Learning point for clinicians
Data have shown myocarditis may occur following mRNA Covid-19 vaccination as regarding to prothrombogenic syndrome following adenoviral vector vaccine injection. However, cardiac complications can still occur after adenoviral vector Covid-19 vaccination and delayed diagnosis will result in high mortality and morbidity. Therefore, healthcare providers should always maintain a high index of suspicion regarding myopericarditis following Covid-19 vaccination because early diagnosis with appropriate treatment significantly improved outcomes.
Introduction
The global pandemic of coronavirus 2019 (Covid-19) has brought ongoing mortality and morbidity since the outbreak in early 2020. Vaccination is considered the most effective intervention and various vaccines are created to help control the disease. However, vaccination is not without risk. Prothrombogenic syndrome was observed following adenoviral vector-based vaccination1 and myocarditis or pericarditis after mRNA vaccines has been reported.2 We are presenting a case of a young Asian male developing myopericarditis with pleuritis postadenoviral vector vaccination.
Case presentation
A previously healthy 23-year-old male student presented to our emergency room with chief complaints of fever, sore throat and progressive myalgia lasting for 4 days and was referred to our hospital after visiting a local clinic. He received his first AstraZeneca Covid-19 vaccine around 1 week before the fever episode. He has no history of systemic disease, medication usage nor travel, or cluster history. The vital sign showed fever with 39.3°C, a heart rate of 130 beats per minute, tachypnea with a respiratory rate of 20 breaths per minute, relatively low blood pressure (108/56 mmHg). Oxygen saturation was 95% under room air condition. Physical examination was unremarkable. An electrocardiogram showed tachycardia with nonspecific ST-segment change. Chest plain film showed a clear lung field with normal heart size. Blood essay revealed leukocytosis (16780/ul) with neutrophil predominance (83.5%) with high band form (8.3%). Elevated C-reactive protein of 18.83 mg/dl, highly elevated D-dimer 1619 ng/ml and mildly elevated troponin-T 104 ng/L with normal CKMB. Covid-19 PCR and Influenzae A and B were all tested negative.
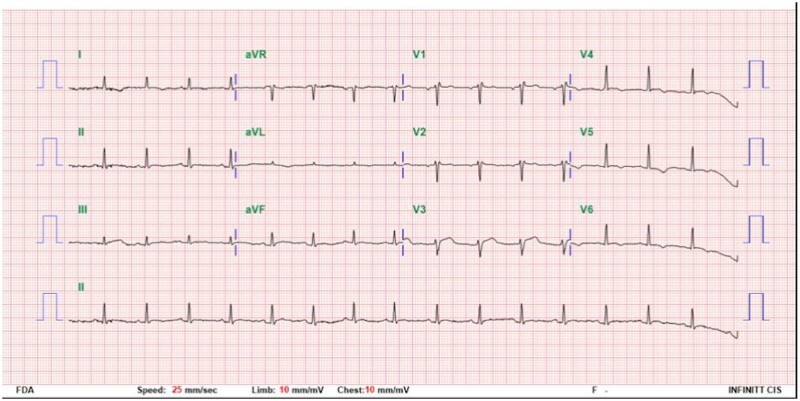
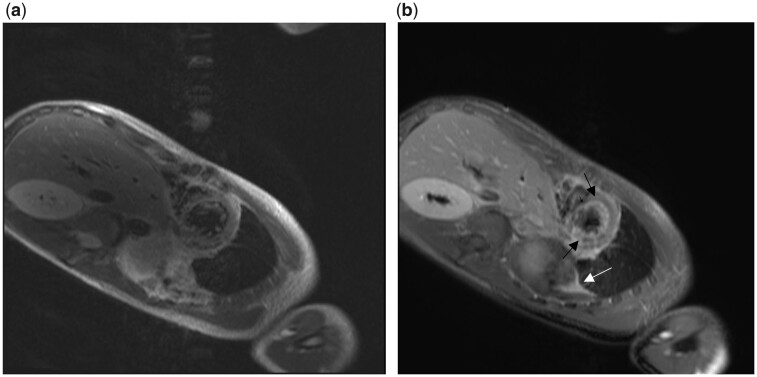
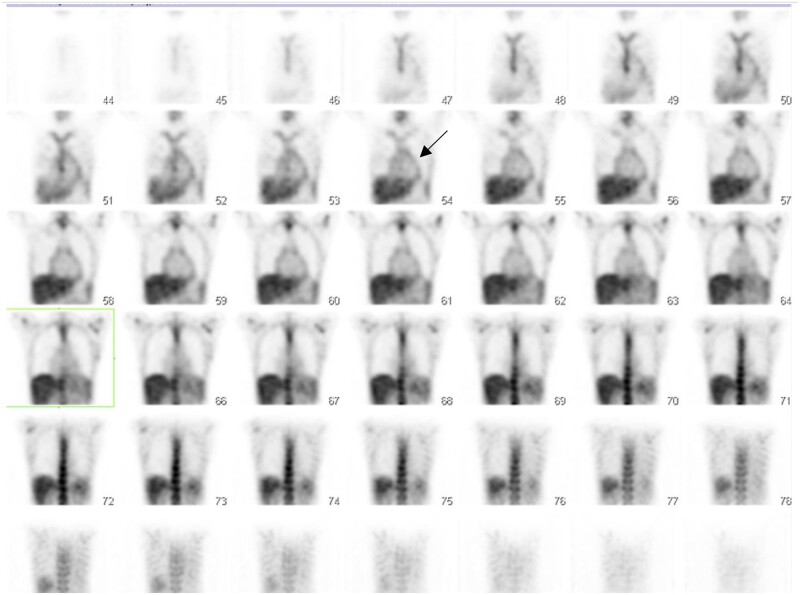
