Abstract
Study Objectives
Insomnia has been on the rise during the 2019 coronavirus disease (COVID-19) pandemic, which may disproportionately affect racial minorities. This study characterized racial disparities in insomnia during the pandemic and evaluated mechanisms for such disparities.
Methods
Participants included 196 adults (48 Black) from a 2016–2017 clinical trial of insomnia treatment who were reevaluated in April 2020. Race was evaluated as a predictor of change in insomnia, impact of COVID-19, and COVID-19 stress. Mediation models using the PRODCLIN method evaluated the extent to which: (1) COVID-19 impact accounted for Black-White disparities in change in insomnia, and (2) COVID-19 stress accounted for associations between discrimination and change in insomnia.
Results
Increases in insomnia symptoms during COVID-19 were greater in Black compared to White participants, with 4.3 times the odds of severe insomnia (Insomnia Severity Index ≥ 22). Symptom severity was associated with pre-pandemic experiences of discrimination. Black participants were also disproportionately impacted by COVID-19, with twice the odds of irreparable loss of income/employment and four times the rate of COVID-19 diagnoses in their sociofamilial network compared to White participants. The disproportionate impact of COVID-19 accounted for 69.2% of the relationship between race and change in insomnia severity, and COVID-19 related stress accounted for 66.5% of the relationship between prior history of racial discrimination and change in insomnia severity.
Conclusions
Black-White disparities in insomnia severity during COVID-19 may be driven by structural inequities resulting in the disproportionate impact of COVID-19 on Black Americans. Results lend support for the minority stress model in the context of sleep health.
Clinical Trial Registration
Sleep to Prevent Evolving Affecting Disorders (SPREAD). NCT number: NCT02988375. https://clinicaltrials.gov/ct2/show/NCT02988375.
Keywords: COVID-19, insomnia, health disparities, discrimination, minority stress
Statement of Significance.
This study examined the racial disparities in insomnia during the 2019 coronavirus disease (COVID-19) pandemic and tested mechanisms driving such disparities. Results document Black-White disparity in insomnia severity, impact on daily life from the COVID-19 pandemic, and COVID-19 related stress, which likely stem from long-standing structural racism. Results also demonstrate that this Black-White disparity is driven by the disproportionate impact of the COVID-19 pandemic on Black relative to White Americans due to structural racism. Finally, results also lend support for the role of minority stress in racial disparities in sleep health, with results indicating that experiences of racial discrimination before the pandemic potentiated the impact of the pandemic on stress and insomnia.
Introduction
Among the long-standing challenges made even more salient by the 2019 Coronavirus Disease (COVID-19) pandemic is the pervasiveness and severity of racial health disparities in the United States. In fact, amidst the pandemic, the Centers for Disease Control and Prevention declared racism a serious public health threat, exemplified by the significantly higher rates of COVID-19 infection and mortality among Black relative to White Americans [1–3], and by the rise in violence against Asian-Americans and Pacific Islanders due to the national scapegoating of Chinese people for the coronavirus [4]. Many more occurrences during the COVID-19 pandemic have highlighted the multifactorial complexities that cause and maintain racial disparities.
Apart from coronavirus infection, the COVID-19 pandemic has also had health consequences extending well-beyond symptoms of the virus. Increases in mental health problems, including symptoms of insomnia, posttraumatic stress, anxiety, and depression have already been observed in the context of COVID-19 [5–9]. As a consequence, COVID-related disability and mortality will include impairment from mental illness, which is already a leading contributor to global disease burden [10]. Insomnia has been among the most prevalent problems during the pandemic, with the prevalence of clinically significant insomnia increasing between 47% and 189% [11, 12] compared to before the pandemic [13]. Importantly, insomnia is a robust risk factor for a cascade of medical and psychiatric morbidities, making it an important variable in health trajectories. Sleep disturbances and insomnia have been described as fundamental contributors to health disparities in cardiovascular disease [14]. Emerging research also indicates that early intervention for insomnia may significantly improve stress and resilience [15], and reduce concurrent depression and prevent incident depression by 50% [16–18].
Despite being a significant problem during the COVID-19 pandemic, the racial disparity in insomnia symptoms during the pandemic has not been well-characterized. Though the landscape of racial disparities research in insomnia prior to the COVID-19 pandemic has been mixed, there is growing evidence that Black Americans and people from other minoritized races experience more severe insomnia than White Americans. For example, relative to White Americans, Black Americans have a 67% increased risk of insomnia disorder with short sleep [19], which is among the most severe phenotypes of insomnia [20]. Furthermore, a large prospective study found that Black Americans were two times more likely to exhibit chronic insomnia (>1 year) than White Americans [21]. Research using objective measures of sleep also found that racially minoritized individuals exhibit longer sleep latencies and wake after sleep onset [22]. Given that Black Americans have been disproportionately impacted by COVID-19, it is likely that the disparity in insomnia would widen during the pandemic.
In addition to characterizing the racial disparities in insomnia, it is equally important to identify mechanisms driving such disparities to avoid the conflation of race as a risk factor as opposed to a social construct that functions as a proxy for racism. Specifically, the mechanisms driving adverse health outcomes in racial minorities are not caused by an individual’s race but instead by the various social and structural barriers to health that disproportionately impact minoritized individuals. For example, prior studies have identified perceived discrimination as a critical mechanism driving more severe sleep disturbances and insomnia in communities of Black, Indigenous, and people of color [23–29]. Indeed, those who report higher levels of discrimination have increased odds of moderate to severe insomnia (54% and 84% increase, respectively), and also generally show less sleep that is of worse quality [23, 29]. Furthermore, these effects are likely exacerbated by the additional stress of a global pandemic [30].
Beyond interpersonal discrimination, there are systemic social and structural inequities that may further account for racial/ethnic disparities in sleep health and insomnia. For example, acculturation stress and chronic stress are associated with greater insomnia symptom severity in Latinx/Hispanic adults [27, 28]. Furthermore, associations between insomnia and race/ethnicity are often attenuated or eclipsed by associations between insomnia symptoms and socioeconomic factors downstream from structural discrimination (e.g. employment status, education, food security, night work, noisy neighborhood) or health indicators (e.g. body mass index, physical activity, health problems) [27, 31–36]. Disparities in stress exposure, economic prosperity, and access to health care are also probable explanatory factors for racial disparities that would be exacerbated due to the COVID-19 pandemic, which together can then potentiate worse insomnia symptoms.
