Abstract
Background
Despite evidence of the nosocomial transmission of novel coronavirus Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) in hospitals worldwide, the contributions of the pathways of transmission are poorly quantified.
Methods
We analysed national records of hospital admissions and discharges, linked to data on SARS-CoV-2 testing, using an individual-based model that considers patient-to-patient, patient-to-healthcare worker (HCW), HCW-to-patient and HCW-to-HCW transmission.
Results
Between 1 March 2020 and 31 December 2020, SARS-CoV-2 infections that were classified as nosocomial were identified in 0.5% (0.34–0.74) of patients admitted to an acute National Health Service trust. We found that the most likely route of nosocomial transmission to patients was indirect transmission from other infected patients, e.g. through HCWs acting as vectors or contaminated fomites, followed by direct transmission between patients in the same bay. The risk of transmission to patients from HCWs over this time period is low, but can contribute significantly when the number of infected inpatients is low. Further, the risk of a HCW acquiring SARS-CoV-2 in hospital is approximately equal to that in the community, thereby doubling their overall risk of infection. The most likely route of transmission to HCWs is transmission from other infected HCWs.
Conclusions
Current control strategies have successfully reduced the transmission of SARS-CoV-2 between patients and HCWs. In order to reduce the burden of nosocomial COVID-19 infections on health services, stricter measures should be enforced that would inhibit the spread of the virus between bays or wards in the hospital. There should also be a focus on inhibiting the spread of SARS-CoV-2 between HCWs. The findings have important implications for infection-control procedures in hospitals.
Keywords: SARS-CoV-2, healthcare workers, patients, healthcare-acquired infection, transmission
Key Messages.
Nosocomial novel coronavirus Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infections were identified in 0.5% (0.34–0.74) of patients admitted to an acute National Health Service trust between 1 March 2020 and 31 December 2020 according to Public Health England and European Centre for Disease Prevention and Control definitions of nosocomial, using national admission data records.
Modelling using data from this time period suggests that the most likely route of nosocomial transmission to patients was indirect transmission from other infected patients, i.e. transmission from outside of a bay, e.g. through healthcare workers (HCWs) acting as vectors or contaminated fomites, followed by direct transmission between patients in the same bay.
The risk of transmission to patients from HCWs remains low, but can contribute significantly to the burden of nosocomial infections when the number of infected inpatients is low.
Results also suggest that the risk of a HCW acquiring SARS-CoV-2 in hospital is approximately equal to that in the community, thereby doubling their overall risk of infection, and that the most likely route of transmission to HCWs is transmission from other infected HCWs.
Interventions to reduce the burden of nosocomial SARS-CoV-2 infections should focus on reducing the indirect (inter-bay/ward) spread of the virus and developing strategies to reduce the risk of HCW-to-HCW transmission.
Introduction
Since the identification of novel coronavirus Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) in January 2020, there have been confirmed cases in both hospitalized patients and healthcare workers (HCWs) that are suspected to be nosocomial in origin. Identifying the source of infection in these cases is complicated by the variable incubation period,1 the possibility of transmission from asymptomatic or pauci-symptomatic cases2 and widespread community transmission. Airborne and droplet transmission is the predominant route, but there is also potential for environmental transmission to both patients and HCWs through contaminated surfaces,3 and the Health and Safety Investigation Branch (HSIB) identified opportunities for HCWs to spread the virus due to issues with building design and reduced cleaning in shared staff areas, lack of social distancing, shared equipment or the absence of universal face coverings in non-clinical areas.4 There is evidence that in a nosocomial setting, transmission can be mitigated by vigilant basic infection-control measures including the wearing of surgical masks, and hand and environmental hygiene.5
A set of guidelines has been issued by the European Centre for Disease Prevention and Control that can be used to classify a case related to a recent hospitalization event as nosocomial in origin6 but, even when nosocomial acquisition is suspected, it is not possible to attribute the source of infection to either other patients or HCWs in most cases. This issue is further complicated by conflicting reports of the infection prevalence in HCWs, with some studies finding that it is in line with community prevalence7 and others identifying an increased risk to patient-facing staff.8 In the absence of detailed genomic data, it is difficult to classify a detected case as either community or nosocomially acquired, although results from the REACT-2 study suggest that by 13 July 2020, HCWs were approximately twice as likely to have antibodies to SARS-CoV-2 than people in non-healthcare roles8 and it is therefore possible that up to half of infections in HCWs over that period were nosocomial in origin. Contemporaneous studies estimating the levels of infection in HCWs in UK trusts by polymerase chain reaction (PCR) produced prevalence estimates ranging from 0% to 59% of the HCW population under study.9–13
Mathematical models are powerful tools that can be used to estimate the probability and risk of a transmission occurring between two individuals and within populations. We have developed an individual-based model that simulates transmission between and within patients and HCWs. Through analysis of national data, meta-analyses of contemptuous studies on HCW-infection rates and calibration of this model, we have identified the highest risk routes for transmission of SARS-CoV-2 within hospitals.