On the following day, dyspnea with tachycardia worsen and repeated laboratory data showed elevating cardiac enzyme (CK/CM-MB: 41/1.5 U/l to peak level 331/29 U/l in 8 h after admission) high NT-proBNP (4289 pg/ml) were noted and ECG showed dynamic change with lateral lead (V4–V6) T wave Inversion change (Figure 1). The cardiologist was consulted and cardiac echography showed preserved Left ventricular systolic function without regional wall motion anomaly. Cardiac angiography was suggested for evaluation but was deferred by family. Bisoprolol was prescribed for symptomatic control. However, despite cardiac enzyme returned to normal within 1 day, follow-up echography showed anteroseptal hypokinesia with pericardial effusion formation compared to previous cardiac echo done 2 days ago. Valsartan was added. Detailed autoimmune serology survey showed only mild elevated Rheumatoid factor (24 IU/ml, normal value < 15IU/ml). Myocarditis is suspected and due to the lack of a device for cardiac biopsy, we performed cardiac magnetic resonance exam (CMRI). T1 with gadolinium enhancement over pericardium and myocardium confirmed the presence of pericarditis with myocarditis (Figure 2). Steroid, colchicine, aspirin were prescribed. Fever, chest discomfort subsided after treatment. However, fever flared up after we tapered steroid dose. Chest X-ray showed bilateral pleural effusion and pleuralcentesis (Right: 250 cc, Left: 280 cc) found strawy fluid with exudative nature with neutrophil predominance leukocytosis. Culture studies were all negative therefore Gallium Inflammation scan was arranged for an occult infection survey and only pericardial uptake was found which supported the diagnosis of myopericarditis (Figure 3). No fever was noted after we titrate up steroid. The patient was discharged in stable condition after 10 days of admission and repeated studies arranged in out-patient visit 1 week after discharge showed normalized cardiac function with a total resolution of pericardial and pleural effusion.
Figure 1.
Twelve-lead electrocardiography showed lead I, V4–V6 T wave inversion, revealed possibility of myocardial damage.
Figure 2.
Cardiovascular magnetic resonance T1 image without (a)/with (b) gadolinium injection. The endocardium and epicardium gadolinium enhancement (black arrow) confirmed inflammation, supported the diagnosis of myopericarditis. Moreover, enhancement in pleural effusion suggested concurrent pleuritis (white arrow).
