Abstract
Patients undergoing catheter ablation for atrial fibrillation (AF) are routinely admitted for observation overnight in the hospital. With the rising incidence of AF among the population, increased volumes of procedures are placing increased demands on hospital resources. The purpose of this study was to evaluate the efficacy and safety of same day discharge in patients undergoing ablation for AF when compared to patients admitted for overnight observation. We performed a retrospective analysis using a multicenter cohort among patients who were discharged home after elective pulmonary vein isolation (PVI) ablation for AF. In our analysis, we found no statistically significant difference between patients discharged on the day of their procedure when compared to patients admitted for overnight observation in terms of 90-day readmission, major adverse cardiovascular events and death. This study shows that same day discharge after AF ablation is a feasible option. Future studies are needed to elicit the appropriate protocol to use.
Keywords: Atrial Fibrillation, Pulmonary Vein Isolation, Same Day Discharge
Introduction
Atrial Fibrillation (AF) is the most commonly diagnosed cardiac arrhythmia, with an estimated 6.1 million cases in the United States and is expected to double by 2030 1. Catheter ablation for AF is a common procedure performed to scar or eliminate the triggers that cause AF. It is an effective treatment and has been shown to be superior to antiarrhythmic therapy in patients with symptomatic AF. With continued advancement in pulmonary vein (PV) ablation, procedural outcomes have seen tremendous improvement while complications have gone down significantly These factors have led to an increased number of AF ablation procedures being performed 2-4.
It is common practice and expert medical consensus to keep patients overnight in the hospital after an AF ablation procedure. However, the inpatient costs are extremely high and the increased number of procedures being performed place increased demand on the healthcare system 5. Furthermore, the emergence of the COVID-19 pandemic has greatly affected health care delivery worldwide. A massive reallocation of health care resources has created major obstacles to routine medical care in addition to the need to limit disease transmission as infected patients fill hospital beds. As a result, research is being done to evaluate more cost-efficient models of post-ablation care without compromising the quality of the current practice or risking further complications in patients. This has led to research being performed on the efficacy and safety of early or same-day discharge after AF ablation. Research has already been performed showing same-day discharge is safe and effective for less complex ablations such as atrial flutter. AF ablation is generally a more complex procedure with longer sedation times and higher levels of anticoagulation 6-7.
The purpose of this study is to examine the potential relationship between patients undergoing AF ablation being discharged on the same day versus the standard overnight hospital admission.
Methods
Data Collection
This is a retrospective multicenter cohort study among patients who were discharged home after elective pulmonary vein isolation (PVI) ablation for AF at hospitals and surgical centers in the United States run by Hospital Corporations of America (HCA) between January 2015 and December 2018. All outpatient procedures in adults over 18 years of age were included. Patients who were inpatient or were hospitalized over 48 hours were excluded.
Inclusion Criteria:
. Age > 18 years
. Outpatient PVI ablation
. Hospital stay <48 hours.
Exclusion Criteria
. An inpatient stay prior to the procedure
. Hospital stay > 48 hours post-procedure.
Using the above-mentioned inclusion-exclusion criteria, patient encounters were pulled by data analysts using CPT codes for PVI ablation. Patient encounters that met the exclusion criteria were eliminated and resultant encounters were used for the study. 17,724 ablation procedures were pulled from HCA’s electronic data warehouse. 14,290 of these patients underwent PVI ablation on the day they presented to the hospital. Admissions < 48hours were randomly selected from these patients leaving a patient population of 13,567 patients.
Patient data included patient demographics, date of admission, date of discharge and home medications. Limited medical history was obtained through ICD 10 codes. Readmission at 90 days was evaluated by reviewing the patient encounters and matching with the patient account number (e.g., if the same account number had a second encounter within 90 days after the date of the procedure, it qualifies for all-cause readmission). Principal and sub investigators were blinded and provided with de-identified data only [Table 1].
Table 1. Patient Encounters.
| Number of Patient Encounters | |
|---|---|
| Same-day discharge | 1255 |
| Overnight stay | 12312 |
| Total | 13567 |
Table 1. table 1.
