Abstract
Background
In the absence of a vaccine, the global spread of COVID-19 during 2020 has necessitated non-pharmaceutical interventions to curb the rise of cases.
Purpose
The article uses the health belief model and a novel rapid mobile survey to examine correlates of reported mask-wearing as a non-pharmaceutical intervention in South Africa between May and August 2020.
Methods
Two-way tabulations and multivariable analysis via logistic regression modeling describe correlations between reported mask-wearing and factors of interest among a sample of 7074 adults in a two-period national longitudinal survey, the National Income Dynamics Study-Coronavirus Rapid Mobile Survey (NIDS-CRAM).
Results
In line with the health belief model, results showed that self-efficacy, the prevalence of others’ mask-wearing in the same district, and affluence were positively associated with reported mask-wearing. Those who reported staying at home were significantly less likely to report wearing a mask. There was little evidence that the expected severity of the disease if contracted, affects these decisions. Hypertension, obesity, or being overweight (measured three years earlier) did not have a significant association with mask-wearing. The prevalence of mask-wearing increased significantly from May to August 2020 as COVID-19 cases increased and lockdown restrictions were eased. Contrary to the health belief model, we found that despite having a higher mortality risk, the elderly had significantly lower odds of mask-wearing.
Conclusion
In South Africa, the mask-wearing adherence has increased rapidly. It is concerning that the elderly had lower odds of mask-wearing. This should be examined further in future research.
Keywords: COVID-19, South Africa, Face-coverings, Masks, Prevention
Implications.
Practice: This study adds to existing evidence that showed that the health belief model fares well in describing the main factors influencing mask-wearing during the pandemic. The study showed the importance of local social norms as a predictor of mask-wearing.
Policy: It is encouraging to see high and increasing levels of self-reported mask-wearing, but worrying that mortality risk does not affect mask-wearing. This provides additional impetus to target communication promoting mask-wearing in this high-risk group.
Research: In particular, it is worrying that the elderly has significantly lower odds of wearing masks. This should be examined further in future research. It may be that a different strategy is needed because the elderly are in general more reluctant to change and therefore needs more motivation to change their behavior.
INTRODUCTION
The global spread of COVID-19 during 2020 caused at least 2.69 million official deaths by 19 March 2021 and has placed a direct and significant burden on health systems, in addition to the indirect effect of lockdowns on societies and economies [1–6]. In the absence of population immunity through universal vaccination, adherence to non-pharmaceutical interventions (NPIs) is the main avenue to curb the disease’s devastation. NPIs aimed at slowing the transmission of COVID-19 such as physical distancing, hand hygiene, and wearing face masks have enabled many countries to navigate the reopening of schools and the return to economic activity in the shadow of the pandemic. However, to effectively contain the spread of the virus, adherence to NPIs requires large-scale behavior change and societal buy-in.
We rely on the Health Belief Model (HMB) to understand the transmission mechanisms of the large-scale behavior changes needed to decrease COVID-19 transmission. The HBM is a conceptual framework that is widely used for understanding health behavior, like the adoption of NPIs during COVID-19.
NPI adherence during this pandemic is challenging for at least three reasons. First, many of those who need to make sacrifices by adhering to NPIs will not directly benefit in terms of the reduced mortality risk resulting from these measures. For example, sacrifices are required from young and prime-aged adults who have higher infection rates because they are more socially and economically active. Benefits will, however, largely accrue to adults with co-morbidities and those 60 years or older who have a significantly higher risk of becoming seriously ill or dying when infected with COVID-19 [7,8]. This is pertinent since transmission is often driven by younger and prime-aged adults [9,10]. To have maximum impact, NPI adherence thus requires altruism or a sense of solidarity from young and prime-aged adults. A second challenge is that benefits to NPI adherence are not tangible or immediate, whereas the sacrifices are observed and need to be maintained daily. When engaging in COVID-19 prevention measures, we do not receive feedback about the impact that our efforts and actions have had on the risk of contracting an invisible virus or the risk of transmitting the virus if asymptomatic [11]. A third challenge is that behavior change needs to be maintained over a long period with an uncertain endpoint [12]. The long duration creates the risk of NPI fatigue—an inability to sustain feelings of cautiousness, together with boredom, prompt risk-taking, and carelessness [13]. It could also lead to erroneous learning, where individuals underestimate their infection risk because they have not yet contracted the virus, and consequently become less vigilant [14]. An example of erroneous learning from feedback in this context would be someone believing that they are not at high risk because they have not yet become infected [14].
Masks have been shown to limit the spread of infectious diseases [15]; the evidence base for mask-wearing has expanded significantly with research during the COVID-19 pandemic [16–23]. It is now established that because the coronavirus spreads mainly via respiratory droplets, masks can offer effective protection from contracting the virus to both the wearer and others [21,24,25]. Masks are more effective at containing the virus when combined with physical distancing [19,21]. Additionally, because mask-wearing is visually observed and required in public and social settings, there is a strong potential role for the adherence of others and implied social norms in promoting adherence.
This study focuses on the self-reported use of masks in the context of one of the most unequal societies in the world: post-apartheid South Africa. South Africa’s wide socioeconomic spectrum allows us to observe how social circumstances affect compliance cost and in turn, whether such costs can be prohibitive for mask-wearing take-up and adherence. The South African case study is also interesting because the government responded pre-emptively to the pandemic while cases were still relatively low, by implementing one of the strictest lockdowns globally, including the prohibition of the sale of alcohol and tobacco [26]. Our longitudinal data set documents self-reported behavior and beliefs from 7 May to 27 June 2020 (first survey) and again from13 July to 13 August 2020 (second survey). This period includes a substantial increase in freedom of movement with the move from alert level 4 to alert level 3 on 1 June as well as a steep rise in COVID-19 cases and hospitalizations, peaking in July.
Over this period there were also important shifts in government policy towards mask-wearing based on rapidly changing evidence on the effectiveness of this preventive measure. After an initial period of discouraging mask-wearing for asymptomatic or non-sick individuals, mask-wearing become mandatory on 29 April, and on 12 July non-compliance with mask-wearing became criminalized with penalties of up to six months imprisonment. Under these mandatory rules, taxi drivers, shop owners, and other authorities became responsible for ensuring that the public wore masks in their shops or taxis, and faced prosecution if they were caught flouting these regulations. During this time messages from government officials reinforced the narrative that behavior change by citizens and adherence to NPIs would “flatten the curve” of infections. Electronic Supplementary Material 2 outlines key points in the government’s public communication and policy regarding mask-wearing.
This study responds to recent calls in this journal for research on predictors of mask-wearing that would benefit from larger sample longitudinal surveys and can examine sociodemographic and regional differences in mask-wearing [27]. We are in a position to present such analysis because of the Coronavirus Rapid Mobile Survey (NIDS-CRAM) dataset [28,29]: a novel, rapid mobile longitudinal study which was designed to include respondents from across the socioeconomic spectrum, carefully drawing from the sampling frame of an existing large national longitudinal survey. This study examines data from two waves of this longitudinal dataset.
METHODS
Respondents and setting
During the time that the survey was planned, the country was facing a strict lockdown with minimal freedom of movement, which precluded in-person data gathering. Due to concern about the social impact of the pandemic and the lockdown, a multi-institutional and multidisciplinary group of 30 social science researchers collaborated with policymakers and civil society partners to conceptualize, design, fund, and conduct rapid surveys. Various modalities were explored but because of concerns about non-response amongst the poor due to the costs of connectivity and access to devices, computer-assisted telephone interviewing surveys (CATI) were preferred over internet or SMS surveys. The survey focused on the socio-economic consequences and behaviors around COVID-19.
