Abstract
Objectives
This study systematically evaluates age and race differences in mental health symptoms as they unfold microlongitudinally during the coronavirus disease 2019 (COVID-19) pandemic with a focus on within-person reactivity to forecasting and experiencing COVID-19 stress.
Method
A daily diary approach was used to examine predictors of daily anxiety and depressive symptoms among 526 adults (White [54%] and Black American [46%]) aged 21–79. A total of 3,605 online diaries were collected for 21 consecutive days between October and November, 2020. In addition to mental health symptoms, participants reported forecasted (next 24 h) stress as well as experienced (past 24 h) stress related to COVID-19.
Results
Patterns of reactivity to forecasted and experienced COVID-19 stress depended on age and race. White older adults displayed greater reactivity to COVID-19-related stress than White younger adults, but the effects of COVID-19-related stress were consistently detrimental for the daily anxiety of Black Americans, regardless of age. For Black Americans, age was less negatively associated with depressive symptoms than for White Americans. Increases in experienced COVID-19 stress were also more strongly associated with increases in depressive symptoms for Black Americans relative to White participants.
Discussion
This study moves beyond cross-sectional, descriptive work within the context of the COVID-19 pandemic and emphasizes the dynamic nature of within-person reactivity patterns that differ by age and race. Although White older adults experienced an increase in daily anxiety when forecasting COVID-19 stress, the co-occurring pandemic of systemic racism may be more powerful than age-related vulnerabilities for Black adults.
Keywords: Anxiety, COVID-19, Depressive symptoms, Reactivity, Stress
Coronavirus disease 2019 (COVID-19) has had a significant negative impact on the health and well-being of the U.S. population. Systemic and daily changes to individuals’ lives have notably impacted the mental health of the population, particularly increasing mental health symptomatology (Ettman et al., 2020; Salari et al., 2020). Although this pandemic has population-wide ramifications, certain groups may be disproportionately negatively affected , such as older adults and Black Americans (Garcia et al., 2020; Taylor, 2020). Understanding age and race differences in stress reactivity during the pandemic has potential to provide insights that will be helpful for both clinicians and public health officials.
The impact of experienced stress on mental health is well known (e.g., LeMoult, 2020; Miura et al., 2008). However, the pandemic involves both existing and emerging stressors, so it is important to examine the temporal space before stressors occur in addition to the reactions to experienced stressors. We focus on both the experience and forecasting of pandemic-specific stress and its impact on daily mental health symptomatology. Stressor forecasting involves predicting whether a stressor will occur within an upcoming defined period of time (Neubauer et al., 2018; Neupert et al., 2019). The extant literature on stressor forecasting is mixed on age or race differences in mental health outcomes, but we draw on the anticipatory stress framework (Neupert et al., 2019) that highlights the importance of individual as well as contextual differences to understand forecasted and experienced stressors for daily well-being. Neupert and Bellingtier (2019) found age differences in daily forecasting and subsequent emotional response, where younger adults benefited more from forecasting a home-related stressor than older adults. Understanding the effects of stressor forecasting as it relates to daily well-being across the life span is an important avenue of inquiry both for general understanding of the mental health symptom development as well as specific understanding of the impacts of an ongoing global pandemic. The dynamic nature of the pandemic (e.g., increases in cases, updated health recommendations) has been associated with fluctuating mental health and well-being over time. In the current study, we leverage a daily diary design over a 3-week period to capture dynamic fluctuations in COVID-19 stress and mental health and evaluate age and race differences in within-person reactivity to forecasting and experiencing daily COVID-19 stress. The daily diary framework, combined with the measurement of both experienced and forecasted stress, allows us to move beyond cross-sectional individual differences and focus on near real-time anticipation and effects of stress from a within-person perspective.