Methods
Patient-level data collection
Secondary Uses Service (SUS) data linked to test data from PHE’s Second-Generation Surveillance System (SGSS) were obtained for all admissions within the study period (1 March 2020 through to 1 December 2020) that form the start of a continuous inpatient spell completed before the end of December. In all cases, data are grouped by week of admission. Nosocomial admissions are those that relate to a positive COVID-19 test carried out whilst the patient was in hospital, on the 8th day following admission or later. Negative admissions are those for patients who had no positive COVID-19 test during the study period. All figures include readmissions and the same patient can have admissions to more than one trust. Patients are linked by National Health Service (NHS) number or, when that is missing, date of birth and local identifier. If either of those is also missing, then the patient is removed from the data set.
Meta-analyses of HCW-infection rates
Levels of UK hospital HCW infection with COVID-19 were analysed using data from studies included in worldwide reviews of hospital-based HCW risk factors and serology. Four reviews of hospital-based HCW risk factors and serology were identified from a literature search of PubMed and medXriv (Chen et al.,9 Chou et al.,10 Gómez-Ochoa et al.,11 Galanis et al.12). These studies were included in a meta-analysis together with a multicentre study conducted by Public Health England (PHE).13 This identified 21 studies, with test data collected during 3 March to 12 June from settings in seven NHS England regions and Scotland. Analyses were conducted for current-infection testing (PCR tests) and cumulative-infection testing (antibody tests or combined results from antibody and PCR tests), with additional details gathered from the studies to enable stratification by COVID-19 symptom history, to gather more granular temporal and spatial details (where detailed data were only published in graphical format, these were extracted using the digitize package in R14).
Individual-based model
We have developed an individual-based model that simulates transmission between and within patients and HCWs. The model is described in full in Supplementary Material (available as Supplementary data at IJE online) but key features are described here.
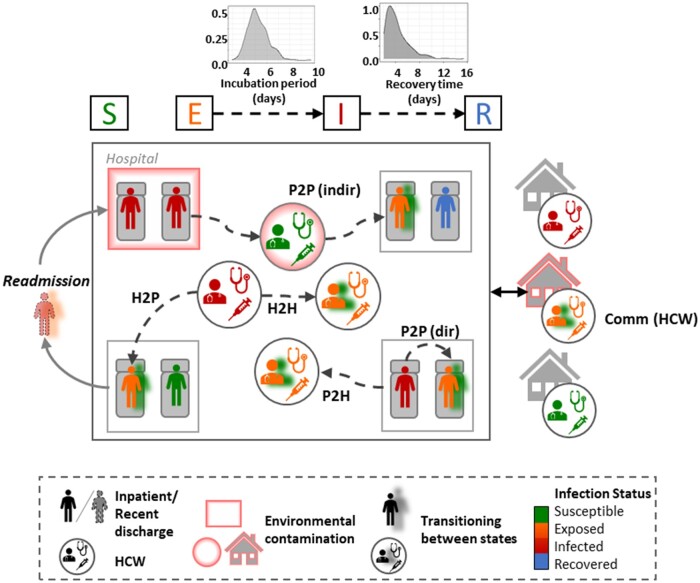
The model simulates transmission via six distinct pathways, namely transmission: (i) to HCWs in the community from the general population (commScale), (ii) to HCWs from infected patients in the hospital (P2H), (iii) to HCWs from other HCWs while at work (H2H), (iv) to patients sharing a bay with infected patients (P2P (direct)), (v) to patients directly from infected HCWs (H2P), (vi) to patients from other infectious patients outside of a shared bay, e.g. by HCWs acting as a vector for droplets or from contaminated fomites (P2P (indir)) (Figure 1). The model is calibrated to linked patient and test data from the SUS data set and SGSS between 1 March 2020 and 1 December 2020, a meta-analysis of early prevalence data in HCWs in the literature and data from the SARS-CoV-2 Immunity and Reinfection Evaluation (SIREN) study15 (Supplementary Figure S1, available as Supplementary data at IJE online). Adherence to infection prevention and control (IPC) guidelines such as wearing personal protective equipment (PPE) and increased ward cleaning is implicit in the parameterization since the data used to calibrate the model are taken from NHS trusts during the first wave when these measures we already in place. We assume that once a patient enters a bay, they remain there for the entirety of their stay and that a suspected COVID-19 patient would be preferentially placed in bays with other confirmed or suspected cases. Through calibration of this model, we have identified the pathways associated with the highest risk of transmission to both patients and HCWs (Figure 1). The hospital capacity is fixed at 1000 beds and 8000 HCWs (∼4000 on shift at any time). In this work, hospital occupancy is set to 65% (as observed in the first wave) meaning that patients are admitted until 650 of the 1000 beds available are filled with a mix of COVID-19 and non-COVID-19 patients. However, if 65% of the beds are full and there are more COVID-19 patients to be admitted on that day (according to the admissions file, see Supplementary Material 1, available as Supplementary data at IJE online), then the occupancy is allowed to temporarily exceed 65% until the next time step when fewer non-COVID-19 patients will be recruited to bring the occupancy back down to 65%.
