Abstract
We present the first ever reported case of a super morbidly obese patient (BMI > 60) with drug refractory, symptomatic persistent atrial fibrillation who underwent an uncomplicated, but unsuccessful PVI ablation procedure and subsequently underwent AV node ablation and cardiac resynchronization therapy – pacemaker (CRT-P) insertion using a zero fluoroscopy technique. This case demonstrates the following two critical points: (1) difficulties in the treatment of massively obese patients with arrhythmias1; (2) increased use of fluoroless procedures2-4.
Keywords: Atrial Fibrillation Ablation, Obesity, Fluoroless procedures
INTRODUCTION
It has been observed that obesity has become a global pandemic and more so in United States. In the US, 48% of all Americans are obese (body mass index of > 30 kg/m2) and 12% are super obese 5. Super obese or Class III patients are defined as having a BMI of Greater than 40 kg/m26. We describe a SANS FLUORO (zero fluoroscopy) ablation of a super morbidly obese patient with longstanding, persistent AF that was unsuccessful, followed by fluoroless successful AV node ablation and CRT-P implantation.
CASE REPORT
49 year old super morbidly obese gentleman (BMI 60.3 kg/m2, 213.2 kg or 469 lbs) with longstanding persistent atrial fibrillation, hospitalized multiple times with AF with uncontrolled rates and HFpEF (Heart Failure with preserved Ejection Fraction of 40%) who had had multiple unsuccessful cardioversions despite being placed on amiodarone. Other medical problems included: hypertension, obstructive sleep apnea, and history of non-compliance. The patient described severe dyspnea on exertion with debilitation to the point that he was mostly bed bound using a urinal and bedside commode. His left atrium was moderately dilated at 4.6 cm2.