The NIDS-CRAM (National Income Dynamics Study-Coronavirus Rapid Mobile Survey) study respondents include adults aged 18 and older residing in South Africa who had previously participated in the 2017 survey of the nationally representative National Income Dynamics Study (NIDS) [30]. Although NIDS-CRAM is smaller in size than the NIDS survey, it is still partially nationally representative.
South Africa’s COVID-19 regulation to limit the spread of the disease is categorized into five alert levels, with alert level 5 characterized as the most prohibitive in movement and freedom of choice. Alert level 5 of lockdown, which started on 26 March 2020, did not allow for any movement outside one’s own house, except for grocery shopping, medical reasons, or for essential workers. Alert level 4 allowed priority sector employees to return to work and opened a daily three-hour slot for exercise. During these alert levels, the sale of alcohol and tobacco was banned, and the military was employed to enforce the rules. Alert level 3 permitted onsite work to resume for most professions (excluding potential high-risk transmission jobs like beauty salons or gyms), and allowed exercise at any time during the day.
Data for the first NIDS-CRAM survey was collected between 7 May and 27 June 2020 and coincided with both lockdown alert level 4 (up to 31 of May) and alert level 3 (from 1 June). The second survey took place between 13 July and 13 August 2020 (all categorized as alert level 3). This period includes the steep rise and fall of South Africa’s first wave of COVID-19. The policies associated with each level are summarized in Electronic Supplementary Material 2 and Electronic Supplementary Material 1 tracks the overlap between the two surveys and the COVID-19 lockdown restrictions.
Sampling
For the NIDS-CRAM survey, a sub-sample was drawn from National Income Dynamics Study (NIDS) 2017 using a stratified sampling design. NIDS is a five-wave national longitudinal survey, collected between 2008 and 2017. Stratification was based on household per capita income decile, race, age categories, and urban location, resulting in 99 strata. A total of 17,568 individuals from the original NIDS sample were asked to participate in NIDS-CRAM, of whom 7074 agreed (40%) in the first survey.
The survey used “batch sampling”; the fieldwork team received new “batches” of the sample with 2500 observations each, drawn randomly from each of the 99 stratum in proportion to the strata’s representation share in the NIDS 2017 sample [31]. This strategy was selected because there was uncertainty about the drivers of non-response to a telephone survey under these circumstances. “Batch sampling” allowed the sampling rate to be adjusted as information about response rates became available. It ensures that the sample of respondents is comparable across the survey period, enabling tracking of broad trends within surveys.
Our ex-ante power calculations showed that even with a much lower realized sample size of 3000 observations per survey the longitudinal study would have been powered to identify a 3.2 percentage point increase in mask-wearing of a base of 50% in the first period. The relationship between sample size, power, and the detectable percentage point change at 5% significance is in shown Electronic Supplementary Material 3.
This study is largely reliant on the data from NIDS-CRAM’s first and second surveys. For variables that are not captured in NIDS-CRAM but are fairly stable over the medium term such as hypertension screenings and weight measurements, we use NIDS 2017. We also use data on diagnosed Coronavirus cases on the district level from the Mediahack Collective [32] and data on trends in searches for masks from Google Trends.
Measures
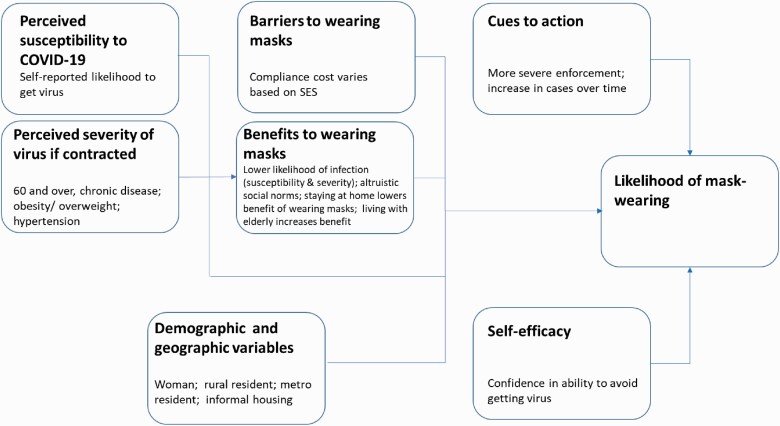
Our analysis follows the expanded health belief model [33–35], with constructs to capture (a) cues to action and the (b) perceived susceptibility to COVID-19, (c) perceived severity of COVID-19 if one would contract it, (d) perceived benefits of face covering-wearing, (e) perceived barriers to mask-wearing including compliance costs and (f) self-efficacy. The links between these constructs and their empirical approximations for COVID-19 prevention are summarized in Table 1.
Table 1.
Constructs of the health belief model and related empirical measures for COVID-19 prevention through mask-wearing
| Constructs of the health belief model | Measures |
|---|---|
| Cues to action | • Linear time trend for the time of the interview (in half months) |
| Perceived susceptibility to COVID-19. | • Perceived to be susceptible to COVID-19 |
| Perceived severity of COVID-19 if contracted | • Respondent aged 60 or over • Respondent has a chronic condition • High blood pressure in 2017 • Obese in 2017 • Overweight in 2017 |
| Perceived benefits of mask-wearing |
Individual avoiding infection
• Perceived to be susceptible to COVID-19 & perceived severity of COVID-19 if contracted Altruistic social norms about avoiding harm to others • Share of respondents in that district—excluding the respondent her- or himself—reporting the wearing of masks. • Living with person aged 60 or older |
| Perceived barriers to mask-wearing | • Compliance cost approximated by socioeconomic status |
| Self-efficacy | • Perceived ability to avoid virus (self-efficacy) |
Benefits to wearing masks include avoiding individual infections and complying with altruistic social norms about avoiding harm to others. The benefits to the wearer are captured with the measures for perceived susceptibility to COVID-19 and the perceived severity of COVID-19 if contracted. Local variation in social norms about the wearing of masks is represented by the share of respondents in that district—excluding the respondent her- or himself—reporting the wearing of masks. Additionally, benefits to wearing masks would be increased for respondents living with a person aged 60 or older and it would be reduced for those who report that they stay at home, and therefore have less need for protecting themselves and others because they presumably have minimal contact with others.
Self-efficacy is based on whether the respondent thought they could avoid contracting the virus. Figure 1 provides an overview of how the empirical model has been constructed to embody the health belief theory and shows the interrelationship amongst its various components.
Fig 1.
Health belief model and the likelihood of wearing masks.
NIDS-CRAM MEASURES
NPI adoption
First and second survey
The questions asking respondents about their behavior changes in the first and second waves were structured to be open-ended. In the first instance, we began by asking, “Have you changed your behavior since learning about the Coronavirus?” and followed up with the question, “In what ways have you changed your behavior?” The second survey was conducted shortly after. To acknowledge that we had previously asked about behavior, we changed the question to: “Are you behaving differently to protect yourself from the Coronavirus?”. All responses were recorded and included, for example, reporting handwashing, wearing a face mask, physical distancing, and staying at home. Interviewers were instructed not to read out options, but to select applicable items in the order they were reported, and respondents were not limited in the number of behaviors they could report. They were also allowed to report other behavior which was captured as text.
