Abstract
India and the United States have both witnessed a high burden of COVID-19 infections since the pandemic was declared in early 2020. However, the COVID-19 restrictions have met with mixed responses in India and the US. Despite recommendations to continue social isolation and personal hygiene measures, India has not been able to curb the rise in daily cases. Our findings demonstrate the difference in the manner by which India and the US differ in their emergency handling of patients. We conducted a thorough review of the existing protocols and data concerning emergency responses in India and the US. The triage and care of suspected COVID-19 positive patients is different across India and the US. We find that there is a shortage of oxygenation, vaccination and other essential supplies in India. Further, the US is able to triage patients through telemedicine and EMS before suspected COVID-19 patients arrive, which is less prevalent in India. Our study identifies the importance of the emergency department (ED) as a critical contributor to the prevention and care of suspected and confirmed COVID-19 patients. Hospitals in India have been struggling to accommodate a huge influx of patients during its second wave with the ED playing a key link in their COVID-19 response.
Keywords: Emergency department, Emergency medicine, COVID-19, India, United States, Triage, Telemedicine, Personal protective equipment, Infection prevention control
Highlights
-
•
India and the US have both witnessed a high number of COVID-19 cases since the dawn of the pandemic.
-
•
The South East Asian country as compared to the US applied different emergency handling protocols during the different waves.
-
•
With this review, we synthesize protocols and data concerning emergency responses across India and the US.
-
•
We identify that the triage and care of suspected patients is reliant on the oxygenation, vaccination, and other supplies.
-
•
This study presents a succinct overview of the critical contributors to the prevention and care of suspected and confirmed COVID-19 patients.
Key messages
What is already known about this subject?
India and the US have both witnessed a high number of COVID-19 cases since the dawn of the pandemic in early 2020. Despite recommendations by concerned authorities, the South East Asian country as compared to the US applied different emergency handling protocols during the previous waves.
What does this study add?
With this review, we present a synthesis of existing and previous protocols and data concerning emergency responses across India and the US. We identify that the triage and care of suspected patients is reliant on the oxygenation, vaccination, and other supplies, which is associated to a myriad of other factors including social isolation and integrated health prognoses indicators.
How might this impact on clinical practice or future developments?
This study presents a succinct overview of the critical contributors to the prevention and care of suspected and confirmed COVID-19 patients. Since the onset of the pandemic, both countries have applied subjective measures to curb the rise in the number of cases. The central measure that developing countries ought to focus on are the emergency medicine protocols, as with any other nation that has efficiently controlled morbidity and mortality due to COVID-19.
1. Background
In 2019, we witnessed the deadly emergence of the coronavirus disease (COVID-19), now known to be caused by the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). The outbreak of this virus was initially designated as a “public health emergency of international concern (PHEIC), which was then followed by declaring COVID-19 as a global pandemic on March 11, 2020. The COVID-19 pandemic is the biggest public health crisis in the last century. The pandemic has intensely challenged the healthcare infrastructure across the world, with a heavier impact on low- and middle-income countries (LMICs) including India. We must recognize the urgent need to improve healthcare infrastructure, especially in LMICs. Further, this pandemic has highlighted the need for developing novel testing facilities, preparing human resources for future events, and adequate support for frontline healthcare workers [1].
India is the second-most densely populated country in the world and has witnessed one of the highest burdens of COVID-19 cases. As a result, the COVID-19 crisis has created an intensely stressful situation for the Indian healthcare system. The Ministry of Health and Family Welfare in India confirmed a total of 266,598 COVID-19 cases on June 9, 2020, from 32 states. Furthermore, India reported 7471 COVID-19 related deaths, which translated into a case-fatality rate of 2.8%, not accounting for the under-reported cases [2]. The World Health Organization (WHO) reported around 378,075 new cases in India daily. This accounted for about 47% of new COVID-19 cases reported worldwide and approximately 276 daily COVID-19 daily cases per million populations [3,4]. The overwhelming burden in cases overworked the entire healthcare system in India, especially the emergency departments (EDs). Emergency and critical care systems are suffering immensely from a lack of essential resources. Not only are resources scarce, but healthcare workers have also been suffering from an overload of work, severe working conditions, and the high risk of contracting and transmitting COVID-19, due to the scarcity of personal protective equipment (PPE). All of this together with lack of funding adds to the substantial burden ED's have had to face in India [5].
The rapid spread of COVID-19 heavily influenced healthcare systems across the United States (US) as well, requiring EDs to adapt quickly to the overwhelming number of cases presented. The US also witnessed extreme devastation and mass casualties during the peak of the COVID-19 surge. In the earlier stages of the COVID-19 pandemic, New York City Health and hospitals recognized the imperative to respond in real-time to rapidly evolving clinical, operational, and communication needs across its hospitals to ensure that all New Yorkers suffering from COVID-19 would have access to emergency, inpatient, and critical care services [6]. On March 13, 2020, the US declared a national state of emergency due to COVID-19. From March 29 to April 25, 2020, there was a noticeable decline in COVID-19 related ED visits in the US by 42%. After this decline, there was a rise in COVID-19 related ED visits throughout July 2020, but at lower levels compared to the previous year. Towards the end of 2020 up until January 2021, COVID-19 ED visits fell to around 25% of that from pre-pandemic levels [7].
