Abstract
Introducing comprehensive surveillance is recommended as an urgent public health measure to control and mitigate the spread of coronavirus disease 2019 (COVID-19) worldwide. However, its implementation has proven challenging as it requires inter-organizational coordination among multiple healthcare stakeholders. The purpose of this study was to examine the role of soft and hard mechanisms in the implementation of inter-organizational coordination strategies for COVID-19 surveillance within Colombia, drawing on evidence from the cities of Bogotá, Cali and Cartagena. The study used a case study approach to understand the perspectives of local and national authorities, insurance companies and health providers in the implementation of inter-organizational coordination strategies for COVID-19 surveillance. Eighty-one semi-structured interviews were conducted between June and November 2020. The data were analysed by codes and categorized using New NVivo software. The study identified inter-organizational coordination strategies that were implemented to provide COVID-19 surveillance in the three cities. Both soft (e.g. trust and shared purpose) and hard mechanisms (e.g. formal agreements and regulations) acted as mediators for collaboration and helped to address existing structural barriers in the provision of health services. The findings suggest that soft and hard mechanisms contributed to promoting change among healthcare system stakeholders and improved inter-organizational coordination for disease surveillance. The findings contribute to evidence regarding practices to improve coordinated surveillance of disease, including the roles of new forms of financing and contracting between insurers and public and private health service providers, logistics regarding early diagnosis in infectious disease and the provision of health services at the community level regardless of insurance affiliation. Our research provides evidence to improve disease surveillance frameworks in fragmented health systems contributing to public health planning and health system improvement.
Keywords: Care coordination, care integration, inter-organizational, coordination, public health, COVID-19, qualitative research
Key messages.
This qualitative study examined new forms of inter-organizational coordination to support health system surveillance of COVID-19 in three Colombian cities.
The roles of, and interplay between, both ‘hard’ and ‘soft’ mechanisms for supporting inter-organizational relationships were highlighted, as collaboration was encouraged by a national emergency declaration and formal tripartite agreements locally which, in turn, improved inter-organizational trust and legitimized local leadership.
Using evidence from the introduction of coordinated disease surveillance, our findings highlight mechanisms for improving inter-organizational collaboration in market-based and fragmented health systems internationally.
Introduction
The widespread impact of the COVID-19 pandemic has made implementation of public health surveillance an urgent strategy of public health authorities to control and mitigate the disease within health systems internationally (Randazzo et al., 2020). Surveillance of COVID-19 aims to enable rapid detection, isolation, testing and monitoring of trends in cases and deaths; to identify, follow-up and impose quarantine upon potential contacts; to detect and contain clusters and outbreaks; to monitor epidemiologic trends and to contribute to understanding of the virus in different environments (World Health Organization, 2020). Epidemiological public health surveillance can also generate real-time data for decision-making on disease monitoring and control (Ibrahim, 2020). However, implementation of surveillance strategies in the context of a sanitary emergency has challenged health systems with varying resources internationally (Dalglish, 2020). One hypothesis for explaining such difficulties is that effective coordination among the different organizations within health systems is required to support adaptation to COVID-19 (Legido-Quigley et al., 2020). This paper outlines two propositions concerning the influence of structural (hard) and motivational (soft) mechanisms on coordination between health system organizations and examines their relevance in the coordination of public health surveillance of COVID-19 in Colombia.
Mechanisms influencing inter-organizational coordination
The emphasis on improving coordination, or how different organizations work together in the joint planning and delivery of care, is not new and has emerged in previous policy work on improving health systems, e.g. the longstanding agenda for coordinating care across institutions (Rummery, 2009; Shigayeva et al., 2010). Increased coordination of care has been subject to considerable research, including suggested barriers and enablers (Cameron et al., 2014; Vargas et al., 2016), and recommendations aimed at policymakers for supporting coordinated change (Best et al., 2012).
In evaluating the relevance of previous research on improving coordination arrangements to the challenges posed by COVID-19, we suggest that two qualifications are needed. First, health system changes in response to COVID-19 have been undertaken rapidly against a background of emergency or ‘crisis’ planning. Much of the health systems change literature has assumed judicious planning of change over a much longer time interval (e.g. assembling a robust evidence base and social coalition for change) (Turner et al., 2016a,b; Best et al., 2012). Little is known about how temporal constraints of introducing change in a context of emergency influences their planning and implementation. Second, the mechanisms of change in an emergency context, particularly the roles of and interplay between ‘softer’ and ‘harder’ mechanisms of change, could differ from those typically relied upon during ‘care as usual’ (Wensing et al., 2020).
Different perspectives on the key factors that influence coordination arrangements between institutions exist. One relates to structural challenges or impediments to coordinating different institutions within health systems. In relation to Latin America, structural difficulties of implementing comprehensive public health measures among different health systems have been suggested (Giovanella et al., 2020). Structural challenges include coordinating collective surveillance programmes (e.g. community strategies) with individual interventions (e.g. clinical treatment), prioritizing population needs over market rules, and encouraging collaboration between organizations that normally compete for patients (Giovanella et al., 2020).
To address such structural challenges, some of the literature on health system coordination emphasizes ‘hard’ interventions that influence formal relationships within health systems These include administration and regulatory change that promotes collaboration (Auschra, 2018), formalization of relationships (Casey, 2008), including inter-organizational contracting arrangements, and changes to the financing of organizations, including the provision of financial incentives linked to quality standards (Turner et al., 2016a). In response to the COVID-19 pandemic, emergency planning and preparedness, including the availability of slack resources, is hypothesized to support necessary adaptation of roles and responsibilities across the health system (Boin and Van Eeten, 2013).
Proposition 1: Structural barriers, e.g. market-like incentives, encourage health system fragmentation and undermine coordination among organizations
A structural perspective on coordination only considers structural properties of health systems and potential impediments arising from these. Another perspective on coordination emphasizes behavioural or motivational factors, including ‘soft’ incentives such as ‘shared purpose’ triggered in response to the significant threat to life posed by COVID-19. ‘Soft’ mechanisms of change refer to interpersonal or social processes that encourage shared commitment among organizations to a proposal for change. Inter-organizational collaborations can be conceptualized in an interpersonal way as ‘a negotiation between people from different organizations with a commitment to working together to secure improvements which could not have been achieved by acting alone’ (Dickinson, 2010, p. 815). Softer mechanisms include exercising political skill and leadership (Wildridge et al., 2004; Casey, 2008; Clarke et al., 2021), building trust and faith among collaborators (Huxham, 2003; Zuckerman et al., 1995), mutual successes and task achievement (Vangen and Huxham, 2003), ambition and authenticity, information exchange, interpersonal communication, a balance of power, sharing resources (Aunger et al., 2021) and stakeholder involvement, notably of powerful actors with the ability to stymie change (Best et al., 2012). In response to COVID-19, the emergency context might enrich interpersonal commitment in representing a ‘burning platform’ that requires rapid action to be addressed (Turner et al., 2021). For example, a study of a US academic medical centre found that the pandemic had become a ‘catalyst’ for improved teamwork among the centre’s staff (Srinivasan et al., 2020).
