Abstract
Background
Smartphone technologies have been recently developed to assess heart rate and rhythm, but their role in accurately detecting atrial fibrillation (AF) remains unknown.
Objective
We sought to perform a meta-analysis using prospective studies comparing Smartwatch technology with current monitoring standards for AF detection (ECG, Holter, Patch Monitor, ILR).
Methods
We performed a comprehensive literature search for prospective studies comparing Smartwatch technology simultaneously with current monitoring standards (ECG, Holter, and Patch monitor) for AF detection since inception to November 25th, 2019. The outcome studied was the accuracy of AF detection. Accuracy was determined with concomitant usage of ECG monitoring, Holter monitoring, loop recorder, or patch monitoring.
Results
A total of 9 observational studies were included comparing smartwatch technology, 3 using single-lead ECG monitoring, and six studies using photoplethysmography with routine AF monitoring strategies. A total of 1559 patients were enrolled (mean age 63.5 years, 39.5% had an AF history). The mean monitoring time was 75.6 days. Smartwatch was non-inferior to composite ECG monitoring strategies (OR 1.06, 95% CI 0.93 – 1.21, p=0.37), composite 12 lead ECG/Holter monitoring (OR 0.90, 95% CI 0.62 – 1.30, p=0.57) and patch monitoring (OR 1.28, 95% CI 0.84 - 1.94, p=0.24) for AF detection. The sensitivity and specificity for AF detection using a smartwatch was 95% and 94%, respectively.
Conclusions
Smartwatch based single-lead ECG and photoplethysmography appear to be reasonable alternatives for AF monitoring.
Keywords: Smartwatch, Atrial Fibrillation, Photoplethysmography
Introduction
Atrial fibrillation (AF) is the most common cardiac arrhythmias affecting over 33.5 million people worldwide, increasing morbidity and mortality 1-3. AF is frequently subclinical or paroxysmal, which causes a significant barrier to its expedient diagnosis and treatment. Electrocardiogram (ECG) is often normal between the episodes and reflects only single time-point measurements. Other implantable or recording devices are limited by user activation, external factors and are either expensive or invasive. Photoplethysmography was recently developed and implemented in wearable Smartwatches in 2017, providing a cost-effective and non-invasive means for continuous ECG monitoring. Over the past two years, several large-scale prospective trials have compared Smartwatch technology with current monitoring standards for AF detection, such as ECG, Holter Monitor (HM), Implantable Loop Recorder (ILR), and Patch Monitoring (PM). Since initial development, several studies have become available comparing smartwatch technology with the current standards 4-12. Hence, we performed a meta-analysis comparing the accuracy of Smartwatch-based single-lead ECG and PPG to current monitoring standards for AF detection.
Methods
Search Strategy
The initial search strategy was developed by two authors (KA and GM). Systematic search, without language restriction, using PubMed, EMBASE, SCOPUS, Google Scholar, and ClinicalTrials.gov from inception to November 25th, 2019 using the keywords: “smartwatch” OR “watch” AND “atrial fibrillation” or “watch” AND “atrial fibrillation detection.”
Study Selection
The eligibility criteria our systematic review and meta-analysis included:
1. All prospective studies reporting clinical outcomes comparing Smartwatch technology simultaneously with current monitoring standards (ECG, Holter, and Patch monitor).
2. Human subjects aged ≥ 18 years
3. Studies in the English language.
Case reports, editorial, and systematic reviews were excluded.
Data Extractions
Two investigators independently performed the literature search and screened all titles and full-text versions of all relevant studies that met the study inclusion criteria.
The references of all identified articles were also reviewed for relevant studies meeting the eligibility criteria. The data from the included studies were extracted using a standardized protocol and a data extraction form. Any discrepancies between the two investigators were resolved with a consultation with the senior investigator (DL). The following data were extracted: title, year of publication, type of study, mean age, sample size, baseline technology used, specific watch used, the specific algorithm used for AF detection, comparator modality, the quantity of ECG leads, and time monitored [Table 1]. Quantitative data on AF detection, including a discrete number of AF events, sensitivity, and specificity, were obtained [Table 2]). The Newcastle Ottawa Scale [Table 3] was used to appraise the quality of the included studies 13. We rated the quality of the studies (good, fair, and poor) by awarding stars in each domain. A “good” quality score required 3 or 4 stars in the selection, 1 or 2 stars in comparability, and 2 or 3 stars in outcomes. A “fair” quality score required 2 stars in the selection, 1 or 2 stars in comparability, and 2 or 3 stars in outcomes. A “poor” quality score reflected 0 or 1 star(s) in selection, or 0 stars in comparability, or 0 or 1 star(s) in outcomes.
Table 1. Baseline characteristics of the studies included in our meta-analysis.
