Baseball contact injuries were more often severe (2.1%) than contact injuries in softball (0.9%) (P < .01), and patients evaluated with baseball contact injuries were more likely to be treated and admitted (2.0%) than those evaluated with softball contact injuries (0.8%) (P < .01).
Figure 1.
Comparison of diagnosis and injured body part between baseball and softball. (A) When comparing contact injuries, there was a significant difference in diagnosis (P < .01) and injured body part (P < .01). (B) There was also a difference among field injury diagnosis (P < .01) and injured body part (P < .01). (C) When comparing throwing injuries, there was a difference among injured body part (P < .01) but not diagnosis (P = .12).
Figure 2.
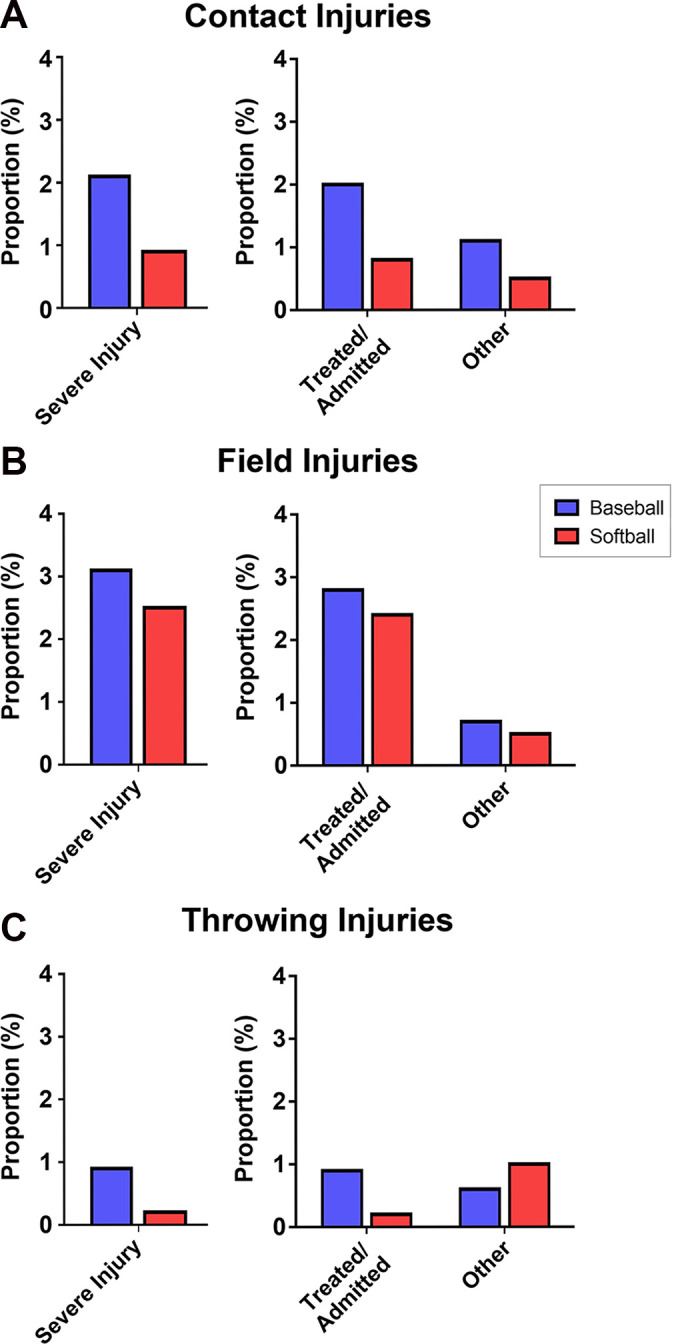
Comparison of disposition and severity between baseball and softball. (A) When comparing contact injuries, there was a significant difference in disposition (P < .01) and severity (P < .01). (B) There was no difference among field injury disposition (P = .19) or severity (P = .16). (C) When comparing throwing injuries, there was a difference among severity (P = .014) but not disposition (P = .35).