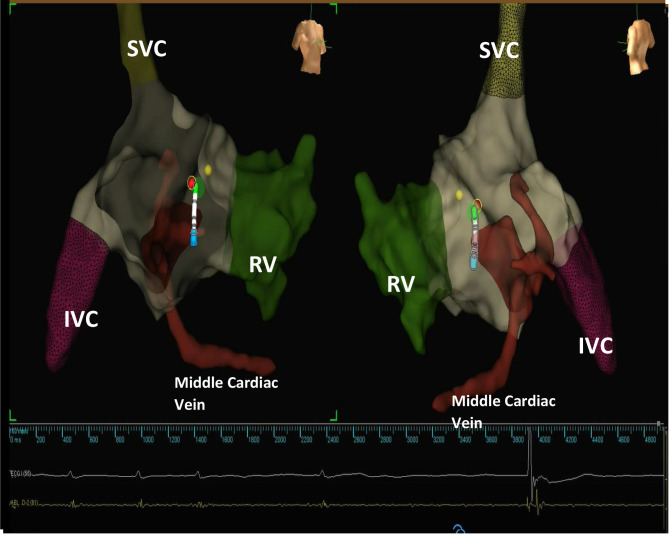
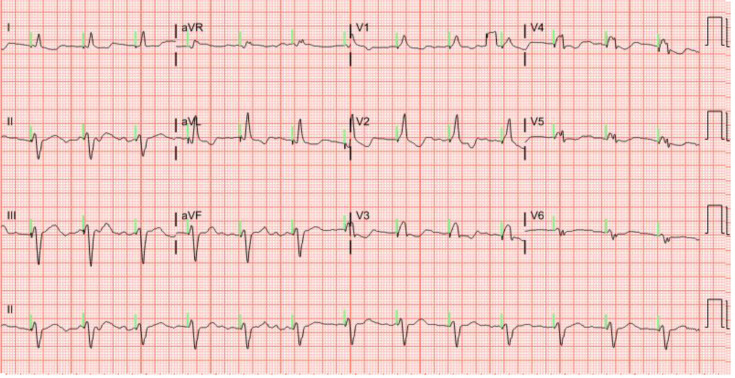
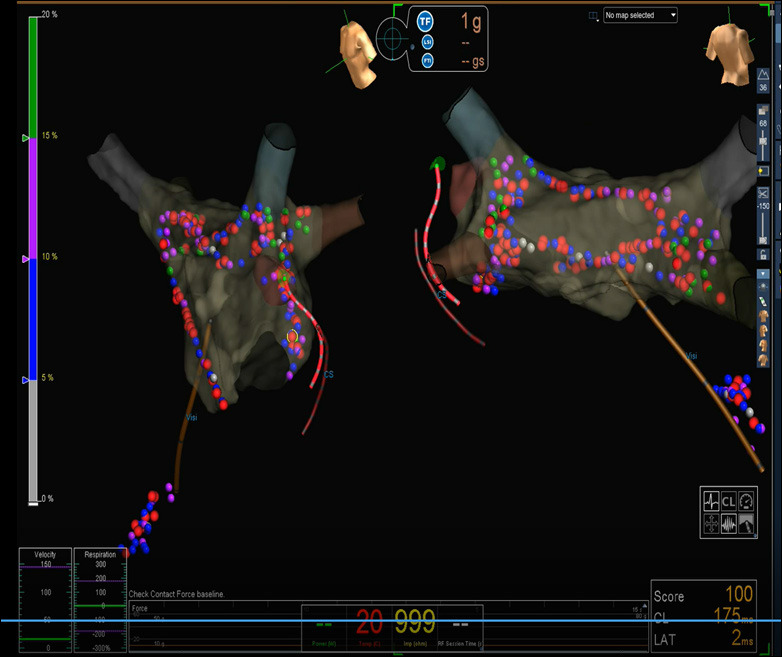
On his 4th admission with exacerbation of HFpEF as well as AF with uncontrolled rates [Figure 1], heart catheterization revealed only non-obstructive coronary artery disease. Due to his relatively young age, we initially attempted a rhythm control strategy with Pulmonary Vein Isolation (PVI). PVI was performed in his bariatric bed as the table would not support his weight. Additionally, portable C arm was not used as it would not fit beneath the bed and images would be sub-standard. The bed was placed in the EP lab, and the Abbott Precision system was used. The patient was intubated for airway protection. Three sheaths were placed in the right groin without complication. A 3-D electro-anatomic impedance-based map of the RA was generated using a coronary sinus catheter whereas the RA was mapped with the HD Grid multi-spline catheter. The LA map was compared to a previous chest CTA to ensure that all veins were accounted for. An intracardiac echocardiography (ICE) catheter was extensively utilized to visualize RA, SVC, transseptal puncture, left atrial ablation and pericardial space to ensure safety. We also used an irrigated force sensing ablation catheter to improve safety and efficacy (45 W anteriorly and 40 W posteriorly). Despite pulmonary vein isolation, posterior wall isolation, mitral and cavo-tricuspid isthmus ablation, and complex fractionated atrial electrogram ablations (CAFÉ) [Figure 2]; restoration of sinus rhythm even with cardioversion x2 with 720 J (simultaneous use of 2 external cardiac defibrillators in biphasic mode) was unsuccessful.
Figure 1. ECG revealing Atrial Fibrillation with rates in the 120s and diffuse non-specific ECG changes.