* for Plethysmograph
SW: Smartwatch
♱ for iPhone ECG
PPI: Pulse-pulse intervals
| Study | Perez et al | Bashar et al | Wasserlauf et al | Dorr et al | Tison et al | Bumgarner et al | Faranesh et al | Rajakariar et al | Genicot et al |
|---|---|---|---|---|---|---|---|---|---|
| Year | 2019 | 2019 | 2019 | 2019 | 2018 | 2018 | 2019 | 2019 | 2018 |
| Type | Prospective | Prospective | Prospective | Prospective | Prospective | Prospective | Prospective | Prospective | Prospective |
| Mean Age | 59 | N/A | 72.1 | 76.4 | 42 | 68 | N/A | 67 | 60 |
| # enrolled | 450 | 37 | 24 | 508*, 549♱ | 51 | 93 | 96 | 200 | 100 |
| Baseline tech used | Plethysmo-graph | Plethysmo-graph | Kardiaband | Plethysmo-graph | Plethysmo-graph | SW single lead ECG (Kardia band) | Plethysmo-graph | SW single lead ECG (iPhone ECG) | Plethysmo-graph |
| Specific watch used | Apple Watch | Samsung Simband | Apple Watch | Samsung Gear Fit2 | Apple Watch | Apple Watch | Fitbit SW | N/A | N/A |
| Specific algorithm used | PPI on plethysmo-graphy | PPI on plethysmo-graphy | Smart- Rhythm 2.0 (Kardia band) | PPI on plethysmo-graphy | PPI on plethysmo-graphy | Kardiaband | N/A | Kardiaband | PPI on plethysmo-graphy |
| Comparator | 7-day ECG patch - single lead | Holter Monitor | Reveal LINQ | iPhone ECG | Ambulatory ECG post-cardioversion | Ambulatory ECG post-cardioversion | Single lead ECG patch (Cardea SOLO) | 12-lead ECG | 24-hour Holter Monitor |
| # of leads in comparator | Single | Multiple | Single | Single | 12-lead | 12-lead | Single | 12-lead | 12-lead |
| Time monitored | 117 days | N/A | 31,349 hours | 1 min each | 30 min | 30 second strips | 7 days | N/A | 99 days |
Table 2. Quantitative Evaluation of Atrial Fibrillation Events Detected.
* for Plethysmograph
AF: Atrial Fibrillation
♱ for iPhone ECG
SW: Smartwatch
| Study | Perez et al | Bashar et al | Wasserlauf et al | Dorr et al | Tison et al | Bumgarner et al | Faranesh et al | Rajakariar et al | Genicot et al |
|---|---|---|---|---|---|---|---|---|---|
| # enrolled | 450 | 37 | 24 | 508*,549♱ | 51 | 93 | 96 | 200 | 100 |
| # with AF | 153 | 10 | 24 | 237 | 51 | 93 | 35 | 38 | N/A |
| % with AF | 34 | 27 | 100 | 46.65 | 100 | 100 | 36.46 | 19 | N/A |
| Sensitivity of SW AF detection | N/A | 98.18% | 97.70% | 93.70% | 98% | 93% | N/A | 89.5% | N/A |
| Specificity of SW AF detection | N/A | 98.07% | 98.90% | 98.20% | 90.20% | 84 | N/A | 94.40% | N/A |
Table 3. Qualitative Evaluation of Included Studies Using Newcastle-Ottawa Scale.
| Study | Selection(max 4 stars) | Comparability(max 2 stars) | Outcome(max 3 stars) |
|---|---|---|---|
| Perez et al | **** | ** | *** |
| Bashar et al | *** | ** | ** |
| Wasserlauf et al | **** | ** | *** |
| Dorr et al | **** | ** | *** |
| Tison et al | **** | ** | ** |
| Bumgarner et al | **** | ** | *** |
| Faranesh et al | **** | ** | *** |
| Rajakariar et al | **** | ** | ** |
| Genicot et al | **** | ** | *** |
Outcomes
The primary outcome evaluated in our study was the accuracy of AF detection. Accuracy was determined with concomitant usage of ECG monitoring, Holter monitoring, loop recorder, or patch monitoring.
Statistical Analysis
Statistical analysis for odds ratio (OR) estimates of each study was calculated using Stata (Version 16.1, StataCorp, College Station, TX 77845). Subsequent meta-analysis was performed using Comprehensive Meta-Analysis (CMA) software (version. 3.3.070, Biostat, Englewood, NJ 07631) with a random-effects model. Results were expressed as an OR with a 95% confidence interval (CI). Higgins I-squared (I2) was used to quantify heterogeneity (I2<50% was defined as low) 14. P < 0.05 was considered statistically significant. Sensitivity analyses were performed for outcomes that demonstrated significant heterogeneity (I2 >50%) to assess the individual contribution to the aggregate. Funnel plots were also used in conjunction with sensitivity analysis to assess for publication bias.
Results
Search Results and study characteristics
A total of 1,045 citations were identified [Figure 1] during the initial search. Nine hundred four records were excluded, and a total of 51 relevant articles were identified. After a detailed evaluation, nine articles ultimately met the inclusion criteria enrolling a total of 1,559 patients [Figure 1]. A total of 1559 patients were enrolled (mean age 63.5 years, 39.5% had an AF history). The mean monitoring time was 75.6 days. [Table 1] summarizes the study characteristics of the included trials.
Figure 1. PRISMA flow diagram.
Primary Outcome [Figure 2]
Figure 2. Diagnostic Utility of Smartwatch Technology for Atrial Fibrillation Detection: The Smartwatch-AF Study.
