Abstract
Background
vaccination uptake in the UK and increased care home testing are likely affecting care home visitation. With scant scientific evidence to date, the aim of this longitudinal qualitative study was to explore the impact of both (vaccination and testing) on the conduct and experiences of care home visits.
Methods
family carers of care home residents with dementia and care home staff from across the UK took part in baseline (October/November 2020) and follow-up interviews (March 2021). Public advisers were involved in all elements of the research. Data were analysed using thematic analysis.
Results
across 62 baseline and follow-up interviews with family carers (n = 26; 11) and care home staff (n = 16; 9), five core themes were developed: delayed and inconsistent offers of face-to-face visits; procedures and facilitation of visits; variable uptake of the COVID-19 vaccine; misinformation, education and free choice; frustration and anger among family carers. The variable uptake in staff, compared to family carers, was a key factor seemingly influencing visitation, with a lack of clear guidance leading care homes to implement infection control measures and visitation rights differently.
Conclusions
we make five recommendations in this paper to enable improved care home visitation in the ongoing, and in future, pandemics. Visits need to be enabled and any changes to visiting rights must be used as a last resort, reviewed regularly in consultation with residents and carers and restored as soon as possible as a top priority, whilst more education needs to be provided surrounding vaccination for care home staff.
Keywords: dementia, COVID-19, vaccination, social care, care homes, staff, older people, qualitative
Key Points
Variable uptake of vaccination in care home staff was a key factor contributing to enabling visits.
Lack of clear guidance for care homes on managing infection control and visitation rights.
Family carers were angered at being unable to visit their relatives face-to-face despite being vaccinated
Background
Care homes have been affected to the greatest extent by the COVID-19 pandemic, heightened by the fact that residents are most susceptible to the virus. In 2021 alone, over 10,000 care home residents in England have passed away from COVID-19 [1].
There is emerging quantitative evidence on COVID-19 outbreaks in care homes and management of infection risks [2, 3], with a body of research into the effects on health care staff yet limited evidence on the impact on social care staff [4, 5]. In a recent international report by Low-Fay [6], summarising the limited available evidence into the effects of the pandemic on residents, family carers and staff, the authors made strong recommendations for safe visiting to be enabled immediately, to ensure improved well-being for all involved. Social engagement is vital [7], and research into lack of social engagement in the community for people with dementia has already shown detrimental impacts on faster deterioration [8]. The negative impact of lack of social engagement has also been shown in the care home setting [9, 10].
Guidance surrounding care homes and visitation, and infection control, where they are available [11], are changing rapidly. This is particularly the case more recently due to the large vaccination rollout across the UK, with over half of the population vaccinated with a first dose in April 2021. Care home residents and health and social care staff were prioritised in accessing the vaccine, as well as family carers, with reports of reduced vaccination rates among social care staff. A survey into vaccine hesitancy in Liverpool-based care home staff showed that on average only half of care home staff in each care home (51.4%) had been vaccinated, with concerns about lack of vaccine research, misinformation about fertility side effects, and being off-site stated as common reasons for vaccine hesitancy [12]. However, data are based on a survey with only 50% of approached Liverpool-based care homes responding, and are specific to this region within North West England, with no qualitative data to date on vaccination of care home staff across the UK or other countries. This is important to understand, however, as social care staff provide care to some of the most vulnerable members of our society, in particular those groups who are most vulnerable to infection and mortality from COVID-19 [13]. Moreover, there is no research to date showcasing the impact of vaccination rollout and increased testing across care homes and family carers on visitation, whilst we know that testing in care homes proves to be an effective measure of infection control [14].
In March 2021, the government made two announcements and allowed at first one essential visitor into the care home (8th of March), which was followed by a second essential visitor (29th of March). Different countries have different regulations, and in the Netherlands for example, there is a law against blanket care home closures to family and friends. This is also currently being debated in the UK.
The aim of this study was to explore the longitudinal impact of the pandemic on care home visiting rights and the effects of vaccination and testing on visitation. With no evidence to date, this study will provide crucial first findings with potential implications for care home visitation guidance.
Methods
Participants and recruitment
Family carers who have a relative with dementia residing in a care home, and care home staff, were eligible to take part. Participants were included if they were aged 18+ and were residing/working in the UK Initial recruitment took place via advertisement on social media and third sector organisations in October 2020. Participants were purposefully sampled for follow- up interviews in March 2021, in order to gather longer-term experiences of both family carers and the care home workforce, following significant public health changes at that time such as, the COVID-19 vaccination rollout in the UK and a further national lockdown.