COVID-19 poses higher health risk to older adults (Nikolich-Zugich et al., 2020), resulting in higher rates of death and disability than younger and middle-aged adults (Sharma, 2020). The Strength and Vulnerability Integration (SAVI; Charles, 2010) model suggests that while older adults may be more psychologically resistant to short-term stressors, they may actually be more psychologically vulnerable to the effects of long-term stressor exposure. However, research during the pandemic has found that older adults may be faring better than younger adults (Klaiber et al., 2021; Pearman et al., 2021), suggesting that older adults may indeed be benefiting from enhanced emotion regulation during this time. Younger adults appear to be more susceptible to mental health consequences of the pandemic (e.g., Varma et al., 2021) with factors such as lack of sleep, lower levels of resilience, previous mental health issues, and loneliness acting as mediators in this relationship. However, given that age advantages for older adults in emotion regulation tend to be smaller over short timescales (Charles et al., 2016), it is important to take a microlongitudinal approach to see if (a) COVID-19-related stress affects people of different ages disparately on a daily basis and (b) whether the anticipation of COVID-19-related stress can affect daily mental well-being.
In addition to age, systemic inequities as well as other longstanding social, environmental, and economic disparities have put specific racial groups at greater risk of both contracting and dying from COVID-19 (Garcia et al., 2020; Kupferschmidt & Cohen, 2020). In particular, limited access to health care and having essential occupations that increase exposure have excessively burdened many Black Americans during the pandemic (Centers for Disease Control and Prevention, 2020). Additionally, the social zeitgeist of racial justice and recognition of racial disparities may increase the anticipation of prejudice and discrimination, leading to psychological and physiological stress responses among minorities (Pascoe & Smart Richman, 2009), thus making them more vulnerable to amplified psychological distress (Cobb et al., 2021; Kujawa et al., 2020) during this time. For instance, Rudenstine and colleagues (2020) showed that a greater frequency of exposure to COVID-19 stressors was associated with elevated levels of anxiety and depressive symptoms in Black Americans. Whether the effect of these disparities also varies by age is unknown but represents an important question.
Current Study
Using a sample of White and Black American adults ranging in age from 21 to 79, we move beyond descriptive work and examine the within-person effects of forecasted daily stress (next 24 h) as well as experienced daily stress (past 24 h) due to the pandemic on daily anxiety and depressive symptoms. We hypothesized that both experiencing and forecasting daily stress related to COVID-19 would be directly related to increases in that day’s anxiety and depressive symptoms (i.e., mental health reactivity), with these effects being more severe for younger (Brose et al., 2020; Pearman et al., 2020) and Black participants (Ibrahimi et al., 2020; Sneed et al., 2020). Because there are no published studies about daily or cross-sectional stressor forecasting specifically in Black American samples, we examined the synergistic effects of age and race on mental health reactivity to forecasted and experienced COVID-19 stress without making explicit predictions.
Method
Participants
Individuals were recruited online using two platforms: Qualtrics Panels and Amazon Mechanical Turk (MTurk). Participants had to identify as “Black or African American” or “White,” live in the United States, and be 21 years or older with no diagnosis of dementia. Informed consent was provided electronically. The final sample included 526 participants (60% female and 40% male), including 243 Black and 283 White individuals. Participant ages ranged from 21 to 79 years (M = 45.52, SD = 15.45). Regarding current household income, 32% of the sample had an income of $25,000 or less, 55% had an income between $25,000 and $100,000, and 13% had an income of $100,000 or more. Regarding employment status, the most common category was working full-time (45%), 15% of the sample was retired, and 10% was unemployed or laid off. The study was approved by the Georgia Institute of Technology Institutional Review Board.
Materials
Daily anxiety
On a scale ranging from 1 (not at all) to 4 (very much so), participants answered 12 items from the State–Trait Anxiety Inventory (Spielberger, 1989) about how anxious they felt over the past 24 h (within-person reliability = .83).
Daily depressive symptoms
On a scale from 0 (rarely or none of the time) to 3 (all the time), participants responded to the 10-item Center for Epidemiologic Studies—Depression scale (Radloff, 1977) about how depressed they felt within the past 24 h (within-person reliability = .66).
Forecasting daily COVID-19 stress
On a 5-point scale from 1 (not at all likely) to 5 (extremely likely), participants responded to the question “How likely is it that you will experience stress related to COVID-19 within the next 24 hours?”