Proposition 2: ‘Soft’ motivational incentives, e.g. shared purpose, encourage informal coordination among organizations, even where structural incentives are lacking.
Taking into account these propositions about improving coordination arrangements between organizations, this paper addresses the following research question: what were the relative roles of structural and motivational incentives in shaping coordination arrangements among organizations to enable COVID-19 surveillance? It addresses this question using interviews with health system stakeholders in Colombia concerning how they perceived, and engaged in, inter-organizational collaboration to support surveillance of COVID-19.
The health system in Colombia
This study of the implementation of COVID-19 surveillance strategies is contextualized in the Colombian health system. Table 1 describes the characteristics of the Colombian health system and its response to COVID-19. It is composed of actors at multiple levels: public health surveillance is provided by departments and municipalities; healthcare provision is the responsibility of private and public insurers; national surveillance is the responsibility of the national institute of health and health regulations and insurance contracts are enforced by the national Ministry of Health. Due to the responsibilities of national bodies, there are similarities across local contexts due to their compliance with national surveillance and regulation; however, potential differences arise locally in public health surveillance and health service provision depending on the actions of local government and insurance companies.
Table 1.
Characteristics of the Colombian health system of its response to COVID-19
| Structure |
|
|
|
|
| Coverage |
| In Colombia, affiliation to the General Health Security System—SGSSS—is composed of two insurance schemes. The contributory that covers formally employed and independent workers and the subsidized that covers individuals classified as poor according to a proxy means test (SISBEN) (Escobar et al., 2009) |
|
| Financing sources |
|
| COVID-19 preparedness |
|
|
|
The Colombian health system has been characterized as fragmented, segmented and market-oriented (Hernández, 2002; Jaime, 2016). It has faced multiple dilemmas in recent years, including financing arrangements, appropriate access to healthcare, medical autonomy, and balancing the mix of public and private providers (Alvarez-Rosete and Hawkins, 2018; Amaya-Lara, 2016; Atun et al., 2015; Garcia-Subirats et al., 2014; Vargas Bustamante and Méndez, 2014). However, recent policy developments prior to COVID-19’s arrival promoted the strengthening of leadership of coordination arrangements between institutions, including ‘integrated health care networks’ (Vargas et al., 2018; 2015; Vázquez et al., 2015). From a structural perspective, the fragmentation of the system, both in service provision and in their planning, has been theorized to limit the speed of implementation of widescale epidemiological surveillance systems (Giovanella et al., 2020).
COVID-19 surveillance in Colombia
At a global level, epidemiological surveillance measures for infectious diseases have focussed on preventive strategies such as quarantine, early detection of cases and isolation. Surveillance data on positive events have been used for informing decision-making on adjusting public health actions during the outbreak of epidemics worldwide (Declich and Carter, 1994; Centers for Disease Control and Prevention, 1988). Even though Colombia has long required public health surveillance of infectious diseases such as dengue, malaria, leishmaniasis, chagas, zika and chikungunya, the unprecedented nature, scale and threat to life posed by COVID-19 represented a particular challenge for implementing public health surveillance. Like many countries internationally, Colombia promoted the WHO key COVID-19 recommendations for public health surveillance (World Health Organization, 2020).
The declaration of a national state of emergency in Colombia in March 2020 (República de Colombia, 2020a) allowed for greater flexibility over the financing of health services, including additional State funding, and the performance of individual and collective organizational roles within the health system. Drawing on the flexibility provided by the national state of emergency, the Ministry of Health published a national contingency plan to respond to the pandemic in April 2020 (Ministerio de Salud y Protección Social, 2020). Further national resolutions (e.g. República de Colombia, 2020b) empowered local authorities at the city and department level to take actions necessary to preserve public order and guarantee the health of their inhabitants. To support local public health responses to COVID-19, local authorities were encouraged to develop formal agreements among health system stakeholders within their locality to support coordinated actions in response to COVID-19. Formal agreements were reached in the localities studied in April (Cartagena), May (Cali) and September 2020 (Bogotá).
The need to formalize coordination between these actors was based on two factors. First, insurance companies’ responsibilities were limited to their affiliated users; they were not able to test and trace associated cases that had different insurance affiliations. In the majority of cases, a household, cluster or a specific geographical area of risk required the participation of multiple insurance companies to attend and assess the members of their particular insurance scheme (Figure 1). Second, the national health institute and the local health secretaries were unable to implement timely surveillance without collaboration with insurance companies nationally, which were often the first actors to be informed of potential cases. Even though these two actors were responsible for the surveillance of nationally notifiable diseases, including COVID-19, regardless of insurance affiliation, case numbers exceeded the testing and tracing capacity of these actors early in the pandemic, stimulating awareness of the need for improving inter-organizational collaboration. Comprehensive data on the effectiveness of domiciliary surveillance could not be identified; however, an executive manager of one national insurance provider indicated in a newspaper interview that 82% of positive cases were identified and monitored at home, without the need for hospital attendance (Portafolio, 2020).
Figure 1.
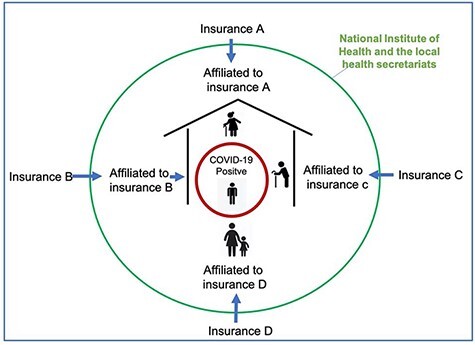
Household social security affiliation diagram
Materials and methods
This paper is derived from a qualitative study of the coordination of responses to COVID-19 within the Colombian health system (Turner and Niño, 2020). We undertook case studies (Yin, 2013), using a combination of descriptive and theory-driven approaches, to understand how stakeholders involved in the planning and delivery of health responded to the pandemic in Colombia and perceived inter-organizational collaboration in such responses (e.g. coordination of surveillance across localities). The Consolidated Criteria for Reporting Qualitative Studies checklist was used for reporting study design, data collection and analysis, and findings (O’brien et al., 2014).