Ethical approval was obtained from the University of Liverpool ethics committee (Ref: 7626) prior to study commencement, and an amendment later granted for the follow-up interviews.
Data and data collection
Baseline interviews were conducted between October and November 2020, and follow-up interviews were conducted in March 2021, when vaccinations were ongoing and restrictions were lifted to allow first one, then two visitors into the care home and hold hands using PPE. Figure 1 shows a timeline of care home restrictions in comparison with national changes, whereby it is important to highlight that each nation (England, Wales, Scotland, Northern Ireland) imposed their own restrictions from summer 2020.
Figure 1.
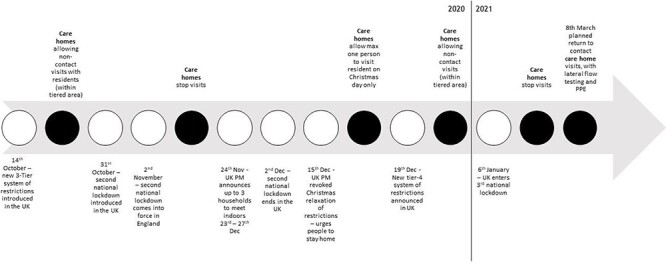
Timeline of UK public health restrictions in the time of COVID-19, from October 2020 to March 2021. White circles indicate UK restrictions, and black circles indicate care home restrictions in response to the public health measures at that time.
We collected basic demographic characteristics of participants including age, gender, ethnicity, as well as relationship with relative with dementia and dementia subtype from family members, and years of working in the care home sector, staff role and size of the care homes from care home staff.
The interview topic guides for baseline and follow-up interviews were co-produced with clinicians, unpaid carers of people living with dementia and academics. Iterations of the topic guide were circulated between team members until a final version was agreed. During baseline interviews, participants were asked about changes to their caring roles since the pandemic, their experiences of viral testing and COVID-19 safety measures employed in the care home, resident visits and communications between family members the care home, and the impact of the restrictions on the staff and residents. Follow-up interview questions centred on changes to participants’ experiences and restriction impacts over time, and included further questions about their experiences of and views about COVID-19 vaccination and vaccine uptake in care home residents and staff and for themselves as carers, as well as changes to visiting arrangements.
Semi-structured, remote interviews were conducted, with participants offered their preferred form of communication (phone or online). Interviews were audio-recorded, with verbal consent obtained and recorded at the beginning of each interview. Audio files were transcribed and in the process anonymised. The average length of interview at baseline was 29 (± 11) minutes, [12–58], and at follow-up was 24 (±7) minutes [13–37].
Data analysis
Transcripts were coded using thematic analysis [15]. Baseline interviews were coded shortly after data collection, and follow-up interviews were coded separately shortly after follow-up data collection. Data saturation was observed in the baseline interviews, and interviews ceased after interview 42. In the follow-up interviews, data saturation was suspected after interview 18, but the following two interviews were honoured as these had already been arranged with the participants, and saturation was confirmed. Using thematic analysis, five research team members all experienced in qualitative analysis, including one former carer trained up in data analysis (JC), coded the transcripts. Specifically, each transcript was coded individually by two research team members before meeting and discussing developing themes and codes. In the first meeting, we had coded three quarters of transcripts and discussed the findings to help with subsequent conceptualisation of themes. After the final analysis meeting, final themes were presented to all team members, highlighting both an inductive and subsequent deductive analysis approach.
Public involvement
Three carers (two former, one current) were active team members and involved in all aspects of the study, from conceptualisation of the project, to designing study documents, helping interpreting findings, and dissemination. One carer was also involved in the analysis of the data. Public advisers were reimbursed according to NIHR INVOLVE guidelines.
Results
We conducted a total of 62 interviews (42 baseline and 20 follow-up interviews). At baseline, 26 family carers and 16 care home staff participated. At follow-up, 11 family carers and 9 care home staff participated. Across all baseline interviewees, the majority were female (n = 31), White British (n = 35) and with a mean age of 54.8 (±15.9). The majority of participants resided in the least disadvantaged quintile (IMD = 1) as reported from their postcode IMD score. Of the 26 family carers recruited, the majority were adult children (n = 16), with the remaining relations spouse or partner. The most common dementia subtype, of the PLWD residing in a care home, was Alzheimer’s (n = 8), followed by Lewy body (n = 6) and vascular (n = 4). Of the 16 care home staff, the mean years of working in a care home was 9.3 (±10.6), with care assistant and manager the most common job roles (n = 4 respectively). All care home staff worked at different care homes, and participants resided across the UK. Table 1 shows the full demographics of the recruited participants in both the baseline and follow-up interviews.