In examining racial disparities during the COVID-19 pandemic, it would be remiss to ignore the long history of racial discrimination that predates and potentiates the disproportionate burden of the pandemic on marginalized individuals. For these individuals, the COVID-19 pandemic compounded pre-existing social and structural racism. For example, the disproportionate COVID-19 infection and mortality rates in Black Americans stem from long-standing structural racism that have led to increased exposure to the virus (e.g. due to occupational and/or living circumstances that limit the ability for social distancing and self-isolation), limited and differential access to healthcare services (e.g. COVID-19 testing and care), and limited access to accurate and updated COVID-19 risks and recommendations. These are additive to the racism predating the pandemic; for example, in addition to George Floyd’s fatality driven by racial discrimination and institutional racism, a postmortem positive antigen test indicated that he also exhibited persistent viral activity from a prior COVID-19 infection [37]. Similarly, violence during the pandemic is reminiscent of both on-going and past racial traumas [38–40], which is additive to the generalized stress of a pandemic. Even indirect exposure to discrimination (e.g. media documentation of the murder of George Floyd) can trigger vicarious experiences of discrimination in marginalized individuals [41–43], which would only compound pandemic stress and exacerbate insomnia.
The potentiation of worse insomnia in marginalized individuals during the pandemic due to prior stress is consistent with the minority stress model, which has been used as a critical framework for understanding health disparities [44–46]. This model posits that minorities experience stress that is unique and chronic, arising from social and structural inequities that are additive to general stressors experienced by all people. The accumulation of minority stress, in turn, drives adverse health outcomes in marginalized individuals. Indeed, research has already implicated long-standing and pre-existing disparities in metabolic burden in Black Americans (e.g. obesity, hypertension, and diabetes) as key drivers of the greater susceptibility to COVID-19 infection and mortality along with other negative health outcomes [30, 47]. Additionally, COVID-19 related psychosocial stress (e.g. social isolation from quarantine) may further exacerbate pre-existing disparities (e.g. reduced sense of belonging due to racial discrimination) that then widen the racial disparity in insomnia severity during the pandemic [23, 24, 30].
The overarching aim of this study was to characterize racial disparities in insomnia during the COVID-19 pandemic and evaluate mechanisms driving such disparities. These aims were part of a larger study that examined resilience in the sleep and stress systems during the COVID-19 pandemic in a sample of adults who completed treatment for insomnia prior to the pandemic [48]. Participants in this trial predominantly resided in the Detroit metropolitan area, which was disproportionately impacted by the COVID-19 pandemic [49]. We hypothesized that Black participants would experience more insomnia, COVID-related disruptions to daily life, and COVID-related stress compared to White participants. We also hypothesized that the disproportionate impact of the COVID-19 pandemic would partially mediate racial disparities in increased insomnia during the pandemic. In addition, based on a minority stress model in which prior discrimination compounds the impact of future stressors, we tested the hypothesis that discrimination (pre-pandemic) would potentiate increased insomnia during the pandemic through increases in COVID-19 specific stress.
Methods
Participants for this study were recruited from a previous randomized controlled trial (Sleep to Prevent Evolving Affecting Disorders [SPREAD] trial: NCT02988375) that tested the efficacy of insomnia treatment in preventing incident depression [16, 17]. Participants received either digital Cognitive Behavioral Therapy for insomnia (dCBT-I) or a treatment-as-usual (TAU) condition that comprised sleep education. Participants in the SPREAD trial were enrolled between 2016 and 2017, with a final sample of 358 in the dCBT-I condition and 300 in the control condition. Those in the dCBT-I condition completed six sessions of dCBT-I, and those in the TAU sleep education condition received six weekly e-mails based on the National Institutes of Health (NIH) guide to healthy sleep [50]. All treatment and study materials were provided in English. Eligible participants met criteria for insomnia disorder based on the Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM-5), and participants were excluded if they reported a diagnosis of any untreated sleep disorders other than insomnia (e.g. obstructive sleep apnea, restless legs, narcolepsy, etc.), or bipolar or seizure disorders. Because the SPREAD trial included a depression prevention aim, individuals with high depression chronicity (self-reported daily or near-daily depressed mood and anhedonia) were excluded (see Cheng et al. [17] for additional details).
All 658 participants in the SPREAD trial were eligible for this follow-up study. The recruitment plan targeted enrollment at 200 participants to achieve sufficient statistical power to evaluate the primary study aims. Email invitations were sent during the last week of April 2020, 5 weeks into the Michigan state-wide stay-at-home order, with approximately 40 000 cases and 3800 deaths across the state. Enrollment was closed in the first week of May when the targeted sample size was achieved. The sample included 208 participants; of these individuals, only one identified as Asian, eight reported race unknown (or did not wish to report), and three identified with more than one race. Only two White participants endorsed an ethnicity of Hispanic or Latino. Both race and ethnicity data were self-reported. Given the small size of the subgroups, the final analyses included 196 individuals who reported their race as either Black (n = 48) or White (n = 148).
Measures of interest
Insomnia.
Symptoms of insomnia were assessed using the 7-item Insomnia Severity Index (ISI) [51], with higher scores indicating increased insomnia severity (range 0–28). To establish precedence in the mediation analysis to support causal inferences, posttreatment ISI scores from before the COVID-19 pandemic was subtracted from ISI measured during the pandemic to produce a measure of resurgence of insomnia symptoms.
Additionally, because the ISI is not designed to assess insomnia in response to a specific event, a prompt was included to assess the impact of the COVID-19 pandemic on sleep using a four-point Likert scale. The prompt was, “How much impact did the COVID-19 pandemic have on your sleep?”, and responses ranged from Not at all (0) to Very much (4). Results from this item were examined independently and were not incorporated into the ISI.
Coronavirus Impact Scale.
Degree of impact on daily life from the COVID-19 pandemic was measured using the Coronavirus Impact Scale (CIS). The CIS was made available through a collection of COVID-19 Research Tools assembled by the Office of Behavioral and Social Sciences Research at the NIH [50]. The CIS rates the degree of change across 11 domains of daily life on a four-point Likert scale (0 = no change, 1 = mild, 2 = moderate, 3 = severe). Domains assessed included routines; income/employment; access to food, medical care, and mental treatment; access to social support; pandemic related stress; familial stress and discord; and diagnoses and severity of COVID-19 in immediate as well as extended family and/or close friends. The scale has adequate internal consistency (α = 0.64–0.75) and validity, with mean scores ranging from 9.2 to 12.0 across five validation samples that consisted of primary caregivers (https://psyarxiv.com/kz4pg/).