Experiencing daily COVID-19 stress
Participants responded to the question, “How much stress have you experienced in the past 24 hours due to the COVID-19 outbreak?” on a scale ranging from 1 (none at all) to 5 (extreme).
Perceived risk of developing COVID-19
Individual differences in perceived risk of developing COVID-19 were collected in the first diary and used as a between-person covariate. On a 5-point scale from 1 (very low) to 5 (very high), participants responded to the question, “What do you think is the risk of you developing COVID-19?”
Procedure
Survey data were collected online using Qualtrics. Individuals from the Qualtrics Panel and MTurk completed up to 21 daily diaries between October 29 and November 18, 2020. Participants were compensated $5 for completing the first diary, which took approximately 25 min. The remaining daily diaries each took approximately 15 min to complete and participants were compensated $2 per diary. To encourage consistent participation throughout the 21-day study, a bonus payment of $5 was awarded for completing 19 diaries. The total number of collected diaries was 3,605. Depending on the number of completed diaries, participants could have been compensated up to $51 for participating in the study.
Results
Descriptive statistics can be found in Table 1. The sampling platform (Qualtrics Panels and MTurk) was included in all analyses to account for differences between the two samples. Compared to the MTurk sample, the Qualtrics sample was older, had fewer years of education, was disproportionately female, and had a greater number of Black Americans.
Table 1.
Descriptive Statistics for the Sample and Study Variables
| Variables | Mean | SD | Min | Max | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | 45.52 | 15.45 | 21 | 79 | — | ||||||||
| 2. Education (years) | 13.56 | 4.04 | 1 | 30 | .19** | — | |||||||
| 3. Gender | — | — | 0 | 1 | .13** | −.05 | — | ||||||
| 4. Race | — | — | 0 | 1 | −.43** | −.16** | a | — | |||||
| 5. Sample | — | — | 0 | 1 | .09* | −.12** | b | c | — | ||||
| 6. COVID-19 risk | 2.74 | 1.21 | 1 | 5 | −.01 | .09* | .02 | −.04 | .04 | — | |||
| 7. Forecasting COVID-19 stress | 2.54 | 1.33 | 1 | 5 | −.09* | .06 | .00 | −.04 | .05 | .39** | — | ||
| 8. Experiencing COVID-19 stress | 2.09 | 1.12 | 1 | 5 | −.17** | −.02 | −.05 | .07 | .15** | .28** | .68** | — | |
| 9. Anxiety | 2.09 | 0.67 | 1 | 4 | −.24** | −.07 | .08 | .02 | .07 | .23** | .42** | .41** | — |
| 10. Depressive symptoms | 9.61 | 6.50 | 0 | 29 | −.25* | −.08 | .07 | .04 | .14** | .26** | .45** | .46** | .79** |
Notes: Gender is coded as male = 0 and female = 1; race is coded as White = 0 and Black or African American = 1; sample is coded as MTurk = 0 and Qualtrics = 1. COVID-19 = coronavirus disease 2019.
aGender was equally distributed across race, χ2(1) = 2.71, p = .10.
bThe Qualtrics sample was disproportionately female, χ2(1) = 9.14, p < .01.
cThe Qualtrics sample had a greater number of Black Americans, χ2(1) = 72.16, p < .001.
*p < .05. **p < .01.
Results from fully unconditional models revealed that there was significant variance within and between persons in both outcomes (anxiety: 28% within person and 72% between person; depressive symptoms: 21% within person and 79% between person). Separate multilevel models were conducted for anxiety (Models 1 and 2) and depressive symptoms (Models 3 and 4) with the same predictors across both outcomes (Table 2). Daily (Level 1) predictors included the forecast (Models 1 and 3) or the experience (Models 2 and 4) of COVID-19 stress, with each Level 1 slope indexing within-person reactivity to forecasted or experienced COVID-19 stress. Person-level (Level 2) predictors included covariates (sample: MTurk or Qualtrics, perceived risk of contracting COVID-19, gender, years of education), age, and race. Our question regarding age and race differences in reactivity was addressed through a three-way cross-level interaction (Stress × Age × Race) in each model that also included the two-way interactions.
Table 2.