Participants
The findings are based on a dataset of 81 semi-structured interviews conducted between June and November 2020. In total, 114 potential participants were approached for an interview; the participation rate was 71%. No participants withdrew from the study once they had participated in an interview. Diverse health system stakeholders at the national level and in the three cities were included (Table 2). We included interviews with stakeholders that worked at national governmental bodies directly involved in the planning of COVID-19 response (n = 9). In each city, we interviewed representatives of the local government involved in health planning and delivery (n = 22), representatives of health insurance companies (n = 13) and representatives of hospitals and clinical laboratories (n = 37).
Table 2.
Characteristics of interviewees
| Organization | Structure of the health system | Type of organization | N |
|---|---|---|---|
| National government | National level—planning | Public | 9 |
| Cartagena | |||
| Local government | Local level—planning | Public | 9 |
| Health insurances, prepaid companies | Insurance | Public and private | 6 |
| Hospitals | Service delivery | Private | 5 |
| Hospitals | Public | 2 | |
| Laboratories | Public and private | 2 | |
| Cali | |||
| Local government | Local level—planning | Public | 5 |
| Insurance companies, prepaid companies | Insurance | Public and private | 2 |
| Hospitals | Service delivery | Private | 10 |
| Hospitals | Public | 2 | |
| Laboratories | Public and private | 2 | |
| Bogotá | |||
| Local government | Local level—planning | Public | 8 |
| Insurance companies, prepaid companies | Insurance | Public and private | 5 |
| Hospitals | Service delivery | Private | 8 |
| Hospitals | Public | 4 | |
| Laboratories | Public and private | 2 | |
| Total | 81 | ||
Data collection
The study participants were recruited using purposive (Palinkas et al., 2015) and snowball sampling (Lewis-Beck et al., 2004). To inform purposive sampling, we mapped key organizations and stakeholders involved in the response to the emergency at the national level and the three cities. All participants contacted had senior positions and were able to provide an overview of their organization’s experiences of COVID-19. The stakeholders approached were highly involved in decision-making on COVID-19, especially during the period of data collection (the first 6 months of the emergency in Colombia). Interviewees were asked if they were able to provide contact details for other relevant stakeholders and/or if they could leave us in touch with them. Using snowball sampling (Lewis-Beck et al., 2004) facilitated participants’ willingness to be interviewed. Having mapped relevant stakeholders at the outset of the study helped us to balance potential sampling bias derived from snowball sampling.
Given that data collection took place during the Colombian ‘lockdown’, all the interviews were conducted virtually using online platforms: Microsoft Teams (n = 78), Zoom (n = 2), and Google Meet (n = 1). Microsoft Teams is the platform the university uses the most for online meetings and the one we considered the safest in terms of privacy: (1) it notifies all participants when recording and (2) recordings are only available to the people on the call or people invited to the meeting. Institutional emails were used to create the links for the interviews so participants were protected by the University privacy policy. In the cases of Zoom and Google Meet, the participant chose the platform of their preference; participants considered it was easier for them to connect to the meeting if they used a platform they already knew.
Ethics approval for this research was received from the research ethics committee at the University of los Andes (1166–2020). All participants provided informed consent before being interviewed and agreed to be recorded. Audio files were saved using a unique code; all transcriptions were anonymized by replacing participants’ names with codes. A topic guide informed the interviews (supplement a); however, the questions were adapted to each interviewee’s context (Patton, 1990).
Analysis
The data were analysed thematically using inductive and deductive approaches (Bradley et al., 2007). All the interviews were transcribed verbatim and coded using New NVivo software. Deductively, the research team coded the interviews following 10 main codes and 22 sub-codes that were derived from the study objective and its theoretical framework. Inductively, emerging categories were identified that could help us understand COVID-19 surveillance and inter-organizational coordination in the particular context of the Colombian health system (Table 3).
Table 3.
List of codes, sub-codes and emerging categories
| Key code | Sub-codes | Emerging codes relevant to understand inter-organizational coordination |
|---|---|---|
| Organization response | Decision-making processes | |
| Organization priorities | ||
| Enablers (financial legal, social relations, information access and use) | ||
| Pre-existing conditions | ||
| Barriers (financial legal, social relations, information access and use) | ||
| Challenges | ||
| Infrastructure/installed capacity | ||
| Human resources | ||
| Forms of innovation (processes, productions, relationships, services) | ||
| Indirect impact in other services | ||
| Coordination and cooperation | National and local government relationship | |
| Inter-organization involvement | Legal frameworks (Convenio tripartita) | |
| Responsibility distribution | ||
| Public and private relationships | Resource allocation | |
| Pre-existing conditions | ||
| Leadership | ||
| Intersectoral involvement | ||
| Mayor system change theory | Feedback loops | |
| Health system stakeholder engagement | Communication | |
| Implementing change | ||
| Learning from history | ||
| Levers | Hard levers | |
| Soft levers | ||
| Health system characteristics | Fragmentation | |
| Segmentation | ||
| Trust | ||
| Surveillance system operation | ||
| Service planning and implementation | ||
| Information systems | ||
| Corruption | ||
| Expertise narratives | - - - | |
| Social determinants of health | ||
| Technology use and appropriation | ||
| Evidence production and use |
Results
The results are organized into two themes. First, we examine perceived structural barriers to the implementation of coordinated work between health secretaries, insurance companies and health providers. Second, we explain how the pandemic came to represent among participants a stimulus for actors to work together, leading to the development of strategies that relied on inter-organizational coordination to perform COVID-19 surveillance.
Structural barriers to inter-organizational coordination
Inter-organizational coordination between the health secretaries, insurance companies and health providers to implement surveillance measures was described by participants as novel: there was a lack of previous collaborative relationships through which these actors shared responsibilities, financial resources and human resources. Structural barriers were identified that had impeded such coordination within the health system historically.
Fragmentation among healthcare actors
A perceived structural barrier to coordination was fragmentation among different healthcare actors, both nationally and locally. At the national level, a stakeholder pointed out that negotiating and reaching agreements between the key actors of the health system was often challenging as a result of health system fragmentation. Fragmentation was apparent in the co-existence of different insurance schemes and different health providers that could belong to the public or the private sector. Reaching an agreement between insurance companies and local health secretariats was described by one national level participant as a necessity to cope with fragmentation:
We also have to take into account that this situation, that is, that the health system is segmented and fragmented (…) there are rules for the subsidized, the contributive, the military forces, the magisterium. In addition, we deal with the fragmentation of responsibilities, this is something that had an impact in the negotiations (Ministry of Health representative, SH-A-023).