Figure 1.
Schematic representation of the individual-based model used in this analysis. Patients and healthcare workers (HCWs) can be in any of the infection states Susceptible, Exposed (infected but not yet infectious), Infected [infected and infectious, can be presymptomatic (i.e. detectable but not yet symptomatic), symptomatic or asymptomatic] or Recovered, and transition between states probabilistically. Patients can be infected directly from other patients or from HCWs, and there is also a pathway for the indirect spread of infection. HCWs can be infected by patients or other HCWs and also by the general community while they are not on shift. P2P, patient-to-patient transmission; P2H, patient-to-HCW transmission; H2P, HCW-to-patient transmission; H2H, HCW-to-HCW transmission; Comm, community acquisition.
Simulations
The model was simulated for 1536 time steps covering a time period of 256 days (6 steps per simulated day) aligning with the collection period of the patient-level data. Individual-level patient and HCW data on infection status and location were recorded at each time step.
Model calibration
Where data were available, identifiable parameters were assigned values from the literature (Supplementary Table S1, available as Supplementary data at IJE online). The unidentifiable parameters were iteratively calibrated to within acceptable ranges using the methodology described by Joslyn et al.16 The set of criteria whereby simulations were deemed to be representative of observed data were derived from aggregated hospital-level data on the infection rate in patients and HCWs drawn and are defined in Table 1. Initially, log-10 uniform probability distributions were assumed for all transmission probabilities and parameters were allowed to take on any value from 1 to 10–10. One thousand Latin Hypercube sampled parameter sets were generated and simulations were executed as described in the ‘Simulations’ section. For the next iteration, a new distribution was derived for each parameter set by identifying the highest-density regions for each parameter set in which any of the tests were satisfied. This was repeated for two further iterations until a subset of runs passed all four tests (Supplementary Figures S2 and S3, available as Supplementary data at IJE online). The parameter sets that passed all four tests were then assessed qualitatively against data on patient and HCW infections (Supplementary Figure S3, available as Supplementary data at IJE online) and carried forward for the next stage of the analysis. The calibrated parameter ranges were also compared qualitatively to the parameter values in a previously published simple deterministic model of hospital transmission.17 A sensitivity analysis of the test criteria values and calibrated parameter values was performed and the partial-rank correlation coefficients are shown in Supplementary Figure S3 (available as Supplementary data at IJE online).
Table 1.
Criteria for an outcome to be defined as related to a feasible parameter set
| Criteria | Minimum | Maximum | Source | |
|---|---|---|---|---|
| 1 | Maximum number of cases identified in a day in the NHSE situation report standardized by number of beds in the trust | 0.0077 | 0.058 | NHSE situation report |
| 2 | Maximum number of cases in a day after 1 June in the NHSE situation report standardized by number of beds in the trust | 0 | 0.012 | NHSE situation report |
| 3 | Maximum proportion of susceptible patients who develop a nosocomial SARS-CoV-2 infection over entire data/simulation period | 0.01 | 0.1 | 17 |
| 4 | Proportion of HCWs infected over entire data/simulation period | 0.025 | 0.25 | 15 /Figure 3 |
NHSE, National Health Service, England; HCWs, healthcare workers.
Defining testing criteria
Ranges for criteria 1 and 2 were standardized by trust size (total number of beds) and taken to be the 25th and 75th percentiles of the National Health Service, England (NHSE) Situation Report data set to avoid the estimates being skewed by reporting irregularities. The proportion of susceptible patients who acquired a nosocomial infection was estimated to be <10% based on a previous modelling study demonstrating this outcome in a high-prevalence area with higher-than-normal transmission rates.17 The proportion of infected HCWs over the course of the epidemic was taken from the publicly accessible SeroTracker database (https://serotracker.com/Analyze) combined with data from the meta-analysis described above and published data from the SIREN study.15 The range that a result must fall into to pass the test relating to each criteria is detailed in Table 1.