Second survey
In the second survey, a question pertaining specifically to mask-wearing was posed to respondents after the initial NPI question. Respondents were asked directly whether they wore a mask when going out in public in the previous seven days.
District prevalence of wearing masks
We calculated the prevalence of wearing masks per district as the share of survey respondents in the respondent’s cluster who reported that they were wearing masks. It excludes the respondent.
Interview times
To account for differential timing of interviews and the changing regulations, our analysis contains interview time measures that categorize observations based on the date of interview, in half-month periods.
Socio-economic and demographic measures
Respondents reported on their areas of residence (urban or rural), residence building structure, gender identity, age, and employment. We also use grant receipt and hunger to check the robustness of our results to the inclusion of alternative socioeconomic proxies. The hunger variable was binary and measured in response to the question, “In the last 7 days has anyone in your household gone hungry because there wasn’t enough food?” The grant receipt variable was based on the question “Do you personally receive any kind of government grant?”
Health measures
During the first NIDS-CRAM survey, respondents were asked whether they have one or more of the following chronic conditions: HIV, tuberculosis, lung conditions, heart conditions, or diabetes. Respondents did not need to indicate which condition. Respondents with certain chronic conditions have been identified as susceptible to serious COVID-19 consequences [36,37].
NIDS survey 5 (2017) measures
Socioeconomic quintiles
Due to concerns about a high share of missing values (available for 6490 of the 10,126 observations in our estimation sample) as well as the accuracy and reliability of the income variable in NIDS-CRAM, we derived a socioeconomic index to capture differences in living standards using the 2017 NIDS. It includes electricity; housing (informal housing; hut; formal housing); sanitation (bucket system, pit latrine, flush toilet); access to piped water; and the ownership of a range of assets including a mobile phone, a car, a computer, a stove, and a lounge set. The weights for the index are estimated with multiple correspondence analysis. To allow for non-linear effects across quintiles in South Africa’s polarized and highly unequal society, we construct quintiles. The bottom quintile represents the most affluent and the top quintile the poorest. To gauge the stability of quintile classification over time we compare shifts in the quintile classification of respondents who were interviewed in NIDS 2014 [38] and NIDS 2017: we find that less than 10% of respondents move more than one quintile away from their original quintile classification.
Biometric data
Anthropometric data on respondents’ weight, height, and blood pressure were drawn from the NIDS 2017 data to identify whether respondents suffered from high blood pressure (defined as 140/90mmHg or higher), were overweight (with a body mass index exceeding 25), or obese (with a body mass index exceeding 30). Blood pressure was measured twice, both times in the left arm and allowing for a 5 min rest period between measurements. They were tested with an automated BP monitor, the Omron M7 BP with a multi-size cuff, which was factory-calibrated. Hypertension, being overweight, or being obese have been identified as key risk factors for COVID-19 mortality [39–41]. These measurements were taken in 2017, but this biometric information on blood pressure and body mass index conveys valuable information on the medical risk because lifestyle-related health conditions tend to persist, and the associated risks accumulate over time. Based on the comparison between 2014 and 2017 measurements in NIDS for respondents who were interviewed in both surveys, we find that classifications remained stable across the three years: 88.7% for the overweight indicator; 91.8% for the obesity indicator; and 79.5% of the hypertension indicator.
Measures from sources other than NIDS-CRAM and NIDS
Prevalence of COVID-19 cases at the time of interview
These are the cumulative COVID-19 cases per 100,000 in the district at the time of the interview. The district case data was based on officially released numbers and collated by the Mediahack Collective [32]. The Mediahack Collective is a group of independent journalists who specialize in digital storytelling and developed a COVID-19 dashboard for South Africa in March 2020.
Google searches for “mask”
Using the Google interest index, we can measure search interest for masks relative to the highest point for the past 12 months in South Africa. The index ranges between 0 and 100, with 100 representing peak popularity. The most popular related search queries for users searching for this term between 31 August 2019 and 31 August 2020 were “face mask” (100), “the mask” (27), “masks” (21), “n95 mask” (17) and “surgical mask” (14). The numbers in brackets are again a search interest indicator and measured relative to the most. The trend was near identical when using the plural “masks” for the search term.
Data analyses
The article draws on descriptive and multivariable regression analysis to answer the key questions around NPI adherence and the determinants of mask-wearing. Specifically, logistic regression models were conducted to determine which subgroups were more likely to adhere to mask-wearing. We also test for the possibility of trade-offs in NPI adoption. The NIDS-CRAM survey allowed respondents to list more than one self-reported behavior change. This design can also be used to assess whether there are complementarities or trade-offs in the preventative choices individuals make. For example, respondents who report that they stay at home may have less reason to wear masks since their exposure to public spaces is limited or non-existent. At the same time, it would be expected that mask-wearing becomes more prominent as lockdown levels ease.
Descriptive statistics are reported for the pooled sample, and where appropriate we distinguish between findings from the May/June 2020 interview and the July/August 2020 interview. We conduct multivariate analysis for the pooled sample using logit regressions. We report on the odds ratios. Statistical significance is defined as p ≤ 0.05.
RESULTS
In the second survey, 5676 of the 7074 respondents were interviewed again, which represents a rate of attrition of 19%. Attrition is predominantly due to respondents being uncontactable, and in-person follow-up not being possible. Post-stratified panel weights were used to correct for sampling bias due to attrition [31].
Of the respondents in our estimation sample, 14% were 60 years or older. Of respondents, 19% had at least one chronic condition. In the 2017 NIDS survey, one in five respondents (20%) were reported as being hypertensive, more than half (52%) were overweight, and one-quarter were obese (27%).
In response to the open-ended question about behavior change following the pandemic, most respondents in our estimation sample reported that they wore masks (62%). There was a discrepancy in self-reported mask-wearing behavior as measured by this open-ended question, compared to the closed question that was asked in the second survey. When asked about mask-wearing specifically and directly, 96% of respondents in the survey reported wearing masks in public. This is in contrast to the much lower 74% of respondents who reported wearing face masks based on their answer to the open-ended question about post-pandemic changes in their behavior in the second survey.
Of the respondents, 35% thought that they were susceptible to COVID-19, while 51% perceived themselves to not be susceptible and 14% did not know. The share that thought they were susceptible to COVID-19 increased from 29% to 41% between the two surveys. Also, COVID-19 susceptibility had a strong relationship with the socioeconomic quintiles: 48% of the most affluent quintile considered themselves susceptible, but only 27% of the most vulnerable quintile. In both cases, the difference was significant (Prob> F = 0.0000).
The overwhelming majority of respondents (83%) reported self-efficacy, stating that they believed that they could avoid contracting the virus. There was no significant variation in self-efficacy between the two surveys. Self-efficacy was significantly lower amongst the most affluent quintile (79%) than amongst the most vulnerable (84%) (Prob > F = 0.0498).
The mean district average for the self-reported wearing of masks was 61%. Two out of five respondents (40%) reported that they stayed at home to protect themselves against the virus. Of respondents, a share of 23% was living with someone 60 years or older.
Less than half of the respondents were employed 45%. Slightly more than half of the respondents were women 53%. Rural and metropolitan residents constituted respective shares of 30% and 37% of respondents. Informal housing residents represented 11% of respondents (Table 2).