Under the national model of ‘managed competition’, health insurers and providers viewed one another as ‘competitors’ that were not obliged to work together:
The [insurance companies] view each other with suspicion, because they are enemies from a commercial point of view; it is a perfectly normal situation in a market that is tight; the same thing happened with hospitals (Secretary of Health representative, Bogotá, SH-B-025).
Volume and diversity of provider organizations
The volume and diversity of insurance companies and health providers inhibited their coordination across each city. Providers were diverse in terms of the scale of their infrastructure and their administrative systems, processes and information management. An interviewee from Cali described the difficulties of coordinating 17 insurance companies operating in the city, stressing the need for a leader that could help these organizations to reach shared agreements:
I do believe that there is a need for a health insurances’ coordinator at the local or national level, one who heads those organizations and puts them into a regime because the agreement has worked but it is exhausting, that is, there are 17 [insurers], and as I said, they do not have the same performance (Secretariat of Health representative, Cali, SH-C-008).
Arm’s length relationships among organizations
Arm’s length relationships between planners and providers of care contributed to distrust between the health secretaries, insurance companies and health providers. The planning secretariats would often play the role of auditing providers’ services including the conditions of their infrastructure, with the consequence that the relationship between planners and providers was confined to narrow bureaucratic and administrative procedures, with the threat of sanctions:
The Secretariat is often calling us to close our doors, to assess if we are accomplishing the secretariat guidelines and permits needed to keep the services open. Never to say, ‘hey let’s have a conversation’ (Secretariat of Health representative, Bogotá, SH-B-003).
History of unfulfilled contractual arrangements
Unfulfilled contractual agreements for the delivery of health services also contributed to mistrust between actors. In Cartagena, for example, hospitals feared that costs associated with the treatment of COVID-19 patients would not be reimbursed due to economic debts that had not been paid by local authorities historically, undermining their willingness to take on new responsibilities:
It is necessary that they regain out trust, not respect because they will always have respect for representing the State, but trust. And to regain trust, they have to put an end to that indifferent behavior regarding their financial obligations that they acquire with us (Hospital director, Cartagena, SH-D-002).
Poorly defined organizational roles and relationships
Organizational roles in response to COVID-19 were poorly defined, initially, due to a lack of communication among the diversity of actors within the health system. This contributed to uncertainty and tensions over which organizations should carry out and finance particular public health functions such as ‘testing and tracing’ during the early stage of the pandemic, as this example from Cali shows:
Initially, the national government designated that the health secretariats were going to be in charge of testing, and that it was going to be for free. This was April or May [2020]. Suddenly, the government said it was the [insurance companies’] responsibility. There was not a clear decision from the beginning. It was not clear if it was a public health entity the responsible and all the resources had to come from [a fund for emergency mitigation] – all the resources were coming from the government - or is it was funded by capitation and services delivered like any other disease (Hospital Director, Cali, SH-C-007).
In summary, coordination and cooperation among health providers was not a usual practice in Colombia prior to COVID-19’s arrival. The interviewees stated that the relationships between insurers, service providers, both public and private, and local authorities were minimal and restricted to specific activities. They described multiple structural barriers for coordination within the health system. However, the pandemic was seen as a trigger for addressing some of the structural barriers to coordination just described.
Mechanisms of inter-organizational coordination to improve COVID-19 surveillance
The coordination of actors to undertake COVID-19 surveillance (as shown in Table 4) was underpinned by hard and soft coordination mechanisms.
Table 4.
Public health surveillance responsibilities in the Colombian healthcare system
| Activities | Responsible |
|---|---|
| Public health surveillance | National Health Institute (INS), Departments and municipalities (local health secretaries) |
| Sample testing | Public and private health providers (private clinical laboratories and health secretaries) |
| Payers (who pay for the service) | Health insurance companies (EPS), prepaid insurance companies, for patients with no payment capacity: public health services |
| Enforcement of health regulations and insurance contracts | Ministry of Health |
Hard mechanism: formal agreements clarified roles, responsibilities and resource use
In order to implement a timely surveillance strategy for COVID-19, the three cities studied developed formal agreements between the health secretaries, the insurance companies and health providers, including laboratories, for COVID-19 testing. In the case of Bogotá and Cali, the strategy was called ‘Convenio Tripartita’ (‘Tripartite Agreement’), while Cartagena introduced a similar strategy called ‘Cuidemonos Cartagena’. The formal inter-organizational agreements defined their respective functions as well as shared responsibilities and financial resources for responding to COVID-19:
We made the decision to privilege the home care of patients, not only as a logical way to care for these people, but as a way to prevent patients from reaching the emergency services en masse and congesting them. However, to do that home care, we had to make a common pool of resources with the insurers. This is a massive change for us (Health Secretariat representative, Bogotá, SH-B-025).
The inter-organizational agreements had three purposes. First, to enable diagnostic testing of all members of a family or community, irrespective of their insurance affiliation. Some interviewees stated that coordination approaches to testing were needed because a single organization did not have the resources or the capacity to carry out these activities. The insurance companies were able to test their clients, but they could not guarantee that other suspected cases in the same cluster covered by other insurance companies could be tested, meaning they could not perform contact tracing or control the local risk of exposure.
Second, the agreements improved the collection and sharing of data for facilitating early diagnosis, performing active case identification, contact tracing and monitoring, and centralized data management and surveillance. Data management for public health surveillance, traditionally implemented by the health secretariats and national health institute, was widened to include other actors, including health providers and insurance companies. In Cali, a ‘passive’ approach to epidemiological surveillance was adopted historically. The pandemic, in stimulating shared data management between the secretariat and the health providers, enabled an ‘active’ approach to the search for cases in specific households and neighbourhoods.
The epidemiological surveillance group as it was historically used routine surveillance. I would say that a passive surveillance where reports were made from the institutions, but not an active surveillance that is the search, which is behind the cases and identify cluster and test suspected cases (Insurance company representative, National level, SH-C-008).