AF Detection
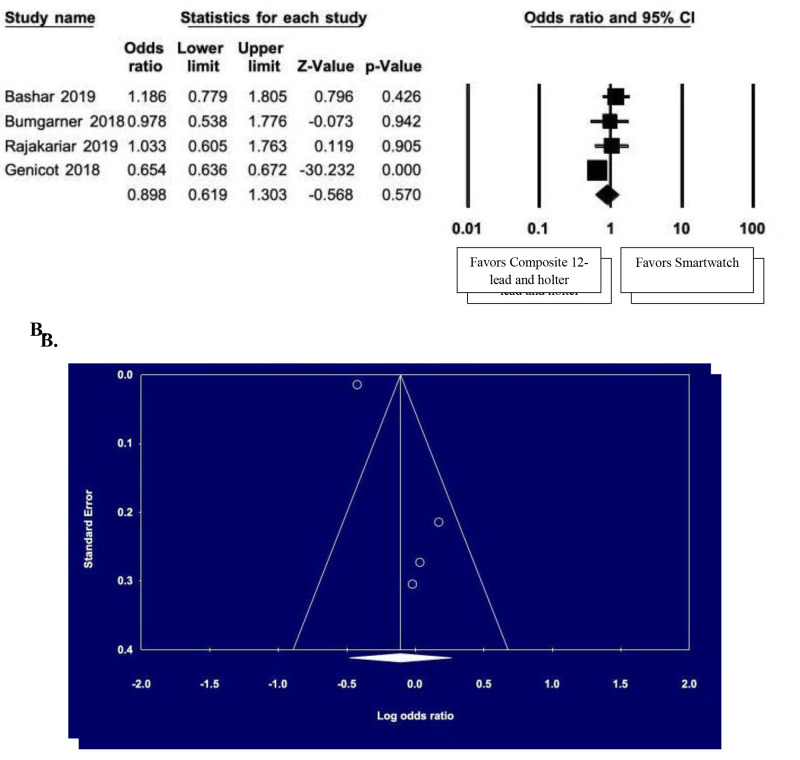
Smartwatch was non-inferior to composite ECG monitoring strategies (OR 1.06, 95% CI 0.93 – 1.21, p = 0.37) [Figure 3A], composite 12 lead ECG/Holter monitoring (OR 0.90, 95% CI 0.62 – 1.30, p = 0.57) [Figure 4A] and patch monitoring (OR 1.28, 95% CI 0.84 - 1.94, p = 0.24) [Figure 5A] for AF detection. Both mean sensitivity and specificity for AF detection using smartwatch was 95% and 94%, respectively. Several studies demonstrated statistically significant differences in AF sensing capability. Perez et al., Faranesh et al., and Tison et al. demonstrated statistically significant oversensing 4, 8, 10, while Wasserlauf et al. and Genicot et al. demonstrated smartwatch comparative undersensing 6, 12.
Figure 3. A. Smartwatch Monitoring vs. Composite ECG, Holter, Loop Recorder and Patch Monitor; B. Funnel plot demonstrating asymmetry suggestive of publication bias.
Figure 4. A. Smartwatch Monitoring vs. Composite 12-Lead ECG and Holter Monitoring; B. Funnel plot demonstrating asymmetry suggestive of publication bias.
Figure 5. Smartwatch Monitor vs. Patch Monitor.
Sensitivity Analysis
Due to significant heterogeneity observed in the primary outcome, a sensitivity analysis was performed by excluding one study at a time to see if any study had a substantial contribution to observed heterogeneity. The heterogeneity found may be associated with individual study differences, institutional variation, and the difference in evaluation among the included studies.
Sensitivity analysis performed on a composite analysis [Figure 3B] demonstrated no significant heterogeneity changes (I2 = 99.2%). In comparison, the reduction in heterogeneity (from I2 = 75.3% to 0%) was observed with the exclusion of Genicot et al., which had a significant proportion of weight in the study for watch monitoring vs. composite 12 lead and Holter monitoring comparison. This is consistent with the single study outlier noted in the corresponding funnel plot [Figure 4B]. Sensitivity analysis was not performed on watch monitoring vs. patch monitoring comparison as only two studies were included in the subgroup analysis (I2 = 99.1%).
Publication Bias
In addition to sensitivity analysis, publication bias was assessed visually using funnel plots [Figure 3], demonstrating asymmetrical funnel plot figures. Consequently, despite the overall findings of no difference between watch monitoring and routinely practiced wearable/implantable devices, results should be interpreted with caution (given funnel plot asymmetry and high heterogeneity).
Discussion
Our analysis demonstrated no significant difference in AF detection in Smartwatch monitoring compared to composite ECG monitoring, Holter monitoring, loop recorder, and patch monitoring [Figure 2]. There has been a progressive increase in the incidence and prevalence of AF worldwide, with an increased risk of morbidity and mortality. Atrial fibrillation is known to have a significant impact on health care costs, with the major cost-drivers being the loss of productivity, stroke, and hospitalizations 1. Studies have also shown that increased AF burden directly correlates with thromboembolic stroke risk 15-19. Accordingly, increased awareness of AF symptoms and early clinical diagnosis is imperative to prevent long term morbidity and mortality. Often, given the asymptomatic nature of paroxysmal AF, long term monitoring for detecting these clinically relevant silent AF episodes is essential 4, 20. Although cardiac implantable electronic devices are commonly used for monitoring of silent AF episodes, they are associated with potential disadvantages such as invasiveness of the procedure, procedure-related complications, and long-term patient discomfort 4. There is a growing need to develop non-invasive and wearable technology to enable continuous monitoring of silent arrhythmias in high-risk patients 21.