Unstandardized Estimates (Standard Errors) From Multilevel Models With Forecasting and Experiencing COVID-19 Stress Predicting Daily Anxiety and Daily Depressive Symptoms
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| Variables | Anxiety | Anxiety | Depressive symptoms | Depressive symptoms |
| Intercept | 2.47 (0.20)*** | 2.47 (0.20)*** | 13.48 (1.85)*** | 13.06 (1.79)*** |
| Sample | 0.23 (0.08)** | 0.19 (0.08)* | 3.92 (0.75)*** | 3.63 (0.74)*** |
| COVID-19 risk | 0.09 (0.02)** | 0.09 (0.02)*** | 0.99 (0.21)*** | 1.00 (0.21)*** |
| Gender | 0.13 (0.06)* | 0.15 (0.05)** | 1.11 (0.53)* | 1.23 (0.52)* |
| Education | −0.01 (0.01) | −0.00 (0.01) | −0.07 (0.07) | −0.06 (0.64) |
| Race | −0.51 (0.27) | −0.78 (0.26)** | −9.04 (2.47)** | −8.82 (2.37)** |
| Age | −0.02 (0.00)*** | −0.02 (0.00)*** | −0.21 (0.03)*** | −0.21 (0.03)*** |
| Forecasting COVID-19 stress | −0.01 (0.04) | −0.06 (0.34) | ||
| Age × Race | 0.00 (0.01) | 0.01 (0.01) | 0.13 (0.05)* | 0.12 (0.05)* |
| Age × COVID-19 forecasting | 0.002 (0.001)* | 0.01 (0.01) | ||
| Race × COVID-19 forecasting | 0.07 (0.07) | 1.23 (0.62)* | ||
| Age × Race × COVID-19 forecasting | −0.00 (0.00) | −0.02 (0.01) | ||
| Experiencing COVID-19 stress | −0.04 (0.05) | −0.10 (0.40) | ||
| Age × Experiencing COVID-19 stress | 0.003 (0.001)** | 0.02 (0.01)* | ||
| Race × Experiencing COVID-19 stress | 0.22 (0.08)** | 1.50 (0.69)* | ||
| Age × Race × Experiencing COVID-19 stress | −0.004 (0.001)* | −0.03 (0.02) | ||
| R 2 between | 24% | 25% | 26% | 29% |
| R 2 within | 5% | 7% | 6% | 7% |
Notes: Gender is coded as male = 0 and female = 1; race is coded as White = 0 and Black or African American = 1; sample is coded as MTurk = 0 and Qualtrics = 1. COVID-19 = coronavirus disease 2019. Unstandardized estimates and standard errors rounded to three decimal places are necessary to show the statistical significance of the p values.
*p < .05. **p < .01. ***p < .001.
Daily Anxiety
Results from Model 1, testing for age and race differences in reactivity to forecasted stressors, revealed that older adults reported less anxiety than younger adults with no main effect of forecasting. There was also a significant Age × Forecasting interaction where increases in forecasting were more strongly associated with increases in anxiety for older (b = 0.11, SE = 0.02, p < .0001) relative to younger (b = 0.10, SE = 0.02, p < .0001) adults based on separate models for younger and older adults (median split at 44). In addition, these separate models indicated heterogeneity within the age groups with significant interindividual differences in reactivity slopes for younger (τ 11 = 0.01, SE = 0.004, p = .006) and older (τ 11 = 0.014, SE = 0.004, p = .0006) participants.