Third, the agreements supported coordinated surveillance and educational work with local communities. In Cartagena, for example, a programme called Heroic Neighborhood (‘Barrio Heroico’, in Spanish) fostered the surveillance at the community level under the guidance of the District’s Health Secretariat and an alliance of insurance companies. The programme’s features included an educational programme to promote health literacy, compliance with isolation measures, mask use, social distancing and COVID-19 surveillance measures within Cartagena’s local communities (Alcaldía Distrital De Cartagena, 2020).
Hard mechanism: declaration of national state of emergency
Actors’ willingness to enter such agreements was supported by the declaration of the state of emergency nationally (República de Colombia, 2020a). The state of emergency decree established the regulations that allowed health organizations to act more flexibly and to transform rapidly their service offerings, mobilize resources and contract with the state to respond to the emergency. The national declaration allowed the actors to negotiate their interests, align existing service delivery activities and involve each organization’s internal legal and administrative procedures to plan and implement the initiatives. Even though participants described the early stage of planning and implementation as both challenging and time consuming, they agreed that once they had settled on a ‘common purpose’ and financing of the agreement, this allowed the different actors to move forward collectively with improving COVID-19 surveillance:
We endorsed the agreement, and we invested a significant amount of money on it. The District also added resources of their own. Then we had to face some challenges such as making everyone agree, setting an agreement with the District, making the lawyers [of the different organizations] reaching an agreement, setting a common purpose for all the insurance companies (which are the competition), finding the IPS [health providers] providing the services as part of the agreement, and consolidate a system of information. We had several challenges, but slowly we moved forward (Insurance Company representative, National level, SH-A-007)
Soft mechanism: inter-organizational communication and interaction
With regard to softer mechanisms of change, COVID-19 triggered communication and interaction among insurance companies and other stakeholders enabling information exchange and resource sharing that supported the development of the strategies in the three cities studied.
I believe that when there is a common purpose and everyone is aware that it is a win-win, we agreed on the fundamentals, which was to think about people, in our city, it is the common purpose, that sense of belonging and that trust, is what allowed us to move forward (Health Insurance representative, National Level, SH-D −006)
Soft mechanism: growing confidence and trust in inter-organizational collaboration
Improved coordination between the different actors was facilitated by growing confidence and trust achieved through joint work as each organization realized that trading ‘blame’ for collaboration would aid the achievement of their mutual objectives.
I think that the key was, in the first place, understanding that it was a problem that affected everyone and that we all lost if we continued to blame ourselves. That was first and understanding that it was better to work together than to remain disjointed, blaming each other. Understand that protecting the community was most important. Save the lives of people who could be affected by the pandemic and that later when the pandemic passed, we could discuss the differences. That was a pact that we made between all of us, let’s put politics and the discussions about money aside, and we are going to concentrate on seeing how we all adjust and comply. And so, we began to work (Policymaker, Cartagena, SH-D-012)
Soft mechanism: sense of shared responsibility for delivering coordinated surveillance
The agreements also created a fertile ground to plan and deliver coordinated surveillance activities. These initiatives facilitated the understanding of the COVID-19 response as a shared responsibility that exceeded the duty of each organization, allowing a collective approach to delivering services, rather than segmenting care by the patient’s insurance affiliation.
For the first time, we were able to coordinate different actors. This is the first time, that insurers and a regulatory body such as the secretariat of health, worked together to provide a response to a public health issue. This has been a coordinated response that has been based on the territory (Secretariat of Health representative, Bogotá, SH-B-002)
Discussion
This study identified structural and motivational barriers to inter-organizational coordination in the Colombian health system historically and indicated how COVID-19 triggered soft and hard mechanisms for working around these pre-existing barriers to support COVID-19 surveillance during the first year of the pandemic. Two propositions concerning critical factors that influence the coordination between institutions were introduced. The first proposition, concerning structural impediments to coordination, was supported by the qualitative data. Pre-existing structural barriers to coordination with the Colombian health system reported by the interviewees included the following: the fragmentation and segmentation of the health system, the major differences among multiple participant organizations, competition for market share among insurance companies, poorly defined roles, unfulfilled contractual agreements and fragmented information systems.
The second proposition, concerning the importance of motivational or ‘soft’ factors for supporting coordination, was found to be necessary but insufficient for enabling shared institutional surveillance of COVID-19. The magnitude of the pandemic, which threatened to overwhelm the capacity of Colombia’s public health surveillance system, became an incentive for cooperation. The growing appreciation of joint work was born from recognition that each organization was facing great challenges to fulfil their roles individually and that only by joining efforts it was possible to provide a response to the emergency. While the severity of the pandemic created ‘soft’ pressure for increased coordination, a ‘hard’ coordination mechanism—the formal institutional agreements—was needed to facilitate concrete practices of coordination.
This leads to a new proposition concerning coordination arrangements among institutions: ‘improving coordination between institutions relies on interplay among hard and soft coordination mechanisms’. As a hard mechanism of coordination, the formal agreements influenced practices of coordination in several ways. First, the agreements provided authority to negotiate new local arrangements among institutions. Negotiation of the local agreements was supported by a state of emergency declaration by national government (e.g. República de Colombia, 2020b), which allowed for flexibility over organizational roles and functions, allowing local authorities to adapt and identify local solutions and mobilized financial resources. With new-found legitimacy bestowed by the national declaration, local authorities were able to participate as mediators to legalize the agreements between insurance companies and health providers.
Second, the agreements formalized specific products of coordination. Organizations were able to share information about positive cases that needed tracing or information about patients who were at higher risk and financial and human resources so they could implement the testing and tracing of cases beyond the insurance affiliation of the patient. The inter-organizational agreements, involving health secretaries, insurance companies and health providers in the three Colombian cities we studied, supported diagnostic testing in people’s homes, the rapid sharing of surveillance data and community outreach work, all of which crossed traditional organizational boundaries within the health system.
Third, inter-organizational trust was improved as a by-product of the processes of collaboration instituted. Through the practice of forming and working in accordance with the formal agreements, insurance companies were able to work as allies instead of seeing each other merely as competitors. The initial pressure for, and subsequent process of collaboration, helped to address distrusting relationships among actors who had thwarted cooperative relationships historically within the Colombian health system.