Photoplethysmography-based technology included in the smartwatches (Apple or Samsung) is regarded as the most accurate method for diagnosing AF 21-24. Photoplethysmography based smart devices; mobile health (Mobile Health) in combination with machine learning, has transformed patient care by precisely and accurately diagnosing AF 25-27. Photoplethysmography in smartwatches consists of an infrared light-emitting diode sensor that detects blood volume changes in the microvasculature , 28. The synchronous changes in blood volume in small blood vessels with each heartbeat are transformed into a physiological pulsatile waveform by Photoplethysmography 21, 28. It is regarded as a portable, low-cost, simple, and wearable technology most suitable for monitoring patients in primary care and community-based clinical settings 21. Furthermore, this technology has been formerly used for measuring oxygen saturation, blood pressure, cardiac output, autonomic changes, and peripheral vascular disease 4; with better reliability than previously used technologies such as pulse palpation, modified sphygmomanometers, and non–12-lead ECG for detection of AF episodes 29-31. Smartwatch-based arrhythmia detection (with a photoplethysmography-based AF detection) is a simple, non-invasive technique and a safer alternative to the routinely utilized AF detection tools.
Previous studies
Several studies have been conducted to assess the efficacy of photoplethysmography based smartwatch technologies for detecting AF episodes. The overall sensitivity and specificity for detecting AF episodes using smartphone technology is approximately 90-96% and 85-99%, respectively 32-37. ECG watchband (KardiaBand, AlivaCor, USA), which is connected to the Apple Watch, was first introduced in April 2017 for detecting AF [38]. Kardiaband was based on a proprietary algorithm (rhythm irregularity and absence of P waves) for AF detection 38 and transmitting a 30s segment of single-lead ECG via Bluetooth to the Apple Watch 38. Similarly, Bumgarner et al. compared the efficacy of the Apple Watch with a standard clinical 12 lead ECG in 100 AF patients and demonstrated that the sensitivity and specificity of the Apple Watch for detecting AF are 93% and 84%, respectively 39. Several other studies have used AlivaCor Kardia Mobile approaches and demonstrated that sensitivity and specificity were >95% 40-42. With the help of motion and noise artifacts and premature atrial contraction algorithms, photoplethysmography based smartwatch detected AF with higher sensitivity (98.18%), specificity (97.43%), and accuracy (97.54%) 5. According to Wasserlauf et al., AF-based smartwatches had higher sensitivity for detecting the AF episodes (episode sensitivity 97.5%) and AF duration (duration sensitivity 97.7%) as compared to implantable cardiac monitor (ICM) 6.
The WATCH-AF trial demonstrated relatively high sensitivity (93.7%), specificity (98.2%), overall accuracy (96.1%), positive predictive value (97.8%), and negative predictive value (94.7%) in diagnosing AF 7, findings that also echoes (comparing simultaneously performed 12-lead ECG) in a recently published study by Rajakariar et al. 43. Using single-channel electrocardiogram (ECG), multi-wavelength photoplethysmography, tri-axial accelerometry, the accuracy, sensitivity, and specificity of detecting AF episodes with Samsung Simband watch was 95%, 97%, and 94%, respectively [34]. Photoplethysmography based smartwatch technology combined with deep neural network passively predicted AF in patients undergoing cardioversion better than standard 12-lead ECG with higher sensitivity (94%) and specificity (90.2%) in an ambulatory care setting 8. Furthermore, although both Apple Watch Series 3 and Fitbit were equipped with Photoplethysmography technology, the precision and accuracy for AF detection was higher in Apple Watch Series 3 (75% correlation) as compared to Fitbit (FBT) Charge HR Wireless Activity Wristband (30% correlation) in a phase-II prospective clinical study conducted in Japan 28. The false-positive rate and accuracy of AF detection in healthy volunteers and AF patients using smartwatches with Photoplethysmography based algorithm was approximately 0.2% and 96%, respectively 44, thus demonstrating the efficacy of photoplethysmography based wearable devices accurately differentiating AF from sinus rhythm in at-risk patients 44.
Limitations
There are several limitations to the performed meta-analysis. The limitations did not include a comprehensive text and comparison to literature.
1. Patients with implantable cardiac pacemakers were excluded from the studies.
2. Some studies included patients with prior history of paroxysmal AF, while others excluded these patients, limiting the generalizability of the studies.
3. Study heterogeneity.
4. Variation in algorithms used for different devices.
5. Differences in metrics of assessment among different studies.
Conclusions
While composite 12-lead ECG, Holter monitor, implantable loop recorders, or patch recording are the standards for AF detection, photoplethysmography based smartwatch technology is a simple, efficient, and non-inferior alternative that may expedite detection and treatment of subclinical AF, preventing morbidity and mortality from stroke and cardiovascular disease.