Figure 3.
Inflammation scan reveals mild increase uptake at the pericardial region, compatible with pericarditis (black arrow).
Discussion
Myopericarditis occurred after vaccination has been reported following small pox,3 DTaP,4 and also post-Covid-19 vaccine injection.5 Recent review shows Covid-19 vaccine-related myocardial injury usually presents in young Caucasian males with a median age of 36 years ago, at 3–10 days post-injection with.6 Data suggest Covid-19 vaccine-related myocarditis or pericarditis are mostly associated with mRNA and rarely following the virus vector vaccine.2 However, the incidence rate in the Asian population is not known and until now, no case report with myopericarditis with pleuritis following the AstraZeneca Covid-19 vaccine has been published.
In our case, symptoms occurred 7 days post-vaccination, and the patient was hospitalized for 12 days with a total recovery and the diagnosis of myopericarditis was based on elevated cardiac enzyme with reduced left ventricular ejection fraction with CMRI showed typical findings fulfilling lake Louise criteria for myocarditis. Inflammation scan also confirmed pericardial involvement without another infection source. In addition to myopericarditis, he has bilateral pleural effusion and resolved together with myocarditis event.
In this case, although specific viral culture studies and myocardium biopsy were not performed due to lack of resource backup but other comprehensive serology studies including autoimmune, human immunodeficiency virus and bacterial cultures for blood and pleural effusion were all negative findings. With the given negative result for the etiology survey, the possibility of vaccine-related myopericarditis with bilateral pleural effusion cannot be totally excluded.
In summary, we acknowledge vaccination is the key factor to significantly reduce the burden of the Covid-19 pandemic. However, postvaccination myocardial injury may occur and lead to the serious adverse event especially in the younger population. There is a global trend toward optimizing vaccination in young adult but concerns for vaccine-induced severe complication has held back the coverage rate. It is crucial to have more data to allow us to estimate the true incidence and understand the disease course in the context of a scientific manner to minimize the fear of getting vaccinated.
Early diagnosis is crucial in cardiac complication therefore it is important for healthcare provider to maintain a high index of suspicions for cardiac symptoms following Covid-19 vaccination.
Conflict of interest. None declared.
References
- 1. Rosenblum HG, Hadler SC, Moulia D, Shimabukuro TT, Su JR, Tepper NK, et al. Use of COVID-19 vaccines after reports of adverse events among adult recipients of Janssen (Johnson & Johnson) and mRNA COVID-19 vaccines (Pfizer-BioNTech and Moderna): update from the Advisory Committee on Immunization Practices - United States, July 2021. MMWR Morb Mortal Wkly Rep 2021; 70:1094–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rosner CM, Genovese L, Tehrani BN, Atkins M, Bakhshi H, Chaudhri S, et al. Myocarditis temporally associated with COVID-19 vaccination. Circulation 2021; 144:502–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sejvar JJ, Labutta RJ, Chapman LE, Grabenstein JD, Iskander J, Lane JM.. Neurologic adverse events associated with smallpox vaccination in the United States, 2002-2004. JAMA 2005; 294:2744–50. [DOI] [PubMed] [Google Scholar]
- 4. Boccara F, Benhaiem-Sigaux N, Cohen A.. Acute myopericarditis after diphtheria, tetanus, and polio vaccination. Chest 2001; 120:671–2. [DOI] [PubMed] [Google Scholar]
- 5. Das BB, Kohli U, Ramachandran P, Nguyen HH, Greil G, Hussain T, et al. Myopericarditis following mRNA COVID-19 vaccination in adolescents 12 through 18 years of age. J Pediatr 2021;238:26–32.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Diaz GA, Parsons GT, Gering SK, Meier AR, Hutchinson IV, Robicsek A.. Myocarditis and pericarditis after vaccination for COVID-19. JAMA 2021; 326:1210–2. [DOI] [PMC free article] [PubMed] [Google Scholar]