Table 2.
Descriptive statistics for variables included in empirical model
| Mean | Standard deviation | ||
|---|---|---|---|
| Outcome | Wearing of masks | 0.62 | 0.49 |
| Susceptible | Not perceived to be susceptible | 0.51 | 0.50 |
| Don’t know whether susceptible | 0.14 | 0.34 | |
| Perceived to be susceptible to COVID-19 | 0.35 | 0.48 | |
| Severity | Respondent aged 60 or older | 0.14 | 0.34 |
| Respondent has a chronic condition | 0.19 | 0.39 | |
| High blood pressure in 2017 | 0.20 | 0.40 | |
| Obese in 2017 | 0.27 | 0.45 | |
| Overweight in 2017 | 0.52 | 0.50 | |
| Benefits | District prevalence of mask-wearing | 0.61 | 0.14 |
| Stay at home | 0.40 | 0.49 | |
| Living with person aged 60 or older | 0.23 | 0.42 | |
| Barriers | Employed | 0.45 | 0.50 |
| SES quintile 1 (most affluent) | 0.17 | 0.38 | |
| SES quintile 2 | 0.22 | 0.41 | |
| SES quintile 3 | 0.21 | 0.41 | |
| SES quintile 4 | 0.21 | 0.40 | |
| SES quintile 5 (poorest) | 0.19 | 0.40 | |
| Cue to action | Prevalence of COVID-19 cases at time of interview | 627.84 | 790.53 |
| Interviewed in second half May | 0.10 | 0.30 | |
| Interviewed in first half June | 0.18 | 0.39 | |
| Interviewed in second half of June | 0.18 | 0.38 | |
| Interviewed in first half July | 0.03 | 0.17 | |
| Interviewed in second half July | 0.38 | 0.49 | |
| Interviewed in first half August | 0.08 | 0.28 | |
| Self-efficacy | Perceived lack of ability to avoid virus | 0.12 | 0.32 |
| Don’t know about self-efficacy | 0.05 | 0.22 | |
| Perceived ability to avoid virus (self-efficacy) | 0.83 | 0.37 | |
| Demographic and geographic variables | Woman | 0.53 | 0.50 |
| Resides in informal building structure | 0.11 | 0.31 | |
| Rural resident | 0.30 | 0.46 | |
| Metro resident | 0.37 | 0.48 | |
| Observations | 10126 |
Note: For staying at home there are 387 missing values, bringing the N to 9739.
Adoption and adherence to NPI behaviors
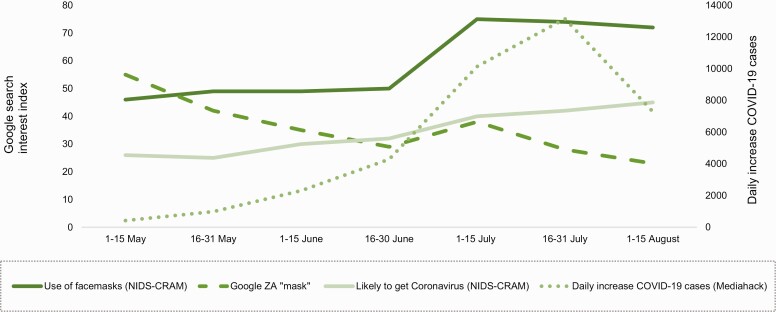
Figure 2 compares the NIDS-CRAM survey’s trends in wearing face masks from June to August 2020 with three other time trends, namely google searches for the term “mask” (reflecting levels of interest and concern, beliefs about contracting COVID-19 as reported in our survey and official and public data on the daily increase in COVID-19 cases over time. This graph enables an initial and tentative examination of some of the hypotheses in the health belief model. However, the trajectory of mask-wearing does not track well with the trends in Google searches, perceived risk, or the average national increase in official COVID-19 cases. Figure 2 does not provide any support for these factors playing a strong role. The trajectory of the mask-wearing trend line shows a sharp rise between the last half of June and the first half of July, which does correspond to the government’s stricter enforcement of the mask-wearing policy, hence including it. This happened at the time when the government was also relaxing constraints about movement outside the home, which would at the same time have increased the need for masks.
Fig 2.
Perceived likelihood of getting Coronavirus (c.f. disease progress and local Google searches for Coronavirus), May to August 2020.
Fifty percent of respondents reported wearing masks in May and June 2020, while 74% of respondents wore masks by July and August after the increased enforcement of the mask-wearing policy and increased movement outside the home. We observe potential trade-offs in the behavioral choices people make. More specifically, while the wearing of masks increased, staying at home, physical distancing, and social distancing decreased as the stringency of the lockdown and the restrictions on movement and economic activity were lifted Table 3.
Table 3.
Reported adoption of and adherence to NPIs.
| May and June (%) | July and August (%) | |
|---|---|---|
| Handwashing | 63 | 60 |
| Physical distancing | 23 | 18 |
| Avoiding big groups | 15 | 8 |
| Stay home | 44 | 37 |
| Wearing masks | 50 | 74 |
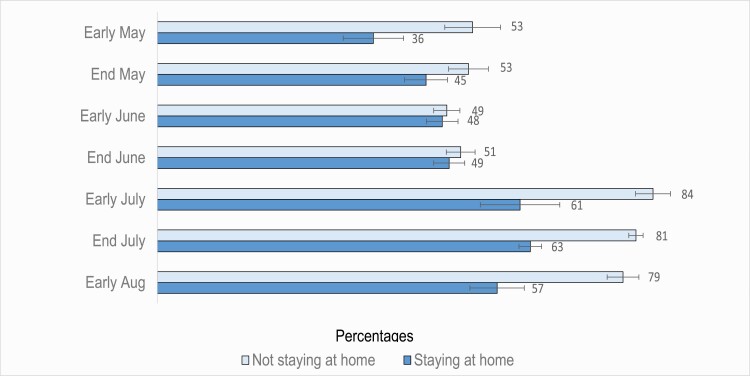
As expected, in line with our theoretical hypothesis about a lower benefit of wearing masks for those who stay at home, we see evidence of substitution effects between face covering-wearing and staying at home in Fig. 3. The figure shows that mask-wearing is more likely in cases where the respondent did not report staying at home as an NPI. The figure shows that the divide in wearing masks between home-stayers and those who venture out has grown over time.
Fig 3.
Percentage of respondents who reported wearing masks, comparing those who stay at home and those who do not, May to August 2020.
Factors associated with mask-wearing
Table 4 shows the results from four variations of logit regressions. The model specification is rooted in the theory framework (Model 1) ( Fig. 3). Model 2 includes staying at home to acknowledge the substitution between wearing masks and staying at home. Model 3 includes living with a person 60 years or older, which is missing for 387 observations in our estimation sample, thus lowering our sample from 10,126 to 9739 for this model and the subsequent model 4. Model 4 includes district-level dummies to account for district-level differences in, for instance, information or awareness about COVID-19, or measurement error in the official COVID-19 prevalence statistics.
Table 4.