Contributions to the research literature
This study contributes to two areas of research: structural influences on health system coordination and mechanisms for facilitating inter-organizational coordination. First, the international literature has identified structural barriers to inter-organizational coordination, including service fragmentation and competitive incentives associated with market-based public health systems like Colombia (Vargas et al., 2016). The absence of clear coordination mechanisms has been found to result in delayed response activities like testing and contact tracing in the context of the COVID-19 emergency (Tromberg et al., 2020). Our study contributes to this literature in highlighting how a wider range of structural barriers associated with market-based healthcare systems (poorly defined roles and relationships concerning coordination, unfulfilled contractual agreements, and fragmented information systems) affected early responses to COVID-19 in Colombia. Moreover, the findings indicate how structural barriers to coordination have knock-on effects on motivational barriers to coordination like distrusting relationships that stem from market-based behaviour. The findings contribute to this literature by indicating the need to address a wider range of structural barriers to coordination to influence, in turn, health system actors’ motivation to engage in coordination arrangements.
Second, this study contributes to debate on encouraging inter-organizational cooperation, which has taken on increased importance in the context of COVID-19. It is recognized that soft incentives are needed to promote cooperation among actors and organizations such as institutional support and motivating professionals’ participation, especially in market-based systems like Colombia (Vargas et al., 2020). Our study similarly supports the need for soft mechanisms of coordination to address mutual distrust that may have developed as a by-product of systemic barriers. However, our findings suggest that soft mechanisms will have little impact on inter-organizational trust in the absence of harder mechanisms for promoting coordination. In the case of COVID-19, formal inter-organizational agreements covering shared roles and responsibilities, data management and financial resources were instrumental in facilitating joined up approaches to the surveillance of COVID-19. Together with the ‘permission’ for innovation represented by COVID-19 (Swaithes et al., 2020), the process of negotiating formal inter-organizational agreements between organizations appeared to improve the quality of interpersonal relationships locally. While recognizing the importance of interpersonal relationships for supporting coordination (Dickinson, 2010), the study deviates from the previous literature on health system coordination that emphasizes ‘soft’ mechanisms exercised at the interpersonal level (e.g. political skill, trust-building exercises, stakeholder involvement) to improve coordination between organizations. Instead, the findings indicate the need to develop ‘hard’ incentives to support collaboration as these were found to influence ‘soft’ outcomes too (i.e. formal agreements or contractual mechanisms for coordination that formalize inter-organizational roles, resources, and relationships). The emphasis on ‘hard’ mechanisms to support coordination complements previous work on major system change that includes a role for designated or top-down coordination in aligning multiple stakeholder interests (Turner et al., 2016a) and work in economics that places emphasis on formal and implicit contracts in shaping inter-organizational behaviour (Williamson, 1991).
Policy and practice implications
The findings indicated, in this case, that ‘hard’ intervention mechanisms supported improvement in the coordination relationships among institutions. While Government actions can be considered as both barriers and enablers to coordination depending on the circumstances (Casey, 2008), in the three cities we studied, interviewees recognized that formalization of relationships, achieved through ‘top-down’ coordination by State actors at the national and local level, were facilitating factors for improving coordination. Hard mechanisms such as formal agreements or contracts and regulatory change originated at the national level, providing the formal authority needed to improve collaboration among a variety of health system stakeholders both nationally and locally. The regulatory changes introduced by the national and local authorities enabled the development of collaborations initiatives among stakeholders from both the public and private sector. In market-based health systems in particular, policymakers need to consider the need for ‘top-down’ intervention, expressed through contracting or regulatory mechanisms, where increased collaboration among institutions is required in response to immediate crises or longer-term system-wide challenges. While environmental disturbances like pandemics may trigger a disposure towards collaboration to address a crisis, formal intervention may well be needed to accomplish changes in relationships among organizations by aligning the multiple stakeholders involved.
The study showed that, to plan new strategies for surveillance based on coordinated work, understanding the influence of, and interplay between, soft and hard mechanisms on inter-organizational coordination in specific contexts is critical. Such an understanding should be informed by qualitative studies that inquire into the sociocultural aspects that shape public health measures to mitigate pandemics (Bavel et al., 2020; Teti et al., 2020; Vindrola-Padros et al., 2020). This study showed that the planning and implementation of surveillance strategies are deeply intertwined with local perceptions about what inter-organizational coordinated work means for different actors and the history of organizational relationships within local health systems In the case of the Colombian health system, we found that formalizing the agreements facilitated sharing information, legal procedures and mobilizing financial resources. However, these processes also required the acknowledgement of a new form of leadership locally (held by the health secretariats) and willingness to engage in inter-organizational relationships concerning COVID-19 surveillance, which were fuelled by initial pressure to act, while trust then developed through the process of collaborative work. Before introducing major changes in the structure of health systems, public health planners should understand how mechanisms of change work at the local level to include incentives that can be properly adapted to the specific contexts of each city or region within the same country.
Limitations
We were unable to conduct face-to-face interviews given the quarantine restrictions taking place in Colombia during the study, although online interviews had a good participation rate (71%) and acquired a range of actors’ perspectives. Triangulating the actors’ reported experiences with observations of everyday interactions relevant for coordinated work (e.g. planning meetings) would be a valuable component of follow-up research that assesses barriers and facilitators to the sustaining of coordination arrangements post-COVID. Finally, the three cities have different local contexts, both socio-economic characteristics and health system arrangements, limiting cross-case comparability and generalizability of the findings to other settings. Moreover, while a range of factors influencing the implementation of coordination arrangements between organizations have been identified, it is not possible to isolate the relative role of softer and harder mechanisms (e.g. the effect of an institutional agreement relative to increased purposeful communications stimulated by the threat to health posed by COVID-19). The results obtained could inform questionnaire items used in further cross-sectional survey research.
Supplementary Material
Acknowledgements
The authors are grateful to all the participants of the study who shared with us their experiences regarding the COVID-19 response in Colombia.
Contributor Information
Simon Turner, School of Management, University of los Andes, Edificio SD, Cl. 21 #1–20, Bogotá, Colombia.
Carolina Segura, School of Management, University of los Andes, Edificio SD, Cl. 21 #1–20, Bogotá, Colombia.
Natalia Niño, School of Medicine, University of los Andes, Carrera 1 No 18 A - 10, Bloque Q Piso 8, Bogotá, Colombia.
Supplementary data
Supplementary data are available at Health Policy and Planning online.
Data availability
The data underlying this article are available in the article and in its online supplementary material.
Funding
This research was funded by the Colombian Ministry of Science, Technology and Innovation through the call ‘Mincienciatón’ (1204101577001).
Author contribution
All authors contributed to conception and design of the work, data collection, data analysis and interpretation, drafting the article and critical revision of the article. All authors gave final approval of the version submitted.
Ethical approval.
The project was approved by the research ethics committee at the University of los Andes (1166–2020). The research was classified as minimal risk.