Field Injuries
Comparisons of field injuries by sport are shown in Figures 1B and 2B. Field injuries were most likely to affect the upper extremity in baseball cases (39%) but were most likely to affect the lower extremity in softball cases (46%) (P < .01). However, field injuries affected the head/neck/face (21% and 19%) and trunk (7% and 5%) similarly in baseball and softball. Additionally, the most common diagnosis for field injuries was fracture/dislocation among baseball cases (31%) and sprain/strain among softball cases (36%) (P < .01). Otherwise, field injuries were similarly likely to result in concussion (4% and 5%), superficial injury (22% and 19%), internal injury (6% and 6%), and other injuries (12% and 12%) in baseball and softball cases. There was no significant difference in injury disposition (P = .19) or severity (P = .16) between field injuries in either sport, with 3.1% and 2.5% of injuries found to be severe and 2.8% and 2.4% of injuries being treated and admitted among baseball and softball cases, respectively.
Throwing Injuries
Comparisons of throwing injuries by sport are shown in Figures 1C and 2C. Throwing injuries among baseball and softball cases were most likely to affect the upper extremity (82% and 76%), but softball cases had a higher proportion of lower extremity injuries (12%) as compared with baseball (4%) (P = .007). Otherwise, throwing injuries were similarly likely to affect the head/neck/face (3% and 3%) and trunk (10% and 9%) in both sports. There was no significant difference in injury diagnosis (P = .12), and most throwing injuries resulted in sprain/strain (51% and 52%), fracture/dislocation (13% and 7%), or other diagnoses (33% and 36%). Baseball throwing injuries were more likely to be severe (0.9%) than softball throwing injuries (0.2%) (P = .014), but were not more likely to be treated and admitted (P = .35).
Discussion
Here, we investigated whether there were differences between youth baseball and softball injuries with respect to mechanism of injury, affected body part, or diagnosis. Baseball injuries were more severe and more likely to affect the head/neck/face region, whereas softball injuries were more likely to affect the lower extremity. Baseball injuries had a greater proportion of fractures/dislocations as compared with softball injuries, which had a greater proportion of sprains/strains. Contact injuries were most common among both sports, but baseball had a higher proportion of contact injuries and an increased severity of contact injuries. Moreover, field injuries more commonly resulted in fractures/dislocations and affected the upper extremity in baseball cases, but more often, they resulted in sprains/strains and affected the lower extremity in softball cases. Throwing injuries were also more likely to affect the lower extremity in softball cases as compared with baseball cases.
Previous studies have also shown that the majority of youth baseball injuries evaluated in the ED most commonly affect the head/neck/face and most often result in soft tissue injuries. 20,38 Moreover, these studies found that being hit by the ball was the most common mechanism of injury for baseball cases. 20,38 Similar studies of softball players have found a more even distribution of injuries in the lower extremity, upper extremity, and head/neck/face region among pediatric cases. 4 Birchak et al 4 also found that pediatric softball players were more likely to be evaluated after being hit by a ball as compared with adult cases. Our results are largely consistent with these previous findings and demonstrate that youth baseball and softball players have differences in injury presentation, such as a higher proportion of head/neck/face injuries among baseball players and a higher proportion of lower extremity injuries among softball players.