Logit model for likelihood of wearing masks
| Theoretical tenet | Variable | Model 1 Odds Ratio |
Model 2 Odds ratio |
Model 3 Odds ratio |
Model 4 Odds ratio |
|---|---|---|---|---|---|
| Susceptible | Perceived susceptibility COVID-19 | ||||
| Don’t know | 1.22** | 1.21** | 1.19 | 1.21** | |
| Perceived to be susceptible | 1.16 | 1.15 | 1.15 | 1.20** | |
| Severity | Respondent aged 60 or older | 0.77*** | 0.77** | 0.73** | 0.74*** |
| Respondent has a chronic condition | 1.00 | 0.99 | 0.98 | 0.98 | |
| High blood pressure in 2017 | 1.07 | 1.07 | 1.10 | 1.10 | |
| Obese in 2017 | 1.10 | 1.11 | 1.12 | 1.12 | |
| Overweight in 2017 | 1.10 | 1.09 | 1.10 | 1.13 | |
| Benefits | District prevalence of mask-wearing | 6.49*** | 6.65*** | 6.87*** | 1.29 |
| Stay at home | 0.65*** | 0.68*** | 0.67*** | ||
| Living with person aged 60 or older | 0.93 | 0.93 | |||
| Barriers | Employed | 1.20** | 1.21 | 1.10 | 1.10 |
| SES 2017 [reference is quintile 1 (most affluent)] | |||||
| SES quintile 2 | 0.72*** | 0.71*** | 0.72** | 0.72*** | |
| SES quintile 3 | 0.73** | 0.71*** | 0.71*** | 0.70*** | |
| SES quintile 4 | 0.79 | 0.77** | 0.79 | 0.79 | |
| SES quintile 5 (least affluent) | 0.83 | 0.81 | 0.81 | 0.85 | |
| Cue to action | Prevalence of COVID-19 cases at time of interview | 1.00 | 1.00 | 1.00 | 1.00 |
| Time of interview | 1.19*** | 1.19*** | 1.20*** | 1.28 | |
| Self-efficacy | Perceived ability to avoid virus (self-efficacy) | ||||
| Don’t know | 0.91 | 0.91 | 0.95 | 0.94 | |
| Perceived self-efficacy | 1.27** | 1.29** | 1.30*** | 1.26** | |
| Demographic and geographic variables | Woman | 1.03 | 1.04 | 1.05 | 1.05 |
| Resides in informal building structure | 0.95 | 0.96 | 0.92 | 0.90 | |
| Rural resident | 0.99 | 0.99 | 0.97 | 1.01 | |
| Metro resident | 1.02 | 1.02 | 0.99 | 1.73 | |
| Observations | 10126 | 10126 | 9739 | 9739 |
**p <.05, ***p <.01, Note: Model 2 includes staying at home to acknowledge the substitution between wearing masks and staying at home. Model 3 includes living with a person 60 years or older. Model 4 includes district dummies.
Odds ratios are reasonably stable across the model specifications. To avoid overcrowding the text, we focus the reporting on the odds ratio of the first model unless we report on a variable that has been added in subsequent models; in this case, we report on the first model in which the variable was included.
We find that those who perceived themselves to be susceptible to the virus were more likely to wear masks than those who did not perceive themselves to be susceptible (aOR: 1.16; 95% CI: 0.99–1.36). The regressions also show that those who did not know whether they were susceptible or not were also more likely to wear masks compared to those who said that they were not susceptible and unlikely to contract COVID-19 (aOR 1.22; 95% CI, 1.01–1.47).
In terms of the association of perceived severity of the virus if contracted and wearing masks: being over 60 years of age was associated with a lower likelihood of reporting face mask-wearing (aOR 0.77; 0.63–0.94). Obese, overweight, and hypertensive respondents had higher odds of wearing masks than their counterparts with lower risk, but the odds ratios were not significantly different from an odds ratio of 1.
Considering the mask-wearing benefits, we found that the prevalence of respondents reporting that others in their district wore masks increased the odds of the respondent reporting that they wear masks (aOR 6.49; 95% CI, 2.97–14.22). When respondents reported that they had changed their behavior since the onset of the pandemic by staying at home, the odds of reporting wearing masks is significantly lower than 1 (aOR 0.65; 95% CI, 0.58–0.74). Living with someone 60 years or older has an odds ratio below 1, but it is not significant.
Potential barriers to wearing masks were explored. Assuming socio-economic status variables to be an important indicator of compliance cost, we consider the association between mask-wearing and employment as well as the socioeconomic status index. Being employed was associated with a higher likelihood of wearing a mask, although the effect is only statistically significant in the first model (aOR 1.20; 95% CI, 1.04–1.39). In terms of socioeconomic status, respondents from quintile 2 (aOR 0.72; 95% CI, 0.57–0.91) and quintile 3 (aOR 0.73; 95% CI, 0.58–0.93) had significantly lower odds of wearing masks than those in SES quintile 1 (the most affluent). There was no significant difference between the odds of wearing masks when comparing the most affluent and those in the two poorest quintiles.
We also conduct sensitivity analysis due to concerns about whether the SES index from 2017 may be an imperfect proxy for socio-economic status. We included indicators of hunger and grant receipt in our models because there were concerns that those who provided income information differed in systematic ways from the rest of the survey sample. Hunger was captured with the question “In the last 7 days has anyone in your household gone hungry because there wasn’t enough food?” and was missing for only 67 observations of our estimation sample. The hunger indicator had an odds ratio of 0.86 but was not significantly different from 1. The grant receipt indicator was based on a question that asked “Do you personally receive any type of government grant?” The grant receipt indicator had an odds ratio of 1.15 but was not significant. The analysis was robust to the inclusion of the hunger and the grant receipt indicators, and findings were not affected by adding these variables.
Next, we consider findings linked to external cues to action over time. Respondents who were interviewed later the year had statistically significantly higher odds of wearing a face mask (aOR 1.19; 95% CI, 1.11–1.28). The official district-level prevalence of COVID-19 per 100,000 did not have an odds ratio significantly different from 1.
In terms of self-efficacy, those who thought that they could avoid contracting the virus were more likely to wear masks (aOR 1.26; 95% CI, 1.05–1.54) than those who said that they did not think that they could avoid contracting the virus. There was no significant difference in the odds ratios comparing those who thought they could not avoid contracting the virus and those who did not know.
None of the four demographic or geographical variables–being a woman, living in informal housing, residing in a rural area, or residing in a metropolitan area–had significant odds ratios.
DISCUSSION
Existing studies and modeling projections suggest that the large and rapid rise in reported face covering-wearing has had a substantial impact on the trajectory of the disease [18,19,21,23]. Early in the pandemic, public health messaging focused on promoting handwashing. At the time, mask use was only recommended for healthcare workers [42]. As more COVID-19 research was generated, it was recognized that the virus spreads mainly through respiratory droplet transmission, that surface transmission is exaggerated, and that pre-symptomatic and asymptomatic individuals are also infectious [43,44]. For these reasons, public health messaging started to encourage the wearing of masks as a high-impact preventative strategy for all [45–47]. Mandatory mask-wearing was introduced in South Africa during alert level 4 at a time when COVID-19 restrictions were slightly eased. Mask-wearing is powerful because it is visual and provides a sense of agency and control amidst greater freedom following the relaxation of restrictions.
