Supplemental Digital Content is available in the text.
Keywords: bystander cardiopulmonary resuscitation, epidemiology, out-of-hospital cardiac arrest, shockable rhythm, survival
Abstract
Background and importance
Bystander cardiopulmonary resuscitation (CPR) and initial shockable rhythm are crucial predictors of survival after out-of-hospital cardiac arrest (OHCA). However, the relationship between dispatcher-assisted CPR (DA-CPR) and initial shockable rhythm is not completely elucidated.
Objective
To examine the association of DA-CPR with initial shockable rhythm and outcomes.
Design, setting and participants
This nationwide population-based observational study conducted in Japan included 59 688 patients with witnessed OHCA of cardiac origin after excluding those without bystander CPR. Patients were divided into DA-CPR (n = 42 709) and CPR without dispatcher assistance (unassisted CPR, n = 16 979) groups.
Outcome measures and analysis
The primary outcome measure was initial shockable rhythm, and secondary outcome measures were 1-month survival and neurologically intact survival. A Cox proportional hazards model adjusted for collapse-to-first-rhythm-analysis time and multivariable logistic regression models were used after propensity score (PS) matching to compare the incidence of initial shockable rhythm and outcomes, respectively.
Main results
Among all patients (mean age 76.7 years), the rates of initial shockable rhythm, 1-month survival and neurologically intact survival were 20.8, 10.7 and 7.0%, respectively. The incidence of initial shockable rhythm in the DA-CPR group (20.4%, 3462/16 979) was significantly higher than that in the unassisted CPR group (18.5%, 3133/16 979) after PS matching (P < 0.0001). However, no significant differences were found between the two groups with respect to the incidence of initial shockable rhythm in the Cox proportional hazards model [adjusted hazard ratio of DA-CPR for initial shockable rhythm compared with unassisted CPR, 0.99; 95% confidence interval (CI), 0.97–1.02, P = 0.56]. No significant differences were observed in the survival rates in the two groups after PS matching [10.8% (1833/16 979) vs. 10.3% (1752/16 979), P = 0.16] and neurologically intact survival rates [7.3% (1233/16 979) vs. 6.8% (1161/16 979), P = 0.13]. The multivariable logistic regression model showed no significant differences between the groups with regard to survival (adjusted odds ratio of DA-CPR compared with unassisted CPR: 1.00; 95% CI, 0.89–1.13, P = 0.97) and neurologically intact survival (adjusted odds ratio: 1.12; 95% CI, 0.98–1.29, P = 0.14).
Conclusion
DA-CPR after OHCA had the same independent association with the likelihood of initial shockable rhythm and 1-month meaningful outcome as unassisted CPR.
Introduction
The presence of witnesses, bystander cardiopulmonary resuscitation (CPR), an initial shockable rhythm, early defibrillation, short CPR duration, short emergency medical service (EMS) response time, and location of the patient at the time of cardiac arrest are crucial prehospital factors associated with neurologically intact survival in patients who experience out-of-hospital cardiac arrest (OHCA) [1,2]. Of these, early CPR is a critical element in the chain of survival [3]. In fact, early CPR performed prior to EMS arrival was associated with a 30-day survival rate more than twice as high as that associated with no CPR before EMS arrival [4]. Moreover, a study from Denmark [5] supports the idea that early intervention (CPR and defibrillation) by bystanders may improve long-term functional outcomes and highlights the necessity to implement and improve strategies that facilitate the initiation of CPR by bystanders and increase public-access defibrillation. The dispatchers’ CPR instructions are crucial for increasing the rate of CPR provision and improving the quality of CPR provided after OHCA [6,7]. However, data comparing the association of the likelihood of an initial shockable rhythm on EMS arrival with dispatcher-assisted CPR (DA-CPR) before arrival of EMS personnel with that with bystander CPR without dispatcher assistance (unassisted CPR) are insufficient. Moreover, no significant differences were found in neurologically intact survival at hospital discharge or at 1 month after OHCA between CPR with and without dispatcher assistance [8–10], while conflicting results were seen in the other studies [11,12]. In this context, it was hypothesised that the likelihood of an initial shockable rhythm after DA-CPR and survival rate are similar to those after unassisted CPR.
To investigate these hypotheses, the incidence of initial shockable rhythm and rates of survival and neurologically intact survival were examined according to the type of bystander CPR prior to EMS arrival.
Methods
Study design and setting
This nationwide, population-based observational study was conducted in Japan between January 2013 and December 2017 and included 59 688 adult patients at least 18 years of age who suffered OHCA of presumed cardiac origin witnessed by laypersons and for whom resuscitation was attempted. The study was approved by the institutional review board of Kanazawa University (No. 1263). The requirement for written informed consent was waived because the study used anonymised data.