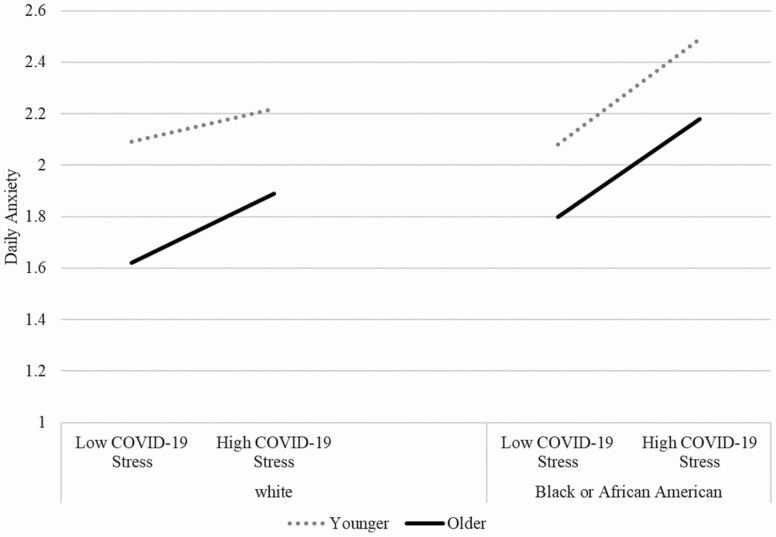
Model 2 tested for age and race differences in experienced daily COVID-19 stress on daily anxiety, and although there was no main effect of stress, the effects of COVID-19 stress did differ by age and race, and the three-way interaction of Age × Race × COVID-19 stress was significant (see Figure 1). Specifically, older White participants were more reactive than younger White participants, but the reactivity slopes for younger and older Black American participants were parallel but significantly steeper than those of White participants. The results also suggest heterogeneity within racial groups, as there were significant interindividual differences in reactivity slopes for White (τ 11 = 0.03, SE = 0.01, p < .0001) and Black participants (τ 11 = 0.03, SE = 0.01, p = .005).
Figure 1.
Coronavirus disease 2019 (COVID-19) stress × Age × Race cross-level interaction predicting daily anxiety. Low and high COVID-19 stress were operationalized as 1 SD below and above the mean, respectively. The lines for younger and older adults represent 1 SD below and above the mean age, respectively. Separate models conducted for Black American or White participants on daily reports of anxiety symptoms revealed that there were age differences in reactivity to COVID-19 stress for White participants (b = 0.003, SE = 0.001, p = .001), but not Black American participants (b = −0.0003, SE = 0.001, p = .846). The reactivity slopes for the Black American participants were significantly steeper than for the White Americans, suggesting that experiencing stress related to COVID-19 was consistently worse for anxiety symptomatology in Black American participants regardless of age.
Daily Depressive Symptoms
Results from Model 3, testing for age and race differences in reactivity to forecasted stressors, revealed that older adults reported fewer depressive symptoms than younger adults and that Black American adults reported fewer depressive symptoms than White adults. Although the three-way interaction of Age × Forecast × Race was not significant, the Age × Race and Forecast × Race interactions were significant. Separate models conducted for White and Black American participants revealed that age was negatively associated with depressive symptoms (b = −0.17, SE = 0.03, p < .0001) and increases in forecasting were associated with increases in depressive symptoms (b = 0.65, SE = 0.12, p < .0001) for White adults, but there was significant heterogeneity in this reactivity slope within White adults (τ 11 = 0.57, SE = 0.22, p = .004). For Black Americans, age was less negatively associated with depressive symptoms (b = −0.11, SE = 0.03, p < .0001) but increases in forecasting were more strongly associated with increases in depressive symptoms (b = 1.16, SE = 0.21, p < .0001) compared to White adults. There was also evidence of heterogeneity in this reactivity process within Black Americans (τ 11 = 1.37, SE = 0.68, p = .022).
Model 4 tested for age and race differences in reactivity to experienced stress, and in addition to the Age × Race interaction, there were age differences in reactivity as well as race differences in reactivity to experienced daily COVID-19 stress, but the three-way interaction was not significant. Increases in daily COVID-19 stress were associated with weaker increases in depressive symptoms for younger (b = 0.98, SE = 0.16, p < .0001) relative to older adults (b = 1.19, SE = 0.20, p < .0001) based on separate models for younger and older adults (median split at 44). There was evidence of heterogeneity within the younger (τ 11 = 0.60, SE = 0.35, p = .042) and older (τ 11 = 1.50, SE = 0.57, p = .004) adults in reactivity. Increases in COVID-19 stress were more strongly associated with increases in depressive symptoms for Black participants (b = 1.31, SE = 0.21, p < .0001) relative to White participants (b = 0.90, SE = 0.15, p < .0001). Although there was evidence of heterogeneity in reactivity within the White participants (τ 11 = 1.07, SE = 0.37, p = .002), there was no significant variance around the reactivity slope for Black American participants (τ 11 = 0.73, SE = 0.55, p = .095).