Due to the severe restrictions on movement in April and May during lockdown alert levels 4 and 5, the benefits of mask-wearing may have been diminished because of the limited opportunities for social interaction. With the move to alert level 3, economic activity was expanded to include most jobs—apart from a few exceptions such as personal care services and gyms deemed to be high-risk—and outdoor exercise was allowed at all times. Schools were also gradually opened, allowing Grade 7 and 12 learners to return on 1 June. Other important changes within the period where the country was under alert level 3 included restaurants reopening and some sports matches resuming on 26 June. It is also important to note that the increase in freedom and responsibility came amidst growing fears about the steep trajectory of COVID-19 cases. On 8 July, the minister of health declared to parliament that the “storm that we have been warning about has arrived.” There were worries about the rapid increase in cases and fears about running out of hospital capacity, which prompted the reinstitution of the alcohol ban on 12 July and the re-closure of schools from 27 July to 24 August. Both hospital admissions and the daily increases in COVID-19 cases peaked in July.
Given the strong emerging evidence in favor of masks, it is encouraging that our data analysis finds a steep rise in the self-reported prevalence of respondents wearing masks. There is a noticeable and sharp upward rise in the half-month where the government’s messages about enforcing mask-wearing became stronger, suggesting that there was an effective cue to action early in July. In May and June 2020 half of the respondents were wearing face masks. By July and August, the wearing of masks had increased to three in four. In line with this descriptive analysis, the logit regressions find significantly higher odds of the wearing of masks for those interviewed later. Our data does not, unfortunately, allow us to distinguish between different plausible triggers: it may have been the rise in cases, the gradually increased prominence of the wearing of face-masks as a preventive measure, the President’s speech linking non-mask-wearing to legal action, or the subsequent media storm that contributed to changes in behavior. At the same time, there was heightened anxiety due to the steep increase in COVID-19 cases during July and August which may have increased the reliance on masks as an NPI. Furthermore, previous studies show that there is an increased use of face masks after governments and public health departments promote using them, particularly during disease outbreaks [33,48,49].
Susceptibility
Our analysis shows that perceived susceptibility to COVID-19 significantly increases mask-wearing. These findings are strongly supported by the literature: a higher perception of susceptibility to an infectious disease is associated with higher compliance with mask-wearing [33,48–54].
Severity
Additionally, we do not find any evidence to support the hypothesis that the severity of COVID-19 has an impact on mask-wearing. There is no evidence of a significant relationship between mask-wearing and the respondent’s COVID-19 mortality risk factors. Previous studies investigating mask use to prevent SARS and influenza transmission found that older adults were more likely to comply with mask-wearing [33,55], and it is a concern that we find that respondents aged 60 and older in South Africa have significantly lower odds ratios for wearing masks. This was contrary to findings such as those of Pereira-Ávila et al. (2020) that found that older individuals were neither less nor more likely to wear masks than younger individuals [56,57]. It is plausible that in South Africa high-risk individuals are not sufficiently informed about their elevated risk for severe disease and mortality.
Barriers
We find that there is a role for perceived barriers and compliance costs. The most affluent had a higher likelihood of wearing masks and there is some evidence of employed respondents having a higher odds ratio for wearing masks, although it is not consistent. Research shows [33] that during outbreaks, perceived susceptibility and perceived severity dwarf the effect of perceived barriers on the wearing of masks.
Benefits
We find evidence suggesting that the wearing of masks may have become a new social norm in many communities, which may further encourage individuals to wear masks. First, it is striking that an affirmative reply is close to universal amongst respondents when asking a closed and specific question about wearing a mask during the previous seven days. This near-universal affirmative on masks is not surprising given that the government indicated that non-compliance could have legal ramifications. The difference between the answers to the closed question and the open-ended question is consistent. We argue that social norms influence behavior because individuals believe that other people expect this behavior from them and there may be social penalties if they do not conform to this expected behavior. Past studies have shown that measurement directiveness—asking specific and closed-ended questions—leads to over-reporting of normative behavior [58,59]. Conversely, when respondents are asked open-ended questions without prompts or listed options, it can cause underreporting due to haste, fatigue, or forgetfulness amongst other issues.
The logistic regressions strengthen this interpretation, showing that the share of respondents who reported that others in their district wore face masks had a large and significant association with the likelihood of the respondent wearing a face mask. Wearing a mask in public, or not, is visible to others and sends a signal. The visibility of such actions enables these practices to disseminate more rapidly, aiding the establishment of social norms about safe and responsible behavior during the pandemic. A study in Japan, for example, found that most Japanese regarded mask-wearing as a sign of respect towards one’s health and therefore mask-wearing became a desirable habit and norm [48]. For these reasons, arguments that mask-wearing should be considered a social practice that is viewed through a social lens, instead of a medical infection control tool only, are increasing [60].
As expected, the benefit of wearing a mask is lower for those who do not leave the house. Respondents who reported staying at home were significantly less likely to report wearing a facemask. Conversely, because this is merely an association and does not signal a causal relationship, this may also indicate that those wearing face masks are less likely to stay at home. This has been raised as a concern: that masks may lead to a false sense of security, and that people will compensate for this risk adjustment by participating in higher-risk activities. This fear of risk compensation may impede effective policymaking and prevention of the spread of the pandemic. However, there has been little evidence of this risk compensation in other countries [61,62]. Framed in a more favorable light, the evidence of a substitution relationship between staying at home and wearing a mask could also be interpreted as showing that masks are a compromise between fear and agency, allowing wearers some freedom to venture outside, engage in economic activities, or go to school while remaining cognizant of their responsibilities and the risks of the pandemics.
Self-efficacy
Our findings show that self-efficacy has a positive and statistically significant association with mask-wearing for all models. In this context, a lack of self-efficacy or confidence in protecting oneself from contracting the virus may be considered a perceived barrier to adhering to mask-wearing.
RESEARCH AND PRACTICE
From the perspective of research on preventative care, it is interesting to see relatively high and quick take-up of mask-wearing for a disease where risks are perceived to be severe and imminent. This study adds to existing evidence that showed that the health belief model fares well in describing the main factors influencing mask-wearing during the pandemic and in an upper-middle-income country with high inequality.
While it is encouraging to see high and increasing levels of self-reported mask-wearing, from the perspective of a policymaker and a health practitioner it is worrying that mortality risk does not improve adherence to mask-wearing. This provides additional impetus to target communication promoting mask-wearing at this high-risk group. In particular, it is worrying that the elderly have significantly lower odds of wearing masks. This should be examined further in future research. It may be that a different strategy is needed because the elderly may be more resistant to change and therefore need a more targeted strategy, customized for their age group.
LIMITATIONS
We are reliant on self-reported information on the wearing of masks. We consider only deliberative risk, raised by the question, “Do you think you are likely to get the Coronavirus?” and not affective or experiential risk, which has been shown to differ from deliberative risk and have important links to behavior. We have information about self-reported chronic illness, age, hypertensive measurements, weight, and height in 2017 but do not know whether those with a higher risk of mortality are aware of these risks. Telephonic interviews have limitations because questions need to be short and few. However, this survey modality was the best option for this purpose given the setting, feasibility constraints, and socio-economic bias of internet and SMS surveys.
Supplementary Material
Acknowledgements
We thank the Allan and Gill Gray Philanthropy, Michael and Susan Dell Foundation and the FEM Education Foundation for funding the NIDS-CRAM surveys, the NIDS-CRAM team, especially Kim Ingle, Tim Brophy and Reza Daniels for quality assurance, data cleaning and management, as well as the Mediahack team who provided us with district-level data on COVID cases.
Contributor Information
Ronelle Burger, Economics Department, Stellenbosch University, Stellenbosch, South Africa.
Carmen Christian, Economics Department, University of the Western Cape, Cape Town, South Africa.
