Abstract
Background
The combination of sofosbuvir and daclatasvir has shown preliminary efficacy for hospitalized patients with COVID-19 in four open-label studies with small sample sizes. This larger trial aimed to assess if the addition of sofosbuvir/daclatasvir to standard care improved clinical outcomes in hospitalized patients with COVID-19.
Methods
This was a placebo-controlled, double-blind, randomized clinical trial in adults hospitalized with COVID-19 at 19 hospitals in Iran. Patients were randomized to oral sofosbuvir/daclatasvir 400/60 mg once-daily or placebo in addition to standard of care. Patients were included if they had positive PCR or diagnostic chest CT, O2 saturation <95% and compatible symptoms. The primary outcome was hospital discharge within 10 days of randomization. Secondary outcomes included mortality and time to clinical events. The trial is registered on the Iran Registry of Clinical Trials under IRCT20200624047908N1.
Results
Between July and October 2020, 1083 patients were randomized to either the sofosbuvir/daclatasvir arm (n = 541) or the placebo arm (n = 542). No significant difference was observed in the primary outcome of hospital discharge within 10 days, which was achieved by 415/541 (77%) in the sofosbuvir/daclatasvir arm and 411/542 (76%) in the placebo arm [risk ratio (RR) 1.01, 95% CI 0.95–1.08, P = 0.734]. In-hospital mortality was 60/541 (11%) in the sofosbuvir/daclatasvir arm versus 55/542 (10%) in the placebo arm (RR 1.09, 95% CI 0.77–1.54, P = 0.615). No differences were observed in time to hospital discharge or time to in-hospital mortality.
Conclusions
We observed no significant effect of sofosbuvir/daclatasvir versus placebo on hospital discharge or survival in hospitalized COVID-19 patients.
Introduction
As the incidence and mortality of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic continues to rise globally, few therapeutic options are recommended for the treatment of symptomatic disease.1
A strategy for tackling this fast-moving pandemic is repurposing existing antivirals or immunomodulators that could be used to treat COVID-19. This strategy takes advantage of established safety profiles and the availability of existing pharmaceuticals. Of the repurposed antivirals that have been investigated, remdesivir showed initial promise, but has since shown little overall clinical benefit and the WHO no longer recommends it for use.2 Various other repurposed antivirals have drawn attention, such as nitazoxanide and lopinavir/ritonavir, but these have not shown a robust clinical benefit and are not recommended for use.1,3 Of immunomodulators, the corticosteroid treatment dexamethasone has been approved for treatment since it was found to reduce mortality in hospitalized patients, but does not have antiviral properties and is effective only at reducing the inflammation of patients with high disease severity.4 Tocilizumab, another immunomodulator, has shown significant survival benefit in the REMAP-CAP and RECOVERY trials.5,6
Sofosbuvir and daclatasvir have been investigated for use against SARS-CoV-2.7–12 Sofosbuvir and daclatasvir are available in a combination tablet and are approved for the treatment of hepatitis C virus, inhibiting viral replication.13,14 In computer models, these direct-acting antivirals have been predicted to be effective inhibitors of enzymes needed for SARS-CoV-2 replication.15–18 In vitro evidence for sofosbuvir activity against SARS-CoV-2 is mixed. Initial studies were negative in certain cell lineages,19–21 but sofosbuvir has been shown to be effective when tested in human cells with the necessary enzymes to convert sofosbuvir into its active form.22 However, the current available dosage of sofosbuvir (400 mg) was not sufficient to inhibit SARS-CoV-2 in vitro.23 Daclatasvir has shown activity against SARS-CoV-2 in vitro and evidence suggests the available dosage form of 60 mg is sufficient to inhibit replication.24,25
In early 2020 there were four small clinical trials in a total of 265 patients that evaluated the efficacy of sofosbuvir/daclatasvir in combination with other antivirals, such as lopinavir/ritonavir, hydroxychloroquine and ribavirin, in hospitalized patients with COVID-19.7–9,12 Results from these four trials were encouraging. Three have been analysed together in a pooled meta-analysis, showing that mortality and time to hospital discharge was slightly improved in patients receiving sofosbuvir/daclatasvir compared with standard of care.10 Despite promising results, the quality of these studies is variable based on small sample sizes, differences in endpoints and comparison arms, and other potential biases, such as lack of randomization or their open-label nature.
Here, we build on these studies by reporting the results of a large, randomized, placebo-controlled trial to test whether sofosbuvir/daclatasvir is an effective treatment for hospitalized patients with COVID-19.
Methods
Study design and patients
DISCOVER (DaclatasvIr and Sofosbuvir for COVid-19 in hospital Emergency Room) was a 1:1 randomized, double-blind, placebo-controlled, multicentre study in 19 hospitals in Iran across 12 cities. The study was conducted according to the Declaration of Helsinki and Iran Ministry of Health requirements for clinical trials and was approved by the Abadan Faculty of Medicine Sciences Institutional Review Board and the Iranian Registry of Clinical Trials (IRCT) registry team. The study protocol is registered with IRCT under IRCT20200624047908N1 available at https://www.irct.ir/trial/49198.