Table 1.
Demographic characteristics of family carers and care home staff
| Family carers baseline (n = 26) | Family carers follow-up (n = 11) | Care home staff baseline (n = 16) | Care home staff follow-up (n = 9) | Total sample (n = 42) | |
|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | N (%) | N (%) | |
| Gender | |||||
| Female Male |
18 (69.2%) 8 (30.8%) |
8 (72.7%) 3 (27.3%) |
13 (81.3%) 3 (18.8%) |
8 (88.9%) 1 (11.1%) |
31 (73.8%) 11 (26.3%) |
| Ethnicity | |||||
| White British White Other BAME Prefer not to say |
22 (84.6%) 2 (7.7%) 2 (7.7%) 0 |
10 (90.9%) 1 (9.1%) 0 0 |
13 (81.3%) 1 (6.3%) 1 (6.3%) 1 (6.3%) |
7 (77.8%) 1 (11.1%) 0 1 (11.1%) |
35 (56.5%) 3 (4.8%) 3 (4.8%) 1 (1.6%) |
| Relationship with PLWD | |||||
| Spouse Partner Adult child |
9 (34.6%) 1 (3.8%) 16 (61.5) |
3 (27.3%) 0 8 (72.7%) |
|||
| Dementia subtype | |||||
| Alzheimer’s disease Mixed dementia Vascular dementia Lewy Body dementia Other Unknown |
8 (30.8%) 2 (7.7%) 4 (15.4%) 6 (23.1%) 2 (7.7%) 4 (15.4%) |
4 (36.4%0 0 2 (18.2%) 4 (36.4%) 1 (9.1%) 0 |
|||
| IMD Quintile2 | |||||
| 1 (least disadvantaged) 2 3 4 5 (most disadvantaged) |
11 (42.3%) 4 (14.5%) 0 3 (11.5%) 1 (3.8%) |
6 (66.7%) 2 (22.2%) 0 0 1 (11.1%) |
3 (23.1%) 3 (23.1%) 3 (23.1%) 1 (7.7%) 3 (23.1%) |
2 (28.6%) 2 (28.6%) 2 (28.6%) 0 1 (14.3%) |
14 (43.8%) 2 (21.9%) 3 (9.4%) 4 (12.5%) 4 (12.5%) |
| Job role | |||||
| Activity Coordinator Care home liaison Care quality Care assistant Senior care assistant Night care assistant Housekeeper Matron Manager |
1 (6.3%) 1 (6.3%) 1 (6.3%) 4 (25.0%) 2 (12.5) 1 (6.3%) 1 (6.3%) 1 (6.3%) 4 (25.0%) |
0 1 (11.1%) 0 3 (33.3%) 0 1 (11.1%) 1 (11.1%) 0 3 (33.3%) |
|||
| Mean (SD), [Range] | |||||
| Age1 | 62.3 (±9.5) [42–89] | 61.1 (±5.2) [51–68] | 41.8 (±16.6) [18–62] | 43.3 (±17.2) [21–60] | 54.8 (±15.9) [18–89] |
| Years of education | 17.9 (±2.9) [11–23] | 18.09 (±1.5) [16–20] | 15.7 (±2.7) [11–20] | 16.4 (±2.6) [11–19] | 17.1 (±3.0) [11–23] |
| Care home capacity | 41.5 (±17.4) [18–76] | 38.9 (±18.2) [18–76] | 42.2 (±15.8) [12–64] | 49.7 (±11.6) [36–64] | 41.7 (±16.6) [12–76] |
| Years working in a care home | 9.3 (±10.6) [1–35] | 7.0 (±11.1) [1–35] | |||
| Years since dementia diagnosis | 6.7 (±3.6) [2–16] | 7.0 (±4.4) [2–16] | |||
| Years (PLWD) residing in a care home | 2.7 (±2.1) [1–10] | 2.8 (±1.9) [1–7] | |||
Qualitative findings
Thematic analysis identified five themes: (i) delayed and inconsistent offers of face-to-face visits; (ii) procedures and facilitation of visits; (iii) variable uptake of the COVID-19 vaccine; (iv) misinformation, education and free choice and (v) frustration and anger in family carers. Table 2 includes key representative quotes from interviews by theme.