As witnessed from previous infectious disease outbreaks in the last two decades, EDs around the world have had to take the lead in medically responding to the pandemic, thus making EDs the first point of contact for any suspected cases and playing a crucial role in termination in transmission [8]. This review intends to give a comparison of ED responses in India and the US towards the COVID-19 pandemic for the evaluation and management of patients, identification of challenges, and implications for emergency medicine physicians.
2. ED protocols in India and USA
Hospitals and healthcare facilities have limited manpower and infrastructure to accommodate the high burden of COVID-19 infected patients. It is thus important to establish protocols for the optimization of resources. Infection prevention control (IPC) is critical for managing patients with suspected COVID-19 infection. As such, upon arrival at the ED of any hospital in India, it is recommended that these patients wear a triple-layered surgical mask and be kept 1 m away from other patients. Good hand hygiene practice and the use of personal protective equipment (PPE) (i.e. triple-layer surgical masks, eye protection, gloves, and gowns) ought to be initiated by healthcare professionals, and droplet and contact precautions should also be applied [9]. Should aerosol-generating procedures be necessary, airborne precautions should also be taken. It is also entirely possible that COVID-19 cases are picked up by outpatient departments or primary care services including telemedicine[10]. Of note, demand for telemedicine has greatly increased in the past year, with the National Teleconsultation Service of the Ministry of Health and Family Welfare, and major hospitals such as the Apollo Hospitals Group and Amrita Hospitals, being active providers [11].
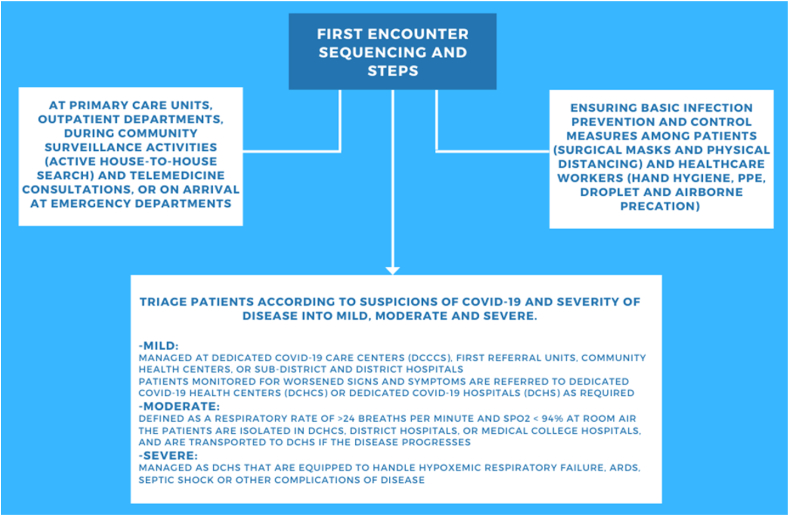
When detected in such instances, mild COVID-19 cases are first managed at Dedicated COVID Care Centers (DCCCs), First Referral Units, Community Health Centers, or sub-district and district hospitals. Patients are monitored for worsening signs and symptoms which might prompt an urgent referral to a Dedicated COVID Health Centre (DCHC) or Dedicated COVID Hospital (DCH). As of 11 May 2020, 7740 dedicated COVID-19 health facilities (DCCCs, DCHCs, and DCHs) have been identified in 483 districts [12]. The Times of India reported that this number has since risen to 26 DCHs with 757 ICU and 1868 isolation beds as of 21 Apr 2021 [13]. It is recommended that patients with moderate COVID-19 infection be isolated in DCHCs, District Hospitals, or Medical College Hospitals to contain virus transmission. The defining clinical assessment parameters for moderate COVID-19 infection are a respiratory rate (RR) greater than 23 breaths per minute and oxygen saturation (SpO2) of less than 94% on room air (range 90–94%). Transportation to a DCH is recommended should the disease progress. Patients diagnosed with severe COVID-19 infection will be managed in DCHs equipped to handle decompensation due to hypoxemic respiratory failure, acute respiratory distress syndrome (ARDS), or septic shock. A standardized protocol for COVID-19 patient management at emergency departments in India is shown in Fig. 1.
Fig. 1.
A flowchart of emergency department standardized COVID-19 protocols in India.
The US recognizes that emergency medical services (EMS) personnel are critical in responding to calls for medical assistance, the triaging of patients, and the provision of emergency treatment and transport for the ill and injured. Thus, in addition to enforcing IPC practices amidst the COVID-19 pandemic, the CDC currently also recommends closer coordination among 911 Public Safety Answering Points/Emergency Communication Centers (PSAP/ECCs), and the development of modified caller queries in conjunction with an EMS medical director (14). Given so, 911 PSAP/ECCs should now first determine whether an incoming call concerns a potential COVID-19 patient, by asking for the signs and symptoms of COVID-19, and the patient's recent contact history [14,15]. Suspicion for a COVID-19 infection should be communicated to the EMS personnel before his/her arrival on the scene, following which the number of EMS personnel exposed to the patient should be limited, and appropriate PPE, including but not limited to respirators, goggles, or a face shield, gloves, and gowns, should be donned. Should the patient require further evaluation and management, the EMS personnel should notify the receiving healthcare facility ahead of time for appropriate infection control precautions to be taken before the patient's arrival [9,14,15]. Consistent with IPC measures implemented in India, the CDC also recommends hand hygiene, routine use of PPE, droplet and contact precautions, and airborne precautions should aerosol-generating procedures be performed. Universal source control measures, such as the use of facemasks to cover a person's mouth and nose, and physical distancing of at least 6 feet between people, should be implemented at all times [9,14,15].