Hospitalized patients with clinically diagnosed COVID-19 by either PCR positivity or COVID-19-compatible chest CT scan findings were considered for inclusion if they were >18 years old and provided written informed consent. Individuals were required to have an oxygen saturation <95% and at least one symptom of fever (oral temperature ≥37.8°C), dry cough, severe fatigue or dyspnoea. Patients were excluded if they had renal failure, were pregnant or breastfeeding, had multi-organ failure or required intubation on admission, had significant arrhythmias, were on amiodarone, had previous sofosbuvir use for current infection or were allergic to sofosbuvir/daclatasvir. Participants enrolled in other interventional trials were also excluded.
The original inclusion criteria were more restrictive and included only participants with onset of symptoms ≤7 days and those <75 years. Participants with previous COVID-19 infection, severe physical disability, active cancer, immune suppression, immune compromisation and previous or current use of experimental COVID-19 medicine were excluded. In the first week of the study, the enrolment rate was too low so these exclusion criteria were removed.
Randomization and intervention
Block randomization was done using a computer-generated list with 1:1 allocation and a block size of four. Randomization and preparation of study medication were performed centrally and blocks were distributed among participating centres. None of the researchers, treating physicians or participants was aware of the participant group allocation throughout the duration of the trial.
Eligible and consenting participants were randomized to receive either standard of care plus sofosbuvir/daclatasvir 400/60 mg (Sovodak, RojanPharma, Tehran) or standard of care plus placebo. Sofosbuvir/daclatasvir or placebo were administered orally, once daily for 10 days. The sofosbuvir/daclatasvir and placebo were in tablet form, identical in appearance and were pre-packed in bottles of 10 tablets. Standard of care was administered following national treatment guidelines, which varied throughout the study and included concomitant use of interferon-β, dexamethasone (or other corticosteroids), lopinavir/ritonavir and other therapeutic agents.
Procedures
All patients admitted to participating hospitals with a clinical diagnosis of COVID-19 were evaluated for eligibility. Patients meeting the eligibility criteria and consenting to the study were randomized and received the first dose of study medication within 48 h of admission. Patients were visited daily and relevant information and complications or adverse events were recorded. Only complications leading to discontinuation of medicine or adverse events thought to be due to the study medicine were reported. All data were entered into an online system within 48 h and were checked for consistency and errors by a central team.
If patients were discharged earlier than 10 days, they were be instructed to continue the study medication to complete the 10 day course. All participants were contacted 14 days after discharge to ask about compliance, possible re-admission and late complications. If individuals were not able to be contacted at the 14 day post-discharge visit, efforts were taken to ascertain whether the participants were still alive or had died during this period.
Outcome measures
The primary endpoint was hospital discharge within 10 days after randomization where participants were discharged on the managing physician’s decision based on the absence of fever or dyspnoea, no or improved cough and fatigue, and tolerance of oral feeding, with a stable O2 saturation of ≥95%. During the first 2 weeks of the study, it became clear that the ≥95% O2 saturation criterion for clinical recovery and subsequent discharge was not possible to enforce due to shortages of hospital beds. As such, at the beginning of the third week of the study this final criterion was removed. Some individuals self-discharged from hospital (i.e. discharged without physician consent). For these individuals, the same criteria were used to assess whether individuals met the primary outcome using results from their last day of hospitalization.
Secondary endpoints were hospital discharge within 14 days of randomization, time to hospital discharge, mortality and days of intubation. For mortality we consider two outcomes: in-hospital mortality (i.e. follow-up ceased at hospital discharge) and overall mortality (i.e. including individuals who died during the 14 day post-discharge follow-up). Time-to-event outcomes (hospital discharge and in-hospital mortality) were assessed up to day 14 after discharge.
The original secondary endpoints included days admitted in the ICU. Because of the shortage of ICU beds in many participating hospitals throughout the study, this endpoint would not have carried reliable information and was removed.
Statistical analysis
The sample size was calculated to detect a 10 percentage point increase in the primary outcome of hospital discharge by day 10 based on an expected proportion of 70% in the control arm. To provide at least 95% power with a two-sided 5% significance level, it was determined that 500 patients should be allocated to each arm (total 1000 patients). No interim analyses were planned.
Treatment arms were compared for the intent-to-treat population including all randomized patients. Descriptive statistics were used to summarize baseline characteristics. For the primary endpoint, all individuals who were discharged within 10 days were considered an event, including individuals self-releasing from hospital who met the recovery criteria. The proportion of patients achieving the outcome was tabulated by treatment arm as the count and proportion and was compared using risk ratios (RRs) and their corresponding 95% CI. Dichotomous secondary outcomes were analysed in the same manner as the primary outcome. A summary of participant clinical status at day 10 is provided using counts and percentages. Days of intubation was described using descriptive statistics in participants experiencing intubation.