Conflict of interest statement.
The authors declare no competing interests.
References
- Alcaldía Distrital De Cartagena . 2020. Barrio Heroico hizo intervención en Tierrabomba para prevenir la Covid-19. https://www.cartagena.gov.co/plan-de-desarrollo-2016-2019-primero-la-gente/informe-tecnico-del-plan-de-desarrollo-2016-2019-a-marzo-2018/93-acciones-comunicacionales/1498-barrio-heroico-hizo-intervencion-en-tierrabomba-para-prevenir-la-covid-19, accessed 1 March 2021.
- Alvarez-Rosete A, Hawkins B. 2018. Advocacy coalitions, contestation, and policy stasis: the 20 year reform process of the Colombian Health System. Latin American Policy 9: 27–54. [Google Scholar]
- Amaya-Lara JL. 2016. Catastrophic expenditure due to out-of-pocket health payments and its determinants in Colombian households. International Journal for Equity in Health 15: 182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atun R, Monteiro de Andrade LO, Almeida G et al. 2015. Health-system reform and universal health coverage in Latin America. The Lancet 385: 1230–47. [DOI] [PubMed] [Google Scholar]
- Aunger JA, Millar R, Greenhalgh J et al. 2021. Why do some inter-organisational collaborations in healthcare work when others do not? A realist review. Systematic review 10: 82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auschra C. 2018. Barriers to the integration of care in inter-organisational settings: a literature review. International Journal of Integrated Care 18: 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bavel J, Baicker K, Boggio P et al. 2020. Using social and behavioural science to support COVID-19 pandemic response. Nature Human Behaviour 4: 460–71. [DOI] [PubMed] [Google Scholar]
- Best A, Greenhalgh T, Lewis S et al. 2012. Large-system transformation in health care: a realist review. Milbank Quarterly 90: 421–56.doi: 10.1111/j.1468-0009.2012.00670.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boin A, Van Eeten MJ. 2013. The resilient organization. Public Management Review 15: 429–45. [Google Scholar]
- Bradley E, Curry L, Devers K. 2007. Qualitative data analysis for health services research: developing taxonomy, themes, and theory. Health Services Research 42: 1758–72.doi: 10.1111/j.1475-6773.2006.00684.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cameron A, Lart R, Bostock L et al. 2014. Factors that promote and hinder joint and integrated working between health and social care services: a review of research literature. Health & Social Care in the Community 22: 225–33. [DOI] [PubMed] [Google Scholar]
- Casey M. 2008. Partnership-success factors of interorganizational relationships. Journal of Nursing Management 16: 72–83. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . 1988. Guidelines for evaluating surveillance systems. MMWR Supplements 37: 1–18. [PubMed] [Google Scholar]
- Clarke JM, Waring J, Bishop S et al. 2021. The contribution of political skill to the implementation of health services change: a systematic review and narrative synthesis. BMC Health Services Research 21: 260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalglish S. 2020. COVID-19 gives the lie to global health expertise. Lancet 395: 1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Declich S, Carter AO. 1994. Public health surveillance: historical origins, methods and evaluation. Bulletin of the World Health Organization 72: 285–304. [PMC free article] [PubMed] [Google Scholar]
- Dickinson H. 2010. ‘Why partnership working doesn’t work’: pitfalls, problems and possibilities in English health and social care. Public Management Review 12: 811–28. [Google Scholar]
- Escobar ML, Giedion U, Giuffrida A et al. 2009. Colombia: after a decade of health system reform. In: Glassman AL, Escobar ML, Giuffrida A, Giedion U (eds). From Few to Many Ten Years of Health Insurance Expansion in Colombia, Inter-American Development Bank, pp. 1–13. https://publications.iadb.org/publications/english/document/From-Few-to-Many-Ten-Years-of-Health-Insurance-Expansion-in-Colombia.pdf#page=11, accessed 15 December 2021.
- Garcia-Ramirez J, Nikoloski Z, Mossialos E. 2020. Inequality in healthcare use among older people in Colombia. International Journal for Equity in Health 19: 168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia-Subirats I, Vargas I, Mogollón-Pérez AS et al. 2014. Barriers in access to healthcare in countries with different health systems. A cross-sectional study in municipalities of central Colombia and north-eastern Brazil. Social Science and Medicine 106: 204–13. [DOI] [PubMed] [Google Scholar]
- Giovanella L, Vega R, Tejerina-Silv H et al. 2020. Es la atención primaria de salud integral parte de la respuesta a la pandemia de Covid-19 en Latinoamérica? Trabalho, Educação e Saúde 19: e00310142. [Google Scholar]
- Guerrero R, Gallego AI, Becerril-Montekio V et al. 2011. The health system of Colombia. Salud pública méxico 53: s144–55. [PubMed] [Google Scholar]
- Hernández M. 2002. Reforma sanitaria, equidad y derecho a la salud en Colombia. Cadernos de Saúde Pública 18: 991–1001. [DOI] [PubMed] [Google Scholar]
- Homedes N, Ugalde A. 2005. Why neoliberal health reforms have failed in Latin America. Health policy 71: 83–96. [DOI] [PubMed] [Google Scholar]
- Huxham C. 2003. Theorizing collaboration practice. Public Management Review 5: 401–23. [Google Scholar]
- Ibrahim N. 2020. Epidemiologic surveillance for controlling Covid-19 pandemic: types, challenges and implications. Infect Public Health 13: 1630–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaime S. 2016. Participación social en sistemas de salud fragmentados: ¿una relación virtuosa? Revista Gerencia y Políticas de Salud 15: 38–56. [Google Scholar]
- Legido-Quigley H, Asgari N, Teo Y et al. 2020. Are high-performing health systems resilient against the COVID-19 epidemic? The Lancet 395: 848–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis-Beck M, Bryman A, Futing Liao T. 2004. The SAGE Encyclopedia of Social Science Research Methods. Thousand Oaks: Sage Publications. [Google Scholar]
- Ministerio de Salud y Protección Social . 2020. Plan de contingencia para responder ante la emergencia por COVID-19. https://www.minsalud.gov.co/salud/publica/PET/Documents/ABRIL%20PLAN%20DE%20CONTINGENCIA%20PARA%20RESPONDER%20ANTE%20LA%20EMERGENCIA%20POR%20COVID-19%20%281%29.pdf, accessed 20 December 2020.