3. Changed dynamics and emergency medicine physicians’ perspectives
According to the report of Global Health Security Index (2019), India ranked 67th while the US has ranked second out of 195 countries in terms of emergency preparedness and capacity [16]. Globally, healthcare systems have been constrained, despite trying to adapt to the ongoing COVID-19 pandemic [17,18]. ED physicians have been observed to be appropriate doctors in medical care for severe patients with COVID-19 with their ability to handle critical care in a high-pressure environment [19]. India has around 926,000 doctors serving 1.3 billion; out of them less than 20,000 doctors are trained in pulmonology, anesthesiology, critical care and emergency medicine—the key departments require respiratory care and active life-saving intervention. National Study of emergency physician workforce 2020 has reported 48,835 clinically active US emergency physicians for a population of 311.1 million in the US [20]. Innovative cost-effective strategies to address human resource crunch like the ad-hoc appointment of allied healthcare professional in emergency care along with temporary deployment of healthcare professional from the private sector was done in India to handle the patient load.
Considering the unknown risk of transmission and severity of disease, the provision of PPE is a crucial component in infection control strategies for EM health care professionals to safely care for suspected and confirmed COVID-19 patients. Importantly, PPE is required for the protection of patients, the public, and the health care community [21,22]. Currently tackling this pandemic, emergency physicians are at grave risk of acquiring COVID-19, especially from aerosolizing procedures such as intubation required by 3.2% of diseased patients [[23], [24], [25]]. Sampling and heavy paperwork at the ER department are potential sources of infection as well [[26], [27], [28]]. The main hindrance to halt the transmission of COVID-19 infection exclusively lies in a prompt and valid use of complete PPE covering head to toe inclusive of gowns, face masks, face shields, goggles, air-purifying respirators, and gloves [29,30]. Despite being an integral right for access to apt PPE, the two largest economies of the world including India and the US have faced scarcity of PPE during this pandemic [31].
A survey done in three major states of India, among 392 HCWs, had reported inadequate availability of PPE in most healthcare settings. The scarcity of PPEs in India had obligated front-line health care workers into extended and repeated use of PPE, increasing their risk of getting infected [32]. As per a survey conducted in May 2020 in the US, 87% of Nurses reported reusing a single-use disposable mask or N95 respirator reflecting PPE Shortage [16]. Out of these 27% of nurses had been exposed to confirmed COVID-19 patients without wearing appropriate PPE. This has been reflected in the mortality burden from HCWs in both countries; same time both countries have started in-house manufacturing of PPE reducing their dependency on other PPE manufacturing countries. Stopping the ban on the export of PPE, investing in manufacturing, procuring, and building up an inventory of necessary PPE supplies has helped India avert the crisis of jeopardizing its health workers' security.
4. Changed dynamics and emergency medicine physicians’ perspectives
A survey conducted in healthcare workers treating patients with COVID-19 in NYC has reported experiencing substantial distress from fears of COVID-19 transmission, clinical challenges, and perceived lack of control, to concerns about family and home life with large proportions screening positive for acute stress, depressive symptoms, and sleep disturbances [[33], [34], [35]]. Indian HCWs have also reported being facing mental issues such as stress, anxiety, and sleep-related problems such as insomnia and burnout [36]. Considering India's low doctor-to-patient ratio, the increase in COVID-19 patients has proved extremely overwhelming for its health personnel. Scheduling a roster for healthcare staff might ensure a balanced workload and rest periods for health workers. With the ongoing continued patient influx of COVID 19, an emergency physician from India and the US are working for long hours, facing a daily extra patient load. Despite long working hours, ED physicians are partially relieved with help of physicians from other specialties. This situation has posed a new challenge of vulnerable emergency physician staffing and rostering vulnerable emergency physician populations with increased risk of serious disease and death from COVID-19 include physicians at older ages, those with chronic medical conditions including cardiac and pulmonary diseases, immunosuppression, and pregnancies.
Due to the higher susceptibility to infection, health workers more than 60 years of age and those having comorbidities are advised to be engaged in consultation, coordination, and administrative tasks. Given the shortage of beds, ventilators, and medicine in India, Indian ED physicians have surfaced violence by patients and attendants. This may impact the morale of Indian doctors, with imparting physical and mental burdens secondary to the pandemic. The Indian government approved an ordinance that makes violence against healthcare workers a non-bailable offense, punishable by up to seven years’ imprisonment, amid concerns that the COVID-19 pandemic has stirred an upsurge of such targeted violence. In the US, implemented measures included optimizing the workforce, increasing backup call system, adjusting shifts based on patient arrival times, volume, and surge predictions, minimizing exposure to COVID-19, and reducing PPE use through telemedicine, huddles, creating lower risk emergency department care areas, and standardizing intubations to limit exposure [37].