Discussion
This study was designed to move beyond cross-sectional descriptive work and investigate age and race differences in daily dynamics of mental health during the COVID-19 pandemic with particular emphasis on forecasted and experienced COVID-19 stress. Younger adults were significantly more likely to rate themselves as anxious or depressed than older adults, which is consistent with previous work showing that older adults are reporting better overall mental health than younger adults during the pandemic (Barber & Kim, 2021). In line with the strength concept from the SAVI model, older adults appear to have the benefits of psychological strength and emotion regulation as an overall response to the pandemic (Charles, 2010). However, when looking at dynamic associations on a daily basis, forecasting higher COVID-19 stress was associated with increases in anxiety symptoms for older adults compared to younger adults. There are challenges unique to this pandemic that will not have previously been experienced in people’s lifetimes and therefore may not benefit from age-related emotional learning. This, coupled with the increased risk of death from COVID-19 in older adults, is possibly creating this anticipatory anxiety response to COVID-19-related stress forecasting. Interestingly, the age-related strengths in emotion regulation associated with the SAVI model only held true for White older adults. For Black adults, experiencing COVID-19 stress was linked to increased anxiety regardless of age, and the reactivity for Black Americans was consistently stronger than that of White adults of all ages. This suggests that the co-occurrence of a racially imbalanced pandemic threat (Vasquez Reyes, 2020) coupled with existing systemic inequity may be more powerful than age-related strengths or vulnerabilities for Black adults’ anxiety.
At the mean level, Black Americans and White participants did not differ on levels of anxious or depressive symptomatology. However, we found that higher levels of experienced daily COVID-19 stress were more uniformly associated with increases in mental health symptomatology for Black Americans compared to White adults across all ages. That is, the negative impact of experiencing COVID-19 stress on depressive symptoms was consistent within the Black sample (i.e., lack of statistical variability around reactivity slope), regardless of age. This reactivity pattern suggests that the experience of COVID-19 stress may be contributing to the higher depressive burden of the pandemic for Black Americans not only overall (Kujawa et al., 2020) but also on a daily basis. This is an important finding that further confirms the added burden of the pandemic on Black Americans’ mental health. To reduce these mental health disparities, culturally competent interventions that target individuals at disproportionate risk of negative mental health outcomes are needed (Novacek et al., 2020).
Limitations and Future Directions
Two sampling platforms (Qualtrics Panels and MTurk) were used to ensure enough participants were in each racial group, but the Qualtrics sample was older and had more Black Americans than the MTurk sample. Additionally, the single-item measures of COVID-19-related stress were general in nature and did not probe the content or context of the stressors. Participants did not report the type of stressors they experienced or forecasted, or the everyday life domains (e.g., work, interpersonal relationships) impacted by the stressors, which could be fruitful to pursue in future work. It is possible that the observed patterns of stronger reactivity may be associated with lower starting values of anxiety and depressive symptoms. However, in all models except for Black Americans’ depressive symptoms in response to experienced COVID-19 stress, we find evidence of variance around the slopes, suggesting that there are individual differences in patterns of reactivity that may not be tied to a statistical artifact. Finally, measures of mental health in this report are indicators of endorsed symptoms, not actual diagnoses or help-seeking. Our findings lay the groundwork for future studies and work focused on outreach, especially to Black Americans across the adult life span in terms of managing burden and preventing mental health crises.
Conclusions
Although older adults reported better mental health than younger adults overall, the anticipation of COVID-19 stress was associated with a larger increase in anxiety symptomatology, particularly in White older adults. We also document daily mental health outcome disparities among Black Americans and White adults that are related to both forecasts and experiences of COVID-19-related stress. This is particularly important because the developmental processes that were previously identified with respect to forecasting (e.g., Neupert et al., 2019) were developed based on primarily White samples. A continued public policy focus on addressing systemic racism and the implications therein is clearly of import, particularly because of the protracted nature of the pandemic and the ongoing stressors related to it, such as employment challenges, health care disparities, and vaccine inequities.