The increased incidence of head/neck/face injuries and superficial injury diagnoses among baseball cases is likely reflective of the fact that baseball players were more likely to be injured because of contact mechanisms than were softball players. The results of this study show that the head/neck/face is the most common site of contact injuries and that superficial injuries, such as contusions and lacerations, are the most common diagnoses. This observation is also consistent with other studies that have reported higher rates of oral and maxillofacial injuries due to contact sports. 28
The prevalence and severity of baseball and softball injuries evaluated in the ED, underscored by annual pediatric baseball injury rates of more than 100,000 in previous decades, call for increased safety measures and protective equipment. 20 This is especially important with regard to youth baseball players, who were found to have more severe contact injuries in this study. Previous safety efforts to reduce impact injuries within baseball have shown mixed results. The use of softer-core baseballs and chest protectors composed of various materials has shown inconsistent results in reducing impact injury to the chest. 18,26 However, Marshall et al 21 demonstrated that the use of face guards and a safety ball called the reduced-impact ball reduced the risk of ball-related injury and facial injury. Fewer studies have assessed the efficacy of softer balls and face guards within softball, but some studies have shown that fielder’s masks could reduce the impact of being struck by the ball and reduce the risk of facial fracture. 24,36 Although baseball had a higher rate of contact injuries, the majority of softball injuries within softball were also due to contact. Further research into protective equipment, such as reduced-impact balls and face guards and face shields, is needed for youth softball injury prevention.
The increased prevalence of injuries affecting the lower extremity, including throwing injuries and field injuries, among softball players can be due to a variety of reasons. One of the most significant reasons is the dramatic sex gap that exists between the sports, as reflected by youth baseball cases being 90% male and youth softball cases being 92% female in this study. Female athletes are at increased risk for lower extremity injuries, such as anterior cruciate ligament and meniscal injuries, for a variety of proposed reasons, including increased joint laxity, decreased neuromuscular control, and other anatomic differences. 2,3,25,32 The increased prevalence of throwing injuries affecting the lower extremity is likely due to differences in throwing mechanics, which can affect the kinetic chain. For example, softball players demonstrate increased glenohumeral range of motion and bilateral symmetry as compared with baseball players. 34 Moreover, softball players rely more on hip complex stability, as shown by a concomitant decrease in hip range of motion and strength when experiencing upper extremity pain. 15,27 Studies have shown that injury-prevention programs can improve core stability among athletes and reduce the risk of ankle sprains and lower extremity injury among female athletes by improving neuromuscular control through a variety of strength, balance, plyometric, and core exercise training. 8,17 As such, there should be greater implementation of injury-prevention programs within youth softball to improve throwing mechanics and lower extremity neuromuscular control. There should also be a greater emphasis on teaching better techniques for base sliding, which can be a source of lower extremity field injuries. 9
Limitations
This study acquired data using the NEISS database, which utilizes a representative sample of 100 US EDs to estimate nationwide injury patterns and injury rates. As a result, data from the NEISS database are subject to sampling bias, and some types of injury may have been disproportionately over- or underrepresented. Moreover, the NEISS database only records a brief case narrative for each injury, and mechanisms of injury could not always be determined based on the lack of granular information in the case narratives. The NEISS database contains anonymous patient data and consequently does not report if patients have been evaluated multiple times, potentially leading to another source of error.
Additionally, not all softball and baseball injuries are evaluated in the ED. Many players may bring their injuries to urgent care centers or their athletic trainer, primary care physician, and orthopaedic surgeon without visiting the ED. In this way, visits to the ED are not completely representative of all injuries affecting baseball and softball players.
Conclusion
Differences in player characteristics and athletic technique predispose youth baseball and softball players to different patterns of injury. Youth baseball players are more likely to have injuries affecting the head/neck/face region, whereas youth softball players are at greater risk for sprains/strains and lower extremity injuries. Youth baseball players are more likely to have severe injuries, although the majority of all baseball and softball injuries are nonsevere. Injury-prevention programs to improve lower extremity neuromuscular control should be used more widely among youth softball players, and league guidelines should be improved to reduce the rate of contact injuries among both sports. Further studies should evaluate youth baseball and softball injury trends and the pattern of injury in other clinical contexts, such as sports medicine and urgent care visits.
APPENDIX
Table A1.