Data Analysis
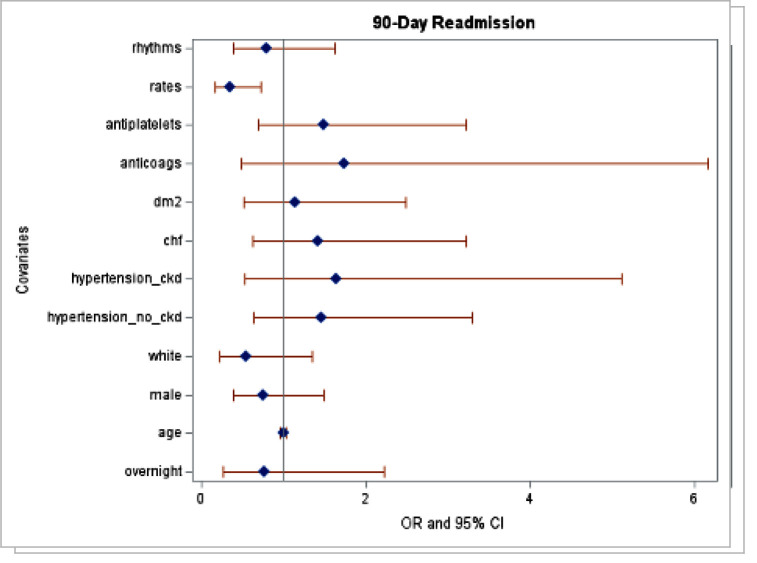
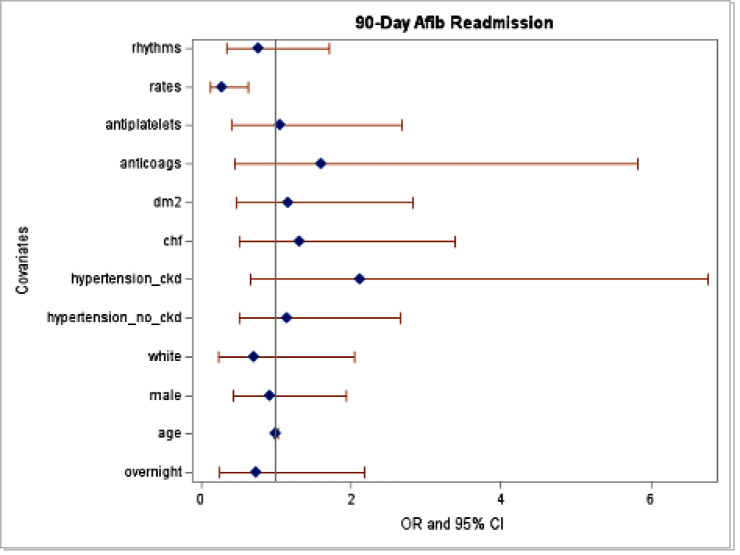
The resultant data was entered into SPSS software for analysis. Logistic regression analysis was made to evaluate for 90-day readmission rates. Multiple logistic regression was performed for both 90-day all cause readmission and 90-day AF readmission. Variables included in the model are overnight status, age, sex, race (white/other), hypertension without CKD, hypertension with CKD, CHF, diabetes type II, anticoagulants, antiplatelets, rate control medications, and rhythm control medications.
Results
There was no statistically significant difference in mortality, major adverse cardiovascular events, 90-day all-cause readmission or 90-day AF readmissions. A logistic regression analysis was performed and found no statistically significant difference between patients who were admitted overnight when compared to patients discharged on the same day as their AF ablation in terms of 90-day all-cause readmission and 90-day AF readmission. In a subgroup analysis, there was a statistically significant decrease in 90-day all-cause readmission in patients discharged on rate lowering medications versus those who were not (p-value 0.005, OR 0.358, 95% CI 0.175-0.734) [Table 2]-[Table 3]-[Table 4].