COVID-19 related stress.
Stress and trauma specific to the COVID-19 pandemic were assessed using the 22-item Impact of Events Scale [52] (IESCOVID-19). The IES measures the amount of distress associated with a specific event. Although the IES allows individuals to specify the event in question, we predetermined “the COVID-19 pandemic” in the instructions as we were interested in measuring stress specifically associated with the COVID-19 pandemic. The total score on the IES ranges from 0 to 88. The IES score comprises three component scores: cognitive intrusion, avoidance, and hyperarousal. Both cognitive intrusion and avoidance describe psychological experiences of stress prior to the assimilation of the trauma, the cognitive intrusion reflecting repeated thoughts about the trauma, and avoidance reflecting effortful avoidance of reminders of the trauma. The third component describes physiological hyperarousal as a cluster of post-traumatic stress disorder symptoms.
Racial discrimination.
Racial discrimination was assessed during the 2016–2017 SPREAD trial via a single-item measure from the Commonwealth Fund 2001 Health Care Quality Survey [53] and the 2003 California Health Interview Survey [54]. These are validated and population-based surveys that are widely cited in academic research [55–57], and used in briefings for Congress and other governmental agencies to increase equity in health care policies. The prompt was “Thinking about your race or ethnicity, how often have you felt treated badly or unfairly because of your race or ethnicity.” with responses ranging from 0 to 4 (“Never” to “All the time”) and treated as a continuous variable in analyses. The construct validity of this measure has been demonstrated using health outcomes known to be associated with other measures of racism [55, 57, 58].
Analytic approach
All models in this manuscript (except those testing demographic differences) included treatment condition, sex, and household income (coded as an ordinal variable, see Table 1) as covariates. Age was included as a covariate during model building but was removed from the final models due to non-significance. Sensitivity analyses were also conducted in a subsample of females to examine potential effects of intersectionality [59, 60]; however, analyses were precluded from the final analyses due to redundancy with the full sample.
Table 1.
Baseline sample characteristics by group
| White (n = 148) | Black (n = 48) | |
|---|---|---|
| Age (M ± SD) | 45.7 ± 14.2 | 43.0 ± 12.9 |
| Sex (female) | 73.6% | 93.8% |
| 2019 household income | ||
| Very low (<15k) | 6.8% | 10.4 % |
| Low (<35k) | 24.3% | 16.7% |
| Middle (<75k) | 33.8% | 52.1% |
| High (≥75k) | 35.1% | 20.8% |
| Pre-COVID ISI (M ± SD) | 9.2 ± 6.2 | 10.8 ± 5.6 |
| Received dCBT-I | 51.0% | 40.0% |
| Perceived discrimination | 0.39 ± 0.67 | 1.50 ± 1.01 |
No group differences were detected except for sex and perceived discrimination.
dCBT-I, digital Cognitive Behavioral Therapy for Insomnia.
Racial disparities in the impact of the COVID-19 pandemic on insomnia (ISI) were tested using linear regressions. Racial disparities in daily life during the pandemic (CIS) and COVID-19 specific stress (IESCOVID-19) were tested using multivariate regression models accounting for all variables within the same models (i.e. the domains of functioning on the CIS, and the three subscales on the IESCOVID-19) to reduce the risk of family-wise error. Racial disparities were tested using the omnibus effect of race across all dependent variables in the multivariate model, and beta coefficients of race as the predictor (adjusted and standardized) were used to explore the magnitude of potential differences in subcomponents. Because two items on the CIS were count variables (i.e. count of family members diagnosed with COVID-19), negative binomial models were used to generate an incident rate ratio as the parameter estimate.
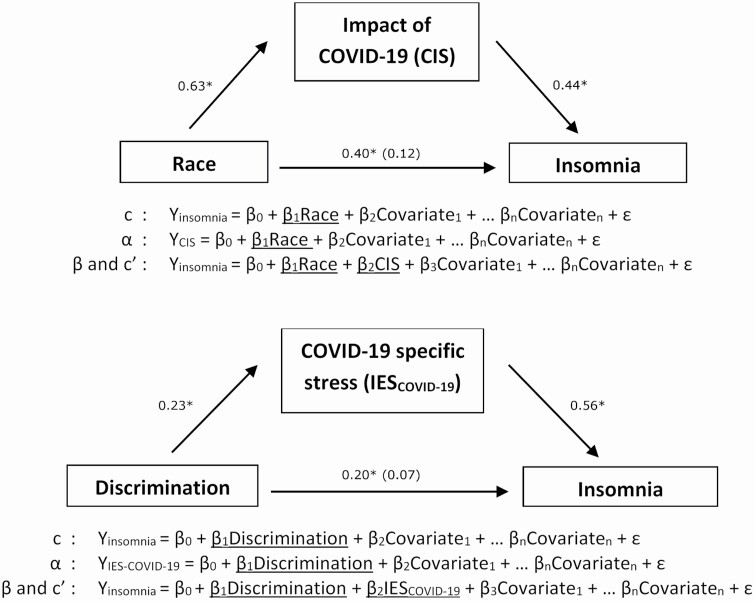
To examine disparities in the impact of the pandemic as a mechanism contributing to Black-White disparities in increased insomnia severity during the pandemic, a mediation analysis was conducted in accordance with procedures outlined by Fairchild and MacKinnon [61], with significance testing of the indirect effect using the distribution of the product approach (i.e. the PRODCLIN method) implemented in R [62]. This method is less vulnerable to Type I errors compared to traditional significance tests [63], and does not assume a normal distribution, which allows for asymmetric confidence intervals (CIs) [64, 65]. Statistical significance was determined if the 95% CI for the indirect effect did not include zero. The parameters required for the PRODCLIN approach (pathways α, β, c, and c′) were determined via three ordinary least squares regression models with covariates. Specifically, three regression models were conducted for the mediation analysis (see Figure 1): (1) the direct effect of the predictor (race) on the outcome variable (change in insomnia severity, i.e. ISI during the pandemic − ISI pre-pandemic), (2) the effect of the predictor (race) on the proposed mediator (impact of the COVID-19 pandemic), and finally (3) the effect of the mediator on the outcome variable. The indirect (i.e. mediated) effect of the predictor on the outcome variable was tested using the product of the α and β parameter estimates.