The Fire and Disaster Management Agency (FDMA) of Japan supervises the nationwide EMS system [13]. During the study period, all EMS personnel performed CPR following the Japanese CPR guidelines and attempted resuscitation by using automated external defibrillators (AEDs), inserting airway adjuncts and peripheral intravenous catheters, and administering Ringer’s lactate solution [13–15]. Only specially trained emergency life-saving technicians are permitted to insert tracheal tubes and administer intravenous epinephrine after receiving online instructions from a physician [13]. EMS personnel in Japan are legally prohibited from terminating resuscitation on the field.
The FDMA has provided a standard outline for dispatcher CPR instructions and has recommended that local fire departments modify the content of telephonic dispatcher assistance according to the actual circumstances in the local area [16,17]. DA-CPR is offered when dispatchers determine that they must advise a bystander to aid the resuscitation of a patient experiencing OHCA. Generally, the dispatcher offers CPR instructions for chest compression plus rescue breathing (conventional) or chest compression-only CPR, depending on the skill or knowledge of the bystander. DA-CPR is not offered in cases in which cardiac arrest is uncertain during the call.
Data collection and quality control
In 2005, the FDMA launched an ongoing prospective population-based observational study that includes all patients with OHCA in Japan who receive resuscitation by EMS personnel [3]. EMS personnel and the physician in charge of each centre record data from the patients using a Utstein-style recommended guideline template [18].
The characteristics included in the dataset were as follows: patient sex and age; aetiology of cardiac arrest; initial cardiac rhythm; presence of bystander witnesses; bystander CPR manoeuvre; time of collapse, receipt of emergency calls, vehicle arrival at the scene and EMS initiation of CPR; 1-month survival; and neurologically intact survival. Neurological outcomes were defined using the Cerebral Performance Category (CPC) scale scores [18], which were determined by the physician in charge.
Study endpoints
The primary study endpoint was an initial shockable rhythm recorded by EMS personnel using AED pads soon after EMS-initiated CPR. Secondary endpoints were 1-month survival, and 1-month neurologically intact survival (defined as a CPC scale of 1 or 2, CPC 1–2).
Statistical analysis
Continuous variables were expressed as means and standard deviations. Categorical variables were expressed as numbers and percentages. Effect size and variability were reported as odds ratios or hazard ratios (HRs) with 95% confidence intervals. To determine the association of bystander CPR with the likelihood of an initial shockable rhythm and outcomes, patients were classified into DA-CPR and unassisted CPR groups. Propensity score (PS) matching analyses between the two groups were performed using a logistic regression model that included six variables (age, sex, calendar year, rural or urban area, call-to-EMS response time, and witness status). One-to-one nearest neighbour matching without replacement was performed between the groups using a calliper width of 0.20 times of the SD of the logit of the PS. The success of the PS matching procedure was determined by comparing the distributions of the patient characteristics in the matched sample by calculating an absolute standardised difference. An absolute standardised difference of at least 0.1 indicated a significant difference between the groups. A Cox proportional hazards model was applied by adjusting the collapse-to-first-rhythm-analysis time before and after PS matching. As the registry data did not include precise first-rhythm-analysis times, we used the collapse-to-EMS-initiated CPR time as a substitute for collapse-to-first-rhythm-analysis time for analyses. This may cause an underestimation of collapse-to-first-rhythm-analysis time because, according to Japanese CPR guidelines, rhythm analysis is performed by EMS personnel after initiation of CPR using AED pads [14,15]. The six potential prehospital confounders (age, sex, calendar year, rural or urban area, witnessed status and CPR types) in the Cox proportional hazards model were selected based on biological plausibility and data reported in previous studies. To evaluate the association between CPR type and rates of survival and CPC 1–2, multivariable logistic regression analyses were performed before and after PS matching using six prehospital variables (age, sex, calendar year, EMS-response time, initial shockable rhythm and CPR type). All data were analysed using the JMP statistical package software, version 15-Pro (SAS Institute Inc., Cary, North Carolina, USA). All the reported tests were two-tailed, and P < 0.05 was considered statistically significant.