Table 2. Patient Distribution.
| Same-day discharge (N=1255) | Overnight Stay (N=12312) | |||||
|---|---|---|---|---|---|---|
| Yes | No | % | Yes | No | % | |
| Mortality | 1 | 1254 | 0.08 | 4 | 12308 | 0.03 |
| 90-day all-cause readmission | 5 | 1250 | 0.4 | 31 | 12281 | 0.25 |
| 90-day AFib readmission | 5 | 1250 | 0.40 | 24 | 12288 | 0.20 |
Table 3. 90-day All-Cause Readmissions.
| Adjusted Odds Ratio | 95% CI | P-value | |
|---|---|---|---|
| Overnight | 0.771 | 0.266-2.238 | 0.633 |
| Age | 0.994 | 0.962-1.026 | 0.709 |
| Male | 0.754 | 0.385-1.477 | 0.411 |
| HTN/no CKD | 1.472 | 0.653-3.315 | 0.351 |
| HTN/CKD | 1.724 | 0.557-5.334 | 0.344 |
| CHF | 1.433 | 0.632-3.246 | 0.389 |
| DM 2 | 1.178 | 0.539-2.577 | 0.682 |
| Anticoagulant Medication | 1.732 | 0.487-6.154 | 0.396 |
| Anti-platelet Medication | 1.472 | 0.684-3.167 | 0.322 |
| Rate Control Therapy | 0.358 | 0.175-0.734 | 0.005 |
| Rhythm Control Therapy | 0.805 | 0.398-1.629 | 0.545 |
Table 4. 90- Day AF Readmission.
| Adjusted Odds Ratio | 95% CI | P-value | |
|---|---|---|---|
| Overnight | 0.736 | 0.248-2.183 | 0.58 |
| Overnight | 0.999 | 0.975-1.024 | 0.949 |
| Male | 0.91 | 0.427-1.94 | 0.807 |
| HTN/no CKD | 1.148 | 0.498-2.645 | 0.745 |
| HTN/with CKD | 2.171 | 0.684-6.894 | 0.188 |
| CHF | 1.323 | 0.515-3.398 | 0.56 |
| DM 2 | 1.187 | 0.49-2.878 | 0.704 |
| Anticoagulant Medication | 1.602 | 0.441-5.819 | 0.474 |
| Anti-platelet Medication | 1.036 | 0.405-2.649 | 0.941 |
| Rate Control Therapy | 0.276 | 0.12-0.638 | 0.003 |
| Rhythm Control Therapy | 0.767 | 0.344-1.71 | 0.516 |
Table 2. table 2.
Discussion
AF is the most prevalent cardiac arrhythmia in clinical practice. The incidence and prevalence of AF are expected to increase drastically over the next decades, further increasing procedural volumes for AF ablation and hospital demand. Catheter ablation for AF is the most common ablation procedure and typically requires at least one overnight hospital stay 8-10. The new burdens placed upon the healthcare industry by the COVID-19 pandemic have further compromised the delivery of these procedures for many institutions worldwide. Given the current state of the COVID-19 pandemic, many institutions have elected to reduce non-urgent procedures to preserve resources, reduce viral transmission and maximize hospital capacity. A model of same day discharge for patients undergoing ablation for atrial fibrillation may play an important role in the post-surge period as well as throughout seasonal pandemic fluctuations in the future.
Census projection estimated approximately three million individuals in the U.S. with a diagnosis of AF in 2020, with a projected increase to ~5.6 million people by 2050 11. With the growing number of diagnoses, AF ablation procedures have continued to rise with a decrease in complications. Thus far there is no standardized recommendation regarding discharge time after catheter ablation. Historically, the majority of centers have and many still admit patients for at least one overnight stay following AF ablation procedures 12-15. A same day discharge approach can not only improve patient experience and satisfaction, but it can reduce the burden on our healthcare system and cut down on unnecessary healthcare costs.
There are a growing number of studies investigating same-day discharge. Deyell et al reported on over 3,000 patients at two centers in Canada undergoing same-day discharge for AF ablation. In their study, the primary reason for later discharge were access site problems, intraprocedural complications, late procedure times, and complications related to anesthesia 13-19. Other studies have shown up to 80% of patients undergoing AF ablation may be amenable to same-day discharge if avoidable delays in care and complications had been anticipated. Many studies were conducted at single centers and have used protocols and patient selection when addressing same-day discharge 20-25. Our study is unique in that it was conducted across multiple centers across the nation and no patient selection or protocols were implemented. Despite this, our results still showed no significant difference in mortality, MACE, or 90-day readmission in patients undergoing PVI ablation for AF when discharge on the same day as the procedure.