Figure 1.
Schematic of the mediation analyses. All analyses adjusted for treatment condition, sex, and household income as covariates. Pre-COVID-19 insomnia severity was subtracted from COVID-19 era insomnia severity to better approximate insomnia associated with the COVID-19 pandemic. Parameter estimates are included for the pathways. *p < .05.
We also examined perceived discrimination pre-pandemic as a predictor of pandemic-related stress (IESCOVID-19) and change in insomnia severity (i.e. ISI during the pandemic − ISI pre-pandemic), controlling for treatment condition, sex, household income, and race as covariates. Finally, we tested COVID-19 specific stress (IESCOVID-19) as a mediator in the relationship between prior perceived discrimination and change in insomnia severity during the pandemic (see Figure 1). In contrast with the first mediation model that tested CIS as a mediator, COVID-19 specific stress (IESCOVID-19) was selected a priori as the mediator for this analysis because it is better aligned with the minority stress hypothesis that specifically posits the accumulation of stress as a driving mechanism of health outcomes.1
Given that research conducted during a global pandemic may be vulnerable to selection bias [66, 67], we utilized sampling weights for all analyses to mitigate differences in the probability of selection into the study relative to the original population of SPREAD trial participants. Sampling weights equal to the reciprocal of the selection probability in each condition were used to balance the probability of selection based on insomnia severity following treatment in the SPREAD trial. Insomnia severity was categorized as non-clinically significant (ISI ≤ 7), subthreshold (ISI > 7 and ≤ 14), or clinically significant (ISI ≥ 15). The final weighted mean (9.8 ± 5.7 SD) did not differ significantly from the population mean (10.4 ± 5.8 SD). Additionally, comparison of the final sample in this study to those in the SPREAD trial revealed no differences in treatment compliance [t(840) = 1.104, ns], moderate-to-severe insomnia at post-treatment [χ2(1) = 0.581, ns], insomnia remission at post-treatment [χ 2(1) = 2.27, ns], nor by demographic variables (race: χ 2(1) = 0.120, ns; age: t(864) = 0.25, ns; sex: χ 2(1) = 0.017, ns; and income: χ 2(3) = 2.5, ns). Together, these data suggest that selection bias was likely minimal.
Results
Demographics
The final sample comprised 196 participants (see Table 1 for a summary of sample characteristics by group). On average, the sample age was 44.7 ± 14.1 SD, 78.4% female, and reported mild ISI scores (12.2 ± 6.9 SD). Black participants in this COVID follow-up study were more likely to be female (χ 2[1] = 7.55, p < .01) and reported more discrimination (F[1,194] = 77.31, p < .001) compared to White participants. There were no Black-White differences in income (b = −0.27 ± 0.30, ns), receipt of dCBT-I (b = −0.45 ± 0.34, ns), or post-treatment pre-pandemic insomnia symptoms (b = 0.36 ± 0.84, ns).
Disparities during the COVID-19 pandemic
Insomnia.
While no racial differences in insomnia were detected acutely following insomnia treatment in 2016–2017, Black participants reported more severe insomnia symptoms during the COVID-19 pandemic compared to White individuals after controlling for pre-COVID insomnia severity, treatment condition, sex, and household income, B = 0.37 ± 0.16 SE, p < .05 (see Table 2). Additionally, the odds of severe insomnia (ISI ≥ 22) was 4.2 times higher in Black compared to White participants, 95% CI = 2.4 to 7.3, p < .001. To further link sleep disturbances to COVID-19, an additional analysis also examined the extent to which sleep disturbances were attributed to COVID-19. Results showed that black participants attributed their sleep difficulties more to the COVID-19 pandemic than White participants, B = 0.40 ± 0.17 SE, p < .05.
Table 2.
Racial differences in the impact of the COVID-19 pandemic adjusted for treatment condition, sex, and household income
| White (n = 148) | Black (n = 48) | Statistical test values | |
|---|---|---|---|
| ISI | 11.2 ± 6.6 | 14.8 ± 7.6 | t(194) = 3.2, p < .001, d = 0.51 |
| CIS | 11.0 ± 4.5 | 14.2 ± 5.3 | t(202) = 4.1, p < .001, d = 0.65 |
| IESCOVID-19 | 24.5 ± 12.8 | 33.6 ± 17.0 | t(202) = 3.3, p < .001, d = 0.60 |
As reference, the range of CIS scores across five samples of primary caregivers during the pandemic was 8–12 (https://psyarxiv.com/kz4pg/).
ISI, Insomnia Severity Index; CIS, Coronavirus Impact Scale; IESCOVID-19, Impact of Events Scale specific to the COIVD-19 pandemic; d, Cohen’s d.
Coronavirus Impact Scale.
After accounting for covariates, the multivariate regression analysis indicated that Black participants were more severely impacted by the pandemic compared to White participants, F(26, 382) = 2.5, p < .001. This was reflected in the beta coefficient (standardized and adjusted) for the total CIS score, B = 0.61 ± 0.16 SE, p < .001, with the mean score for Black participants falling above the range found in primary caregivers during the pandemic (see Table 2 for summary statistics). Follow-up to the omnibus effect showed that Black-White differences were most pronounced in the domains of disturbances to family income/employment, diagnosis and symptom severity of COVID-19 in immediate family members, and diagnosis and symptom severity of COVID-19 in extended family members and/or close friends. Specifically, Black participants reported greater loss of family income/employment compared to White participants, B = 0.38 ± 0.17 SE, p < .05, with twice the odds of being unable to meet essential needs or fiscal responsibilities, OR = 2.04, 95% CI = 1.1 to 3.8. Incidence rate ratios indicated that COVID-19 diagnoses in immediate family members were 2.3 times higher in Black versus White participants, 95% CI = 1.6 to 3.3, with symptoms that were also more severe, B = 0.65 ± 0.16 SE, p < .001. The Black-White disparity in COVID-19 diagnoses and severity was even higher in extended family members and/or close friends: the incidence rate ratio indicated that COVID-19 diagnoses were 4.0 times higher in Black versus White participants, 95% CI = 3.1 to 5.1, with symptoms that were also more severe, B = 1.11 ± 0.15 SE, p < .001.
COVID-19 related stress.