5. A deliberation of patient and familial perspectives
The spread of misinformation fueled by fear and stigmatization of people suffering from or suspected of acquiring COVID-19 infection could result in under-reporting of the actual number of cases [38]. The feelings of fear and anxiety during the pandemic may have stemmed from the uncertainty related to the transmission and spread of disease, infodemics and misinfodemics, exposure to the infection, social distancing, and travel restrictions [39,40]. The COVID-19 pandemic has not only presented as an epidemiologic crisis but also a psychological one. The distress of living in conditions like isolation, unemployment, and financial issues, and fear of losing your loved ones can adversely affect mental well-being. Some aspects of the pandemic that seem to affect people to a greater degree include separation from loved ones, loss of freedom, and feelings of vulnerability and helplessness. Several studies have highlighted the impact on the psychological health of the population subgroups that have a higher chance of exposure, including children, school/college-going students, and healthcare workers. The pandemic has increased the prevalence of anxiety, depression, obsessive behaviors, panic attacks, hoarding, paranoia, and post-traumatic stress disorder (PTSD) in the long term [41].
When assessing the suicide incident during the pandemic in India, a higher rate of suicide was associated with fear of getting infected with COVID-19, followed by the financial crisis, loneliness, social boycott and quarantine, employment-related stress, and problems due to lockdown. There is a need for widespread access to telehealth services to overcome the psychological impact [42]. Social distancing is difficult to carry out for people that are underprivileged and residing in slums or small places. The lockdown has forced a large number of workers who had migrated to big cities in search of livelihood and employment opportunities to travel back to their native villages. It has been documented that over 50 million people have migrated from Bihar, Punjab, Assam, Odisha, Madhya Pradesh, Uttar Pradesh, Rajasthan, and West Bengal to Delhi and Maharashtra for employment. The rise of psychosocial issues is inevitable among these workers and their families [43].
Under normal circumstances, the available beds in India were 3.2 per 1000 for the rural population and 11.9 per 1000 for the urban population-figures that desperately need to increase to put up with the growing number of COVID-19 patients [44]. Decreased hospital bed capacity has resulted in extended waiting time and delayed patient care. Disruption and discrepancies have also been reported for treatment and vaccination of other diseases like pneumonia, tuberculosis, meningitis, whooping cough, diphtheria, tetanus, and Hepatitis B. Delay in out-patient services such as dialysis and chemotherapy have also been noticed. To accommodate larger populations, public places like educational institutions, stadiums and large grounds, hotels, etc. were temporarily turned into COVID-19 facilities and isolation wards [45].
The US hospitals in at least 25 states suffered from a critical shortage of healthcare workers including doctors, nurses, and other paramedical staff as the number of cases increased throughout the US. Many severely ill patients had to travel very long distances in search of an available bed. Shortage of hospital staff was reported in states including Alabama, Michigan, Minnesota, Wisconsin, Kansas, Utah, Oklahoma, Ohio, Missouri, Illinois, New Mexico, Texas, Tennessee, North and South Dakota, Nebraska, Colorado, Wyoming, Arkansas, Indiana, Georgia, California, Montana, and South Carolina. These shortages were primarily caused by overwhelming numbers of patients as well as doctors and paramedical staff being infected with or exposed to COVID-19 [46]. While the vaccination roll-out is ongoing in both India and the US, it is extremely important to recognize symptomatology of mental health diseases to easily identify them early on and to seek social support.
6. Implications for public health and healthcare workers
Emergency medical and critical care services are considered as a gateway for universal health care access for major flow of patients, especially for inpatient care in the second & tertiary level of infrastructure [47,48]. Considering this entry point, ED services might play a remarkable role as architecture and implementer for effective approaches and modus operandi against COVID-19 in routine practice [49,50]. Given the planned new revised SOP for emergency medicine triage, strict adherence to these safety procedures shall be advocated to prevent further disease clustering. HCW from ED has been first-level health care delivery for severe pandemic cases with knowing the severity of COVID disease acted as a barricade, preparing the rest of the health care system to face challenges of this COVID Pandemic [8]. Virtual teleconsultations, triage mobile help services, and Compliance with CDC infection and prevention control guidance has helped both nations to reduce COVID Pandemic after an early wave of COVID [45]. Indian EMD's, similar to other LMICs, are still in the preliminary phase with a shortfall of proper emergency facilities with manpower crunch. Along with these overloaded EMDs with patient surges, shortage of beds, oxygen concentrators have alarmed the system to reconsider investing in public healthcare budgets [51,52]. HCWs from both nations were frustrated about people's attitudes about noncompliance with safe distancing and mask-wearing protocols [53,54]. Along with physical exhaustion, burnout and stress were higher among health care workers in both nations-reflecting a dire need to be diligent about their mental health [55,56].
For both countries, healthcare workers have confronted the issue of lack of relevant PPE compromising their safety [52,57,58]. Considering the severity of COVID-19 disease and transmission risk, HCWs were expected to be provided with PPE and prophylactic vaccinations. Safety and security for physical and mental health, clinical and illness insurance coverage ideally should have been prioritized. Both nations have tried to tackle this pandemic through preparedness, modified protocol for triage, treatment, and including intubation protocol [59,60]. Infection control and airborne precaution in India possibly might have reduced the transmission of COVID-19. Capacity building of staff, reorganization of EMDs, strengthening of existing resources and SOP, refilling of existing vacant health care positions have been proved instrumental to tackle further epidemics [[61], [62], [63]]. Innovative approaches by the US including Public Safety Answering Points/Emergency Communication Centers helped to reduce the patient contact time ED Managers and health care physicians shall be actively involved in health care policy forms and yearly health care budgeting. This pandemic has helped for futuristic thought for capacity building of EMDs. Individual EDs from different geographical conditions from the US and India shall consider writing their experiences and innovation for prompt recognition and diagnosis, segregation, and treatment of Symptomatic cases.