Results
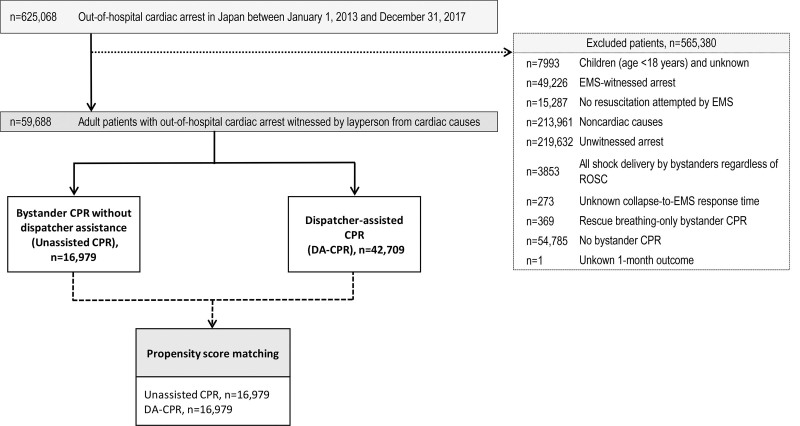
Between 2013 and 2017, the details of attempted resuscitation for 625 068 patients with OHCA in Japan were documented in the FDMA database. Figure 1 shows the inclusion and exclusion criteria for the present study. A group of 59 688 patients (9.5% of those in the registry) met the following inclusion criteria and were included in this study: adult patients who suffered OHCA with presumed cardiac aetiology, witnessed by laypersons, and bystander CPR. Patients were divided into DA-CPR (n = 42,709) and unassisted CPR (n = 16,979) groups.
Fig. 1.
Study inclusion flowchart. CPR, cardiopulmonary resuscitation; DA, bystander-assisted; EMS, emergency medical services; ROSC, return of spontaneous circulation.
The baseline characteristics of the participants before and after PS matching are shown in Table 1. PS matching considerably improved the absolute standardised differences in each group. Collapse-to-first-CPR time in the unassisted CPR group was significantly shorter than that in the DA-CPR group by 0.9 minutes (after PS matching, mean, 2.3 minutes vs. 3.2 minutes, P < 0.0001).
Table 1.
Baseline characteristics of unassisted cardiopulmonary resuscitation and dispatcher-assisted cardiopulmonary resuscitation groups before/after propensity score matching
| Characteristic | Prepropensity score matching | Postpropensity score matching | ||||
|---|---|---|---|---|---|---|
| Unassisted CPR | DA-CPR | ASDa | Unassisted CPR | DA-CPR | ASDa | |
| (n = 16 979) | (n = 42 709) | (n = 16 979) | (n = 16 979) | |||
| Year | ||||||
| 2013 | 3490 (20.6) | 7799 (18.3) | 0.06 | 3490 (20.6) | 3492 (20.6) | <0.01 |
| 2014 | 3587 (21.1) | 8220 (19.2) | 0.05 | 3587 (21.1) | 3608 (21.3) | <0.01 |
| 2015 | 3322 (19.6) | 8439 (19.8) | <0.01 | 3322 (19.6) | 3371 (19.9) | 0.01 |
| 2016 | 3295 (19.4) | 8909 (20.9) | 0.04 | 3295 (19.4) | 3277 (19.3) | <0.01 |
| 2017 | 3285 (19.4) | 9342 (21.9) | 0.06 | 3285 (19.4) | 3231 (19.0) | 0.01 |
| Sex – man | 9264 (54.6) | 24 996 (58.5) | 0.08 | 9264 (54.6) | 9303 (54.8) | <0.01 |
| Age (years), mean (SD) | 77.4 (14.9) | 76.7 (14.8) | 0.04 | 77.4 (14.9) | 77.5 (14.9) | 0.04 |
| Initial cardiac rhythm | ||||||
| Shockable | 3133 (18.5) | 9254 (21.7) | 0.08 | 3133 (18.5) | 3462 (20.4) | 0.08 |
| Geographic Japanese regions | ||||||
| Rural areab | 4216 (24.8) | 10 428 (24.4) | 0.01 | 4216 (24.8) | 4224 (24.9) | <0.01 |
| Bystander witness status | ||||||
| Witnessed by family member | 5500 (32.4) | 27 030 (63.3) | 0.65 | 5500 (32.4) | 5500 (32.4) | <0.01 |
| Witnessed by nonfamily member | 11 479 (67.6) | 15 679 (36.7) | 0.65 | 11 479 (67.6) | 11 479 (67.6) | <0.01 |
| Collapse-to-call time (minutes), mean (SD) | 2.1 (7.7) | 3.4 (6.8) | 0.18 | 2.3 (7.6) | 2.5 (6.6) | 0.03 |
| Call-to-EMS response time (minutes), mean (SD) | 9.5 (4.1) | 9.5 (3.9) | 0.01 | 9.4 (4.1) | 9.5 (4.2) | 0.04 |
| Collapse-to-first-CPR time (minutes), mean (SD) | 2.2 (4.6) | 4.2 (6.0) | 0.37 | 2.3 (4.6) | 3.2 (5.3) | 0.19 |
| Collapse-to-first-rhythm-analysis time (minutes), mean (SD) | 11.7 (7.9) | 13.1 (7.3) | 0.17 | 11.9 (7.9) | 12.2 (7.0) | 0.04 |
| Bystander CPR durationc (minutes), mean (SD) | 9.6 (7.7) | 9.0 (6.1) | 0.09 | 9.7 (7.7) | 9.1 (6.5) | 0.08 |
Values are reported as n (%) unless indicated otherwise.