Time-to-event endpoints of day 28 hospital discharge and in-hospital mortality were analysed using Kaplan–Meier survival curves. Treatment groups were compared using the log-rank test. For 28 day hospital discharge, individuals who died during hospitalization were censored on day 29 after randomization to indicate they did not have an improvement and give an unbiased estimate of discharge rate. For 28 day in-hospital mortality, patients discharged prior to day 28 were assumed to have survived until after 28 days after randomization. Both analyses censored patients self-discharging or with withdrawal of consent at day of exit. Analyses considered only the original episode of hospitalization and any hospital readmissions or deaths after the initial hospitalization were not captured.
Post-hoc subgroup analyses of the primary outcome were carried out for key predictors. These were gender, age (<60 years versus ≥60 years), presence or absence of any comorbidities, time since symptom onset (≤4 days versus >4 days and ≤8 days versus >8 days), baseline O2 saturation (≤90% versus >90%), baseline PCR positivity and use of concomitant dexamethasone. These analyses were restricted to participants with non-missing subgroup data for the variable of interest and comparison between groups was done using the χ2 test. Findings from this analysis should be considered exploratory.
A P value was considered statistically significant at the P < 0.05 threshold. Data were analysed using Stata (version 16.1) by two separate independent analysts for quality control purposes.
Results
Patient characteristics
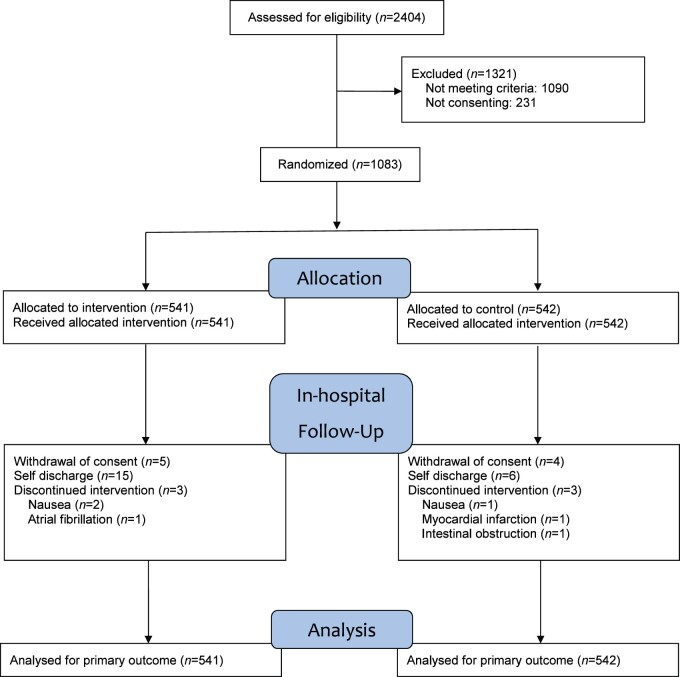
Between July and October 2020, 2404 participants were screened for eligibility and, of these participants, 1090 were not eligible (Table S1, available as Supplementary data at JAC Online). The primary reason for ineligibility was an oxygen saturation ≥95% (67%; 728/1090). Of the 1314 eligible patients, 231 did not consent to the study and, finally, 1083 participants were enrolled and included in the intent-to-treat population: 541 were randomized to the sofosbuvir/daclatasvir group and 542 to the placebo group (Figure 1).
Figure 1.
Participant flow diagram. This figure appears in colour in the online version of JAC and in black and white in the print version of JAC.
Patients in the sofosbuvir/daclatasvir and placebo groups were generally well balanced at the time of randomization (Table 1). The median age of participants was 58 years (IQR 45–69); 585 (54%) patients were men versus 498 (46%) women. The most frequent comorbidities observed were hypertension (34%) and diabetes (28%). Baseline laboratory findings and vitals were balanced across treatment arms. The median time since symptom onset was 8 days (IQR 6–10) for both groups. Overall, 79% of patients had PCR-confirmed SARS-CoV-2; all participants had CT lung involvement. At randomization, most individuals were not receiving additional oxygen (74%); 25% were receiving nasal oxygen.
Table 1.
Baseline characteristics
| Sofosbuvir/daclatasvir (N = 541) | Control (N = 542) | |
|---|---|---|
| Baseline demographics | ||
| age (years), median (IQR) | 57 (45–69) | 59 (46–69) |
| sex (female), n (%) | 250 (46) | 248 (46) |
| BMI (kg/m2), median (IQR) | 27 (24–31) | 27 (24–30) |
| Vitals on admission, median (IQR) | ||
| oxygen saturation (%) | 90 (88–93) | 90 (87–93) |
| respiratory rate (breaths/min) | 20 (18–23) | 20 (18–23) |
| temperature (°C) | 37 (36.7–37.5) | 37 (36.8–37.5) |
| Comorbidities, n (%) | ||
| hypertension | 187 (35) | 181 (34) |
| diabetes | 153 (28) | 146 (27) |
| ischaemic heart disease | 53 (10) | 46 (8) |
| asthma | 28 (5) | 24 (4) |
| COPD | 9 (2) | 14 (3) |
| COVID-19 diagnosis | ||
| PCR positive, n (%) | 430 (79) | 426 (79) |
| CT lung involvement percentage categories, n (%)a | ||
| 0–25 | 94 (17) | 85 (16) |
| 26–50 | 267 (49) | 293 (54) |
| 51–75 | 138 (26) | 123 (23) |
| 76–100 | 42 (8) | 41 (8) |
| days since symptom onset, median (IQR)b | 8 (6–10) | 8 (6–10) |
| Laboratory findings, median (IQR) | ||
| white blood cells (/μL) | 5900 (4500–8400) | 5900 (4400–8640) |
| neutrophils (%) | 75 (67–83) | 74 (65–82) |
| lymphocytes (%) | 18 (11.5–25.2) | 19 (12.4–26.0) |
| absolute lymphocyte count (/μL) | 1013 (740–1425) | 1068 (767–1412) |
| c-reactive protein (mg/L) | 36 (20–63) | 36 (20–62) |
| Oxygenation status, n (%)c | ||
| room air | 397 (73) | 408 (75) |
| nasal oxygen | 143 (26) | 133 (25) |
| intubated | 1 (0.2) | 1 (0.2) |
Baseline characteristics were obtained at screening unless otherwise stated.