Patient Exclusion Criteria
| Exclusion Criterion | Description | No. of Excluded Cases (Unweighted) |
|---|---|---|
| Sport | Not attributable to a single sport | 72 |
| Location | Home, farm, street, mobile vehicle, or industrial area | 1926 |
| Diagnosis | Ingestion, aspiration, chemical burn, thermal burn, anoxia, electric shock, poisoning, or radiation | 63 |
| Body part | Ingested, full body, unknown | 316 |
| Total excluded | 2377 |
Table A2.
Algorithm for Determining Injury Mechanism From Case Narratives
| Mechanism: Contact Injury (n = 17,193 cases) |
| 1 AND 2 AND 3 AND 4 |
| 1. Contains “hit” or “struck” or “blow” or “ricochet” |
| 2. Does not contain “fell” or “slid” or “trip” or “slip” or “throwing” or “colli” or “ran into” or “catch” or “caught” |
| 3. Does not contain “dove” or “diving” followed by “ball” |
| 4. Does not contain “dove” followed by “base” |
| Mechanism: Throwing Injury (n = 1048 cases) |
| 1 AND 2 |
| 1. Contains “pitch” or throwing” |
| 2. Does not contain “pitching machine” or “hit” or “struck” or “at bat” or “colli” or “slid” |
| Mechanism: Field Injury (n = 9944 cases) |
| [1 OR 2 OR (3 AND 4 AND 5) OR (6 AND 7 AND 8 AND 9) OR 10] AND 11 |
| 1. Contains “slid” |
| 2. Contains “dove” then “base” |
| 3. Contains “colli” |
| 4. Contains “ran into” |
| 5. Contains “player” or “catcher” or “someone” |
| 6. Contains “catch” or “caught” |
| 7. Contains “dove” then “ball” |
| 8. Contains “diving” then “ball” |
| 9. Does not contain “batting cage” |
| 10. Contains “slip” or “ran into” or “fell” or “trip” or “running” |
| 11. Not included in “unintended contact” or “throwing” mechanisms |
| Mechanism: Unknown/Other |
| 1. Not included in the “contact injuries,” “throwing injuries,” or “outfield injuries” mechanisms |
Footnotes
Final revision submitted July 3, 2021; accepted August 6, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: K.J.M. has received education payments from Smith & Nephew. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval was not sought for the present study.
References
- 1. Adirim TA, Cheng TL. Overview of injuries in the young athlete. Sports Med. 2003;33(1):75–81. [DOI] [PubMed] [Google Scholar]
- 2. Agel J, Rockwood T, Klossner D. Collegiate ACL injury rates across 15 sports: National Collegiate Athletic Association Injury Surveillance System data update (2004-2005 through 2012-2013). Clin J Sport Med. 2016;26(6):518–523. [DOI] [PubMed] [Google Scholar]
- 3. Beynnon BD, Vacek PM, Newell MK, et al. The effects of level of competition, sport, and sex on the incidence of first-time noncontact anterior cruciate ligament injury. Am J Sports Med. 2014;42(8):1806–1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Birchak JC, Rochette LM, Smith GA. Softball injuries treated in US EDs, 1994 to 2010. Am J Emerg Med. 2013;31(6):900–905. [DOI] [PubMed] [Google Scholar]
- 5. Brant JA, Johnson B, Brou L, Comstock RD, Vu T. Rates and patterns of lower extremity sports injuries in all gender-comparable US high school sports. Orthop J Sports Med. 2019;7(10):2325967119873059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Caine D, Caine C, Maffulli N. Incidence and distribution of pediatric sport-related injuries. Clin J Sport Med. 2006;16(6):500–513. [DOI] [PubMed] [Google Scholar]
- 7. Caine D, Maffulli N, Caine C. Epidemiology of injury in child and adolescent sports: injury rates, risk factors, and prevention. Clin Sports Med. 2008;27(1):19–50. [DOI] [PubMed] [Google Scholar]