Funding
None declared.
Conflict of Interest
None declared.
References
- Barber, S. J., & Kim, H. (2021). COVID-19 worries and behavior changes in older and younger men and women. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 76(2), e17–e23. doi: 10.1093/geronb/gbaa068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brose, A., Blanke, E. S., Schmiedek, F., Kramer, A. C., Schmidt, A., & Neubauer, A. B. (2020). Change in mental health symptoms during the COVID-19 pandemic: The role of appraisals and daily life experiences. Journal of Personality, 89(3), 468–482. doi: 10.1111/jopy.12592 [DOI] [PubMed] [Google Scholar]
- Charles, S. T. (2010). Strength and Vulnerability Integration (SAVI): A model of emotional well-being across adulthood. Psychology Bulletin, 136(6), 1068–1091. doi: 10.1037/a0021232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charles, S. T., Piazza, J. R., Mogle, J. A., Urban, E. J., Sliwinski, M. J., & Almeida, D. M. (2016). Age differences in emotional well-being vary by temporal recall. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 71(5), 798–807. doi: 10.1093/geronb/gbv011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . (2020). Health equity considerations and racial and ethnic minority groups. https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/race-ethnicity.html
- Cobb, R. J., Erving, C. L., & Byrd, W. C. (2021). Perceived COVID-19 health threat increases psychological distress among Black Americans. Ethnic and Racial Studies, 44(5), 806–818. doi: 10.1080/01419870.2021.1867216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ettman, C. K., Abdalla, S. M., Cohen, G. H., Sampson, L., Vivier, P. M., & Galea, S. (2020). Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Network Open, 3(9), e2019686. doi: 10.1001/jamanetworkopen.2020.19686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia, M. A., Homan, P. A., García, C., & Brown, T. H. (2020). The color of COVID-19: Structural racism and the pandemic’s disproportionate impact on older racial and ethnic minorities. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 76(3), e75–e80. doi: 10.1093/geronb/gbaa114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ibrahimi, S., Yusuf, K. K., Dongarwar, D., Maiyegun, S. O., Ikedionwu, C., & Salihu, H. M. (2020). COVID-19 devastation of African American families: Impact on mental health and the consequence of systemic racism. International Journal of MCH and AIDS, 9(3), 390–393. doi: 10.21106/ijma.408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klaiber, P., Wen, J. H., DeLongis, A., & Sin, N. L. (2021). The ups and downs of daily life during COVID-19: Age differences in affect, stress, and positive events. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 76(2), e30–e37. doi: 10.1093/geronb/gbaa096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kujawa, A., Green, H., Compas, B. E., Dickey, L., & Pegg, S. (2020). Exposure to COVID-19 pandemic stress: Associations with depression and anxiety in emerging adults in the United States. Depression and Anxiety, 37(12), 1280–1288. doi: 10.1002/da.23109 [DOI] [PubMed] [Google Scholar]
- Kupferschmidt, K., & Cohen, J. (2020). Race to find COVID-19 treatments accelerates. EClinical Medicine, 25, 1412–1413. doi: 10.1016/j.eclinm.2020.100455 [DOI] [PubMed] [Google Scholar]
- LeMoult, J. (2020). From stress to depression: Bringing together cognitive and biological science. Current Directions in Psychological Science, 29(6), 592–598. doi: 10.1177/0963721420964039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miura, H., Ozaki, N., Sawada, M., Isobe, K., Ohta, T., & Nagatsu, T. (2008). A link between stress and depression: Shifts in the balance between the kynurenine and serotonin pathways of tryptophan metabolism and the etiology and pathophysiology of depression. Stress (Amsterdam, Netherlands), 11(3), 198–209. doi: 10.1080/10253890701754068 [DOI] [PubMed] [Google Scholar]
- Neupert, S. D., & Bellingtier, J. A. (2019). Daily stressor forecasts and anticipatory coping: Age differences in dynamic, domain-specific processes. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 74(1), 17–28. doi: 10.1093/geronb/gby043 [DOI] [PubMed] [Google Scholar]