All individuals had CT involvement.
Reported is the day to randomization since first symptoms.
Oxygen status reported was that at randomization. No individuals were intubated at hospital admission as per the eligibility criteria.
The most frequent concomitant medications administered as part of standard of care were interferon-β (54%), dexamethasone (53%), lopinavir/ritonavir (33%) and remdesivir (16%). Concomitant medication administration was balanced across treatment arms (Table 2). Study medication was discontinued prematurely in six patients (three in each arm); two of these cases were considered to be due to study medication (one in each arm).
Table 2.
Concomitant medications administered as standard of care
| Concomitant medications | Sofosbuvir/daclatasvir (N = 541), n (%) | Control (N = 542), n (%) |
|---|---|---|
| Interferon-β | 293 (54) | 291 (54) |
| Dexamethasone | 298 (55) | 272 (50) |
| Other corticosteroids | 93 (17) | 94 (17) |
| Lopinavir/ritonavir | 176 (33) | 183 (34) |
| Azithromycin | 121 (22) | 119 (22) |
| Remdesivir | 93 (17) | 76 (14) |
| Hydroxychloroquine | 70 (13) | 69 (13) |
| Atazanavir | 60 (11) | 57 (10) |
| Naproxen | 44 (8) | 52 (10) |
| Intravenous immunoglobulin | 5 (1) | 2 (0) |
| Ribavirin | 4 (1) | 0 (0) |
Primary outcome
Results for the primary outcome of hospital discharge within 10 days are shown in Table 3. The primary outcome was achieved by 415/541 (77%) participants in the sofosbuvir/daclatasvir group and 411/524 (76%) in the placebo group. There was no significant difference between treatment arms (RR 1.01, 95% CI 0.95–1.08, P = 0.734).
Table 3.
Primary and secondary outcomes
| Sofosbuvir/daclatasvir (N = 541) | Control (N = 542) | RR (95% CI) | P | |
|---|---|---|---|---|
| Primary outcome, n (%) | ||||
| hospital discharge within 10 days | 415 (77) | 411 (76) | 1.01 (0.95–1.08) | 0.734 |
| Secondary outcomes, n (%) | ||||
| hospital discharge within 14 days | 435 (80) | 448 (83) | 0.97 (0.92–1.03) | 0.340 |
| in-hospital mortalitya | 60 (11) | 55 (10) | 1.09 (0.77–1.54) | 0.615 |
| overall mortalityb | 71 (13) | 62 (11) | 1.15 (0.83–1.58) | 0.399 |
Includes deaths at any point during the initial hospitalization; follow-up ceased at hospital discharge.
Includes deaths at any point during the study including the initial hospitalization through the day 14 post-discharge visit.
At day 10, in the sofosbuvir/daclatasvir arm, 415 (77%) had been discharged, 34 (6%) had died, 13 (2%) were intubated, 62 (11%) were on nasal or room air and the remaining 17 (3%) had either self-discharged from hospital or withdrawn consent without meeting recovery criteria. Results were similar in the placebo arm; 411 (76%) had been discharged, 34 (6%) had died, 10 (2%) were intubated, 78 (14%) were on nasal or room air and the remaining 9 (2%) had self-discharged or withdrawn consent.
In subgroup analyses of the primary outcome there were no differences between treatment arms by sex, age, presence of comorbidities, time since symptom onset, oxygen saturation at baseline, baseline PCR positivity and concomitant dexamethasone use (Table 4).
Table 4.