7. Conclusion
Both India and the United States followed CDC recommendations and mandated their communities to wear masks and maintain social distancing. However, this was challenging for India as many are unable to socially distance themselves due to their living conditions in slums or close living spaces. Because of this, COVID-19 has mostly affected crowded localities and cities of India. As COVID-19 restrictions remain and cases continue to rise in India, there has been an increase in suicide rates. Fear and stress are rising in India as the people face loneliness, financial crises, pressure to quarantine, and the worry of decreasing available beds in hospitals. India and the United States had similar approaches to protect their population against the growing incidence of COVID-19 through mandating PPE use and promoting infection control. However, the two countries differ in their triage and care of suspected COVID-19 positive patients due to healthcare infrastructure differences. The US can triage through telemedicine and EMS before arrival to the hospital. However, India lacks countrywide access to telemedicine services and has recently had an increase in migration to the urban cities, meaning that overcrowding is an essential contributor. This is important because the ED plays a primary role in the prevention and isolation of COVID-19. In the US, patients can be diagnosed with COVID-19 before their arrival at the hospital and precautions can be made which may not be common for their Indian counterparts. Finally, there is an increase in the emergency room waiting times, subsequent delay of care, and potential spread from a COVID-19 positive patient, as hospitals in India struggle to accommodate such a large population.
Provenance and peer review
Not commissioned, externally peer reviewed.
Sources of funding
None acquired.
Ethical approval
Not required.
Consent
No human or animal subjects were involved.
Author contribution
Zouina Sarfraz and Azza Sarfraz contributed equally in conceptualizing, analysing and writing the paper. Muzna Sarfraz, Namrata Hange Farah A. Chohan, Hanyou Loh, Claire Stringfellow, Esha Jain, and Miguel Felix contributed in writing and reviewing. Ivan Chérrez-Ojeda supervised the study.
Registration of research studies
-
1.
Name of the registry: Not applicable
-
2.
Unique Identifying number or registration ID: Not applicable
-
3.
Hyperlink to your specific registration (must be publicly accessible and will be checked): Not applicable
Guarantor
Zouina Sarfraz and Azza Sarfraz are co-guarantors of the study.
Declaration of competing interest
None to disclose.
Acknowledgments
We would like to acknowledge Jack Michel MD for his pursuits in promoting scholarly research activities.
Contributor Information
Zouina Sarfraz, Email: zouinasarfraz@gmail.com.
Azza Sarfraz, Email: azza.sarfraz@aku.edu.
Ivan Cherrez-Ojeda, Email: ivancherrez@gmail.com.
References
- 1.Mitra P., Misra S., Sharma P. COVID-19 pandemic in India: what lies ahead. Indian J. Clin. Biochem. 2020 doi: 10.1007/s12291-020-00886-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pal R., Yadav U. COVID-19 pandemic in India: present scenario and a steep climb ahead. J. Prim. Care Community Heal. 2020 doi: 10.1177/2150132720939402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization (WHO) Novel coronavirus disease (COVID-19) situation update report- 68. https://cdn.who.int/media/docs/default-source/wrindia/situation-report/india-situation-report-68.pdf?sfvrsn=8d7c2076_4 n.d.
- 4.Omer S.B., Malani P., Del Rio C. The COVID-19 pandemic in the US: a clinical update. JAMA, J. Am. Med. Assoc. 2020 doi: 10.1001/jama.2020.5788. [DOI] [PubMed] [Google Scholar]
- 5.Golechha M. India should ramp up its emergency medicine and critical care infrastructure to combat COVID-19. Postgrad. Med. J. 2021 doi: 10.1136/postgradmedj-2020-138249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Uppal A., Silvestri D.M., Siegler M., Natsui S., Boudourakis L., Salway R.J., Parikh M., Agoritsas K., Cho H.J., Gulati R., Nunez M., Hulbanni A., Flaherty C., Iavicoli L., Cineas N., Kanter M., Kessler S., Rhodes K.V., Bouton M., Wei E.K. Health Aff; 2020. Critical Care and Emergency Department Response at the Epicenter of the Covid-19 Pandemic. [DOI] [PubMed] [Google Scholar]
- 7.Adjemian J., Hartnett K.P., Kite-Powell A., DeVies J., Azondekon R., Radhakrishnan L., Santen K.L. va, Rodgers L. MMWR Surveill. Summ; 2021. Update: COVID-19 Pandemic–Associated Changes in Emergency Department Visits — United States, December 2020–January 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Heymann E.P., Exadaktylos A. How the COVID-19 pandemic illustrated the importance of emergency medicine, and its vital role as a pillar of the healthcare system. Emerg. Med. J. 2020 doi: 10.1136/emermed-2020-209735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mohfwgovin . Mohfw; 2020. Revised Guidelines on Clinical Management of COVID – 19. [Google Scholar]