Table 2.
Interview quotes by theme
| Theme | Quotes |
|---|---|
| THEME 1: Delayed and inconsistent offers of face-to-face visits | |
| Varied visitation rights |
|
| Individual care home decisions |
|
| Logistical issues |
|
| THEME 2: Procedures and facilitation of visits |
|
|
|
| THEME 3: Variable uptake of the COVID-19 vaccine |
|
| THEME 4: Misinformation, education, and free choice |
|
|
|
| THEME 5: Frustration and anger among family carers |
|
THEME 1: Delayed and inconsistent offers of face-to-face visits
Varied visitation rights
Family carers experienced varied visitation rights, with some carers only visiting briefly before Christmas and a general uncertainty as to when the care homes would resume normal face-to-face visits again (Table 2, quote 1). For many carers, this meant that they had not been able to visit their relative for almost a year, as restrictions had not lifted significantly in some homes since the beginning of lockdown (Table 2, quote 2). Some care homes appeared to be wary of enabling visits waiting for vaccinations to take place protecting everyone as much as possible prior to enabling visits again (Table 2, quote 3).
Individual care home decisions
Each care home appeared to implement the guidance in the way they saw best, with some homes enabling visits and to a greater extent, whilst others were more reluctant to enable visits (Table 2, quotes 4–5). This was reflected in some staff not wanting family carers coming into the home for fear of virus transmission (Table 2, quote 6), albeit some staff themselves had not been vaccinated, thereby increasing the risk of infection transmission. Family carers were thus unable to control visitation, regardless of being vaccinated themselves, and were reliant on each care home to make its own decisions in terms of visitation (Table 2, quote 7).
Logistical issues
Increased testing and other infection control measures, adapting visits and usual working routines, and attending alternative face-to-face visits all add additional workload for care home staff. Staff highlighted the additional demands this places on their time, which results in less ward time to care for residents (Table 2, quote 8). In some care homes, additional staff had been recruited specifically for these COVID-19-related measures, whilst in others staff had to be taken off the ward and could not care for the residents (Table 2, quote 9). This could lead to some care homes being better placed at enabling more visits, whilst others did not have the staff capacity to enable many visits.
THEME 2: Procedures and facilitation of visits
Family carers had mixed experiences surrounding visitation, with alternatives to face-to-face visits not beneficial for all due to dementia- and ageing-related issues of hearing, vision and lack of understanding (Table 2, quote 10). The majority of visits that occurred were alternative face-to-face visits (pod and window visits). Care homes implemented strict testing, PPE, and distancing procedures, and family carers shared the lengthy logistics of visiting their relatives, involving testing ahead of the visit and having to wait outside until the test comes back negative (Table 2, quotes 11–12). Despite adhering to social distancing measures at the time of data collection and before (which changed during the period of data collection), one family carer recounted how her mother with dementia came up to her and hugged her, with the carer appreciating it was against the infection control measures but knowing she had done everything possible to minimise any infection risks (Table 2, quote 12).
The announcement of essential visitor status caused some difficulties for family carers where more than one person wanted to visit the relative at the home face to face. Some carers who were interviewed were not allocated the essential visitor status but their sibling or other relative instead. This could cause issues within the family, particularly when relatives did not speak with one another and were not receiving any information from the one family member who was allowed to visit face-to-face under new guidance (Table 2, quote 13). Compared to pre-pandemic and earlier pandemic experiences, which showed some family support growing amongst relatives, the new announcements caused potential rifts amongst relatives in deciding who was allowed to visit (Table 2, quote 14).
THEME 3: Variable uptake of the COVID-19 vaccine
There was a variable uptake in vaccination between family carers and care home staff. All family carers had been vaccinated, whilst not all staff had or colleagues within the same care home had not been vaccinated. Vaccination was overall also slower in staff, according to family carers, than amidst themselves, who had all been keen to get vaccinated (Table 2, quote 15).
Variations in, and reduced uptake of, vaccination in staff compared to family carers was cause for concern, with some family carers actively questioning why some staff had not been vaccinated (Table 2, quotes 16–17). This was, however, only the case where family carers knew about the rate of staff vaccination at the homes, which often was not the case, showcasing a wider lack of communication between care homes and families (Table 2, quotes 18–19).