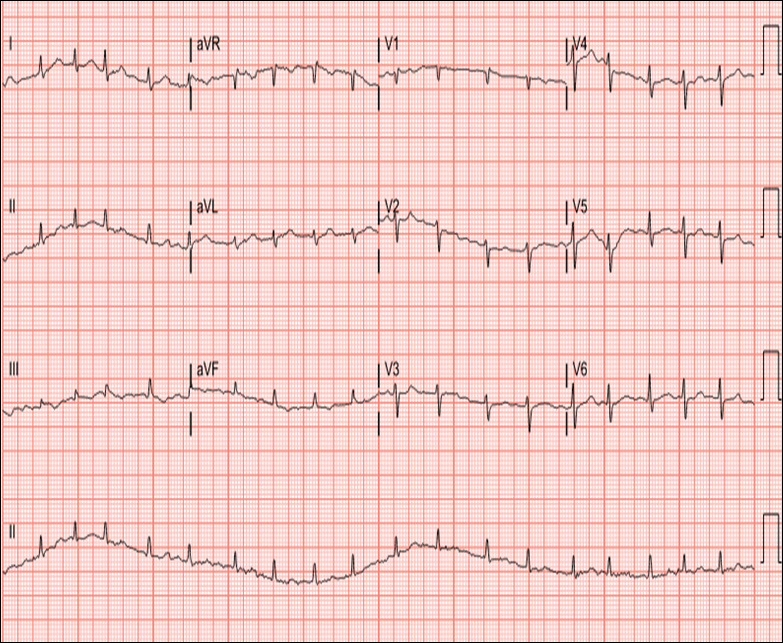
Figure 2. AP and PA view of Electro Anatomic Map of ablation lesions with CS catheter and Vizigo sheath. Impedance scale is shown on the left. Red lesions denote that Lesion Severity Index of > 4.5.
His symptoms improved and his AF rates were controlled in the 80s on amiodarone 400 mg twice daily. Due to neurologic side effects, amiodarone was discontinued which led to re-hospitalization with AF rates to the 140s only 2 weeks later. At this point, it was decided that AV node ablation and pacemaker would be the last resort treatment.
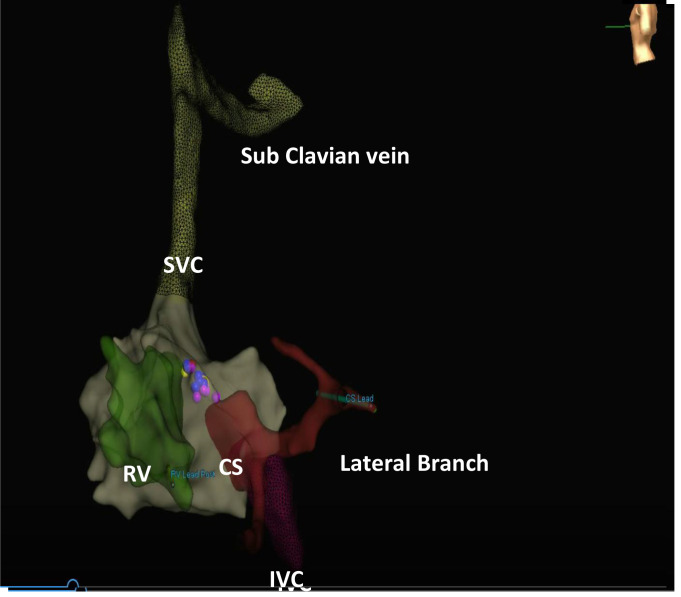
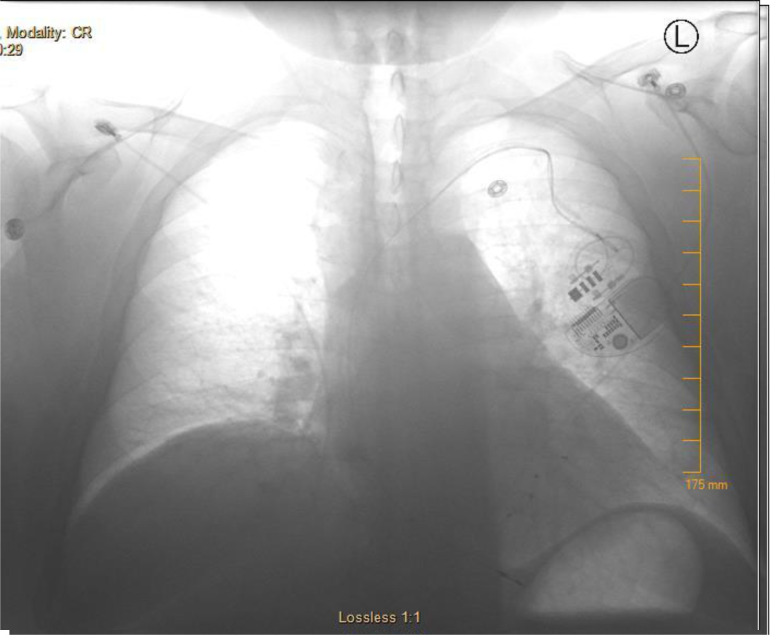
The patient underwent a completely fluoroless CRT-P insertion under general anesthesia as well as AV node ablation utilizing a single left subclavian access [Figure 3]. 3 D electroanatomic mapping with the Abbott Precision system was utilized to generate a detailed map of the right atrium, right ventricle, and coronary sinus with branches. The RV lead was visualized using alligator clips that connected to the mapping system. Injury current was also used to confirm satisfactory placement of active fixation screw in the low septum. The CS sheath was advanced over the ablation catheter deep in the vein. The Biotronik Vision wire with in the CS lead both of which are visible on the 3D map utilizing double alligator clips to guide the lead successfully into a previously mapped lateral CS branch. There were no complications with access or lead placement [Figure 4]. RV threshold was 0.5 V @ 0.5 msec and LV threshold was 2.5 V @ 0.5 msec [Figure 5]. The following day he was able to ambulate around the unit for the first time and at his 2 week follow up, he had lost 11.4 kg (25 lbs) [Figure 6]. After 7 months, the EF has recovered to 60% and he has not required hospitalization.
Figure 3. Fluoroless Ablation of AV node with resulting paced rhythm. Left view is RAO with cutaway revealing the os of the coronary sinus as well. Yellow dot denotes the His position and Red dot denotes ablation lesion.