Results
The risk of nosocomial infection in patients and HCWs over the first wave
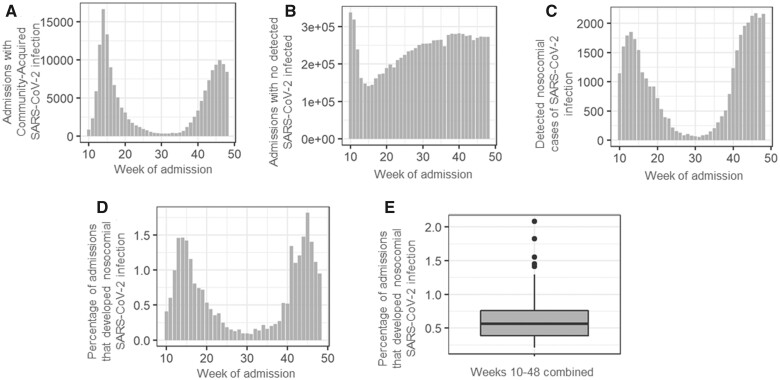
NHSE and PHE define a healthcare-associated case as any patient who tests positive for SARS-CoV-2 for the first time ≥8 days post admission to hospital.6,18 Over the course of the first wave (1 March 2020 to 31 August 2020), one-third of all laboratory-confirmed cases in England were linked to a record of hospital attendance, 15.4% of which (∼5.3% of all confirmed cases) were suspected to be healthcare-associated,19 although this figure is likely biased by the increased likelihood of a case being detected in hospital inpatients compared with those in the general community. From the analysis data from acute NHSE trusts over an extended time period from weeks 10–48 (1 March 2020 to 1 December 2020), the number of non-COVID-19 admissions per week ranged from 140 000–290 000 and the number of patients who developed a nosocomial infection in a single week peaked at ∼2000 (Figure 2A–C). The probability of a patient acquiring a nosocomial SARS-CoV-2 infection during a hospital-admission spell increased with the number of infected admissions in the week that the eventual nosocomial case was admitted (Figure 2A, C and D) and ranged from 1.7% at the peak of the epidemic to 0.125% towards the end of the first wave (week 35, Figure 2D). Between weeks 10 and 48, ∼0.5% of patients admitted to the 147 acute trusts had a detected nosocomial COVID-19 infection according to NHSE definitions (Figure 2D).
Figure 2.
SARS-CoV-2 status of patients admitted to147 acute National Health Service, England (NHSE) trusts between weeks 10 and 48. (A) and (B) Total number of admitted patients testing positive (A) and negative (B) for SARS-CoV-2 on admission to hospital by week of admission. (C) Number of nosocomial cases detected in patients admitted to hospital in weeks 10–48 by week of admission. (D) Percentage of admissions that went on to develop a detected nosocomial SARS-CoV-2 infection by week of admission. (E) Percentage of all negative admissions between weeks 10 and 48 that developed a nosocomial SARS-CoV-2 infection. Data were obtained from the Secondary Uses Service (SUS) data set as admissions within the study period (March to November) and form the start of a continuous inpatient spell completed before the end of December. In all cases, data are grouped by week of admission. Nosocomial admissions are those that relate to a positive SARS-CoV-2 test carried out whilst the patient was in hospital, on the 8th day following admission or later. Negative admissions are those for patients who had no positive SARS-CoV-2 test during the study period. All figures include readmissions and the same patient can have admissions to more than one trust.
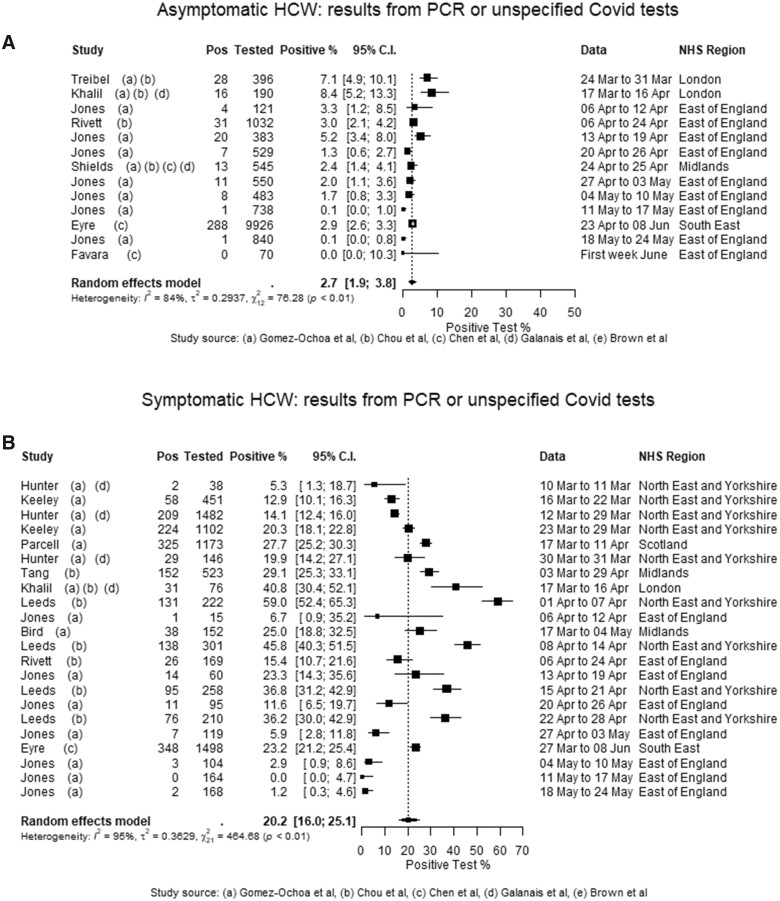
Few data sources exist that accurately track HCW-infection rates over the first wave. To address this issue, we performed a meta-analysis of studies estimating proportions of HCWs exposed at the individual-trust level and found that serological studies estimated cumulative prevalence ranges from 3% to 48% (Figure 3). Stratifying the meta-analysis by COVID-19-symptom status provided greater homogeneity in sampled populations, with the caveat that the definition of ‘symptomatic’ is study-specific; noting anosmia was added to the UK COVID-19 definition towards the end of the period spanned by these studies, on 18 May 2020.20 The pooled estimate for positivity in asymptomatic subjects was 2.7% [95% confidence interval (CI): 1.9–3.8] and for studies excluding self-isolating HCW from the data, 2.4% (95% CI: 1.6–3.8) (Figure 3A).13 The pooled estimate for symptomatic subjects was 20.2% (95% CI: 16.0–25.1). A forest plot (arranged in order of the study period midpoint) demonstrates a clear ‘rise and fall’ temporal pattern (Figure 3B). A corresponding symptomatic-stratification meta-analysis of cumulative-infection-rate studies provides pooled estimates of 10.7% (95% CI: 7.1–15.8) in HCW reporting no history of COVID-19 symptoms and 31.6% (95% CI: 24.7–39.4) in post-symptomatic HCW. The SIREN study recruited 20 787 HCWs in England between 10 June 2020 and 9 November 2020, and the results indicate that 31.8% of enrolled HCWs had evidence of previous SARS-CoV-2 infection (by positive antibody test result) by 24 November 2020.15
Figure 3.