References
- 1.Chugh Sumeet S, Havmoeller Rasmus, Narayanan Kumar, Singh David, Rienstra Michiel, Benjamin Emelia J, Gillum Richard F, Kim Young-Hoon, McAnulty John H, Zheng Zhi-Jie, Forouzanfar Mohammad H, Naghavi Mohsen, Mensah George A, Ezzati Majid, Murray Christopher J L. Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation. 2014 Feb 25;129 (8):837–47. doi: 10.1161/CIRCULATIONAHA.113.005119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Xian Ying, O'Brien Emily C, Liang Li, Xu Haolin, Schwamm Lee H, Fonarow Gregg C, Bhatt Deepak L, Smith Eric E, Olson DaiWai M, Maisch Lesley, Hannah Deidre, Lindholm Brianna, Lytle Barbara L, Pencina Michael J, Hernandez Adrian F, Peterson Eric D. Association of Preceding Antithrombotic Treatment With Acute Ischemic Stroke Severity and In-Hospital Outcomes Among Patients With Atrial Fibrillation. JAMA. 2017 Mar 14;317 (10):1057–1067. doi: 10.1001/jama.2017.1371. [DOI] [PubMed] [Google Scholar]
- 3.Wong Christopher X, Brooks Anthony G, Leong Darryl P, Roberts-Thomson Kurt C, Sanders Prashanthan. The increasing burden of atrial fibrillation compared with heart failure and myocardial infarction: a 15-year study of all hospitalizations in Australia. Arch Intern Med. 2012 May 14;172 (9):739–41. doi: 10.1001/archinternmed.2012.878. [DOI] [PubMed] [Google Scholar]
- 4.Perez Marco V, Mahaffey Kenneth W, Hedlin Haley, Rumsfeld John S, Garcia Ariadna, Ferris Todd, Balasubramanian Vidhya, Russo Andrea M, Rajmane Amol, Cheung Lauren, Hung Grace, Lee Justin, Kowey Peter, Talati Nisha, Nag Divya, Gummidipundi Santosh E, Beatty Alexis, Hills Mellanie True, Desai Sumbul, Granger Christopher B, Desai Manisha, Turakhia Mintu P. Large-Scale Assessment of a Smartwatch to Identify Atrial Fibrillation. N Engl J Med. 2019 Nov 14;381 (20):1909–1917. doi: 10.1056/NEJMoa1901183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bashar Syed Khairul, Han Dong, Hajeb-Mohammadalipour Shirin, Ding Eric, Whitcomb Cody, McManus David D, Chon Ki H. Atrial Fibrillation Detection from Wrist Photoplethysmography Signals Using Smartwatches. Sci Rep. 2019 Oct 21;9 (1) doi: 10.1038/s41598-019-49092-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wasserlauf Jeremiah, You Cindy, Patel Ruchi, Valys Alexander, Albert David, Passman Rod. Smartwatch Performance for the Detection and Quantification of Atrial Fibrillation. Circ Arrhythm Electrophysiol. 2019 Jun;12 (6) doi: 10.1161/CIRCEP.118.006834. [DOI] [PubMed] [Google Scholar]
- 7.Dörr Marcus, Nohturfft Vivien, Brasier Noé, Bosshard Emil, Djurdjevic Aleksandar, Gross Stefan, Raichle Christina J, Rhinisperger Mattias, Stöckli Raphael, Eckstein Jens. The WATCH AF Trial: SmartWATCHes for Detection of Atrial Fibrillation. JACC Clin Electrophysiol. 2019 Feb;5 (2):199–208. doi: 10.1016/j.jacep.2018.10.006. [DOI] [PubMed] [Google Scholar]
- 8.Tison Geoffrey H, Sanchez José M, Ballinger Brandon, Singh Avesh, Olgin Jeffrey E, Pletcher Mark J, Vittinghoff Eric, Lee Emily S, Fan Shannon M, Gladstone Rachel A, Mikell Carlos, Sohoni Nimit, Hsieh Johnson, Marcus Gregory M. Passive Detection of Atrial Fibrillation Using a Commercially Available Smartwatch. JAMA Cardiol. 2018 May 01;3 (5):409–416. doi: 10.1001/jamacardio.2018.0136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bumgarner Joseph M, Lambert Cameron T, Hussein Ayman A, Cantillon Daniel J, Baranowski Bryan, Wolski Kathy, Lindsay Bruce D, Wazni Oussama M, Tarakji Khaldoun G. Smartwatch Algorithm for Automated Detection of Atrial Fibrillation. J Am Coll Cardiol. 2018 May 29;71 (21):2381–2388. doi: 10.1016/j.jacc.2018.03.003. [DOI] [PubMed] [Google Scholar]
- 10.Ding Eric Y, Han Dong, Whitcomb Cody, Bashar Syed Khairul, Adaramola Oluwaseun, Soni Apurv, Saczynski Jane, Fitzgibbons Timothy P, Moonis Majaz, Lubitz Steven A, Lessard Darleen, Hills Mellanie True, Barton Bruce, Chon Ki, McManus David D. Accuracy and Usability of a Novel Algorithm for Detection of Irregular Pulse Using a Smartwatch Among Older Adults: Observational Study. JMIR Cardio. 2019 May 15;3 (1) doi: 10.2196/13850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rajakariar Kevin, Koshy Anoop N, Sajeev Jithin K, Nair Sachin, Roberts Louise, Teh Andrew W. Accuracy of a smartwatch based single-lead electrocardiogram device in detection of atrial fibrillation. Heart. 2020 May;106 (9):665–670. doi: 10.1136/heartjnl-2019-316004. [DOI] [PubMed] [Google Scholar]