- 10.Ramkumar P.S. 2011. Tele-Health in India, Landscape of Tele-Health Infrastructure at Points-Ofservice in India. [Google Scholar]
- 11.Indian Medical Council Telemedicine practice guidelines: enabling registered medical practitioners to provide healthcare using telemedicine. Indian Med. Counc. 2020 [Google Scholar]
- 12.PTI Agency . ETHealthworld; 2020. 7,740 Dedicated Covid-19 Health Facilities in 483 Districts Identified: Health Ministry.https://health.economictimes.indiatimes.com/agency/87654375/PTI [Google Scholar]
- 13.TNN . The Times of India; 2021. City Now Has Total 26 Dedicated Covid Hospitals with 757 ICU, 1868 Isolation Beds.https://timesofindia.indiatimes.com/city/kanpur/city-now-has-total-26-dedicated-covid-hospitals-with-757-icu-1868-isolation-beds/articleshow/82169588.cms [Google Scholar]
- 14.CDC . Cdc; 2020. Infection Control Guidance for Healthcare Professionals about Coronavirus (COVID-19) [Google Scholar]
- 15.Centers Control and Prevention . Centers Dis. Control Prev; 2020. Interim Guidance for Emergency Medical Services (EMS) Systems and 911 Public Safety Answering Points (PSAPs) for COVID-19 in the United States. [Google Scholar]
- 16.Cohen J., Rodgers Y. van der M. Contributing factors to personal protective equipment shortages during the COVID-19 pandemic. Prev. Med. (Baltim) 2020 doi: 10.1016/j.ypmed.2020.106263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sarti T.D., Lazarini W.S., Fontenelle L.F., Almeida A.P.S.C. What is the role of Primary Health Care in the COVID-19 pandemic? Epidemiol. e Serv. Saude Rev. Do Sist. Unico Saude Do Bras. 2020 doi: 10.5123/S1679-49742020000200024. [DOI] [PubMed] [Google Scholar]
- 18.Adams J.G., Walls R.M. Supporting the health care workforce during the COVID-19 global epidemic. JAMA, J. Am. Med. Assoc. 2020 doi: 10.1001/jama.2020.3972. [DOI] [PubMed] [Google Scholar]
- 19.Lu X., Xu S. Important role of emergency department doctors after the outbreak of COVID-19 in China. Emerg. Med. J. 2020 doi: 10.1136/emermed-2020-209633. [DOI] [PubMed] [Google Scholar]
- 20.Bennett C.L., Sullivan A.F., Ginde A.A., Rogers J., Espinola J.A., Clay C.E., Camargo C.A. National study of the emergency physician workforce. Ann. Emerg. Med. 2020 doi: 10.1016/j.annemergmed.2020.06.039. 2020. [DOI] [PubMed] [Google Scholar]
- 21.Ong A.C.W., Wee C.L.P., Lee W.L., Goh L.G., Lim G.H. Experience from a multi-disciplinary team Against COVID-19: a healthcare perspective. Int. J. Environ. Res. Publ. Health. 2021 doi: 10.3390/ijerph18041678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tang S., Mao Y., Jones R.M., Tan Q., Ji J.S., Li N., Shen J., Lv Y., Pan L., Ding P., Wang X., Wang Y., MacIntyre C.R., Shi X. Aerosol transmission of SARS-CoV-2? Evidence, prevention and control. Environ. Int. 2020 doi: 10.1016/j.envint.2020.106039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Booth C.M., Matukas L.M., Tomlinson G.A., Rachlis A.R., Rose D.B., Dwosh H.A., Walmsley S.L., Mazzulli T., Avendano M., Derkach P., Ephtimios I.E., Kitai I., Mederski B.D., Shadowitz S.B., Gold W.L., Hawryluck L.A., Rea E., Chenkin J.S., Cescon D.W., Poutanen S.M., Detsky A.S. Clinical features and short-term outcomes of 144 patients with SARS in the greater toronto area. J. Am. Med. Assoc. 2003 doi: 10.1001/jama.289.21.JOC30885. [DOI] [PubMed] [Google Scholar]
- 24.Meng L., Qiu H., Wan L., Ai Y., Xue Z., Guo Q., Deshpande R., Zhang L., Meng J., Tong C., Liu H., Xiong L. Intubation and ventilation amid the COVID-19 outbreak: Wuhan's experience. Anesthesiology. 2020 doi: 10.1097/ALN.0000000000003296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Caputo K.M., Byrick R., Chapman M.G., Orser B.A., Orser B.J. Intubation of SARS patients: infection and perspectives of healthcare workers. Can. J. Anesth. 2006 doi: 10.1007/BF03021815. [DOI] [PubMed] [Google Scholar]
- 26.Hasan A., Nafie K., Abbadi O. Histopathology laboratory paperwork as a potential risk of COVID-19 transmission among laboratory personnel. Infect. Prev. Pract. 2020;2:100081. doi: 10.1016/j.infpip.2020.100081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Amri M.F., Azizan N., Hussain F.A., Hayati F., Rahim S.S.S.A., Azhar Z.I. The challenges and risk of laboratory handling on a histology specimen during COVID-19 pandemic. Ann. Med. Surg. 2021:102242. doi: 10.1016/j.amsu.2021.102242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Misra V., Agrawal R., Kumar H., Kar A., Kini U., Poojary A., Chakrabarti I., Rai S., Singhal A., Shankar S.V. Guidelines for various laboratory sections in view of COVID-19: recommendations from the Indian association of pathologists and microbiologists. Indian J. Pathol. Microbiol. 2020;63:350. doi: 10.4103/IJPM.IJPM_857_20. [DOI] [PubMed] [Google Scholar]