The multivariate regression analysis indicated that Black participants also reported greater COVID-19 related stress compared to White participants, F(6,402) = 2.5, p < .05 (see Table 2 for summary statistics). The adjusted coefficients indicated that Black participants scored higher than White participants on all three subscales of the IESCOVID-19: intrusion, B = 0.41 ± 0.14 SE, p < .01; avoidance, B = 0.53 ± 0.17 SE, p < .01; and hyperarousal, B = 0.40 ± 0.17 SE, p < .05.
Associations between race, COVID-19 impact, and COVID-19 insomnia severity
Mediation analysis supported a significant direct effect in which Black participants reported greater resurgence of insomnia symptoms during the COVID-19 pandemic compared to White participants (pathway c: B = 0.40 ± 0.16 SE, p < .05; difference of 3.1 points on the ISI), after adjusting for treatment condition, sex, and 2019 annual household income. As demonstrated above, Black participants were also disproportionately impacted by the COVID-19 pandemic (pathway α: B = 0.63 ± 0.16 SE, p < .001). Finally, CIS scores remained a significant predictor of insomnia severity even after adjusting for race (pathway β: B = 0.44 ± 0.06 SE, p < .001), but the Black-White disparity in insomnia severity was no longer statistically significant after adjusting for CIS scores (pathway c′: B = 0.12 ± 0.15 SE, ns). The 95% CI of the indirect effect did not overlap with zero (α × β: 0.28, 95% CI = 0.12 to 0.47), and the indirect effect accounted for 69.2% of the greater increases in insomnia severity in Black compared to White participants.
Associations between prior racial discrimination, disparities in COVID-related stress, and COVID-19 insomnia severity
Mediation analysis demonstrated that more frequent encounters of racial discrimination prior to the pandemic predicted greater resurgence of insomnia symptoms during the pandemic (pathway c: B = 0.20 ± 0.08 SE, p < .01; b = 1.7 points on the ISI). Racial discrimination also potentiated COVID-19 related stress (pathway α: B = 0.23 ± 0.08 SE, p < .01). Finally, COVID-related stress remained a significant predictor of greater increases in insomnia severity even after adjusting for history of racial discrimination (B = 0.56 ± 0.06 SE, p < .001); however, discrimination was no longer a significant predictor of insomnia severity (pathway c′: B = 0.07 ± 0.07 SE, ns). The 95% CI of the indirect effect did not overlap with zero (α × β: 0.13, 95% CI = 0.04 to 0.24), and the indirect effect accounted for 66.5% of the relationship between racial discrimination and increases in insomnia severity during the COVID-19 pandemic.
Discussion
The aims of this study were to characterize racial disparities of insomnia during the COVID-19 pandemic and evaluate mechanisms driving such disparities. This was conducted in a sample of individuals who received behavioral treatment for insomnia prior to the pandemic. As expected, we found that Black participants were disproportionately impacted by the pandemic, particularly in the domains of family income and employment as well as higher rates of COVID-19 diagnosis and severity in social and familial networks. We also found that Black participants exhibited more severe insomnia during the pandemic after adjusting for covariates including household income, which suggests that this racial disparity cannot be solely explained by socioeconomic differences. This finding is especially notable as no significant racial differences in insomnia severity were found in the same sample prior to the pandemic after receiving insomnia treatment in 2016/2017. Furthermore, the Black-White disparity in insomnia severity during the pandemic in this sample was approximately threefold the magnitude of disparities found pre-pandemic [17, 68], suggesting that the racial disparities in insomnia grew in conjunction with the disproportionate social stressors during the pandemic. Results also indicated that Black participants reported higher levels of COVID-related stress compared to White participants, and that this stress was associated with a history of perceived racial discrimination prior to the pandemic.
This study also provided evidence that the disproportionate impact of the pandemic on Black Americans may be a key mechanism driving Black-White disparities in insomnia symptoms. This lends further support that racial disparities in insomnia likely result from structural inequities that impact health outcomes. For example, historical barriers to property ownership and social mobility (e.g. mortgage redlining [69], high-density housing [70], discriminatory hiring practices [71, 72], income inequality [73]) likely rendered protective measures out-of-reach, such as social distancing and self-isolation. Additionally, the existing wealth gap between Black and White Americans [74] likely resulted in the more Black Americans needing to continue work through the pandemic. Combined with the fact that Black Americans are overrepresented in industries with front-line workers and without worker protections (e.g. paid sick leave) [75], these disparities exacerbate the risk for and consequences of coronavirus exposure. Together, these long-standing structural inequities likely lead to disproportionate social stressors that precipitated a resurgence or exacerbation of insomnia symptoms, especially in a vulnerable sample with a history of insomnia disorder. Indeed, the mediation model indicated that a significant majority (approximately 70%) of the racial disparity in insomnia severity was explained by the disproportionate impact of the pandemic on Black Americans.
Our results provide further support for the role of minority stress in disparities in sleep health. Specifically, we found that those who reported more frequent experiences of racial discrimination prior to the pandemic also reported more severe COVID-19 specific stress and exhibited more severe insomnia. This aligns with the minority stress model in which minoritized people experience the compounding accrual of unique and chronic social stressors that result in worse long-term health deficits than non-marginalized individuals [44]. Indeed, our results support the hypothesis that higher COVID-19 specific stress mediates the relationship between discrimination and increased insomnia symptoms during the pandemic, suggesting that COVID-19 specific stress may be tapping into a similar or related latent construct as racial discrimination despite a relatively weak correlation (r = .22). In this context (and in alignment with components of the minority stress model), it may be that experiences of discrimination potentiates increased vigilance [76] (e.g. hyperarousal) and expectancies of adverse outcomes due to the COVID-19 pandemic (and thus worry and rumination), which then exacerbate insomnia symptoms and/or depletes cognitive and emotional resources that would otherwise be deployed for coping and emotional regulation. However, it should be noted that this sample was not adequately powered to parse this indirect effect by race (i.e. COVID-19 stress as a mediator between discrimination and insomnia), which would speak more directly to a racial disparity. As such, interpretation of these results should be tempered before this comparison is made in future research.
The strengths of this study include the use of a longitudinal sample that enabled comparison of insomnia severity prior to the onset of the pandemic. Furthermore, individuals in this sample had received behavioral treatment for insomnia that attenuated prior racial disparities in insomnia severity [77], which mitigates pre-COVID disparities as a confounding variable. This research also provides an important contribution to our understanding of the highlighted and exacerbated sleep health disparities seen in Black Americans during the global COVID-19 pandemic.