- 12.M Genicot. Determining the Diagnostic Yield for Atrial Fibrillation Using Continuous Smartwatch Monitoring. Circulation. 2018;0:0–0. [Google Scholar]
- 13.Stang Andreas. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010 Sep;25 (9):603–5. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 14.Higgins Julian P T, Altman Douglas G, Gøtzsche Peter C, Jüni Peter, Moher David, Oxman Andrew D, Savovic Jelena, Schulz Kenneth F, Weeks Laura, Sterne Jonathan A C. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011 Oct 18;343 () doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mittal Suneet, Rogers John, Sarkar Shantanu, Koehler Jodi, Warman Eduardo N, Tomson Todd T, Passman Rod S. Real-world performance of an enhanced atrial fibrillation detection algorithm in an insertable cardiac monitor. Heart Rhythm. 2016 Aug;13 (8):1624–30. doi: 10.1016/j.hrthm.2016.05.010. [DOI] [PubMed] [Google Scholar]
- 16.Glotzer Taya V, Daoud Emile G, Wyse D George, Singer Daniel E, Ezekowitz Michael D, Hilker Christopher, Miller Clayton, Qi Dongfeng, Ziegler Paul D. The relationship between daily atrial tachyarrhythmia burden from implantable device diagnostics and stroke risk: the TRENDS study. Circ Arrhythm Electrophysiol. 2009 Oct;2 (5):474–80. doi: 10.1161/CIRCEP.109.849638. [DOI] [PubMed] [Google Scholar]
- 17.Van Gelder Isabelle C, Healey Jeff S, Crijns Harry J G M, Wang Jia, Hohnloser Stefan H, Gold Michael R, Capucci Alessandro, Lau Chu-Pak, Morillo Carlos A, Hobbelt Anne H, Rienstra Michiel, Connolly Stuart J. Duration of device-detected subclinical atrial fibrillation and occurrence of stroke in ASSERT. Eur Heart J. 2017 May 01;38 (17):1339–1344. doi: 10.1093/eurheartj/ehx042. [DOI] [PubMed] [Google Scholar]
- 18.Swiryn Steven, Orlov Michael V, Benditt David G, DiMarco John P, Lloyd-Jones Donald M, Karst Edward, Qu Fujian, Slawsky Mara T, Turkel Melanie, Waldo Albert L. Clinical Implications of Brief Device-Detected Atrial Tachyarrhythmias in a Cardiac Rhythm Management Device Population: Results from the Registry of Atrial Tachycardia and Atrial Fibrillation Episodes. Circulation. 2016 Oct 18;134 (16):1130–1140. doi: 10.1161/CIRCULATIONAHA.115.020252. [DOI] [PubMed] [Google Scholar]
- 19.Passman Rod, Leong-Sit Peter, Andrei Adin-Cristian, Huskin Anna, Tomson Todd T, Bernstein Richard, Ellis Ethan, Waks Jonathan W, Zimetbaum Peter. Targeted Anticoagulation for Atrial Fibrillation Guided by Continuous Rhythm Assessment With an Insertable Cardiac Monitor: The Rhythm Evaluation for Anticoagulation With Continuous Monitoring (REACT.COM) Pilot Study. J Cardiovasc Electrophysiol. 2016 Mar;27 (3):264–70. doi: 10.1111/jce.12864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sanna Tommaso, Diener Hans-Christoph, Passman Rod S, Di Lazzaro Vincenzo, Bernstein Richard A, Morillo Carlos A, Rymer Marilyn Mollman, Thijs Vincent, Rogers Tyson, Beckers Frank, Lindborg Kate, Brachmann Johannes. Cryptogenic stroke and underlying atrial fibrillation. N Engl J Med. 2014 Jun 26;370 (26):2478–86. doi: 10.1056/NEJMoa1313600. [DOI] [PubMed] [Google Scholar]
- 21.Allen John. Photoplethysmography and its application in clinical physiological measurement. Physiol Meas. 2007 Mar;28 (3):R1–39. doi: 10.1088/0967-3334/28/3/R01. [DOI] [PubMed] [Google Scholar]
- 22.Cadmus-Bertram Lisa, Gangnon Ronald, Wirkus Emily J, Thraen-Borowski Keith M, Gorzelitz-Liebhauser Jessica. The Accuracy of Heart Rate Monitoring by Some Wrist-Worn Activity Trackers. Ann Intern Med. 2017 Apr 18;166 (8):610–612. doi: 10.7326/L16-0353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang Robert, Blackburn Gordon, Desai Milind, Phelan Dermot, Gillinov Lauren, Houghtaling Penny, Gillinov Marc. Accuracy of Wrist-Worn Heart Rate Monitors. JAMA Cardiol. 2017 Jan 01;2 (1):104–106. doi: 10.1001/jamacardio.2016.3340. [DOI] [PubMed] [Google Scholar]