Subgroup analysis of the primary outcome
| Sofosbuvir/daclatasvir (N = 541), n/n (%) | Control (N = 542), n/n (%) | P | |
|---|---|---|---|
| Men | 220/291 (76) | 224/294 (76) | 0.962 |
| Women | 185/250 (78) | 187/248 (75) | 0.716 |
| Patients ≥60 years old | 170/248 (69) | 184/266 (69) | 0.891 |
| Patients <60 years old | 245/293 (84) | 227/276 (82) | 0.783 |
| Any comorbiditya | 215/285 (75) | 203/279 (73) | 0.469 |
| No comorbidity | 200/256 (78) | 208/263 (79) | 0.6474 |
| Days since symptom onset >4 days | 320/422 (76) | 321/422 (76) | 0.936 |
| Days since symptom onset ≤4 days | 95/119 (80) | 90/120 (75) | 0.372 |
| Days since symptom onset >8 days | 109/140 (78) | 121/148 (82) | 0.443 |
| Days since symptom onset ≤8 days | 306/401 (76) | 290/394 (74) | 0.473 |
| Patients with O2 saturation >90% at baseline | 214/254 (84) | 215/257 (84) | 0.984 |
| Patients with O2 saturation ≤90% at baseline | 201/287 (70) | 196/285 (69) | 0.705 |
| PCR positive at baseline | 326/430 (76) | 315/426 (74) | 0.529 |
| PCR negative at baseline | 89/111 (80) | 96/116 (83) | 0.444 |
| Taking dexamethasone | 220/298 (74) | 184/272 (68) | 0.105 |
| Not taking dexamethasone | 195/243 (80) | 227/270 (84) | 0.257 |
P value calculated using χ2 test.
Any comorbidity defined as those with any of hypertension, diabetes, ischaemic heart disease, COPD or asthma.
Secondary outcomes
No statistically significant differences were observed for hospital discharge within 14 days of randomization (RR 0.97, 95% CI 0.92–1.03, P = 0.340; Table 3). Figure 2 shows the 28 day probability of hospital discharge. The median time to discharge was 7 days (IQR 4–10) in the sofosbuvir/daclatasvir group and 6 days (IQR 4–10) in the placebo group. There were no significant differences between groups (P = 0.456). Overall, 48 (9%) individuals in the sofosbuvir/daclatasvir arm were intubated for a median duration of 5 days (IQR 2–9). In the placebo arm, 44 (8%) individuals were intubated for a median of 4 days (IQR 1–8). Of those intubated 90% (83/92) died during hospitalization.
Figure 2.
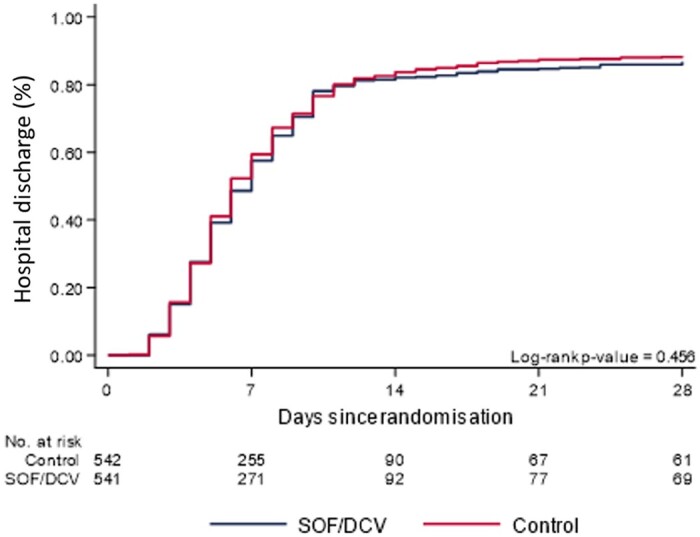
Kaplan–Meier graph of the 28 day probability of hospital discharge. SOF/DCV, sofosbuvir/daclatasvir. This figure appears in colour in the online version of JAC and in black and white in the print version of JAC.
When considering mortality, there were no significant differences between treatment arms for both in-hospital mortality and overall mortality. During the initial hospitalization, there were 60 (11%) deaths in the sofosbuvir/daclatasvir group and 55 (10%) in the control group (P = 0.615). Deaths increased to 71 (13%) and 62 (11%) in the sofosbuvir/daclatasvir and placebo arms, respectively, when considering the 14 day post-discharge follow-up (P = 0.399). Figure 3 shows the Kaplan–Meier plots for the probability of 28 day in-hospital mortality; no significant difference between groups was observed (P = 0.646).
Figure 3.
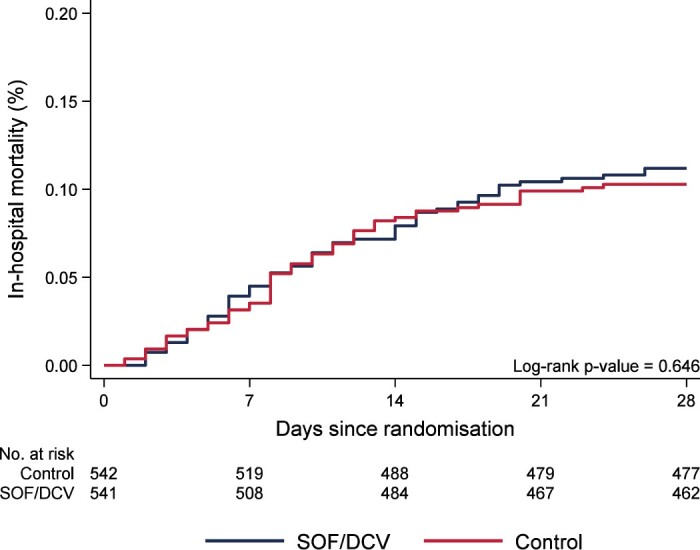
Kaplan–Meier graph of the 28 day probability of in-hospital mortality. SOF/DCV, sofosbuvir/daclatasvir. This figure appears in colour in the online version of JAC and in black and white in the print version of JAC.