There are some limitations to consider regarding the generalizability of these results. First, this sample only included those who previously had exposure to a sleep intervention (including CBT-I) which likely bolstered health and functioning during the pandemic [48]. As such, true magnitude of disparities in the greater population is likely larger than that represented in this sample. Second, our results were limited to Black-White disparities because there was inadequate representation of other races in the sample, resulting in insufficient power to parse analyses by other races/ethnicities. Furthermore, the sample was not balanced by Black and White participants, with fewer number of Black participants which limited more complex analyses that parse effects by race.
Additional considerations regarding the generalizability of these results include that the data were collected in April 2020, and thus may not represent the effects of race or discrimination on insomnia and COVID-related life impact and stress later in the course of the pandemic. Participants were also sampled from communities in the Detroit metropolitan area and may not generalize to other geographic regions, although findings have been consistent with national reports of racial disparities during the COVID-19 pandemic. A few studies examining insomnia symptoms during the COVID-19 pandemic found that urban citizens scored higher in overall insomnia symptoms than rural residents [12, 78]. These results suggest that individuals living in bigger cities may be at a greater risk for insomnia. Rural residence may act as a buffer providing more opportunities for outside physical activity, exposure to natural environments, and less restriction as exposure risk is lower. There are also methodological considerations when interpreting the study results. First, insomnia symptoms were assessed concurrently with COVID-19 impact and stress, and insomnia can contribute to mental health and immune function [79]. Causal inferences about the effects of COVID-19 impact and stress on insomnia symptoms should be tempered by the bidirectional associations between insomnia symptoms, perceived stress, and health outcomes. Another important consideration is that individuals received two different treatments (i.e. dCBT-I and sleep education). Although prior reports indicate that insomnia improved in both treatment conditions [16, 17], CBT-I is the recommended first-line treatment for insomnia [80, 81]. However, all models controlled for treatment condition as a covariate, suggesting that the differences found in this sample were not due to the effect of prior treatment type.
Additional research is also needed to examine the impact of the COVID-19 pandemic on other high-risk populations. For example, there is a need for additional work to examine the impact of the COVID-19 pandemic on Asian American and Pacific Islanders (AAPI) given the rise in anti-Asian racism [39]. The physical and economic assault against AAPI (e.g. xenophobic attacks against Asian restaurants and businesses) are reminiscent of past racial traumas and exclusionary measures such as the Chinese Exclusion Act (federal law prohibiting immigration of Chinese people, including laborers who were critical to building the US infrastructure, e.g. the transcontinental railroad), the Japanese Internment (incarceration of Japanese-American citizens in concentration camps during World War II), and People v. Hall (law barring any individuals of Chinese descent to testify against White people). Similarly, more work is needed to examine the impact of the COVID-19 pandemic on Hispanic/Latinx populations, which represent the largest ethnic minority group in the United States, and Native American and Indigenous peoples. These communities that have been disproportionately impacted by the COVID-19 pandemic and may be especially likely to experience potentiation of COVID-related stress due to historical trauma resulting from colonially-based disease, restriction of geographic and social mobility, and medical abuse and neglect. In addition, this study is underpowered to examine the compounding and interactive effects of sociodemographic characteristics other than race (e.g. gender). Intersectionality between minoritized social statuses likely contribute to sleep health disparities, but they are inadequately understood and rarely evaluated [82].
Conclusion
This study found that Black Americans were disproportionately impacted by the COVID-19 pandemic, and COVID-19 impact partially mediated racial disparities in insomnia symptoms during the pandemic. Indeed, the Black-White disparity in insomnia severity was almost threefold more severe than pre-pandemic levels, even though this sample received treatment for insomnia prior to the pandemic. This study also demonstrated that racial discrimination was associated with an exacerbated impact of the COVID-19 pandemic. These results suggest that prevention and intervention for COVID-related increases in insomnia symptoms may depend upon relief from structural inequities in employment, income, and healthcare among other forms of discrimination experienced by Black Americans. Future research should examine the impact of the COVID-19 pandemic and sleep in other marginalized and intersectional groups (e.g. the AAPI community, minoritized women versus men), and how disparities in sleep health may be improved with more structural equity in the United States.
Acknowledgments
Support for PC was provided from the National Heart Lung and Blood Institute (K23HL138166). We would also like to thank the Division of Sleep Medicine and the staff at the Thomas Roth Sleep Disorders and Research Center at the Henry Ford Health System for their continued support.
Footnotes
Analyses using CIS as a mediator yielded similar results.
Disclosure Statement
Financial Disclosures: PC is funded by the National Heart Lung and Blood Institute (K23HL138166). DJ is funded by the National Heart Lung and Blood Institute (K01HL138211).