- 24.Wallen Matthew P, Gomersall Sjaan R, Keating Shelley E, Wisløff Ulrik, Coombes Jeff S. Accuracy of Heart Rate Watches: Implications for Weight Management. PLoS One. 2016;11 (5) doi: 10.1371/journal.pone.0154420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.White Ryan D, Flaker Greg. Smartphone-based Arrhythmia Detection: Should we encourage patients to use the ECG in their pocket? J Atr Fibrillation. 2017 Dec 19;9 (6) doi: 10.4022/jafib.1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cheung Christopher C, Krahn Andrew D, Andrade Jason G. The Emerging Role of Wearable Technologies in Detection of Arrhythmia. Can J Cardiol. 2018 Aug;34 (8):1083–1087. doi: 10.1016/j.cjca.2018.05.003. [DOI] [PubMed] [Google Scholar]
- 27.Turakhia Mintu P, Kaiser Daniel W. Transforming the care of atrial fibrillation with mobile health. J Interv Card Electrophysiol. 2016 Oct;47 (1):45–50. doi: 10.1007/s10840-016-0136-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Inui Tomohiko, Kohno Hiroki, Kawasaki Yohei, Matsuura Kaoru, Ueda Hideki, Tamura Yusaku, Watanabe Michiko, Inage Yuichi, Yakita Yasunori, Wakabayashi Yutaka, Matsumiya Goro. Use of a Smart Watch for Early Detection of Paroxysmal Atrial Fibrillation: Validation Study. JMIR Cardio. 2020 Jan 22;4 (1) doi: 10.2196/14857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Taggar Jaspal S, Coleman Tim, Lewis Sarah, Heneghan Carl, Jones Matthew. Accuracy of methods for detecting an irregular pulse and suspected atrial fibrillation: A systematic review and meta-analysis. Eur J Prev Cardiol. 2016 Aug;23 (12):1330–8. doi: 10.1177/2047487315611347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hobbs F D R, Fitzmaurice D A, Mant J, Murray E, Jowett S, Bryan S, Raftery J, Davies M, Lip G. A randomised controlled trial and cost-effectiveness study of systematic screening (targeted and total population screening) versus routine practice for the detection of atrial fibrillation in people aged 65 and over. The SAFE study. Health Technol Assess. 2005 Oct;9 (40):iii–iv, ix-x, 1-74. doi: 10.3310/hta9400. [DOI] [PubMed] [Google Scholar]
- 31.Freedman Ben, Camm John, Calkins Hugh, Healey Jeffrey S, Rosenqvist Mårten, Wang Jiguang, Albert Christine M, Anderson Craig S, Antoniou Sotiris, Benjamin Emelia J, Boriani Giuseppe, Brachmann Johannes, Brandes Axel, Chao Tze-Fan, Conen David, Engdahl Johan, Fauchier Laurent, Fitzmaurice David A, Friberg Leif, Gersh Bernard J, Gladstone David J, Glotzer Taya V, Gwynne Kylie, Hankey Graeme J, Harbison Joseph, Hillis Graham S, Hills Mellanie T, Kamel Hooman, Kirchhof Paulus, Kowey Peter R, Krieger Derk, Lee Vivian W Y, Levin Lars-Åke, Lip Gregory Y H, Lobban Trudie, Lowres Nicole, Mairesse Georges H, Martinez Carlos, Neubeck Lis, Orchard Jessica, Piccini Jonathan P, Poppe Katrina, Potpara Tatjana S, Puererfellner Helmut, Rienstra Michiel, Sandhu Roopinder K, Schnabel Renate B, Siu Chung-Wah, Steinhubl Steven, Svendsen Jesper H, Svennberg Emma, Themistoclakis Sakis, Tieleman Robert G, Turakhia Mintu P, Tveit Arnljot, Uittenbogaart Steven B, Van Gelder Isabelle C, Verma Atul, Wachter Rolf, Yan Bryan P. Screening for Atrial Fibrillation: A Report of the AF-SCREEN International Collaboration. Circulation. 2017 May 09;135 (19):1851–1867. doi: 10.1161/CIRCULATIONAHA.116.026693. [DOI] [PubMed] [Google Scholar]