THEME 4: Misinformation, education and free choice
Care home staff reported different issues surrounding information about COVID-19 vaccination, with some of their co-workers misinformed about the vaccine. There appeared to be a lack of credible information and sufficient education to fully inform staff about getting vaccinated, with side effects on fertility as well as being microchipped mentioned as reasons for not getting vaccinated (Table 2, quotes 20–22). Misinformation seemed to have spread via social media and the internet more broadly (Table 2, quote 21). Interviewed staff reported, however, that they spoke with their colleagues about misinformation and talked through their concerns, which led some colleagues to get vaccinated in the end, as well as themselves where the participants were initially reluctant to (Table 2, quote 20).
Staff also reported logistical barriers getting vaccinated, with too little notice provided ahead of the date of vaccination, and no alternative offered. In light of some misinformation, these short windows of time seemed to hinder some staff further in accessing the vaccine, albeit the majority of interviewed staff claiming to be vaccinated (Table 2, quotes 23–25).
Another key factor that influenced vaccination uptake amongst care home staff was the communication from their care home manager. Where the manager actively encouraged all staff to get vaccinated through education and open discussions, vaccination rates, according to interviewed staff, appeared to be higher than in homes where managers were not expressing an opinion (Table 2, quote 26).
THEME 5: Frustration and anger among family carers
Family carers were angry and frustrated about the fact that they had not been able to enter care homes and have face-to-face visits with their relative despite being tested, vaccinated and careful about adhering to restrictions. This was aggravated by family carers seeing care home staff sitting next to their relative behind a pod screen or window, in close proximity, without much knowledge as to whether staff had been vaccinated or not. In addition, on each alternative visit, different members of staff could be facilitating the visit sitting close to the resident, thereby again increasing potential infection risk when family carers had often little to no knowledge communicated to them about vaccination of staff. This intensity of emotions from family carers has increased since the baseline interviews in October/November, when vaccinations did not take place, and family carers were rather frustrated. Since then, however, they clearly experienced stronger emotions in March 2021 when followed-up and no or little changes to care home visitation had been implemented despite vaccination and increased testing (Table 2, quote 27).
Some family carers were frustrated as staff tested positively sequentially over prolonged periods of time, leading to care home closures and family carers unable to visit their relatives, and to some extent blaming staff for not being able to enter the care home, whilst family carers themselves were in strict adherence of the regulations (Table 2, quote 28).
Family carers reported empathy and understanding in the earlier baseline interviews, in contrast to the above accounts depicting frustration and exacerbation in response to the unvaccinated care home workforce. This contrast of emotions appears to relate to the persistent COVID-19 outbreaks in homes, and subsequent visiting restrictions, despite the fact that family carers cannot enter the home in any form during the national lockdown. Therefore, the care home staff were viewed as solely responsible for virus transmission, and thus, the reason for persistent lockdown with homes prohibiting contact visits restarting (Table 2, quote 29).
Discussion
This is the first study to have explored the concerns and issues surrounding vaccination and increased testing on care home visitation. Findings showed how visits were often delayed and inconsistent, and subject to various barriers and implementation of guidelines dependant on each care home. The variability in vaccination between staff and family carers appeared to be the biggest barrier of all, and cause of considerable angst for family carers.
There has been no consistent approach to enabling care home visits during this pandemic. Our findings show that due to a lack of clear guidance, each care home interpreted the guidance themselves and made decisions on how and when visits could be enabled. This left some family carers seeing their relatives via alternative face-to-face visits, whilst others were experiencing delays. This was particularly the case with the March announcement of essential visitors being allowed into English care homes, with care homes not having received any communication from the government about these changes in advance. Social contact and enabling family visits are vital to relatives and residents, however, and a human right [16]. As Lee-Fay and colleagues [6] reported in an international overview of care home recommendations in the time of the pandemic, and now corroborated by our findings, safe visiting needs to be enabled. This could be achieved by ensuring double vaccination of family members, testing pre-visit, temperature checking at the care home, as well as adhering to hygiene measures and washing hands (family members and residents) before and after the visit.