This retrospective multicenter cohort study among patients who were discharged home after elective PVI ablation for AF showed that same-day discharge was not associated with a statistically increased rate of morbidity, mortality, or 90-day readmission rates. In fact, our subgroup analysis showed that being on rate control medications may have a higher impact on readmission than same day discharge. We included this subgroup along with patients on rhythm control medications to be included in our logistical regression analysis to control for confounding variables. Interestingly, being on rate control and not rhythm control was associated with a decrease in readmission rates.
Same day discharge after AF ablation has the potential to reduce healthcare utilization, increase patient satisfaction and lessen the cost per patient encounter. Delivering cost effective healthcare while not compromising the quality of care should be of utmost importance. This study should provide more data reassuring that same-day discharge is safe for the majority of patients undergoing AF ablation. Future research regarding the design of specific protocols and the optimal patient selection are needed.
Limitations
Discharging patients on the same day after the AF ablation procedure is not a common practice. Due to this, our study is limited to an unevenly low distribution of patients who were discharged on the same day. It also affected the distribution of patients based on various demographics. This is a multicenter study involving patient encounters in hospital settings and hospitals. Due to this, there are various confounding factors like operator skill, lab facility, post-operative care management, recognition of immediate complications and follow up care. Regarding decreased readmission in patients on rate control therapy, we included this subgroup along with patients on rhythm control medications to be included in our logistical regression analysis to control for confounding variables. Interestingly, being on rate control and not rhythm control was associated with a decrease in readmission rates. This may be because patients on rhythm control had more refractory or medication-resistant atrial fibrillation. The study was also not specifically powered to look at rate vs. rhythm control, so results should be interpreted with caution.
Conclusions
Our study adds to the growing amount of evidence pointing to the safety and efficacy of same day discharge in patients undergoing AF ablation. Further studies are warranted investigating factors that place patients at increased risk for adverse events at same day discharge.
References
- 1.Colilla Susan, Crow Ann, Petkun William, Singer Daniel E, Simon Teresa, Liu Xianchen. Estimates of current and future incidence and prevalence of atrial fibrillation in the U.S. adult population. Am J Cardiol. 2013 Oct 15;112 (8):1142–7. doi: 10.1016/j.amjcard.2013.05.063. [DOI] [PubMed] [Google Scholar]
- 2.Mujović Nebojša, Marinković Milan, Lenarczyk Radoslaw, Tilz Roland, Potpara Tatjana S. Catheter Ablation of Atrial Fibrillation: An Overview for Clinicians. Adv Ther. 2017 Aug;34 (8):1897–1917. doi: 10.1007/s12325-017-0590-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim Michael H, Johnston Stephen S, Chu Bong-Chul, Dalal Mehul R, Schulman Kathy L. Estimation of total incremental health care costs in patients with atrial fibrillation in the United States. Circ Cardiovasc Qual Outcomes. 2011 May;4 (3):313–20. doi: 10.1161/CIRCOUTCOMES.110.958165. [DOI] [PubMed] [Google Scholar]
- 4.Prabhu Sandeep, Voskoboinik Aleksandr, Kaye David M, Kistler Peter M. Atrial Fibrillation and Heart Failure - Cause or Effect? Heart Lung Circ. 2017 Sep;26 (9):967–974. doi: 10.1016/j.hlc.2017.05.117. [DOI] [PubMed] [Google Scholar]
