Learning point for clinicians
The mRNA-based COVID-19 vaccine causes flare of glomerulonephritis, especially in patients with IgA nephropathy. Clinicians should be aware that disease activity can be exacerbated after vaccination not only in patients who have already been diagnosed with IgA nephropathy but also in patients who have an undiagnosed IgA nephropathy.
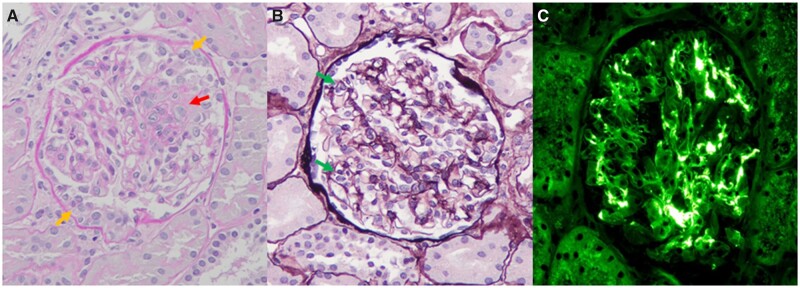
A 17-year-old Japanese male presented to the nephrology clinic with high-grade fever, headache and macrohaematuria. Five months ago, urine dipstick revealed microhaematuria (2+). Although he denied any symptoms following the first dose of Pfizer vaccine against coronavirus disease 2019 (COVID-19) 3 weeks earlier, he had high-grade fever, headache and macrohaematuria 12 h after the second dose for 2 days. Only the fever resolved. Laboratory tests revealed elevated C-reactive protein (CRP) level (2.41 mg/dL, normal <0.15) with normal serum creatinine (SCr) level (0.70 mg/dL, normal 0.65–1.07). Urinalysis showed marked proteinuria (1.0 g/gCr, normal <0.3) and haematuria (>100 red blood cell/high power field (RBC/HPF), normal <5). One week later, CRP resolved, but proteinuria (1.4 g/gCr) and microhaematuria (>100 RBC/HPF) persisted. A renal biopsy was then performed. Light microscopy revealed mesangial cell and matrix proliferation, endocapillary hypercellularity and crescents (Figure 1A and B). Immunofluorescence staining revealed predominantly IgA and C3 deposits with weak IgG deposits in the mesangial areas (Figure 1C). The patient was finally diagnosed of IgA nephropathy. Two months later, proteinuria and microhaematuria persisted, so tonsillectomy with steroid pulse therapy was performed.
Figure 1.
Histological findings of a renal biopsy specimen. (A and B) Renal biopsy specimen reveals mesangial cell proliferation (red arrow), endocapillary hypercellularity (green arrows) and crescents (yellow arrows) (A: Periodic acid-Schiff staining, B: Periodic acid-methenamine silver staining, original magnification ×200). (C) Immunofluorescent staining shows IgA deposits in mesangial area (original magnification ×200).
mRNA vaccines trigger more potent immune responses and are associated with higher rates of glomerulonephritis than other vaccines.1 Recently, there are many reports on either new diagnoses or relapses of glomerulonephritis after COVID-19 vaccinations.1 IgA nephropathy was the most common glomerulonephritis associated with COVID-19 vaccination.1 Despite the lack of subjective symptoms, the patient had an abnormal pre-vaccination urinalysis. Therefore, we suspected that IgA nephropathy had already existed prior to the vaccination and was exacerbated by it. Post-vaccination glomerulonephritis relapse is caused by the upregulation of cell-mediated and/or antibody-mediated immune response(s).1 The cell-mediated response results from the upregulation of CD4+ and CD4+ T cells accompanied by an increased interferon-γ secretion.1 In this case, a high CRP level was observed 2 days post-vaccination, indicating an IgA nephropathy flare with macroscopic haematuria accompanied by severe inflammation. The COVID-19 vaccine is hypothesized to result in the ‘flare’ of an existing disease rather than the development of new IgA antibodies.1 We think this case supports the above hypothesis.
All reported patients with IgA nephropathy post-COVID-19 vaccination developed gross haematuria, with renal biopsy findings of active lesions, including endocapillary hypercellularity, leukocyte infiltration, fibrinoid necrosis and crescents.1–3 An investigation of 10 patients with IgA nephropathy post-COVID-19 vaccination revealed acute kidney injury (AKI) and massive proteinuria in three (30%) and four (40%) cases, respectively.2 AKI and proteinuria affect both renal and life prognoses; thus, they have not only short-term but also long-term adverse effects. Another review revealed that 3 of 16 patients (19%) required intensive treatment with immunosuppressive drugs,1 which may cause susceptibility to infection. The rates of systemic adverse events following the first and second doses of COVID-19 mRNA vaccines were 54.9% and 79.4%, respectively.4 Large-scale intervention studies prior to the general indication of vaccination did not include patients with autoimmune disorders, including renal disease.4,5 In those studies, there were no data confirming blood tests, such as SCr, CRP, or urinalysis 1–3 days post-vaccination, in which gross haematuria in IgA nephropathy is often seen.4,5 After COVID 19 vaccination in clinical practice these days, blood testing and urinalysis are rarely performed even if systemic adverse events occur. Therefore, it is presumed that there has been no confirmation of any exacerbation of microhaematuria, proteinuria, or AKI, except when gross haematuria is clearly noticeable. The general public already knew that the side effects of vaccines were more frequent in younger people, while the corona infections were more likely to become more severe in older people. Although unconfirmed, clinicians should be aware of the potential exacerbation of glomerulonephritis post-vaccination.
Consent
Informed consent was obtained from patient for the publication of this article.
Conflict of interest. None declared.
References
- 1. Klomjit N, Alexander MP, Fervenza FC, Zoghby Z, Garg A, Hogan MC, et al. COVID-19 vaccination and glomerulonephritis. Kidney Int Rep, doi: 10.1016/j.ekir.2021.09.008 [Epub 6 October 2021]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bomback AS, Kudose S, D'Agati VD. De novo and relapsing glomerular diseases after COVID-19 vaccination: what do we know so far? Am J Kidney Dis 2021; 78:477–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kudose S, Friedmann P, Albajrami O, D'Agati VD. Histologic correlates of gross hematuria following Moderna COVID-19 vaccine in patients with IgA nephropathy. Kidney Int 2021; 100:468–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Baden LR, El Sahly HM, Essink B, Kotloff K, Frey S, Novak R, et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med 2021; 384:403–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dagan N, Barda N, Kepten E, Miron O, Perchik S, Katz MA, et al. BNT162b2 mRNA Covid-19 vaccine in a nationwide mass vaccination setting. N Engl J Med 2021; 384:1412–23. [DOI] [PMC free article] [PubMed] [Google Scholar]