Figure 4. Left lateral projection of RV lead, CS lead and ablation lesions. SVC, IVC and middle cardiac vein is also well visualized.
Figure 5. Post CRT-P chest radiograph that is under exposed to reveal lead positions.
Figure 6. Post CRT-P ECG revealing a completely paced rhythm at 80 bpm.
Discussion
This case is important because it outlines 2 distinct issues: management of atrial arrhythmias in super morbid obese patients and the concept of fluoroless procedures. It is well known that obese patients with or without sleep apnea suffer from an increased rate of atrial arrhythmias and HFpEF 5-8. Initially, consideration was given to portable C arm use, but this would have delivered uninterpretable images and prohibitive amounts of X-ray radiation exposure to the patient and the staff (at least 2-4 times normal amounts) due to body habitus9. Additionally, a single stick approach decreased the risk of complications and overall case time length10.
Improvements in 3 dimensional mapping systems have demonstrated capabilities of providing the necessary visual information needed to perform various ablations, especially atrial flutter and atrial fibrillation11. As obesity rates are continuing to rise, these patients will become commonplace in everyday practice. Finally, recent studies have shown that obesity may have a deleterious effect on long term ablation success rates12. This is a particular case that would have been either unsuccessful or extremely technically challenging if reliance on traditional fluoroscopic techniques had been utilized. As a matter of caution, higher level of intracardiac echocardiography skills, very detailed 3 D mapping and low threshold to use fluoroscopy if absolutely needed for safety is important in fluoroless procedures. This case illustrates safety and feasibility of fluoroless procedures in all patients but especially super morbidly patients.