Rene English, Division of Health Systems and Public Health, Global Health Department, Stellenbosch University, Tygerberg campus, Cape Town, South Africa.
Brendan Maughan-Brown, The Southern Africa Labour and Development Research Unit, University of Cape Town, Cape Town, South Africa.
Laura Rossouw, School of Economics and Finance, University of the Witwatersrand, Johannesburg, South Africa.
Authors’ Contributions
Ronelle Burger and Laura Rossouw were the primary data analysts. The team jointly drafted the methods, results, and discussion sections, and revised drafts.
Compliance with Ethical Standards
Funding Sources The study was not funded by any specific grant. Allan and Gill Gray Philanthropy, Michael and Susan Dell Foundation and the FEM Education Foundation funded the NIDS-CRAM surveys
Conflicts of Interest Ronelle Burger, Carmen Christian, Rene English, Brendan Maughan-Brown, and Laura Rossouw declare that they have no conflicts of interest.
Human Rights: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent: Informed consent was obtained from all individual participants included in the study.
Welfare of animals: This article does not contain any studies with animals performed by any of the authors.
Transparency statements
1. Study registration. This study was not formally registered as it was not required (not an RCT)
2. Analytic plan pre-registration. The analytical plan was not formally registered as it was not required (not an RCT).
3. Data availability: De-identified data from this study are available in a public archive: https://www.datafirst.uct.ac.za/dataportal/index.php/catalog/NIDS-CRAM/about
4. Analytic code availability. Analytic code used to conduct the analyses presented in this study are not available in a public archive. They may be available by emailing the corresponding author.
5. Materials availability. All materials used to conduct the study are available in a public archive: https://www.datafirst.uct.ac.za/dataportal/index.php/catalog/NIDS-CRAM/about
References
- 1. Miles DK, Stedman M, Heald AH. Stay at home, protect the national health service, save lives. Int J Clin Pract. 2020;75(3):e1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mandel A, Veetil VP. The economic cost of covid lockdowns: an out-of-equilibrium analysis. Econom Disast Climate Change. Available at SSRN. 2020;4(3):3588421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Acemoglu D, Chernozhukov V, Werning I, Whinston M. Optimal targeted lockdowns in a multi-group SIR Model. NBER Working Paper. 2020;826(62):1–57. [Google Scholar]
- 4. Rowthorn R, Maciejowski J. A cost–benefit analysis of the COVID-19 disease. Oxford Rev Econom Policy. 2020;36(1):S38–S55. [Google Scholar]
- 5. Coibion O, Gorodnichenko Y, Weber M. The cost of the COVID-19 crisis: lockdowns, macroeconomic expectations, and consumer spending. NBER Working Paper. 2020;27141. [Google Scholar]
- 6. Goolsbee A, Syverson C. Fear, lockdown, and diversion: comparing drivers of pandemic economic decline 2020. NBER Working Paper. 2020;27432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Albitar O, Ballouze R, Ooi JP, Sheikh Ghadzi SM. Risk factors for mortality among COVID-19 patients. Diabetes Res Clin Pract. 2020;166:108293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Promislow DEL. A Geroscience Perspective on COVID-19 Mortality. J Gerontol A Biol Sci Med Sci. 2020;75(9):e30–e33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Oster AM, Caruso E, DeVies J, Hartnett KP, Boehmer TK. Transmission dynamics by age group in COVID-19 hotspot counties—United States, April–September 2020. Morbid. Mortal. Weekly Rep. 2020;69(41):1494–1496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Monod M, Blenkinsop A, Xi X, et al. Age groups that sustain resurging COVID-19 epidemics in the United States. Science. 2021;371(6536). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chapman G, Loewenstein G. Why Americans are tiring of social distancing and hand-washing – 2 behavioral scientists explain. The Conversation. 2020. Available at https://theconversation.com/why-americans-are-tiring-of-social-distancing-and-hand-washing-2-behavioral-scientists-explain-139625. Accessibility verified November 18, 2020.
- 12. Eichler R, Levine R. The Performance-Based Incentives Working Group. Performance Incentives for Global Health: Potential and Pitfalls. Washington, DC: CGD Books; 2009:eabe8372. [Google Scholar]
- 13. Loewenstein G. Psychological factors affecting the success of measures to decrease the spread of COVID-19 [IBEN webinar]. 2020. Available at https://youtu.be/puQf0Eh3rr8. Accessibility verified April 13, 2021.
- 14. Loewenstein G. Experimental economics from the vantage‐point of behavioral economics. Econom J. 1999;109(453):25–34. [Google Scholar]
- 15. Jefferson T, Del Mar CB, Dooley L, et al. Physical interventions to interrupt or reduce the spread of respiratory viruses. Cochrane Database System Rev. 2020;11(11):CD006207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ali ST, Wang L, Lau EHY, et al. Serial interval of SARS-CoV-2 was shortened over time by nonpharmaceutical interventions. Science. 2020;369(6507):1106–1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Brauner JM, Mindermann S, Sharma M, et al. Inferring the effectiveness of government interventions against COVID-19. MedRxiv. 2021;371(6531):eabd9338. 10.1101/2020.05.28.20116129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Brooks JT, Butler JC, Redfield RR. Universal masking to prevent SARS-CoV-2 transmission-the time is now. JAMA. 2020;324(7):635–637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Eikenberry SE, Mancuso M, Iboi E, et al. To mask or not to mask: Modeling the potential for face mask use by the general public to curtail the COVID-19 pandemic. Infect Dis Model. 2020;5:293–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Greenhalgh T, Schmid MB, Czypionka T, Bassler D, Gruer L. Face masks for the public during the COVID-19 crisis. Bmj. 2020;369:m1435. [DOI] [PubMed] [Google Scholar]
- 21. Li T, Liu Y, Li M, Qian X, Dai SY. Mask or no mask for COVID-19: A public health and market study. PLoS One. 2020;15(8):e0237691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. López L, Rodó X. The end of social confinement and COVID-19 re-emergence risk. Nat Hum Behav. 2020;4(7):746–755. [DOI] [PubMed] [Google Scholar]
- 23. Lyu W, Wehby GL. Community use of face masks and COVID-19: Evidence from a natural experiment of state mandates in the US. Health Aff (Millwood). 2020;39(8):1419–1425. [DOI] [PubMed] [Google Scholar]
- 24. Prather KA, Wang CC, Schooley RT. Reducing transmission of SARS-CoV-2. Science. 2020;368(6498):1422–1424. [DOI] [PubMed] [Google Scholar]
- 25. Chughtaita AA, Seale H, MacIntyre CR. Effectiveness of cloth masks for protection against Severe Acute Respiratory Syndrome Coronavirus 2. Emerging Infect Dis. 2020;26(10):e200948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Gustafsson M. How does South Africa’s COVID-19 response compare globally? A preliminary analysis using the new OxCGRT dataset. Stellenbosch University Working Paper. 2020. [Google Scholar]
- 27. Barile JP, Guerin RJ, Fisher KA, et al. Theory-based behavioral predictors of self-reported use of face coverings in public settings during the COVID-19 Pandemic in the United States. Ann Behav Med. 2021;55(1):82–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. [dataset]* Spaull N, Burger R, Burger RP, et al. South Africa—National Income Dynamics Study—Coronavirus Rapid Mobile Survey 2020, Wave 2. DataFirst. 2020. Available at https://www.datafirst.uct.ac.za/dataportal/index.php/catalog/827. [Google Scholar]