The treating physicians reported four cases of nausea that they believed were due to the study medication, two in the control group and two in the sofosbuvir/daclatasvir group. One in each group led to discontinuation of medicine. In four other patients the study medication was discontinued although the conditions were not considered to be related to the study medicine by the managing physician. These included one case each of myocardial infarction, intestinal obstruction, atrial fibrillation and nausea; all in the sofosbuvir/daclatasvir group.
Discussion
This trial was a large, double-blind, placebo-controlled, randomized trial designed to evaluate the efficacy of a 10 day course of sofosbuvir/daclatasvir for the treatment of COVID-19. In a total of 1083 patients with COVID-19 infection requiring hospitalization, there was no significant effect of sofosbuvir/daclatasvir versus placebo on hospital discharge or survival. These results were consistent across different subgroups of age, sex, time since onset of symptoms, comorbidities, concomitant medications and baseline vitals.
The results from this double-blind randomized trial are not consistent with earlier clinical trials of sofosbuvir/daclatasvir.7–9,12 In a combined analysis of the four earlier randomized trials and the DISCOVER results presented here, there is no significant benefit associated with sofosbuvir/daclatasvir on hospital discharge (Figure S1). The four earlier trials conducted in Iran and Egypt had a total sample size of 265 patients compared with 1083 patients in the DISCOVER trial. Additionally, all of these trials were open-label and as a result investigator bias may have contributed to the positive result.
Daily doses used in the current trial were selected based on their availability for treatment of hepatitis C and the proven safety and tolerability profile.13,14 Although sofosbuvir and daclatasvir have shown some benefit in reducing viral replication in vitro, the EC50 for sofosbuvir 60 mg is not within pharmacokinetic exposures and the daclatasvir 400 mg EC50 is borderline.23,25 In this trial a large proportion of participants received dexamethasone and other corticosteroids, a drug which has shown survival benefit in patients with severe COVID-19.4 However, dexamethasone moderately decreases daclatasvir exposure as it is a moderate CYP3A inducer.26 Therefore, pharmacokinetic levels of sofosbuvir/daclatasvir may not be high enough to provide efficacy. Future trials should investigate sofosbuvir/daclatasvir at higher doses and without the use of drugs that could lower their concentration. Further, antivirals could also be assessed in combination with other treatments, such as nitazoxanide3 or ivermectin,27 which have shown some promise in small clinical trials.
In DISCOVER, individuals were hospitalized with a median time since symptom onset of 8 days. This may be too far into the course of disease for antivirals such as sofosbuvir/daclatasvir to be effective. Evidence suggests that antivirals show little benefit in late-stage disease. For example, the influenza drug oseltamivir shows the greatest efficacy in the early stages of the disease.28 Treatment trials could adopt a same-day-test-and-treat model wherever possible to ensure that investigational treatments are able to suppress the virus as soon as possible. Further, trials could be aimed at earlier stages of disease, with the aim of preventing hospitalization, such as the clinical trials of budesonide and monoclonal antibody targets for early COVID-19 infection.29,30
The DISCOVER study was performed in a period in Iran in which the epidemic burden was large and the pressure on health systems was great. This could have implications for the population that was able to be enrolled and followed up and for the generalizability of results. Individuals were encouraged to stay at home unless they developed severe symptoms and only the most severe patients were admitted to hospitals. For example, the median oxygen saturation at baseline was 90% in both arms. Additionally, due to lack of hospital capacity, patients who were deemed well enough were discharged quickly and some patients self-discharged once they felt better against the recommendation of their doctors.
Further limitations of this trial include the dichotomization of the primary outcome, possibly leading to loss of information. This was addressed by performing survival analysis of hospital discharge and mortality. Furthermore, a block size of four was used in the randomization process, which could increase the risk of investigators predicting allocation. Finally, adaptions to the eligibility criteria and outcome ascertainment were necessary due to the burden of COVID-19 on the health system and to ensure a sufficient recruitment rate. The adaptions could result in biases in the trial, but were unlikely to have affected the groups differentially and did not affect trial blinding.
In summary, in the DISCOVER trial among adults hospitalized with COVID-19, there was no significant clinical benefit of sofosbuvir/daclatasvir compared with placebo. These findings do not support the use of sofosbuvir/daclatasvir at the available dosage for the treatment of late-stage COVID-19 disease. Future trials of sofosbuvir/daclatasvir could consider using higher doses and be administered in combination with other antivirals and at an earlier stage of disease.