Proportion of healthcare workers (HCWs) testing positive for SARS-CoV-2 over the first wave. Levels of UK hospital HCW COVID-19 infection were analysed using data from studies included in worldwide reviews of HCW risk factors and serology. This identified 21 studies, with test data collected during 3 March to 12 June 2020, from settings in seven National Health Service (NHS) England regions and Scotland. Analyses were conducted for current-infection testing [polymerase chain reaction (PCR) tests] and cumulative-infection testing (antibody tests or combined results from antibody and PCR tests), with additional details gathered from the studies to enable stratification by COVID-19 symptom history, to gather more granular temporal and spatial details (where detailed data were only published in graphical format, these were extracted using the digitize package in R14).
The most probable routes of transmission of SARS-CoV-2 within a hospital environment
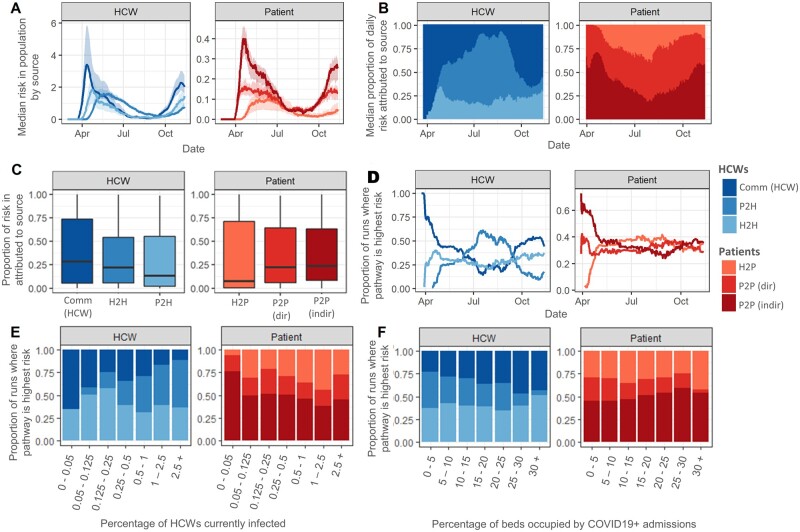
Calibrating the individual-based model output to data from the first wave indicates that whereas the probability of infection of HCWs in the community is higher than that of being infected by either other HCWs or patients, the high contact rate between susceptible HCWs and infected individuals in the hospital (patients or other HCWs) means that the overall risk of transmission to a HCW in a single day, defined as the probability of transmission multiplied by the size of the population at risk, can be greater when in the healthcare setting than in the community (Figure 4A, B and Supplementary Figure S3, available as Supplementary data at IJE online). On average, over the entire simulation period, community transmission is responsible for the highest proportion of the daily risk to a HCW (28.4%; 95% CI: 18.7–39.9) followed by HCW-to-HCW transmission (22.2%; 95% CI: 16.5–29.6) and then patient-to-HCW (13.2%; 95% CI: 8.1– 20.7) (Figure 4C), although the level of risk to a HCW and the most likely source of transmission change over time (Figure 4A and D). During the period in which the transmission rate in the community is high, community transmission is the most likely source of infection in >50% of simulations (Figure 4D), although, between 16 May 2020 and 13 September 2020, when the community incidence rate was greatly reduced due to the first nationwide lockdown,20 HCW-to-HCW transmission becomes the most likely source of transmission in the majority of model runs (Figure 4D). HCW-to-HCW transmission accounts for the highest proportion of daily risk when there is a high proportion of HCWs infected overall (>1%, Figure 4E) but there is an increasingly important role for patient-to-HCW transmission when the proportion of beds occupied by COVID-19-positive admissions is high (Figure 4F). The relative contribution of HCW-to-HCW transmission decreases as the proportion of beds occupied by COVID-19-positive admissions increases (Figure 4E).