- 29. [dataset]* Spaull N, Burger R, Burger RP, et al. South Africa—National Income Dynamics Study—Coronavirus Rapid Mobile Survey 2020, Wave 1. DataFirst. 2020. Available at https://www.datafirst.uct.ac.za/dataportal/index.php/catalog/817. [Google Scholar]
- 30. [dataset]* South African Labour Development Research Unit, University of Cape Town. South Africa—National Income Dynamics Study 2017, Wave 5. DataFirst. 2018. Available at https://www.datafirst.uct.ac.za/dataportal/index.php/catalog/712 [Google Scholar]
- 31. Kerr A, Ardington C, Burger R. Sample design and weighting in the NIDS-CRAM survey. SALDRU Working Paper. 2020. [Google Scholar]
- 32. Mediahack Collective. District Dashboard. 2020. Available at https://mediahack.co.za/datastories/coronavirus/districts/
- 33. Tang CS, Wong CY. Factors influencing the wearing of facemasks to prevent the severe acute respiratory syndrome among adult Chinese in Hong Kong. Prev Med. 2004;39(6):1187–1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the Health Belief Model. Health Educ Q. 1988;15(2):175–183. [DOI] [PubMed] [Google Scholar]
- 35. Janz NK, Becker MH. The Health Belief Model: a decade later. Health Educ Q. 1984;11(1):1–47. [DOI] [PubMed] [Google Scholar]
- 36. Adams ML, Katz DL, Grandpre J. Population-Based estimates of chronic conditions affecting risk for complications from Coronavirus Disease, United States. Emerg Infect Dis. 2020;26(8):1831–1833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Jordan RE, Adab P, Cheng KK. COVID-19: risk factors for severe disease and death. Bmj. 2020;368:m1198. [DOI] [PubMed] [Google Scholar]
- 38. [dataset]* South African Labour Development Research Unit, University of Cape Town. South Africa—National Income Dynamics Study 2014—2015, Wave 4. DataFirst. 2016. Available at https://www.datafirst.uct.ac.za/dataportal/index.php/catalog/570 [Google Scholar]
- 39. Hamer M, Gale CR, Kivimäki M, Batty GD. Overweight, obesity, and risk of hospitalization for COVID-19: A community-based cohort study of adults in the United Kingdom. Proc Natl Acad Sci U S A. 2020;117(35):21011–21013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Lighter J, Phillips M, Hochman S, et al. Obesity in patients younger than 60 Years is a risk factor for COVID-19 hospital admission. Clin Infect Dis. 2020;71(15):896–897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Popkin BM, Du S, Green WD, et al. Individuals with obesity and COVID‐19: A global perspective on the epidemiology and biological relationships. Obes Rev. 2020;21(11):e13128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Zhai Z. Facial mask: A necessity to beat COVID-19. Build Environ. 2020;175:106827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Nogrady B. What the data say about asymptomatic COVID infections. Nature. 2020;587(7835):534–535. Available at https://www.nature.com/articles/d41586-020-03141-3 [DOI] [PubMed] [Google Scholar]
- 44. Lewis D. COVID-19 rarely spreads through surfaces. So why are we still deep cleaning? Nature. 2021;590(7844):26–28. Available at https://www.nature.com/articles/d41586-021-00251-4 [DOI] [PubMed] [Google Scholar]
- 45. NPR Material. CDC “clarifies” guidance on surface spread of COVID-19. Medical Brief. 2020. Available at https://www.medicalbrief.co.za/archives/cdc-clarifies-guidance-on-surface-spread-of-covid-19/. Accessibility verified January 30, 2021.
- 46. Centers for Disease Control and Prevention. COVID-19: Considerations for wearing face masks. 2021. Available at https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/cloth-face-cover-guidance.html. Accessibility verified January 30, 2021.
- 47. Masks4all. What countries require or recommend masks in public? 2020. Available at https://masks4all.co/what-countries-require-masks-in-public/. Accessibility verified January 30, 2021.
- 48. Burgess A, Horii M. Risk, ritual and health responsibilisation: Japan’s ‘safety blanket’ of surgical face mask-wearing. Sociol Health Illness. 2012;34(8):1184–1198. [DOI] [PubMed] [Google Scholar]
- 49. Condon BJ, Sinha T. Who is that masked person: the use of face masks on Mexico City public transportation during the Influenza A (H1N1) outbreak. Health Policy. 2010;95(1):50–56. [DOI] [PubMed] [Google Scholar]
- 50. Lau JT, Griffiths S, Choi KC, Lin C. Prevalence of preventive behaviors and associated factors during early phase of the H1N1 influenza epidemic. Am J Infect Control. 2010;38(5):374–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Lau JTF, Kim JH, Tsui H, Griffiths S. Anticipated and current preventive behaviors in response to an anticipated human-to-human H5N1 epidemic in the Hong Kong Chinese general population. BMC Infect Dis. 2007;7(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Lau JTF, Griffiths S, Au DWH, Choi KC. Changes in knowledge, perceptions, preventive behaviors and psychological responses in the pre-community outbreak phase of the H1N1 epidemic. Epidemiol Infect. 2011;139(1):80–90. [DOI] [PubMed] [Google Scholar]
- 53. Ferng YH, Wong-McLoughlin J, Barrett A, Currie L, Larson E. Barriers to mask wearing for influenza-like illnesses among urban Hispanic households. Public Health Nurs. 2011;28(1):13–23. [DOI] [PubMed] [Google Scholar]
- 54. Chia SE, Koh D, Fones C, et al. Appropriate use of personal protective equipment among healthcare workers in public sector hospitals and primary healthcare polyclinics during the SARS outbreak in Singapore. Occup Environ Med. 2005;62(7):473–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Taylor M, Raphael B, Barr M, Agho K, Stevens G, Jorm L. Public health measures during an anticipated influenza pandemic: Factors influencing willingness to comply. Risk Manag Healthc Policy. 2009;2:9–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Pereira-Ávila FMV, Lam SC, Góes FGB, et al. Factors associated with the use and reuse of face masks among Brazilian individuals during the COVID-19 pandemic. Rev Lat Am Enfermagem. 2020;28:e3360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Fodjo JN, Pengpid S, De Moura Villela EF. Mass masking as a way to contain COVID-19 and exit lockdown in low-and middle-income countries. J Infect. 2020;81(3):e1–e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Brenner PS, DeLamater J. Lies, damned lies, and survey self-reports? identity as a cause of measurement bias. Soc Psychol Q. 2016;79(4):333–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Brenner PS, DeLamater J. Measurement directiveness as a cause of response bias: Evidence from two survey experiments. Sociol Methods Res. 2016;45(2):348–371. [Google Scholar]
- 60. Van Der Westhuizen HM, Kotze K, Tonkin-Crine S, Gobat N, Greenhalgh T. Masks for COVID-19: From medical intervention to social practice. Bmj. 2020;370:m3021. [DOI] [PubMed] [Google Scholar]
- 61. Betsch C, Korn L, Sprengholz P, et al. Social and behavioral consequences of mask policies during the COVID-19 pandemic. Proc Natl Acad Sci U S A. 2020;117(36):21851–21853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Mantzari E, Rubin GJ, Marteau TM. Is risk compensation threatening public health in the COVID-19 pandemic? Bmj. 2020;370:m2913. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.