- 8. Caldemeyer LE, Brown SM, Mulcahey MK. Neuromuscular training for the prevention of ankle sprains in female athletes: a systematic review. Phys Sportsmed. 2020;48(4):363–369. [DOI] [PubMed] [Google Scholar]
- 9. Camp CL, Curriero FC, Pollack KM, et al. The epidemiology and effect of sliding injuries in Major and Minor League Baseball players. Am J Sports Med. 2017;45(10):2372–2378. [DOI] [PubMed] [Google Scholar]
- 10. Carniol ET, Shaigany K, Svider PF, et al. “Beaned”: a 5-year analysis of baseball-related injuries of the face. Otolaryngol Head Neck Surg. 2015;153(6):957–961. [DOI] [PubMed] [Google Scholar]
- 11. Casadei K, Kiel J. Proximal humeral epiphysiolysis (Little League shoulder). In: StatPearls. StatPearls Publishing LLC; 2020. [PubMed] [Google Scholar]
- 12. Consumer Product Safety Commission. National Electronic Injury Surveillance System. Accessed October 1, 2020. https://www.cpsc.gov/Research--Statistics/NEISS-Injury-Data
- 13. Dawson WJ, Pullos N. Baseball injuries to the hand. Ann Emerg Med. 1981;10(6):302–306. [DOI] [PubMed] [Google Scholar]
- 14. Flyger N, Button C, Rishiraj N. The science of softball: implications for performance and injury prevention. Sports Med. 2006;36(9):797–816. [DOI] [PubMed] [Google Scholar]
- 15. Gilmer GG, Washington JK, Dugas JR, Andrews JR, Oliver GD. The role of lumbopelvic-hip complex stability in softball throwing mechanics. J Sport Rehabil. 2019;28(2):196–204. [DOI] [PubMed] [Google Scholar]
- 16. Griffin R, Parks CT, Rue LW III, McGwin G, Jr. Comparison of severe injuries between powered and nonpowered scooters among children aged 2 to 12 in the United States. Ambul Pediatr. 2008;8(6):379–382. [DOI] [PubMed] [Google Scholar]
- 17. Huxel Bliven KC, Anderson BE. Core stability training for injury prevention. Sports Health. 2013;5(6):514–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Janda DH, Viano DC, Andrzejak DV, Hensinger RN. An analysis of preventive methods for baseball-induced, chest impact injuries. Clin J Sport Med. 1992;2(3):172–179. [Google Scholar]
- 19. Krajnik S, Fogarty KJ, Yard EE, Comstock RD. Shoulder injuries in US high school baseball and softball athletes, 2005-2008. Pediatrics. 2010;125(3):497–501. [DOI] [PubMed] [Google Scholar]
- 20. Lawson BR, Comstock RD, Smith GA. Baseball-related injuries to children treated in hospital emergency departments in the United States, 1994-2006. Pediatrics. 2009;123(6):e1028–e1034. [DOI] [PubMed] [Google Scholar]
- 21. Marshall SW, Mueller FO, Kirby DP, Yang J. Evaluation of safety balls and faceguards for prevention of injuries in youth baseball. JAMA. 2003;289(5):568–574. [DOI] [PubMed] [Google Scholar]
- 22. Miller KN, Collins CL, Chounthirath T, Smith GA. Pediatric sports- and recreation-related eye injuries treated in US emergency departments. Pediatrics. 2018;141(2):e20173083. [DOI] [PubMed] [Google Scholar]
- 23. Montero E, Kistamgari S, Chounthirath T, et al. Pediatric sports- and recreation-related dental injuries treated in US emergency departments. Clin Pediatr. 2019;58(11-12):1262–1270. [DOI] [PubMed] [Google Scholar]
- 24. Morris TP, Gellner RA, Rowson S. Do infield softball masks effectively reduce facial fracture risk? Ann Biomed Eng. 2019;47(2):453–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Myer GD, Ford KR, Paterno MV, Nick TG, Hewett TE. The effects of generalized joint laxity on risk of anterior cruciate ligament injury in young female athletes. Am J Sports Med. 2008;36(6):1073–1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Nicholls RL, Elliott BC, Miller K. Impact injuries in baseball. Sports Med. 2004;34(1):17–25. [DOI] [PubMed] [Google Scholar]