Figure 4.
Probability and risk of transmission to patient and healthcare worker (HCW) populations. (A) Median and 95% CI of the risk over time of transmission for each pathway under current interventions from 1000 model runs. (B) Median proportion of daily risk to HCWs and patients attributable to each source of infection. (C) Distribution of the proportion of risk attributed to each source for HCWs and patients over the entire simulation period. (D)–(F) Proportion of model runs in which each transmission pathway contributes the highest risk of transmission per day by date (D), on days on which the percentage of HCWs infected was with the range on the x-axis (E) and on days on which the percentage of beds occupied by COVID-19+ admissions was within the range on the x-axis (F). In all panels, risk is defined as transmission probability× number of susceptible individuals who could be exposed by that route; (e.g. for direct patient-to-patient transmission, where there is one infected patient and five susceptible patients in bay 1, the risk of a direct patient-to-patient transmission occurring in that bay is 1 × bP2P × 5, and the total risk of patient-to-patient transmission is the sum over all bays of bP2P × n_infected × n_susceptible in each bay).
For nosocomial transmission to patients, the most common source of transmission was indirect transmission between patients, which increased with the proportion of beds occupied by COVID-19-positive admissions (Figure 4A, B and F). Similarly to HCWs, the greatest source of risk of transmission to patients changed over time, although, on average, indirect transmission (e.g. by HCWs acting as vectors for droplets or through environmental or fomite contamination) was the most likely source per day (median 24.6%, 95% CI: 18.7–26.4) followed by direct transmission to patients in the same bay as an infected patient (22.2%, 95% CI: 18.3–25.3) and finally by HCW-to-patient transmission (7.1%, 95% CI: 6.1–10.6) (Figure 4C). The risk of transmission from infected HCWs to patients was highest when the proportion of infected HCWs was high (Figure 4E) and from infected patients to others in the same bay was highest when the proportion of overall beds occupied by COVID-19 patients was high (Figure 4F). Despite the absolute risk of transmission to patients from HCWs being low, HCW-to-patient transmission is the highest-rank transmission pathway for patients when the number of HCWs infected is high (Figure 4C and E) and this pathway decreases in significance as the proportion of beds occupied by COVID-19-positive admissions increases (Figure 4C and F).
Discussion
Modelling supported by national data from English hospitals between March and November 2020 suggests that the most likely source of nosocomial transmission to HCWs was other HCWs. Further, the risk of an individual HCW acquiring COVID-19 from another HCW is similar to their risk of acquisition in the community. On average, the risk of HCW acquisition of infection from a patient is less than half that of acquisition in the community but, owing to the high risk of HCW-to-HCW transmission, there is potential for a small number of patient-to-HCW transmissions to seed outbreaks in the HCW population.
The majority of nosocomial infections in hospital inpatients result from indirect transmission from other patients, followed by direct transmission from infected patients to other patients sharing the same bay. We define direct transmission as transmission to patients sharing a hospital bay with an infectious individual resulting from e.g. close-contact aerosol transmission or poor ventilation within the bay. Indirect transmission is defined as transmission from a patient in a particular hospital bay to other patients outside of that bay where such patients may be in the same ward or elsewhere in the hospital. This indicates that avoiding the introduction of the virus into bays occupied by non-COVID-19 patients and the prevention of inter-bay or ward transmission are critical. Modelling suggests that the risk of transmission to patients from HCWs remains low, but can contribute significantly to the burden of nosocomial infections when the number of infected inpatients is low.
These results suggest that IPC measures that are currently being implemented by NHSE trusts are mitigating the risk of transmission between patients and HCWs. We estimate that a maximum of 1% of susceptible inpatients experienced a nosocomial SARS-CoV-2 infection that was identified by PCR testing between March and December 2020, representing close to 40 000 detected cases. This is likely to be an underestimate of the true burden of the nosocomial transmission of SARS-CoV-2, due to (i) asymptomatic infection being less likely to be detected than symptomatic infection and (ii) some cases being misclassified as community-acquired due to cases being classified using a strict cut-off of 8 days between admission and specimen date. Conversely, there is also a possibility that this is an overestimation due to patients being discharged whilst incubating an undetected community-acquired infection that is then classified as a nosocomial case. The probability that an infected individual remains asymptomatic for the entire duration of their illness is estimated to be 16%, with a range of 6–41%.21,22 The simulated results capture this uncertainty by allowing the proportion of inpatients that ever develop a nosocomial infection to reach as high as 3.5% (60% higher than observed in the real-world data) when calibrating. The model calibration implicitly includes the impact of PPE and other IPC measures taken by NHS hospitals over this time period. If these interventions were lifted, we would expect the number of nosocomial infections to increase. The risk of transmission though each pathway may also change; e.g. if HCWs did not wear PPE when treating, they may contribute to a higher proportion of infections in patients, or there may be in increase in indirect patient transmission through HCWs acting as vectors.