Whilst family members were initially (at baseline) more understanding of the situation, albeit upset, the emotional intensity appeared to have changed by follow-up. Family carers were overall frustrated and angry at the strict measures in place for them in terms of visitation, compared to less strict measures on infection control for staff. Family carers were adhering to restrictions and were all vaccinated and willing to test in order to see their relatives as soon as possible. Regardless, the vast majority were only allowed to see their relative behind a window or pod screen, whilst a different member of staff sat close to the relative on each of these alternative face-to-face visits. This was presumably heightened by the consistent lack of communication between care homes and families [11], increasing the emotional upset in family members. The pandemic is having a stark impact on people’s mental well-being already [17, 18], and the inability to visit loved ones can exacerbate low mental well-being in family members, as evidenced in emerging research [9, 10]. Therefore, family carers need to be supported better and considered as vital components in the care and well-being of care home residents. This could be addressed by improved communication between the care home and families, allowing families to have a better insight into the well-being of their relative when visits can be difficult to access, and a more open discussion about the causes of restrictions and balance of risk.
Increased testing and availability of vaccination would be expected to be a facilitator of face-to-face visits. However, variability in vaccine uptake and logistics around planning visits can also act as barriers. There appeared to be misinformation among staff surrounding the consequences and side effects of vaccination. Fertility, microchips and other types of misinformation were raised as concerns, which caused delays in some staff getting the vaccine. Whilst it is beneficial that most staff got vaccinated in the end, any delays in getting vaccinated can cause more time to get infected and to spread the virus, in a population that is one of the most vulnerable in our societies. In addition, this can delay the ability for family carers to visit as infection outbreaks may be more likely. Therefore, to ensure as safe care homes as possible from the virus, and to reduce the tension between family carers and staff by enabling visits, all care home staff should be vaccinated. Ladhani and colleagues [19] for example reported increased infection risk in staff working across multiple care homes. The notion of vaccine hesitancy amongst social care staff is corroborated in a small survey in a small geographical region of the North West of England, reporting vaccine hesitancy in 50% of surveyed care home staff [12]. Equally, lower education in the French working age population has been found to be related to lower vaccine uptake [20]. Whist this showcases that vaccine hesitancy is not restricted to the social care taskforce, and there being a great deal of misinformation surrounding the pandemic in general [21], UK social care staff overall has low educational entry requirements [22], which may be one of the reasons for vaccine hesitancy. However, there are many factors at play, and hesitancy, as indicated by Tulloch et al.’s [12] findings, cannot easily be explained by one single reason. These include ethnicity as well, with people from Black and Pakistani/Bangladeshi minority ethnic backgrounds for example found to be more COVID-19 vaccine hesitant than participants from a White ethnic background in a large longitudinal UK household survey [23]. To overcome the issue of misinformation, more adequate education and information about the vaccines and the benefits need to provided, not just for this but also for future pandemics. In addition, more awareness raising of the benefits of the vaccine in care home staff from minority ethnic backgrounds, as well as trust building and engagement about the vaccine in local community groups [24], may also be suitable avenues to pursue to increase vaccine uptake.
Logistical issues can also provide a barrier to vaccine uptake in care home staff, which in return can impact on decisions about infection control measures in care homes and allowing family members inside. We reported occasions where staff were informed less than an hour before the vaccinations were taking place, which leaves little time for staff to receive proper information about the vaccine and if still unsure, to ask sufficient questions. These difficulties in adequate vaccination rollout contribute to the anger experienced by family carers with fewer staff potentially vaccinated than if there were appropriate timing. This could be overcome by more strategic planning, as well as education and awareness provision from care home managers, with some reported to have been helpful and encouraging the vaccination uptake in this study. This lack of advance notice seems to be supported by a general lack of guidance for care homes, as the announcements of essential visitor rights were equally not communicated to care homes in advance. This strongly highlights the general lack of communication and support from decision makers in managing infection control in the care home settings, so that care homes have to rely on their own judgements. Preliminary findings by Marshall et al. [25] corroborate how care homes were left without much support and instead often supported themselves and received support from their communities.
Based on these novel findings, we make five specific recommendations for the care home sector, to the benefit of staff, family carers and residents:
Face-to-face visits are a human right and the right to see loved ones should only ever be removed as a last resort, regularly reviewed in consultation with residents and carers and restored as a high priority as soon as possible.
Support for care homes for the effective implementation of infection control measures and access to personal protective equipment alongside health staff, to avoid taking staff time away from caring for residents and leading to stopping visits as a default, lower cost, protective response.
Need for better information support and guidance surrounding vaccination for all involved and improved logistical processes for vaccine delivery.
General need for better guidance and communication to support care home staff in their work delivery and communication between care homes and families.
Vaccination of social care staff should be mandatory.