ASD, absolute standardised difference; CPR, cardiopulmonary resuscitation; DA, dispatcher-assisted; EMS, emergency medical services.
An ASD of equal or more than 0.1 was considered to indicate a substantial imbalance between the two groups.
The rural area is constituted 19 prefectures with population of less than 200 inhabitants per km2.
Values were missing for 52 patients (0.09 %) before propensity score matching and for 44 patients (0.13%) after propensity score matching.
The incidence of initial shockable rhythm without adjusting the collapse-to-first-rhythm-analysis time and 1-month outcomes in the unmatched patients are shown in the Supplementary Figure 1 (Supplemental digital content 1, http://links.lww.com/EJEM/A315). The incidences of initial shockable rhythm and survival in the DA-CPR group were significantly higher than those in the unassisted CPR group (shockable rhythm, P < 0.0001; survival, P < 0.05). There was no significant difference between the two groups in the incidence of CPC 1–2 (P = 0.36). In the multivariable logistic regression model, although DA-CPR was associated with decreased odds of 1-month CPC 1–2 (P < 0.05) compared with unassisted CPR, there was no significant difference in 1-month survival between two groups (P = 0.15; Supplementary Figure 2, Supplemental digital content 1, http://links.lww.com/EJEM/A315).
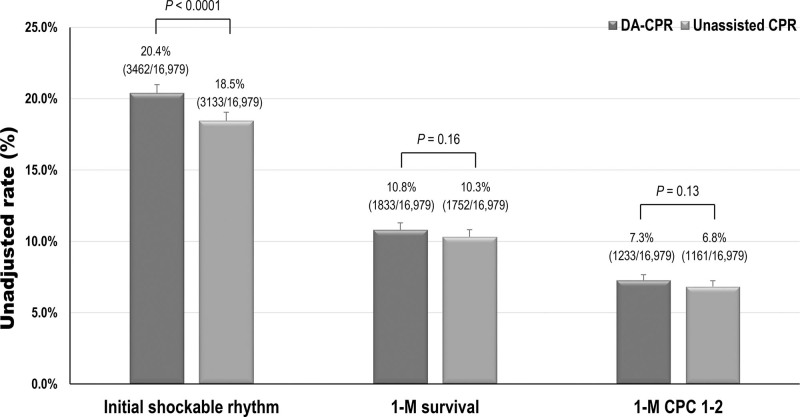
The incidence of initial shockable rhythm without adjusting the collapse-to-first-rhythm-analysis time and 1-month unadjusted outcomes in the matched patients are shown in Fig. 2. The incidence of initial shockable rhythm was significantly higher in the DA-CPR group than in the unassisted CPR group (P < 0.0001). However, there were no significant differences between the two groups in 1-month survival (P = 0.16) and the incidence of 1-month CPC 1–2 (P = 0.13).
Fig. 2.
The incidence of initial shockable rhythm and unadjusted outcomes in the 33 958 matched patients. CPC, cerebral performance category; CPR, cardiopulmonary resuscitation; DA, dispatcher-assisted.
HRs of the DA-CPR for initial shockable rhythm after adjusting for collapse-to-first-rhythm-analysis time are shown in Table 2. There were no significant differences between the DA-CPR and unassisted CPR groups in the association with the likelihood of an initial shockable rhythm, regardless of PS matching (P = 0.52 for pre-PS matching, P = 0.56 for post-PS matching).
Table 2.
Hazard ratios of cardiopulmonary resuscitation group for initial shockable rhythm before/after propensity score matching
| CPR group | Reference | Adjusted hazard ratio | 95% CI | P value |
|---|---|---|---|---|
| DA-CPR | Unassisted CPR | |||
| Before PS matching | 1.00 | 0.99–1.03 | 0.52 | |
| After PS matching | 0.99 | 0.97–1.02 | 0.56 |
CI, confidence interval; CPR, cardiopulmonary resuscitation; DA, dispatcher-assisted; PS, propensity score.