To further reduce the risk of nosocomial transmission in hospitals, interventions to limit indirect patient-to-patient spread as well as transmission to HCWs are required. These interventions could include increased hand-hygiene and surface-cleaning programmes as well as those outlined by the HSIB such as changing the location of equipment that is required regularly to avoid HCWs crowding around desks or stations and encouraging social distancing in non-clinical areas.4 These results suggest that high levels of uptake of a vaccine that significantly reduces transmission among the HCW population will also reduce the impact of HCW-to-HCW transmission and could bring HCW infection in line with the general community. If a vaccine were to be administered to the majority of inpatients a sufficiently long time before admission, then transmissions to and between patients will also fall.
The methodologies applied in this work are applicable to different settings, e.g. other care facilities, non-acute hospitals and health systems in other countries, and can be extended to other time periods. The results presented here have important implications for mitigating transmissions in the event of a vaccine or immune response escaping variant emerging, or for settings in which vaccines have not yet been widely introduced. Additionally, the risk of nosocomial transmission remains, even with increasing rates of vaccination in England. We expect that the dominant routes of transmission will remain dominant with the emergence of more transmissible variants of SARS-CoV-2. In addition, the results presented here can be used to help to determine where interventions to prevent nosocomial transmission may have greatest effect, e.g. in a setting of high HCW-to -HCW transmission; universal masking may be likely to have greatest impact, whereas social distancing of hospital beds may be a more effective strategy when direct patient-to-patient transmission is high.
The model presented here has several limitations. The spatial arrangement of wards and shared spaces such as corridors and bathroom facilities, and their distribution across several buildings, are not represented in the model. These will vary from trust to trust. Further, increased transmission between HCWs working on the same ward, shared staff transport and the idea that HCWs may be more likely to live with other HCWs and therefore be at increased risk in the community are also not included. Another limitation is that patients do not move bays during their time in hospital. The parameter values used in this work are our current best estimates but changes in hospital occupancy levels and patient length of stay would cause changes in the number and proportion of patients and HCWs infected. Sensitivity analyses indicate that occupancy and the length of stay of infected individuals have the most significant impact on the contribution of each route of transmission (Supplementary Figure S4, available as Supplementary data at IJE online). Despite these limitations, we believe that this model adequately captures the main routes of transmission within a hospital and identifies the key risks to patients and HCWs while in hospital. Under current IPC guidelines, all patients should be tested and cohorted into COVID-19-positive and non-infected wards, alongside the widespread usage of face coverings and PPE.23 Our findings suggest that if this were not the case, then the risk of transmission would be much higher and the most likely source of transmission would shift (Supplementary Figure S3, available as Supplementary data at IJE online). For HCWs, if the transmission rate was similar to that in the community early in the epidemic when guidance on face coverings and social distancing had not been introduced, the most significant source of transmission would have been infected patients, followed by HCW-to-HCW and community acquisition. In the patient population, there is potential for even greater indirect spread between patients without IPC measures.
Conclusion
Strategies to mitigate nosocomial transmission in England have successfully reduced the transmission rate of SARS-CoV-2 between patients and HCWs. To further reduce nosocomial transmission, model findings suggest that measures to inhibit the spread of the virus between bays or wards as well as inhibiting the spread of SARS-CoV-2 between HCWs both on the ward and while spending time in shared facilities should be the focus. The findings presented here have important implications for infection-control procedures in acute hospitals in England and the methodologies demonstrated in this work can be applied to other settings such as prisons, care homes and different hospital types globally.
Supplementary data
Supplementary data are available at IJE online.
Ethics approval
Ethics approval was not required for this computational modelling study.
Funding
P.J.W. was supported by the MRC Centre for Global Infectious Disease Analysis [grant MR/R015600/1], which is jointly funded by the UK Medical Research Council (MRC) and the UK Foreign, Commonwealth & Development Office (FCDO), under the MRC/FCDO Concordat agreement and is also part of the EDCTP2 programme supported by the European Union (EU). P.J.W. was also supported by the National Institute for Health Research (NIHR) Health Protection Research Unit (HPRU) in Modelling and Health Economics—a partnership between Public Health England (PHE), Imperial College London and LSHTM [grant NIHR200908].
Data availability
Data available on request.
Supplementary Material
Acknowledgements
We thank Colin Brown for critical reading of the manuscript. Thanks to the SIREN team at PHE for their data insight, to all involved in running SIREN at participating sites and to the SIREN participants.
Author contributions
The study was conceived of by S.E. and J.V.R. Hospital data were extracted, linked and analysed by J.S., D.P. and A.B. SARS-CoV-2 testing data were managed and analysed by A.B. with technical oversight by R.H. The transmission-dynamic model was designed by S.E. and J.V.R., and implemented by S.E. P.J.W. and J.V.R. contributed to the design and interpretation of the analysis. S.E. wrote the manuscript that was critically reviewed and approved by all authors and is the guarantor for this work. The views expressed are those of the authors and not necessarily those of the Department of Health and Social Care, EU, FCDO, MRC, National Health Service, NIHR or PHE.
Conflict of interest
P.J.W. has received payment from Pfizer for teaching of the mathematical modelling of infectious-disease transmission and vaccination.