- 27. Oliver GD, Gilmer GG, Friesen KB, et al. Functional differences in softball pitchers with and without upper extremity pain. J Sci Med Sport. 2019;22(10):1079–1083. [DOI] [PubMed] [Google Scholar]
- 28. Park HK, Park JY, Choi NR, Kim UK, Hwang DS. Sports-related oral and maxillofacial injuries: a 5-year retrospective study, Pusan National University Dental Hospital. J Oral Maxillofac Surg. 2021;79(1):203.e1-203.e8. doi:10.1016/j.joms.2020.07.218 [DOI] [PubMed] [Google Scholar]
- 29. Pytiak AV, Kraeutler MJ, Currie DW, McCarty EC, Comstock RD. An epidemiological comparison of elbow injuries among United States high school baseball and softball players, 2005-2006 through 2014-2015. Sports Health. 2018;10(2):119–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Rice SG, Congeni JA. Baseball and softball. Pediatrics. 2012;129(3):e842–e856. [DOI] [PubMed] [Google Scholar]
- 31. Rice SG, Congeni JA; Council on Sports Medicine and Fitness. Baseball and softball. Pediatrics. 2012;129(3):e842–e856. [DOI] [PubMed] [Google Scholar]
- 32. Rozzi SL, Lephart SM, Gear WS, Fu FH. Knee joint laxity and neuromuscular characteristics of male and female soccer and basketball players. Am J Sports Med. 1999;27(3):312–319. [DOI] [PubMed] [Google Scholar]
- 33. Saper MG, Pierpoint LA, Liu W, et al. Epidemiology of shoulder and elbow injuries among United States high school baseball players: school years 2005-2006 through 2014-2015. Am J Sports Med. 2018;46(1):37–43. [DOI] [PubMed] [Google Scholar]
- 34. Schilling DT, Mallace AJ, Elazzazi AM. Shoulder range of motion characteristics in Division III collegiate softball and baseball players. Int J Sports Phys Ther. 2019;14(5):770–784. [PMC free article] [PubMed] [Google Scholar]
- 35. Schneuer FJ, Bell JC, Adams SE, et al. The burden of hospitalized sports-related injuries in children: an Australian population-based study, 2005-2013. Inj Epidemiol. 2018;5(1):45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Strickland J, Bevill G. Experimental evaluation of softball protective headgear for defensive play. J Appl Biomech. 2019;35(3):202–208. [DOI] [PubMed] [Google Scholar]
- 37. Swenson DM, Collins CL, Best TM, et al. Epidemiology of knee injuries among U.S. high school athletes, 2005/2006-2010/2011. Med Sci Sports Exerc. 2013;45(3):462–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Trofa DP, Obana KK, Swindell HW, et al. Increasing burden of youth baseball elbow injuries in US emergency departments. Orthop J Sports Med. 2019;7(5):2325967119845636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Walters BK, Read CR, Estes AR. The effects of resistance training, overtraining, and early specialization on youth athlete injury and development. J Sports Med Phys Fitness. 2018;58(9):1339–1348. [DOI] [PubMed] [Google Scholar]
- 40. Wasserman EB, Register-Mihalik JK, Sauers EL, et al. The first decade of web-based sports injury surveillance: descriptive epidemiology of injuries in US high school girls’ softball (2005-2006 through 2013-2014) and National Collegiate Athletic Association women’s softball (2004-2005 through 2013-2014). J Athl Train. 2019;54(2):212–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Zaremski JL, Zeppieri G, Jr, Tripp BL. Sport specialization and overuse injuries in adolescent throwing athletes: a narrative review. J Athl Train. 2019;54(10):1030–1039. [DOI] [PMC free article] [PubMed] [Google Scholar]