Nonfinancial Disclosures: none
Authors’ Contributions
Concept and Design: Cheng, Casement, Drake
Acquisition, Analysis, or Interpretation of data: Cuamatzi Castelan, Cheng, Casement
Drafting of manuscript: Cheng, Casement, Cuellar
Critical revision of the manuscript for important intellectual content: Johnson, Kalmbach, Drake
References
- 1. Anyane-Yeboa A, et al. Racial disparities in COVID-19 deaths reveal harsh truths about structural inequality in America. J Intern Med. 2020;288(4):479–480. [DOI] [PubMed] [Google Scholar]
- 2. Shah M, et al. COVID-19 and racial disparities. J Am Acad Dermatol. 2020;83(1):e35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Alcendor DJ. Racial disparities-associated COVID-19 mortality among minority populations in the US. J Clin Med. 2020;9(8):2442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gover AR, et al. Anti-Asian hate crime during the COVID-19 pandemic: exploring the reproduction of inequality. Am J Crim Justice. 2020;45(4):647-667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nelson BW, et al. Rapid assessment of psychological and epidemiological correlates of COVID-19 concern, financial strain, and health-related behavior change in a large online sample. PsyArXiv. 2020. doi: 10.31234/osf.io/jftze. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wang C, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17(5):1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Huang Y, et al. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020;288:112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rajkumar RP. COVID-19 and mental health: a review of the existing literature. Asian J Psychiatr. 2020;52:102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cellini N, et al. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J Sleep Res. 2020;29(4):e13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. World Health Organization. Global Health Estimates 2016: Disease burden by Cause, Age, Sex, by Country and by Region, 2000–2016; 2018. https://www.who.int/healthinfo/global_burden_disease/estimates/en/index1.html. Accessed September 1, 2019. [Google Scholar]
- 11. Kokou-Kpolou CK, et al. Insomnia during COVID-19 pandemic and lockdown: prevalence, severity, and associated risk factors in French population. Psychiatry Res. 2020;290:113128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Voitsidis P, et al. Insomnia during the COVID-19 pandemic in a Greek population. Psychiatry Res. 2020;289:113076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Morin CM, et al. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34(5):601–608. doi: 10.1093/sleep/34.5.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Jackson CL, et al. Sleep as a potential fundamental contributor to disparities in cardiovascular health. Annu Rev Public Health. 2015;36:417–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cheng P, et al. Digital cognitive behavioral therapy for insomnia promotes later health resilience during the coronavirus disease 19 (COVID-19) pandemic. Sleep. 2020;44(4). doi: 10.1093/sleep/zsaa258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Cheng P, et al. Depression prevention via digital CBT for insomnia: a randomized controlled trial. Sleep. 2019;42(4). doi: 10.1093/sleep/zsz150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cheng P, et al. Efficacy of digital CBT for insomnia to reduce depression across demographic groups: a randomized trial. Psychol Med. 2018;49(3):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Batterham PJ, et al. Trajectories of change and long-term outcomes in a randomised controlled trial of internet-based insomnia treatment to prevent depression. BJPsych Open. 2017;3(5):228–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kalmbach DA, et al. DSM-5 insomnia and short sleep: comorbidity landscape and racial disparities. Sleep. 2016;39(12):2101–2111. doi: 10.5665/sleep.6306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Vgontzas AN, et al. Insomnia with objective short sleep duration: the most biologically severe phenotype of the disorder. Sleep Med Rev. 2013;17(4):241–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Singareddy R, et al. Risk factors for incident chronic insomnia: a general population prospective study. Sleep Med. 2012;13(4):346–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Johnson DA, et al. Are sleep patterns influenced by race/ethnicity – a marker of relative advantage or disadvantage? Evidence to date. Nat Sci Sleep. 2019;11:79–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Bethea TN, et al. Perceived racial discrimination and risk of insomnia among middle-aged and elderly Black women. Sleep. 2019;43(1). doi: 10.1093/sleep/zsz208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cheng P, et al. Racial discrimination as a mediator of racial disparities in insomnia disorder. Sleep Health. 2020;6(5):543–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Fuller-Rowell TE, et al. Racial discrimination mediates race differences in sleep problems: a longitudinal analysis. Cultur Divers Ethnic Minor Psychol. 2017;23(2):165–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lee S, et al. Multiple types of perceived job discrimination and sleep health among working women: findings from the sister study. Am J Epidemiol. 2020;189. doi: 10.1093/aje/kwaa075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Alcántara C, et al. Employment status and the association of sociocultural stress with sleep in the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Sleep. 2019;42(4). doi: 10.1093/sleep/zsz002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Alcántara C, et al. Stress and sleep: results from the Hispanic Community Health Study/Study of Latinos Sociocultural Ancillary Study. SSM Popul Health. 2017;3:713–721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ogbenna BT, et al. Discrimination and sleep among Asians and Pacific Islanders adults. Sleep. 2021. doi: 10.1093/sleep/zsab109. [DOI] [PubMed] [Google Scholar]
- 30. Jackson CL, et al. Sleep disparities in the era of the COVID-19 pandemic highlight the urgent need to address social determinants of health like the virus of racism. J Clin Sleep Med. 2020;16(8):1401–1402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kaufmann CN, et al. Racial/ethnic differences in insomnia trajectories among U.S. older adults. Am J Geriatr Psychiatry. 2016;24(7):575–584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kalmbach DA, et al. Insomnia, short sleep, and snoring in mid-to-late pregnancy: disparities related to poverty, race, and obesity. Nat Sci Sleep. 2019;11:301–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Jones RD, et al. Ethnoracial sleep disparities among college students living in dormitories in the United States: a nationally representative study. Sleep Health. 2020;6(1):40–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Paine SJ, et al. Who reports insomnia? Relationships with age, sex, ethnicity, and socioeconomic deprivation. Sleep. 2004;27(6):1163–1169. doi: 10.1093/sleep/27.6.1163. [DOI] [PubMed] [Google Scholar]
- 35. Grandner MA, et al. Sleep symptoms, race/ethnicity, and socioeconomic position. J Clin Sleep Med. 2013;9(9):897–905; 905A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Simonelli G, et al. Neighborhood factors as predictors of poor sleep in the Sueno ancillary study of the Hispanic Community Health Study/Study of Latinos. Sleep. 2017;40(1). doi: 10.1093/sleep/zsw025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Neuman S. Medical Examiner’s Autopsy Reveals George Floyd Had Positive Test for Coronavirus. National Public Radio. https://www.npr.org/sections/live-updates-protests-for-racial-justice/2020/06/04/869278494/medical-examiners-autopsy-reveals-george-floyd-had-positive-test-for-coronavirus. Accessed July 16, 2021. [Google Scholar]
- 38. Chen HA, et al. Anti-Asian sentiment in the United States – COVID-19 and history. Am J Surg. 2020;220(3):556–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Cheng P, et al. Moving beyond the “model minority” myth to understand sleep health disparities in Asian American and Pacific Islander communities. J Clin Sleep Med. 2021. doi: 10.5664/jcsm.9500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Jean T. Black lives matter: police brutality in the era of COVID-19. NC Med J. 2020;81:137–140. [Google Scholar]
- 41. Herda D, et al. No experience required: Violent crime and anticipated, vicarious, and experienced racial discrimination. Soc Sci Res. 2018;70:115–130. [DOI] [PubMed] [Google Scholar]
- 42. Wofford N, et al. The vicarious effects of discrimination: how partner experiences of discrimination affect individual health. Soc Psychol Personal Sci. 2019;10(1):121–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Tynes BM, et al. Online racial discrimination and psychological adjustment among adolescents. J Adolesc Health. 2008;43(6):565–569. [DOI] [PubMed] [Google Scholar]
- 44. Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Bowleg L, et al. Triple jeopardy and beyond: multiple minority stress and resilience among black lesbians. J Lesbian Stud. 2003;7(4):87–108. [DOI] [PubMed] [Google Scholar]
- 46. Carden KD, et al. Minority stress process among older Black Americans: the role of age, perceived discrimination, and anxiety. Aging Ment Health. 2021:1–9. [DOI] [PubMed] [Google Scholar]
- 47. Jean-Louis G, et al. Increased metabolic burden among Blacks: a putative mechanism for disparate COVID-19 outcomes. Diabetes Metab Syndr Obes. 2020;13:3471–3479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Cheng P, et al. Digital cognitive behavioral therapy for insomnia promotes later health resilience during the coronavirus disease 19 (COVID-19) pandemic. Sleep. 2020;44(4). doi: 10.1093/sleep/zsaa258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Ray R, et al. Examining and Addressing COVID-19 Racial Disparities in Detroit. Washington, DC: Brookings Institute; 2021. [Google Scholar]
- 50. National Heart Lung and Blood Institute. Your Guide to Healthy Sleep; 2011. www.nhlbi.nih.gov/health-topics/all-publications-and-resources/your-guide-healthy-sleep.