References
- 1. McAloon C, Collins Á, Hunt K et al. Incubation period of COVID-19: a rapid systematic review and meta-analysis of observational research. BMJ Open 2020;10:e039652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Jiang X-L, Zhang X-L, Zhao X-N et al. Transmission potential of asymptomatic and paucisymptomatic severe acute respiratory syndrome coronavirus 2 infections: a 3-family cluster study in China. J Infect Dis 2020;221:1948–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ong SWX, Tan YK, Chia PY et al. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA 2020;323:1610–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Health and Safety Investigation Branch. COVID-19 transmission in hospitals: management of the risk—a prospective safety investigation. 29 October 2020. https://www.hsib.org.uk/investigations-cases/covid-19-transmission-hospitals/final-report/ (28 October 2021, date last accessed).
- 5. Wong SCY, Kwong RT-S, Wu TC et al. Risk of nosocomial transmission of coronavirus disease 2019: an experience in a general ward setting in Hong Kong. J Hosp Infect 2020;105:119–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. European Centre for Disease Prevention and Control. Surveillance definitions for COVID-19. 15 March 2021. https://www.ecdc.europa.eu/en/covid-19/surveillance/surveillance-definitions (28 October 2021, date last accessed).
- 7. Leeds JS, Raviprakash V, Jacques T, Scanlon N, Cundall J, Leeds CM. Risk factors for detection of SARS-CoV-2 in healthcare workers during April 2020 in a UK hospital testing programme. EClinicalMedicine 2020;26:100513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ward H, Atchison C, Whitaker M et al. SARS-CoV-2 antibody prevalence in England following the first peak of the pandemic. Nat Commun 2021;12:905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chen X, Chen Z, Azman AS et al. Serological evidence of human infection with SARS-CoV-2: a systematic review and meta-analysis. Lancet Global Health 2021;9:e598–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chou R, Dana T, Buckley DI, Selph S, Fu R, Totten AM. Epidemiology of and risk factors for coronavirus infection in health care workers: a living rapid review. Ann Intern Med 2020;173:120–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Gómez-Ochoa SA, Franco OH, Rojas LZ et al. COVID-19 in health-care workers: a living systematic review and meta-analysis of prevalence, risk factors, clinical characteristics, and outcomes. Am J Epidemiol 2021;190:161–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Galanis P, Vraka I, Fragkou D, Bilali A, Kaitelidou D. Seroprevalence of SARS-CoV-2 antibodies and associated factors in healthcare workers: a systematic review and meta-analysis. J Hosp Infect 2021;108:120–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Brown CS, Clare K, Chand M et al. Snapshot PCR surveillance for SARS-CoV-2 in hospital staff in England. J Infect 2020;81:427–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tjtrj P. The digitize package: extracting numerical data from scatterplots. RJ 2011;3:25–26. [Google Scholar]
- 15. Hall VJ, Foulkes S, Charlett A et al. ; SIREN Study Group. SARS-CoV-2 infection rates of antibody-positive compared with antibody-negative health-care workers in England: a large, multicentre, prospective cohort study (SIREN). Lancet 2021;397:1459–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Joslyn LR, Kirschner DE, Linderman JJ. CaliPro: a calibration protocol that utilizes parameter density estimation to explore parameter space and calibrate complex biological models. Cell Mol Bioeng 2021;14:31–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Evans S, Agnew E, Vynnycky E et al. The impact of testing and infection prevention and control strategies on within-hospital transmission dynamics of COVID-19 in English hospitals. Philos Trans R Soc Lond B Biol Sci 2021;376:20200268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. UK Health Security Agency. COVID-19: epidemiological definitions of outbreaks and clusters in particular settings. August 2020. https://www.gov.uk/government/publications/covid-19-epidemiological-definitions-of-outbreaks-and-clusters/covid-19-epidemiological-definitions-of-outbreaks-and-clusters-in-particular-settings (28 October 2021, date last accessed).
- 19. Bhattacharya A, Collin SM, Stimson J et al. Healthcare-associated COVID-19 in England: a national data linkage study. J Infect 2021. doi: 10.1016/j.jinf.2021.08.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Department of Health and Social Care. Statement from the UK Chief Medical Officers on an update to coronavirus symptoms. May 2020. https://www.gov.uk/government/news/statement-from-the-uk-chief-medical-officers-on-an-update-to-coronavirus-symptoms-18-may-2020 (28 October 2021, date last accessed).
- 21. UK Government. Official UK Coronavirus Dashboard. May 2020. https://coronavirus.data.gov.uk (28 October 2021, date last accessed).
- 22. Byambasuren O, Cardona M, Bell K, Clark J, McLaws M-L, Glasziou P. Estimating the extent of asymptomatic COVID-19 and its potential for community transmission: systematic review and meta-analysis. Off J Assoc Med Microbiol Infect Dis Canada 2020;5:223–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. UK Government. COVID-19: infection prevention and control (IPC). January 2020. https://www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-control (28 October 2021, date last accessed).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data available on request.