- 29.W.H. Organization . 2020. Rational Use of Personal Protective Equipment (PPE) for Coronavirus Disease (COVID-19): Interim Guidance. W.H.O. (WHO, W.H. Organization, W.H.O. (WHO), W.H. Organization, W.H.O. (WHO), W.H. Organization, W.H.O. (WHO), W.H. Organization, [Internet]. Geneva; 2020 [cited 2020 Mar 23] [Google Scholar]
- 30.Sarfraz A., Sarfraz Z., Anwer A., Sarfraz M., Siddiq J. Availability, satisfaction and use of personal protective equipment among healthcare workers: a cross-sectional assessment of low- and middle-income countries. J. Occup. Environ. Med. 2020 doi: 10.1097/JOM.0000000000002028. [DOI] [PubMed] [Google Scholar]
- 31.Sharma N., Hasan Z., Velayudhan A., A E.M., Mangal D.K., Gupta S.D. Personal protective equipment: challenges and strategies to combat COVID-19 in India: a narrative review. J. Health Manag. 2020 doi: 10.1177/0972063420935540. [DOI] [Google Scholar]
- 32.Chughtai A.A., Seale H., Islam M.S., Owais M., Macintyre C.R. Policies on the use of respiratory protection for hospital health workers to protect from coronavirus disease (COVID-19) Int. J. Nurs. Stud. 2020 doi: 10.1016/j.ijnurstu.2020.103567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shechter A., Diaz F., Moise N., Anstey D.E., Ye S., Agarwal S., Birk J.L., Brodie D., Cannone D.E., Chang B., Claassen J., Cornelius T., Derby L., Dong M., Givens R.C., Hochman B., Homma S., Kronish I.M., Lee S.A.J., Manzano W., Mayer L.E.S., McMurry C.L., Moitra V., Pham P., Rabbani L.R., Rivera R.R., Schwartz A., Schwartz J.E., Shapiro P.A., Shaw K., Sullivan A.M., Vose C., Wasson L., Edmondson D., Abdalla M. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. Gen. Hosp. Psychiatr. 2020 doi: 10.1016/j.genhosppsych.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Park C.-Y., Kim K., Roth S., Beck S., Kang J.W., Tayag M.C., Griffin M. ADB Briefs; 2019. Global Shortage of Personal Protective Equipment amid COVID-19: Supply Chains, Bottlenecks, and Policy Implications. [Google Scholar]
- 35.Emanuel E.J., Persad G., Upshur R., Thome B., Parker M., Glickman A., Zhang C., Boyle C., Smith M., Phillips J.P. Fair allocation of scarce medical resources in the time of covid-19. N. Engl. J. Med. 2020 doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- 36.Wong M., Huang J., Wong S.H., Kwok K., Teoh J.Y.-C. Is the global health security (GHS) Index a significant factor Associated with COVID-19 control? A country level analysis. SSRN Electron. J. 2020 doi: 10.2139/ssrn.3582746. [DOI] [Google Scholar]
- 37.Lee M.O., Ribeira R., Fang A., Cantwell L., Khanna K., Smith C., Gharahbaghian L. Protecting the emergency physician workforce during the coronavirus disease 2019 pandemic through precision scheduling at an academic tertiary care trauma center. J. Am. Coll. Emerg. Physicians Open. 2021 doi: 10.1002/emp2.12221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.The Lancet, India under COVID-19 lockdown. Lancet. 2020 doi: 10.1016/S0140-6736(20)30938-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sahu D.P., Pradhan S.K., Sahoo D.P., Patra S., Singh A.K., Patro B.K. Fear and anxiety among COVID-19 Screening Clinic Beneficiaries of a tertiary care hospital of Eastern India. Asian J. Psychiatr. 2021 doi: 10.1016/j.ajp.2020.102543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ahuja K.K., Banerjee D., Chaudhary K., Gidwani C. Fear, xenophobia and collectivism as predictors of well-being during Coronavirus disease 2019: an empirical study from India. Int. J. Soc. Psychiatr. 2020 doi: 10.1177/0020764020936323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dubey S., Biswas P., Ghosh R., Chatterjee S., Dubey M.J., Chatterjee S., Lahiri D., Lavie C.J. Psychosocial impact of COVID-19. Diabetes & metabolic syndrome. Clin. Res. Rev. 2020 Sep 1;14(5):779–788. doi: 10.1016/j.dsx.2020.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dsouza D.D., Quadros S., Hyderabadwala Z.J., Mamun M.A. Aggregated COVID-19 suicide incidences in India: fear of COVID-19 infection is the prominent causative factor. Psychiatr. Res. 2020 doi: 10.1016/j.psychres.2020.113145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Choudhari R. COVID 19 pandemic: mental health challenges of internal migrant workers of India. Asian J. Psychiatr. 2020 doi: 10.1016/j.ajp.2020.102254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.World Bank . 2017. Hospital Beds (Per 1,000 People) - South Asia. [Google Scholar]