- 32.Brasier Noé, Raichle Christina J, Dörr Marcus, Becke Adrian, Nohturfft Vivien, Weber Stefan, Bulacher Fabienne, Salomon Lorena, Noah Thierry, Birkemeyer Ralf, Eckstein Jens. Detection of atrial fibrillation with a smartphone camera: first prospective, international, two-centre, clinical validation study (DETECT AF PRO). Europace. 2019 Jan 01;21 (1):41–47. doi: 10.1093/europace/euy176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McManus David D, Lee Jinseok, Maitas Oscar, Esa Nada, Pidikiti Rahul, Carlucci Alex, Harrington Josephine, Mick Eric, Chon Ki H. A novel application for the detection of an irregular pulse using an iPhone 4S in patients with atrial fibrillation. Heart Rhythm. 2013 Mar;10 (3):315–9. doi: 10.1016/j.hrthm.2012.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nemati Shamim, Ghassemi Mohammad M, Ambai Vaidehi, Isakadze Nino, Levantsevych Oleksiy, Shah Amit, Clifford Gari D. Monitoring and detecting atrial fibrillation using wearable technology. Annu Int Conf IEEE Eng Med Biol Soc. 2016 Aug;2016 ():3394–3397. doi: 10.1109/EMBC.2016.7591456. [DOI] [PubMed] [Google Scholar]
- 35.Chan Pak-Hei, Wong Chun-Ka, Poh Yukkee C, Pun Louise, Leung Wangie Wan-Chiu, Wong Yu-Fai, Wong Michelle Man-Ying, Poh Ming-Zher, Chu Daniel Wai-Sing, Siu Chung-Wah. Diagnostic Performance of a Smartphone-Based Photoplethysmographic Application for Atrial Fibrillation Screening in a Primary Care Setting. J Am Heart Assoc. 2016 Jul 21;5 (7) doi: 10.1161/JAHA.116.003428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Krivoshei Lian, Weber Stefan, Burkard Thilo, Maseli Anna, Brasier Noe, Kühne Michael, Conen David, Huebner Thomas, Seeck Andrea, Eckstein Jens. Smart detection of atrial fibrillation†. Europace. 2017 May 01;19 (5):753–757. doi: 10.1093/europace/euw125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Koenig Nicole, Seeck Andrea, Eckstein Jens, Mainka Andreas, Huebner Thomas, Voss Andreas, Weber Stefan. Validation of a New Heart Rate Measurement Algorithm for Fingertip Recording of Video Signals with Smartphones. Telemed J E Health. 2016 Aug;22 (8):631–6. doi: 10.1089/tmj.2015.0212. [DOI] [PubMed] [Google Scholar]
- 38.Chon Ki H, McManus David D. Detection of atrial fibrillation using a smartwatch. Nat Rev Cardiol. 2018 Nov;15 (11):657–658. doi: 10.1038/s41569-018-0057-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bumgarner Joseph M, Lambert Cameron T, Hussein Ayman A, Cantillon Daniel J, Baranowski Bryan, Wolski Kathy, Lindsay Bruce D, Wazni Oussama M, Tarakji Khaldoun G. Smartwatch Algorithm for Automated Detection of Atrial Fibrillation. J Am Coll Cardiol. 2018 May 29;71 (21):2381–2388. doi: 10.1016/j.jacc.2018.03.003. [DOI] [PubMed] [Google Scholar]
- 40.Dash S, Chon K H, Lu S, Raeder E A. Automatic real time detection of atrial fibrillation. Ann Biomed Eng. 2009 Sep;37 (9):1701–9. doi: 10.1007/s10439-009-9740-z. [DOI] [PubMed] [Google Scholar]
- 41.Halcox Julian P J, Wareham Kathie, Cardew Antonia, Gilmore Mark, Barry James P, Phillips Ceri, Gravenor Michael B. Assessment of Remote Heart Rhythm Sampling Using the AliveCor Heart Monitor to Screen for Atrial Fibrillation: The REHEARSE-AF Study. Circulation. 2017 Nov 07;136 (19):1784–1794. doi: 10.1161/CIRCULATIONAHA.117.030583. [DOI] [PubMed] [Google Scholar]
- 42.Soni Apurv, Karna Sunil, Patel Harshil, Fahey Nisha, Raithatha Shyamsundar, Handorf Anna, Bostrom John, Bashar Syed, Talati Kandarp, Shah Ravi, Goldberg Robert J, Thanvi Sunil, Phatak Ajay Gajanan, Allison Jeroan J, Chon Ki, Nimbalkar Somashekhar Marutirao, McManus David D. Study protocol for Smartphone Monitoring for Atrial fibrillation in Real-Time in India (SMART-India): a community-based screening and referral programme. BMJ Open. 2017 Dec 14;7 (12) doi: 10.1136/bmjopen-2017-017668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stark Konstantin, Czermak Thomas, Massberg Steffen, Orban Martin. Watch out for ST-elevation myocardial infarction: a case report of ST-elevation in single-lead electrocardiogram tracing of a smartwatch. Eur Heart J Case Rep. 2020 Dec;4 (6):1–4. doi: 10.1093/ehjcr/ytaa353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bonomi Alberto G, Schipper Fons, Eerikäinen Linda M, Margarito Jenny, van Dinther Ralph, Muesch Guido, de Morree Helma M, Aarts Ronald M, Babaeizadeh Saeed, McManus David D, Dekker Lukas R C. Atrial Fibrillation Detection Using a Novel Cardiac Ambulatory Monitor Based on Photo-Plethysmography at the Wrist. J Am Heart Assoc. 2018 Aug 07;7 (15) doi: 10.1161/JAHA.118.009351. [DOI] [PMC free article] [PubMed] [Google Scholar]