- Neupert, S. D., Neubauer, A. B., Scott, S. B., Hyun, J., & Sliwinski, M. J. (2019). Back to the Future: Examining age differences in processes before stressor exposure. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 74(1), 1–6. doi: 10.1093/geronb/gby074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neubauer, A. B., Smyth, J. M., & Sliwinski, M. J. (2018). When you see it coming: Stressor anticipation modulates stress effects on negative affect. Emotion (Washington, D.C.), 18(3), 342–354. doi: 10.1037/emo0000381 [DOI] [PubMed] [Google Scholar]
- Nikolich-Zugich, J., Knox, K. S., Rios, C. T., Natt, B., Bhattacharya, D., & Fain, M. J. (2020). SARS-CoV-2 and COVID-19 in older adults: What we may expect regarding pathogenesis, immune responses, and outcomes. Geroscience, 42(2), 505–514. doi: 10.1007/s11357-020-00186-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Novacek, D. M., Hampton-Anderson, J. N., Ebor, M. T., Loeb, T. B., & Wyatt, G. E. (2020). Mental health ramifications of the COVID-19 pandemic for Black Americans: Clinical and research recommendations. Psychological Trauma: Theory, Research, Practice and Policy, 12(5), 449–451. doi: 10.1037/tra0000796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pascoe, E. A., & Smart Richman, L. (2009). Perceived discrimination and health: A meta-analytic review. Psychological Bulletin, 135(4), 531–554. doi: 10.1037/a0016059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearman, A., Hughes, M. L., Smith, E. L., & Neupert, S. D. (2020). Mental health challenges of United States healthcare professionals during COVID-19. Frontiers in Psychology, 11, 2065. doi: 10.3389/fpsyg.2020.02065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearman, A., Hughes, M. L., Smith, E. L., & Neupert, S. D. (2021). Age differences in risk and resilience factors in COVID-19-related stress. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 76(2), e38–e44. doi: 10.1093/geronb/gbaa120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff, L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. doi: 10.1177/014662167700100306 [DOI] [Google Scholar]
- Rudenstine, S., McNeal, K., Schulder, T., Ettman, C. K., Hernandez, M., Gvozdieva, K., & Galea, S. (2020). Depression and anxiety during the COVID-19 pandemic in an urban, low-income public university sample. Journal of Traumatic Stress, 34(1), 12–22. doi: 10.1002/jts.22600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salari, N., Hosseinian-Far, A., Jalali, R., Vaisi-Raygani, A., Rasoulpoor, S., Mohammadi, M., Rasoulpoor, S., & Khaledi-Paveh, B. (2020). Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Globalization and Health, 16(1), 1–11. doi: 10.1186/s12992-020-00589-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma, A. (2020). Estimating older adult mortality from COVID-19. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 76(3), e68–e74. doi: 10.1093/geronb/gbaa161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sneed, R. S., Key, K., Bailey, S., & Johnson-Lawrence, V. (2020). Social and psychological consequences of the COVID-19 pandemic in African-American communities: Lessons from Michigan. Psychological Trauma: Theory, Research, Practice and Policy, 12(5), 446–448. doi: 10.1037/tra0000881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielberger, C. D. (1989). State-Trait Anxiety Inventory: Bibliography (2nd ed.). Palo Alto, CA: Consulting Psychologists Press. [Google Scholar]
- Taylor, R. J. (2020). Race and mental health among older adults: Within- and between-group comparisons. Innovation in Aging, 4(5). doi: 10.1093/geroni/igaa056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varma, P., Junge, M., Meaklim, H., & Jackson, M. L. (2021). Younger people are more vulnerable to stress, anxiety and depression during COVID-19 pandemic: A global cross-sectional survey. Progress in Neuro-Psychopharmacology & Biological Psychiatry, 109, 110236. doi: 10.1016/j.pnpbp.2020.110236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasquez Reyes, M. (2020). The disproportional impact of COVID-19 on African Americans. Health and Human Rights, 22(2), 299–307. [PMC free article] [PubMed] [Google Scholar]