Supplementary Material
Acknowledgements
We would like to thank the following persons for their invaluable help in running this study: Zahra Jahandideh, Khadijeh Abrari, Samira Elhamirad, Hakimeh Malaki-Moghadam, Naeimeh Bozorg Ghomi, Roghayeh Nami, Fatemeh Ahmadian, Dariush Rahimi, Zahra Safarpour, Zahra Ostadi, Dr Roozbeh Bayati and Professor Majid Saeedi.
Funding
This trial was sponsored by the Abadan University of Medical Sciences and funded by the International Treatment Preparedness Coalition (grant number ITPC-2020). The funding source was not involved in any aspect of the study, including design, data collection, analysis, interpretation, writing or decision to submit the paper for publication.
Transparency declarations
S. Merat has received travel grants from and is a stockholder of Fanavaran Rojan Mohaghegh Darou Co. A. Nateghi Baygi and H. Nateghi Baygi are employees and stockholders of Fanavaran Rojan Mohaghegh Darou Co. All other authors: none to declare.
Author contributions
Patient enrolment, management and follow-up was performed by M. Abdollahi, F. Abedi, M. Afshari, E. Akbarpour, A. Ali Asgari, A. Anushiravani, Z. Arizavi, Z. Azarkar, E. Azimi, F. Babamahmoodi, A. Bahadori, E. Barahimi, A. Bonyadi, L. Davoodi, A. Davoudi Badabi, S. Dehghan Manshadi, F. Dehghani, A. Ebrahimzadeh, M. Ebrahimzadeh, G. Eslami, H. Esmaeilian, N. Hasooni Bahrini, A. Hormati, H. Hosamirudsari, S. Jelvay, N. Khajavirad, J. Khodadadi, Z. Mehrabi, H. Mirzaei, M. Mobarak, S. Mobarak, M. Moghimi, R. Moslemi, H. Mousavi, S. Mousaviasl, M. Naghipour, Z. Nekoukar, M. Noori Jangi, Z. Poormontaseri, H. Pourmasoomi, E. Radmanesh, A. Sadeghi, M. Salasi, M. Salehi, S. Salmanzadeh, S. Sayar, A. Shabani, M. Shabani, S. Shokouhi, S. Yaghoubi, S. Yeganeh, A. Zeinali, M. Ziaee and F. Zolfaghari. Data collection was performed by E. Akbarpour, M. Hassaniazad, F. Joukar, F. Mansour-Ghanaei, L. Rezaie Keikhaie, A. Tousi and T. Yaghubi Kalurazi. Local study management and supervision was performed by H. Abbaspour Kasgari, M. Afshari, Z. Arizavi, H. Fakheri, A. Hormati, J. Karimi, F. Mansour-Ghanaei, H. Mirzaei, M. Mobarak, L. Rezaie Keikhaie, A. Sadeghi, M. Salasi and M. Ziaee. Central data quality control was performed by D. Merat. Randomization and blinding were managed by E. Akbarpour, A. Nateghi Baygi, H. Nateghi Baygi and A. Sadeghi. Statistical analysis was performed by K. McCann, B. Simmons and H. Wentzel. The first draft of the manuscript was prepared by S. Merat, B. Simmons and H. Wentzel. Central study supervision was performed by A. Hill and S. Merat. The study was designed by A. Hill, S. Merat, S. Mobarak and M. Salasi. All authors read and approved the final manuscript.
Supplementary data
Table S1 and Figure S1 are available as Supplementary data at JAC Online.
References
- 1. WHO. Therapeutics and COVID-19: Living Guideline. https://www.who.int/publications/i/item/WHO-2019-nCoV-therapeutics-2021.1.
- 2. WHO Solidarity Trial Consortium. Repurposed antiviral drugs for Covid-19 - interim WHO Solidarity Trial results. N Engl J Med 2021; 384: 497–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rocco PRM, Silva PL, Cruz FF et al. Early use of nitazoxanide in mild COVID-19 disease: randomised, placebo-controlled trial. Eur Respir J 2021; 58: 2003725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. The Recovery Collaborative Group. Dexamethasone in hospitalized patients with Covid-19. N Engl J Med 2021; 384: 693–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. The REMAP-CAP Investigators. Interleukin-6 receptor antagonists in critically ill patients with Covid-19. N Engl J Med 2021; 384: 1491–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Recovery Collaborative Group. Tocilizumab in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. Lancet 2021; 397: 1637–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Abbaspour Kasgari H, Moradi S, Shabani AM et al. Evaluation of the efficacy of sofosbuvir plus daclatasvir in combination with ribavirin for hospitalized COVID-19 patients with moderate disease compared with standard care: a single-centre, randomized controlled trial. J Antimicrob Chemother 2020; 75: 3373–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Eslami G, Mousaviasl S, Radmanesh E et al. The impact of sofosbuvir/daclatasvir or ribavirin in patients with severe COVID-19. J Antimicrob Chemother 2020; 75: 3366–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sadeghi A, Ali Asgari A, Norouzi A et al. Sofosbuvir and daclatasvir compared with standard of care in the treatment of patients admitted to hospital with moderate or severe coronavirus infection (COVID-19): a randomized controlled trial. J Antimicrob Chemother 2020; 75: 