- O’brien B, Harris I, Beckman T et al. 2014. Standards for reporting qualitative research: a synthesis of recommendations. Academic Medicine: Journal of the Association of American Medical Colleges 89: 1245–51. [DOI] [PubMed] [Google Scholar]
- Palinkas LA, Horwitz SM, Green CA et al. 2015. Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Administration and Policy in Mental Health 42: 533–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton M. 1990. Qualitative Evaluation and Research Methods. California: Sage Publications. [Google Scholar]
- Portafolio . 2020. Suma y articulación de esfuerzos en favor de la salud. 27 September. https://www.portafolio.co/mas-contenido/suma-y-articulacion-de-esfuerzos-en-favor-de-la-salud-545039, accessed 15 December 2021.
- Randazzo W, Cuevas-Ferrando E, Sanjuán R et al. 2020. Metropolitan wastewater analysis for COVID-19 epidemiological surveillance. International Journal of Hygiene and Environmental Health 230: 113621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- República de Colombia . 2020a. Decreto 417 de 17 Marzo 2020 Por el cual se declara un Estado de Emergencia Económica, Social y Ecolófica en todo el territorio nacional. https://www.funcionpublica.gov.co/eva/gestornormativo/norma.php?i=110334, accessed 11 November 2020.
- República de Colombia . 2020b. Resolución 385 del 12 de Marzo de 2020 Por la cual se declara la emergencia sanitaria por causa del coronavirus COVID-19 y se adoptan medidas para hacer frente al virus. https://www.minsalud.gov.co/Normatividad_Nuevo/Resolución%20No.%200385%20de%202020.pdf, accessed 01 December 2020.
- Rummery K. 2009. Healthy partnerships, healthy citizens? An international review of partnerships in health and social care and patient/user outcomes. Social Science and Medicine 69: 1797–804. [DOI] [PubMed] [Google Scholar]
- Shigayeva A, Atun R, Mckee M et al. 2010. Health systems, communicable diseases and integration. Health Policy and Planning 25: i4–20. [DOI] [PubMed] [Google Scholar]
- Srinivasan M, Asch S, Vilendrer S et al. 2020. Qualitative assessment of rapid system transformation to primary care video visits at an academic medical center. Annals of Internal Medicine 173: 527–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swaithes L, Dziedzic K, Sharp CA et al. 2020. Context, context, context: how has covid-19 changed implementation globally and how can we ‘lock in’ learning? Rheumatology 59: 1804–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teti M, Schatz E, Liebenberg L. 2020. Methods in the time of COVID-19: the vital role of qualitative inquiries. International Journal of Qualitative Methods 19: 1609406920920962. [Google Scholar]
- Tromberg B, Schwetz T, Pérez-Stable E et al. 2020. Rapid scaling up of Covid-19 diagnostic testing in the United States - the NIH RADx initiative. The New England Journal of Medicine 383: 1071–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner S, Botero-Tovar N, Herrera MA et al. 2021. Systematic review of experiences and perceptions of key actors and organisations at multiple levels within health systems internationally in responding to COVID-19. Implementation Science 16: 50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner S, Goulding L, Denis J et al. 2016b. Major system change: a management and organisational research perspective. In challenges, solutions and future directions in the evaluation of service innovations in health care and public health. Health Services and Delivery Research.NIHR Journals Library 4: 85–104. [PubMed] [Google Scholar]
- Turner S, Niño N. 2020. Qualitative analysis of the coordination of major system change within the Colombian health system in response to COVID-19: study protocol. Implementation Science Communications 1: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner S, Ramsay A, Perry C et al. 2016a. Lessons for major system change: centralization of stroke services in two metropolitan areas of England. Journal of Health Services Research & Policy 21: 156–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vangen S, Huxham C. 2003. Nurturing collaborative relations: building trust in interorganizational collaboration. The Journal of Applied Behavioral Science 39: 5–31. [Google Scholar]
- Vargas Bustamante A, Méndez CA. 2014. Health care privatization in Latin America: comparing divergent privatization approaches in Chile, Colombia, and Mexico. Journal of Health Politics, Policy and Law 39: 841–86. [DOI] [PubMed] [Google Scholar]
- Vargas I, Garcia-Subirats I, Mogollón-Pérez AS et al. 2018. Understanding communication breakdown in the outpatient referral process in Latin America: a cross-sectional study on the use of clinical correspondence in public healthcare networks of six countries. Health Policy and Planning 33: 494–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vargas I, Mogollón-Pérez A, De Paepe P et al. 2016. Barriers to healthcare coordination in market-based and decentralized public health systems: a qualitative study in healthcare networks of Colombia and Brazil. Health Policy and Planning 36: 736–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vargas I, Mogollón-Pérez AS, De Paepe P et al. 2015. Do existing mechanisms contribute to improvements in care coordination across levels of care in health services networks? Opinions of the health personnel in Colombia and Brazil. BMC Health Services Research 15: 213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vargas I, Eguiguren P, Mogollón-Pérez AS et al. 2020. Understanding the factors influencing the implementation of participatory interventions to improve care coordination: An analytical framework based on an evaluation in Latin America. Health Policy and Planning 35: 962–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vázquez ML, Vargas I, Unger JP et al. 2015. Effectiveness of care integration strategies in health systems of Latin America: EQUITY-LA II study: ingrid Vargas Lorenzo. European Journal of Public Health 25: ckv176.253. [Google Scholar]
- Vindrola-Padros C, Chisnall G, Cooper S et al. 2020. Carrying out rapid qualitative research during a pandemic: emerging lessons from COVID-19. Qualitative Health Research 30: 1049–7323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wensing M, Sales A, Armstrong R et al. 2020. Implementation science in times of Covid-19. Implementation Science 15: 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wildridge V, Childs S, Cawthra L et al. 2004. How to create successful partnerships-a review of the literature. Health Information and Libraries Journal 21: 3–19. [DOI] [PubMed] [Google Scholar]
- Williamson O. 1991. Comparative economic organization: the analysis of discrete structural alternatives. Administrative Science Quarterly 36: 269–96. [Google Scholar]
- World Health Organization . 2020. Public health surveillance for COVID-19. Interim Guidance. https://apps.who.int/iris/handle/10665/333752, accessed 13 January 2021.
- Yin R. 2013. Validity and generalization in future case study evaluations. Evaluation 19: 321–32. [Google Scholar]
- Zuckerman H, Kaluzny A, Ricketts T et al. 1995. Alliances in health care: what we know, what we think we know, and what we should know. Health Care Management Review 20: 54–64. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article are available in the article and in its online supplementary material.