Whilst this study benefits from having captured the precise moment when visitation restrictions were officially eased for care homes in England, and being the first study to explore the impact of heightened infection control measures (testing, vaccination) on care home visitation, there were some limitations. This longitudinal study only interviewed family members of care home residents and care home staff, thereby only collecting some proxy information on how people with dementia residing in the care homes were faring. Considering pandemic restrictions of not collecting data in care homes, as well as the difficulty of obtaining experiential data from people who mostly lack capacity to consent, given their advanced dementia, this was the most feasible way of collecting data. Further research needs to explore impact of restrictions on residents’ well-being and functioning, which can be achieved via quantitative measurements. A positive of the sample is the fact that staff were recruited from 16 different care homes across the UK, thus broadening the representativeness of care home experiences. Additionally, our sample was lacking ethnic minority representation, and mostly included family carers and staff from a White ethnic background. In light of increased susceptibility of people from minority ethnic backgrounds to the virus [13], future research needs to explore their views, as ethnicity may affect behaviour and attitudes towards infection control measures and visitation.
Conclusions
This study provides the first insights into how increased infection control measures (testing and vaccination) and concerns surrounding these have affected care home visitation. The lack of social contact with relatives has been detrimental to family members, with our findings providing strong evidence-based recommendations for the continued handling of the COVID-19 pandemic going forward, as well as for other future infection outbreaks. With voices emerging on implementing a law to enable social contact with loved ones for residents, this study supports this notion, whilst more in-depth research is required on the precise impacts of residents from their points of views.
Acknowledgements
We wish to thank all family carers and care home staff who took part in this study, and we also wish to thank the many family carers who expressed an interest to take part after we were already booked up. We also wish to thank Maxine Martine and Lynne McClymont for transcribing the audio files very swiftly to analyse the data in time.
Contributor Information
Clarissa Giebel, Department of Primary Care and Mental Health, University of Liverpool, Liverpool, UK; NIHR ARC NWC, Liverpool, UK.
Kerry Hanna, Department of Primary Care and Mental Health, University of Liverpool, Liverpool, UK; NIHR ARC NWC, Liverpool, UK.
Jacqueline Cannon, Lewy Body Society, Wigan, UK.
Paul Marlow, NIHR ARC NWC, Liverpool, UK.
Hilary Tetlow, NIHR ARC NWC, Liverpool, UK.
Stephen Mason, Palliative Care Unit, University of Liverpool, Liverpool, UK.
Justine Shenton, Sefton Advocacy, Liverpool, UK.
Manoj Rajagopal, Lancashire and South Cumbria NHS Trust, Preston, UK.
Mark Gabbay, Department of Primary Care and Mental Health, University of Liverpool, Liverpool, UK; NIHR ARC NWC, Liverpool, UK.
Declaration of Conflict of interest
None.
Declaration of Sources of Funding
This study was funded by the Geoffrey and Pauline Martin Trust, with funding awarded to the principal investigator. This is also independent research funded by the National Institute for Health Research Applied Research Collaboration North West Coast (ARC NWC). The views expressed in this publication are those of the author(s) and not necessarily those of the National Institute for Health Research or the Department of Health and Social Care.