3379–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Simmons B, Wentzel H, Mobarak S et al. Sofosbuvir/daclatasvir regimens for the treatment of COVID-19: an individual patient data meta-analysis. J Antimicrob Chemother 2021; 76: 286–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Roozbeh F, Saeedi M, Alizadeh-Navaei R et al. Sofosbuvir and daclatasvir for the treatment of COVID-19 outpatients: a double-blind, randomized, controlled trial. J Antimicrob Chemother 2021; 76: 753–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Yakoot M, Eysa B, Gouda E et al. Efficacy and safety of sofosbuvir/daclatasvir in the treatment of COVID-19: a randomized, controlled study. SSRN Electronic Journal 2020; 10.2139/ssrn.3705289. [DOI] [Google Scholar]
- 13. Merat S. SD1000 Research Team. SD1000: high sustained viral response rate in 1361 patients with hepatitis C genotypes 1, 2, 3, and 4 using a low-cost, fixed-dose combination tablet of generic sofosbuvir and daclatasvir: a multicenter, Phase III clinical trial. Clin Infect Dis 2020; 70: 2206–12. [DOI] [PubMed] [Google Scholar]
- 14. Poustchi H, Majd Jabbari S, Merat S et al. The combination of sofosbuvir and daclatasvir is effective and safe in treating patients with hepatitis C and severe renal impairment. J Gastroenterol Hepatol 2020; 35: 1590–4. [DOI] [PubMed] [Google Scholar]
- 15. Elfiky AA, Mahdy SM, Elshemey WM. Quantitative structure-activity relationship and molecular docking revealed a potency of anti-hepatitis C virus drugs against human corona viruses. J Med Virol 2017; 89: 1040–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chien M, Anderson TK, Jockusch S et al. Nucleotide analogues as inhibitors of SARS-CoV-2 polymerase, a key drug target for COVID-19. J Proteome Res 2020; 19: 4690–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Jacome R, Campillo-Balderas JA, Ponce de LS et al. Sofosbuvir as a potential alternative to treat the SARS-CoV-2 epidemic. Sci Rep 2020; 10: 9294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Beck BR, Shin B, Choi Y et al. Predicting commercially available antiviral drugs that may act on the novel coronavirus (SARS-CoV-2) through a drug-target interaction deep learning model. Comput Struct Biotechnol J 2020; 18: 784–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Xie X, Muruato AE, Zhang X et al. A nanoluciferase SARS-CoV-2 for rapid neutralization testing and screening of anti-infective drugs for COVID-19. Nat Commun 2020; 11: 5214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lo HS, Hui KPY, Lai H-M et al. Simeprevir potently suppresses SARS-CoV-2 replication and synergizes with remdesivir. ACS Cent Sci 2021; 7: 792–802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Liu S, Lien CZ, Selvaraj P et al. Evaluation of 19 antiviral drugs against SARS-CoV-2 infection. bioRxiv 2020; 10.1101/2020.04.29.067983. [DOI] [Google Scholar]
- 22. Levi J. Interpreting in-vitro data for sofosbuvir against SARS-CoV-2: cell lineage is key. ISIRV Therapeutics for COVID-19 Conference, 2020. Oral Poster Presentation. [Google Scholar]
- 23. Kirby BJ, Symonds WT, Kearney BP et al. Pharmacokinetic, pharmacodynamic, and drug-interaction profile of the hepatitis C virus NS5B polymerase inhibitor sofosbuvir. Clin Pharmacokinet 2015; 54: 677–90. [DOI] [PubMed] [Google Scholar]
- 24. Sacramento CQ, Fintelman-Rodrigues N, Temerozo JR et al. In vitro antiviral activity of the anti-HCV drugs daclatasvir and sofosbuvir against SARS-CoV-2, the aetiological agent of COVID-19. 2021; 76: 1874–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Gandhi Y, Eley T, Fura A et al. Daclatasvir: a review of preclinical and clinical pharmacokinetics. Clin Pharmacokinet 2018; 57: 911–28. [DOI] [PubMed] [Google Scholar]
- 26. FDA. DAKLINZA (Daclatasvir) Tablets, For Oral Use. FDA Access Data. 2015; 1–34. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/206843s006lbl.pdf.
- 27. Ahmed S, Karim MM, Ross AG et al. A five-day course of ivermectin for the treatment of COVID-19 may reduce the duration of illness. Int J Infect Dis 2021; 103: 214–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Aoki FY, Macleod MD, Paggiaro P et al. Early administration of oral oseltamivir increases the benefits of influenza treatment. J Antimicrob Chemother 2003; 51: 123–9. [DOI] [PubMed] [Google Scholar]
- 29. Ramakrishnan S, Bafadhel M. Inhaled budesonide for early treatment of COVID-19 - Authors' reply. Lancet Respir Med 2021; 9: e61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Weinreich DM, Sivapalasingam S, Norton T et al. REGN-COV2, a neutralizing antibody cocktail, in outpatients with Covid-19. N Engl J Med 2021; 384: 238–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.