References
- 1.Percell Robert Lee, Sharpe Erin, Allison Timothy, Burt Shirley Mohr, Olmsted Rhonda, Travers Chad. SANS FLUORO Supersized: A case report of Fluoroless Ablation in a Super Morbidly Obese Patient. J Atr Fibrillation. 2018 Dec;11 (4) doi: 10.4022/jafib.2112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chan Kim H, Santucci Peter A. Routine Implant of Biventricular Devices Guided by an Electroanatomic Mapping System - Ready for Prime-Time? J Atr Fibrillation. 2015 Dec;8 (4) doi: 10.4022/jafib.1265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang Henry D, Sharma Parikshit S, Nayak Hemal M, Serafini Nicholas, Trohman Richard G. How to perform electroanatomic mapping-guided cardiac resynchronization therapy using Carto 3 and ESI NavX three-dimensional mapping systems. Europace. 2019 Nov 01;21 (11):1742–1749. doi: 10.1093/europace/euz229. [DOI] [PubMed] [Google Scholar]
- 4.Percell Robert L, Pike Jonathan L, Olmsted Rhonda K, Beideck Jenna E, Nunes Haley L, Johnson Kellie N, Schaffer Matthew, Vachok Lindy B, Sveen Stacy M, Keim Emily J, Mohr-Burt Shirley O, Saalfeld Rose M, Beran Casey A, Allison Timothy W, Stock John F. The Grand SANS FLUORO (SAy No Series to FLUOROsopy) Study: Examining Fluoroscopy Use in More than 1,000 Ablation Procedures. J Innov Card Rhythm Manag. 2020 Sep;11 (9):4224–4232. doi: 10.19102/icrm.2020.1100903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Imes Christopher C, Burke Lora E. The Obesity Epidemic: The United States as a Cautionary Tale for the Rest of the World. Curr Epidemiol Rep. 2014 Jun 01;1 (2):82–88. doi: 10.1007/s40471-014-0012-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pandey Ambarish, Patel Kershaw V, Vaduganathan Muthiah, Sarma Satyam, Haykowsky Mark J, Berry Jarett D, Lavie Carl J. Physical Activity, Fitness, and Obesity in Heart Failure With Preserved Ejection Fraction. JACC Heart Fail. 2018 Dec;6 (12):975–982. doi: 10.1016/j.jchf.2018.09.006. [DOI] [PubMed] [Google Scholar]
- 7.Friedrich M J. Global Obesity Epidemic Worsening. JAMA. 2017 Aug 15;318 (7) doi: 10.1001/jama.2017.10693. [DOI] [PubMed] [Google Scholar]
- 8.Gami Apoor S, Hodge Dave O, Herges Regina M, Olson Eric J, Nykodym Jiri, Kara Tomas, Somers Virend K. Obstructive sleep apnea, obesity, and the risk of incident atrial fibrillation. J Am Coll Cardiol. 2007 Feb 06;49 (5):565–71. doi: 10.1016/j.jacc.2006.08.060. [DOI] [PubMed] [Google Scholar]
- 9.Ector Joris, Dragusin Octavian, Adriaenssens Bert, Huybrechts Wim, Willems Rik, Ector Hugo, Heidbüchel Hein. Obesity is a major determinant of radiation dose in patients undergoing pulmonary vein isolation for atrial fibrillation. J Am Coll Cardiol. 2007 Jul 17;50 (3):234–42. doi: 10.1016/j.jacc.2007.03.040. [DOI] [PubMed] [Google Scholar]
- 10.Arenja Nisha, Knecht Sven, Schaer Beat, Reichlin Tobias, Pavlovic Nikola, Osswald Stefan, Sticherling Christian, Kühne Michael. Comparison of different approaches to atrioventricular junction ablation and pacemaker implantation in patients with atrial fibrillation. Pacing Clin Electrophysiol. 2014 Dec;37 (12):1686–93. doi: 10.1111/pace.12481. [DOI] [PubMed] [Google Scholar]
- 11.Laţcu Decebal Gabriel, Saoudi Nadir. High-resolution/Density Mapping in Patients with Atrial and Ventricular Arrhythmias. Card Electrophysiol Clin. 2019 Sep;11 (3):511–524. doi: 10.1016/j.ccep.2019.05.001. [DOI] [PubMed] [Google Scholar]
- 12.De Maat Gijs E, Mulder Bart A, Berretty Wouter L, Al-Jazairi Meelad I H, Tan Eng-Shiong, Wiesfeld Ans C P, Mariani Massimo A, Van Gelder Isabelle C, Rienstra Michiel, Blaauw Yuri. Obesity is associated with impaired long-term success of pulmonary vein isolation: a plea for risk factor management before ablation. Open Heart. 2018 Jun 5;5 (1) doi: 10.1136/openhrt-2017-000771. [DOI] [PMC free article] [PubMed] [Google Scholar]