- 45.Ghosh A., Nundy S., Mallick T.K. How India is dealing with COVID-19 pandemic. Sensors Int. 2020 doi: 10.1016/j.sintl.2020.100021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Goldhill O. STAT News; 2020. Hospitals in Half the States Are Facing A Massive Staffing Shortage. [Google Scholar]
- 47.Kobusingye O.C., Hyder A.A., Bishai D., Joshipura M., Hicks E.R., Mock C. Emergency medical services – disease control priorities in developing countries. Journal. 2006 [Google Scholar]
- 48.Kobusingye O.C., Hyder A.A., Bishai D., Hicks E.R., Mock C., Joshipura M. Emergency medical systems in low- and middle-income countries: recommendations for action. Bull. World Health Organ. 2005 [PMC free article] [PubMed] [Google Scholar]
- 49.Ford T.R., Fix M.L., Shappell E., Egan D.J., Mannix A., Bailitz J., Li X., Gottlieb M. AEM Educ. Train; 2021. Beyond the Emergency Department: Effects of COVID-19 on Emergency Medicine Resident Education. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Quah L.J.J., Tan B.K.K., Fua T.P., Wee C.P.J., Lim C.S., Nadarajan G., Zakaria N.D., Chan S.E.J., Wan P.W., Teo L.T., Chua Y.Y., Wong E., Venkataraman A. Reorganising the emergency department to manage the COVID-19 outbreak. Int. J. Emerg. Med. 2020 doi: 10.1186/s12245-020-00294-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sriram V., Baru R., Bennett S. Health Policy Plan; 2018. Regulating Recognition and Training for New Medical Specialties in India: the Case of Emergency Medicine. [DOI] [PubMed] [Google Scholar]
- 52.Bhattacharya S., Mahbub Hossain M., Singh A. AIMS Public Heal; 2020. Addressing the Shortage of Personal Protective Equipment during the COVID-19 Pandemic in India-A Public Health Perspective. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Collins N., Crowder J., Ishcomer-Aazami J., Apedjihoun D. Perceptions and experiences of frontline urban Indian organization healthcare workers with infection prevention and control during the COVID-19 pandemic. Front. Sociol. 2021 doi: 10.3389/fsoc.2021.611961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Fischer C.B., Adrien N., Silguero J.J., Hopper J.J., Chowdhury A.I., Werler M.M. Mask adherence and rate of COVID-19 across the United States. PLoS One. 2021 doi: 10.1371/journal.pone.0249891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Greenberg N. Mental health of health-care workers in the COVID-19 era. Nat. Rev. Nephrol. 2020 doi: 10.1038/s41581-020-0314-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Salazar de Pablo G., Vaquerizo-Serrano J., Catalan A., Arango C., Moreno C., Ferre F., Il Shin J., Sullivan S., Brondino N., Solmi M., Fusar-Poli P. Impact of coronavirus syndromes on physical and mental health of health care workers: systematic review and meta-analysis. J. Affect. Disord. 2020 doi: 10.1016/j.jad.2020.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Christopher D.J., Isaac B.T.J., Rupali P., Thangakunam B. Health-care preparedness and health-care worker protection in COVID-19 pandemic. Lung India. 2020 doi: 10.4103/lungindia.lungindia_189_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Young K.P., Kolcz D.L., O'Sullivan D.M., Ferrand J., Fried J., Robinson K. national survey, Psychiatr. Serv; 2021. Health Care Workers' Mental Health and Quality of Life during COVID-19: Results from a Mid-pandemic. [DOI] [PubMed] [Google Scholar]
- 59.Yaffee A.Q., Peacock E., Seitz R., Hughes G., Haun P., Ross M., Moran T.P., Pendley A., Terry N., Wright D.W. Preparedness, adaptation, and innovation: approach to the covid-19 pandemic at a decentralized, quaternary care department of emergency medicine. West. J. Emerg. Med. 2020 doi: 10.5811/WESTJEM.2020.8.48624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mehta Y., Chaudhry D., Abraham O.C., Chacko J., Divatia J., Jagiasi B., Kar A., Khilnani G.C., Krishna B., Kumar P., Mani R.K., Rao B.K., Singh P.K., Singh S., Tiwary P., Wattal C., Govil D., Dixit S., Samavedam S. Critical care for COVID-19 affected patients: position statement of the Indian society of critical care medicine. Indian J. Crit. Care Med. 2020 doi: 10.5005/jp-journals-10071-23395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Dutta A., Fischer H.W. The local governance of COVID-19: disease prevention and social security in rural India. World Dev. 2021 doi: 10.1016/j.worlddev.2020.105234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kashyap A., Raghuvanshi J. A preliminary study on exploring the critical success factors for developing COVID-19 preventive strategy with an economy centric approach. Manag. Res. 2020 doi: 10.1108/MRJIAM-06-2020-1046. [DOI] [Google Scholar]
- 63.Goldschmidt-Clermont P.J. COVID-19 real-world data for the US and lessons to reopen business. PLoS Pathog. 2020 doi: 10.1371/journal.ppat.1008756. [DOI] [PMC free article] [PubMed] [Google Scholar]