- 51. Bastien CH, et al. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2(4):297–307. [DOI] [PubMed] [Google Scholar]
- 52. Weiss DS, et al. Assessing psychological trauma and PTSD. Impact Events Scale—Revised. 1997;19:399–411. [Google Scholar]
- 53. The Commonwealth Fund. 2001 Health Care Quality Survey; 2001. https://www.commonwealthfund.org/publications/surveys/2002/mar/2001-health-care-quality-survey. Accessed January 22, 2020.
- 54. UCLA Center for Health Policy Research. California Health Interview Survey; 2003. http://healthpolicy.ucla.edu/chis/Pages/default.aspx. Accessed January 22, 2020.
- 55. Otiniano AD, et al. Self-reported discrimination and health-related quality of life among Whites, Blacks, Mexicans and Central Americans. J Immigr Minor Health. 2012;14(2):189–197. [DOI] [PubMed] [Google Scholar]
- 56. Gee GC, et al. Associations between racial discrimination, limited English proficiency, and health-related quality of life among 6 Asian ethnic groups in California. Am J Public Health. 2010;100(5):888–895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Shariff-Marco S, et al. Racial/ethnic differences in self-reported racism and its association with cancer-related health behaviors. Am J Public Health. 2010;100(2):364–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Agunwamba AA, et al. Mental health, racial discrimination, and tobacco use differences across rural-urban California. J Rural Health. 2017;33(2):180–189. [DOI] [PubMed] [Google Scholar]
- 59. Kapilashrami A, et al. Intersectionality and why it matters to global health. Lancet. 2018;391(10140):2589–2591. [DOI] [PubMed] [Google Scholar]
- 60. Crenshaw K. Mapping the margins: intersectionality, identity politics, and violence against women of color. Stan Rev. 1990;43:1241. [Google Scholar]
- 61. Fairchild AJ, et al. A general model for testing mediation and moderation effects. Prev Sci. 2009;10(2):87–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Tofighi D, et al. RMediation: an R package for mediation analysis confidence intervals. Behav Res Methods. 2011;43(3):692–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Hayes AF, et al. The relative trustworthiness of inferential tests of the indirect effect in statistical mediation analysis: does method really matter? Psychol Sci. 2013;24(10):1918–1927. [DOI] [PubMed] [Google Scholar]
- 64. Mackinnon DP, et al. Confidence limits for the indirect effect: distribution of the product and resampling methods. Multivariate Behav Res. 2004;39(1):99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. MacKinnon DP, et al. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods. 2002;7(1):83–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Zhao Q, et al. BETS: The dangers of selection bias in early analyses of the coronavirus disease (COVID-19) pandemic. ArXiv Prepr ArXiv200407743. 2020. [Google Scholar]
- 67. Sullivan SG. The need for robust epidemiological evidence during a pandemic. Clin Infect Dis. 2020;71(16):2289–2290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Cheng P, et al. Racial discrimination as a mediator of racial disparities in insomnia disorder. Sleep Health. 2020;6(5):543–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Hernandez J. Redlining revisited: mortgage lending patterns in Sacramento 1930–2004. Int J Urban Reg Res. 2009;33(2):291–313. [Google Scholar]
- 70. Black/African American Communities are at highest risk of COVID-19: spatial modeling of New York City ZIP Code–level testing results – ScienceDirect. https://www-sciencedirect-com.proxy.lib.umich.edu/science/article/pii/S1047279720302933. Accessed September 3, 2021. [DOI] [PMC free article] [PubMed]
- 71. Agan A, et al. Ban the box, criminal records, and racial discrimination: a field experiment. Q J Econ. 2018;133(1):191–235. [Google Scholar]
- 72. Pager D. The mark of a criminal record. Am J Sociol. 2003;108(5):937–975. [Google Scholar]
- 73. Oronce CIA, et al. Association between state-level income inequality and COVID-19 cases and mortality in the USA. J Gen Intern Med. 2020;35(9):2791–2793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Khanal K, et al. Will COVID-19 worsen the racial wealth gap in the United States? J Econ Issues. 2021;55(2):499–508. [Google Scholar]
- 75. Williams JC, et al. Reopening the United States: Black and Hispanic workers are essential and expendable again. Am J Public Health. 2020;110(10):1506–1508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Hicken MT, et al. “Every shut eye, ain’t sleep”: the role of racism-related vigilance in racial/ethnic disparities in sleep difficulty. Race Soc Probl. 2013;5(2):100–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Cheng P, et al. Efficacy of digital CBT for insomnia to reduce depression across demographic groups: a randomized trial. Psychol Med. 2019;49(3):491–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Liu L, et al. Urban-rural disparities in mental health problems related to COVID-19 in China. Gen Hosp Psychiatry. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Taylor DJ, et al. Insomnia as a health risk factor. Behav Sleep Med. 2003;1(4):227–247. [DOI] [PubMed] [Google Scholar]
- 80. Qaseem A, et al. ; Clinical Guidelines Committee of the American College of Physicians. Management of chronic insomnia disorder in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2016;165(2):125–133. [DOI] [PubMed] [Google Scholar]
- 81. Riemann D, et al. European guideline for the diagnosis and treatment of insomnia. J Sleep Res. 2017;26(6):675–700. [DOI] [PubMed] [Google Scholar]
- 82. Jackson CL, et al. A workshop report on the causes and consequences of sleep health disparities. Sleep. 2020;43(8). doi: 10.1093/sleep/zsaa037 [DOI] [PMC free article] [PubMed] [Google Scholar]