- 5.N Akula Devender, Mariam Wassef, Luthra Pallavi, Edward Friedrich, J Katz Daniel, A Levi Steven, Alfred Sacchetti. Safety of Same Day Discharge after Atrial Fibrillation Ablation. J Atr Fibrillation. 2020 May 22;12 (5) doi: 10.4022/jafib.2150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ganesan Anand N, Shipp Nicholas J, Brooks Anthony G, Kuklik Pawel, Lau Dennis H, Lim Han S, Sullivan Thomas, Roberts-Thomson Kurt C, Sanders Prashanthan. Long-term outcomes of catheter ablation of atrial fibrillation: a systematic review and meta-analysis. J Am Heart Assoc. 2013 Mar 18;2 (2) doi: 10.1161/JAHA.112.004549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ahmed Asrar, Ullah Waqas, Hussain Ishtiaq, Roomi Sohaib, Sattar Yasar, Ahmed Faizan, Saeed Rehan, Ashfaq Ammar. Atrial fibrillation: a leading cause of heart failure-related hospitalizations; a dual epidemic. Am J Cardiovasc Dis. 2019;9 (5):109–115. [PMC free article] [PubMed] [Google Scholar]
- 8.Morillo Carlos A, Banerjee Amitava, Perel Pablo, Wood David, Jouven Xavier. Atrial fibrillation: the current epidemic. J Geriatr Cardiol. 2017 Mar;14 (3):195–203. doi: 10.11909/j.issn.1671-5411.2017.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Terasawa Teruhiko, Balk Ethan M, Chung Mei, Garlitski Ann C, Alsheikh-Ali Alawi A, Lau Joseph, Ip Stanley. Systematic review: comparative effectiveness of radiofrequency catheter ablation for atrial fibrillation. Ann Intern Med. 2009 Aug 04;151 (3):191–202. doi: 10.7326/0003-4819-151-3-200908040-00131. [DOI] [PubMed] [Google Scholar]
- 10.Khaykin Yaariv, Morillo Carlos A, Skanes Allan C, McCracken Aaron, Humphries Karin, Kerr Charles R. Cost comparison of catheter ablation and medical therapy in atrial fibrillation. J Cardiovasc Electrophysiol. 2007 Sep;18 (9):907–13. doi: 10.1111/j.1540-8167.2007.00902.x. [DOI] [PubMed] [Google Scholar]
- 11.Lip Gregory Y H, Kakar Puneet, Watson Timothy. Atrial fibrillation--the growing epidemic. Heart. 2007 May;93 (5):542–3. doi: 10.1136/hrt.2006.110791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kowalski Marcin, Parikh Valay, Salcido Jose R, Chalfoun Nagib, Albano Alfred, O'Neill Padraig G, Bowers Mark R, Gauri Andre, Braegelmann Kendra M, Lim Hae W, Akhrass Philippe, Shah Rina, Bekheit Soad, Epstein Laurence M, Aryana Arash. Same-day discharge after cryoballoon ablation of atrial fibrillation: A multicenter experience. J Cardiovasc Electrophysiol. 2021 Feb;32 (2):183–190. doi: 10.1111/jce.14843. [DOI] [PubMed] [Google Scholar]
- 13.Deyell Marc W, Leather Richard A, Macle Laurent, Forman Jacqueline, Khairy Paul, Zhang Ruth, Ding Lillian, Chakrabarti Santabhanu, Yeung-Lai-Wah John A, Lane Christopher, Novak Paul G, Sterns Laurence D, Bennett Matthew T, Laksman Zachary W, Sikkel Markus B, Andrade Jason G. Efficacy and Safety of Same-Day Discharge for Atrial Fibrillation Ablation. JACC Clin Electrophysiol. 2020 Jun;6 (6):609–619. doi: 10.1016/j.jacep.2020.02.009. [DOI] [PubMed] [Google Scholar]
- 14.Creta Antonio, Ventrella Nicoletta, Providência Rui, Earley Mark J, Sporton Simon, Dhillon Gurpreet, Papageorgiou Nikolaos, Chow Anthony, Lambiase Pier D, Lowe Martin, Schilling Richard J, Finlay Malcolm, Hunter Ross J. Same-day discharge following catheter ablation of atrial fibrillation: A safe and cost-effective approach. J Cardiovasc Electrophysiol. 2020 Dec;31 (12):3097–3103. doi: 10.1111/jce.14789. [DOI] [PubMed] [Google Scholar]
- 15.Bartoletti Stefano, Mann Mandeep, Gupta Akanksha, Khan Abdul Muhaymin, Sahni Ankita, El-Kadri Moutaz, Modi Simon, Waktare Johan, Mahida Saagar, Hall Mark, Snowdon Richard, Todd Derick, Gupta Dhiraj. Same-day discharge in selected patients undergoing atrial fibrillation ablation. Pacing Clin Electrophysiol. 2019 Nov;42 (11):1448–1455. doi: 10.1111/pace.13807. [DOI] [PubMed] [Google Scholar]