References
- [1]. Office for National Statistics (ONS) 2021. Dataset: Number of Deaths in Care Homes Notified to the Care Quality Commission, Office for National Statistics, England. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/datasets/numberofdeathsincarehomesnotifiedtothecarequalitycommissionengland (18 May 2021, date last accessed). [Google Scholar]
- [2]. Burton JK, Bayne G, Evans C et al. Evolution and effects of COVID-19 outbreaks in care homes: a population analysis in 189 care homes in one geographical region of the UK. Lancet Healthy Longevity 2020; 1: 21–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3]. Burton JK, Reid M, Gribben C et al. Impact of COVID-19 on care home mortality and life expectancy in Scotland. Age Ageing 2021. 10.1093/ageing/afab080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4]. De Kock JH, Latham HA, Leslie SJ et al. A rapid review of the impact of COVID-19 on the mental health of healthcare workers: implications for supporting psychological well-being. BMC Public Health 2021; 21: 104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5]. Hanna JR, Rapa E, Dalton LJ et al. Health and social care professionals’ experiences of providing end of life care during the COVID-19 pandemic: a qualitative study. Palliat Med 2021. 10.1177/2F02692163211017808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6]. Low-Fay L, Hinsliff-Smith K, Sinha S et al. Safe visiting at care homes during COVID-19: a review of international guidelines and emerging practices during the COVID-19 pandemic. Int J Long-Term Care 2021. https://ltccovid.org/wp-content/uploads/2021/01/Care-home-visiting-policies-international-report-19-January-2021-1.pdf. [Google Scholar]
- [7]. Sommerlad A, Sabia S, Singh-Manoux A, Lewis G, Livingston G. Association of social contact with dementia and cognition: 28-year follow-up of the Whitehall II cohort study. PLoS Med 2019. 10.1371/journal.pmed.1002862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8]. Giebel C, Cannon J, Hanna K et al. Impact of COVID-19 related social support service closures on people with dementia and unpaid carers: a qualitative study. Aging Ment Health 2020. 10.1080/13607863.2020.1822292. [DOI] [PubMed] [Google Scholar]
- [9]. Ayalon L, Avidor S. ‘We have become prisoners of our own age’: from a continuing care retirement community to a total institution in the midst of the COVID-19 outbreak. Age Ageing 2021. 10.1093/ageing/afab013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10]. Van der Roest HG, Prins M, van der Velden C et al. The impact of COVID-19 measures on well-being of older long-term care facility residents in the Netherlands. JAMDA 2020; 21: 1569–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11]. Giebel C, Hanna K, Cannon J et al. Taking the ‘care’ out of care homes: the moral dilemma of institutional long-term care provision during COVID-19. Health Soc Care Community (revisions submitted). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12]. Tulloch JSP, Lawrenson K, Gordon AL et al. COVID-19 vaccine hesitancy in care home staff: a survey of Liverpool care homes. MedRxiv preprint 2021. 10.1101/2021.03.07.21252972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13]. Daras K, Alexiou A, Rose TC et al. How does vulnerability to COVID-19 vary between communities in England? Developing a small area vulnerability index (SAVI). J Epidemiol Community Health 2021. 10.1136/jech-2020-215227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14]. Micocci M, Gordon AL, Seo MK et al. Is point-of-care testing feasible and safe in care homes in England? An exploratory usability accuracy evaluation of a point-of-care polymerase chain reaction test for SARS-COV-2. Age Ageing 2021. 10.1093/ageing/afab072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15]. Braun V, Clarke C. Using thematic analysis in psychology. Qual Res Psychol 2006; 3: 77–101. [Google Scholar]
- [16]. Butchard S, Kinderman P. Human rights, dementia, and identity. Eur Psychol 2019; 24: 159–68. [Google Scholar]
- [17]. Fancourt D, Steptoe A, Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiatry 2021; 8: 141–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18]. Hanna K, Giebel C, Tetlow H et al. Emotional and mental wellbeing following COVID-19 public health measures on people living with dementia and carers. J Geriatr Psychiatry Neurol 2021. 10.1177/2F0891988721996816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19]. Ladhani SN, Chow JY, Janarthanan R et al. Increased risk of SaRS-CoV-2 infection in staff working across different care homes: enhanced COVID-19 outbreak investigations in London care homes. J Infect 2020; 81: 621–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20]. Schwarzinger M, Watson V, Arwidson P, Alla F, Luchini S. COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. Lancet Public Health 2021; 6: E210–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21]. Green M, Musi E, Rowe F et al. Identifying how COVID-19-related misinformation reacts to the announcement of the UK national lockdown: an interrupted time-series study. Big Data Soc 2021. 10.1177/2F20539517211013869. [DOI] [Google Scholar]
- [22]. House of Commons Committee of Public Accounts . The Adult Social Care Workforce in England. House of Commons, London, England: 2018. https://publications.parliament.uk/pa/cm201719/cmselect/cmpubacc/690/690.pdf [Google Scholar]
- [23]. Robertson E, Reeve KS, Niedzwiedz CL et al. Predictors of COVID-19 vaccine hesitancy in the UK household longitudinal study. Brain Behav Immun 2021; 94: 41–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24]. Razai MS, Osama T, McKechnie DGJ. COVID-19 vaccine hesitancy among ethnic minority groups. BMJ 2021; 372: N513. [DOI] [PubMed] [Google Scholar]
- [25]. Marshall F, Gordon A, Gladman JRF, Bishop S. Care homes, their communities, and resilience in the face of the COVID-19 pandemic: interim findings from a qualitative study. BMC Geriatr 2021; 21: 102. [DOI] [PMC free article] [PubMed] [Google Scholar]