- 16.Marijon Eloi, Albenque Jean-Paul, Boveda Serge, Jacob Sophie, Schmutz Mathieu, Bortone Agustin, Combes Nicolas, Zimmermann Marc. Feasibility and safety of same-day home discharge after radiofrequency catheter ablation. Am J Cardiol. 2009 Jul 15;104 (2):254–8. doi: 10.1016/j.amjcard.2009.03.024. [DOI] [PubMed] [Google Scholar]
- 17.Chu Edward, Zhang Chi, Musikantow Daniel R, Turagam Mohit K, Langan Noelle, Sofi Aamir, Choudry Subbarao, Syros Georgios, Miller Marc A, Koruth Jacob S, Whang William, Dukkipati Srinivas R, Reddy Vivek Y. Barriers and financial impact of same-day discharge after atrial fibrillation ablation. Pacing Clin Electrophysiol. 2021 Apr;44 (4):711–719. doi: 10.1111/pace.14217. [DOI] [PubMed] [Google Scholar]
- 18.Haegeli Laurent M, Duru Firat, Lockwood Evan E, Lüscher Thomas F, Sterns Laurence D, Novak Paul G, Leather Richard A. Feasibility and safety of outpatient radiofrequency catheter ablation procedures for atrial fibrillation. Postgrad Med J. 2010 Jul;86 (1017):395–8. doi: 10.1136/pgmj.2009.092510. [DOI] [PubMed] [Google Scholar]
- 19.Ignacio Dr Mondragon, Jarma Dr Joaquín J, Nicolas Vecchio, Gustavo Daquarti, Leandro Tomas, Milagros Caro, Vasquez Elias, Alberto Giniger, Santiago Rivera, Gaston Albina, Fernando Scazzuso. Current Safety of Pulmonary Vein Isolation in Paroxysmal Atrial Fibrillation: First Experience of Same Day Discharge. J Atr Fibrillation. 2018 Dec;11 (4) doi: 10.4022/jafib.2077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rajendra Anil, Hunter Tina D, Morales Gustavo, Osorio Jose. Prospective implementation of a same-day discharge protocol for catheter ablation of paroxysmal atrial fibrillation. J Interv Card Electrophysiol. 2021 Nov;62 (2):419–425. doi: 10.1007/s10840-020-00914-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.König Sebastian, Svetlosak Martin, Grabowski Marcin, Duncker David, Nagy Vivien K, Bogdan Stefan, Vanduynhoven Philippe, Sohaib Syed Mohammad Afzal, Malaczynska-Raipold Katarzyna, Lane Deirdre A, Lenarczyk Radoslaw, Bollmann Andreas, Hindricks Gerhard, Potpara Tatjana S, Kosiuk Jedrzej. Utilization and perception of same-day discharge in electrophysiological procedures and device implantations: an EHRA survey. Europace. 2021 Jan 27;23 (1):149–156. doi: 10.1093/europace/euaa301. [DOI] [PubMed] [Google Scholar]
- 22.Sahashi Yuki, Kawamura Iwanari, Aikawa Tadao, Takagi Hisato, Briasoulis Alexandros, Kuno Toshiki. Safety and feasibility of same-day discharge in patients receiving pulmonary vein isolation-systematic review and a meta-analysis. J Interv Card Electrophysiol. 2021 Feb 25; () doi: 10.1007/s10840-021-00967-3. [DOI] [PubMed] [Google Scholar]
- 23. Lakkireddy D. Safety of same day discharge after atrial fibrillation ablation. 2020;12(5):2150. Journal of Atrial Fibrillation. . 2020;0:2150. doi: 10.4022/jafib.2150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Field Michael E, Goldstein Laura, Corriveau Kevin, Khanna Rahul, Fan Xiaozhou, Gold Michael R. Same-day discharge after catheter ablation in patients with atrial fibrillation in a large nationwide administrative claims database. J Cardiovasc Electrophysiol. 2021 Sep;32 (9):2432–2440. doi: 10.1111/jce.15193. [DOI] [PubMed] [Google Scholar]
- 25.Reddy S Ashwin, Nethercott Sarah L, Chattopadhyay Rahul, Heck Patrick M, Virdee Mohan S. Safety, Feasibility and Economic Impact of Same-Day Discharge Following Atrial Fibrillation Ablation. Heart Lung Circ. 2020 Dec;29 (12):1766–1772. doi: 10.1016/j.hlc.2020.02.016. [DOI] [PubMed] [Google Scholar]