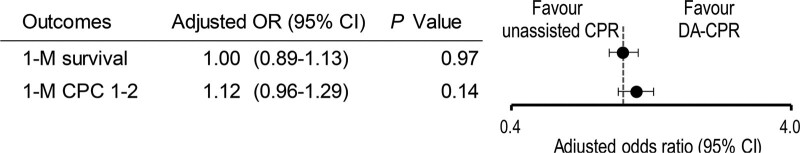
Figure 3 showed the adjusted odds ratios of DA-CPR for 1-month outcomes compared with unassisted CPR by using the multivariable logistic regression. DA-CPR was not associated with increased odds of 1-month survival (P = 0.97) or the incidence of CPC 1–2 (P = 0.14).
Fig. 3.
Adjusted odds ratios of DA-CPR for 1-month outcomes compared with unassisted CPR in the matched patients. CI, confidence interval; CPC, cerebral performance category; CPR, cardiopulmonary resuscitation; DA, dispatcher-assisted; OR, odds ratio.
Discussion
In this nationwide, population-based observational study, no differences were found between DA-CPR and unassisted CPR in the likelihood of an initial shockable rhythm after adjusting for collapse-to-first-rhythm-analysis time. This may be the first large-scale cohort study to clearly show that the likelihood of an initial shockable rhythm after DA-CPR is the same as that after unassisted bystander CPR.
As an initial shockable rhythm is the most important predictor favouring survival in patients with OHCA, it is crucial to identify factors associated with a shockable rhythm as the first recorded cardiac rhythm [19]. Previous studies have shown that male sex, bystander-witnessed cardiac arrest, bystander CPR, cardiac arrest in a public location, cardiovascular disease, and medication prescription are associated with a shockable rhythm while advanced age, cardiac arrest in a private home, and longer EMS response time are associated with an unshockable rhythm [20–23]. Of the positive predictors of shockable rhythm, bystander CPR was the strongest predictor with an adjusted odds ratio of 2.17 compared with no bystander CPR among bystander-witnessed patients with a time to first rhythm analysis <10 minutes in a multivariable logistic regression model [20]. However, one study showed no association between bystander CPR and initial shockable rhythm [23]. As shockable rhythm dissolves into asystole over time [19], these conflicting results may be attributed to whether the analytic model included the time elapsed from collapse. In the present study, a Cox proportional hazard model was applied to determine the association between bystander CPR and initial shockable rhythm after adjusting for call-to-first-rhythm-analysis time. However, previous studies [20,22] used a multivariable logistic regression model without adjusting the time elapsed between collapse and rhythm analysis. The Cox proportional hazard model adjusted for elapsed time may be more suitable for analysing the likelihood of an initial shockable rhythm than the multivariable logistic regression model. A previous study from Korea showed that the incidence rate of defibrillation, as a surrogate index of shockable rhythm, in the DA-CPR group was the same as that in the CPR without dispatcher assistance, using a Cox regression model [8]. The present study may be the first to show the associations between DA-CPR and unassisted CPR and an initial shockable rhythm using the Cox proportional hazard model.
In the present study, there were no significant differences in 1-month outcomes after OHCA between the DA-CPR and unassisted CPR groups. These results are consistent with those of several previous studies [8–10]. However, other previous studies showed the benefits of unassisted CPR over DA-CPR owing to the shorter time from collapse to initiation of bystander CPR and the higher quality of CPR [11,12], which are inconsistent with present results. Several plausible reasons could explain the present findings. Both the interval from collapse to bystander CPR and the quality of bystander CPR may be associated with an initial shockable rhythm and outcomes. Regarding the time of initiation of bystander CPR, Rea et al. found that the DA-CPR group had a longer time to initiate bystander CPR compared with the bystander CPR without dispatcher assistance group (mean, 2.9 minutes vs. 2 minutes) [24]. Similarly, in the present study, the collapse-to-first-CPR time in the DA-CPR group was significantly longer than that in the unassisted group (post-PS matching, mean, 3.2 minutes vs. 2.3 minutes). This time difference of <1 minute in the initiation of bystander CPR between the two bystander CPR groups did not influence the initial shockable rhythm rate and outcomes in the present study.
Regarding the quality of bystander CPR, the unassisted CPR group presumably included trained individuals who were more confident in performing high-quality CPR than those in the DA-CPR group [25]. Meanwhile, Teo et al. [26] showed that a higher proportion of bystanders in the DA-CPR cohort achieved the correct compression rate and had correct hand placement compared with those without dispatcher assistance. Moreover, previous study showed that dispatcher-assisted compression-only CPR had better CPR quality than dispatcher-assisted conventional CPR [27]. In the present study, the crude incidence of an initial shockable rhythm in patients with dispatcher-assisted compression-only CPR was significantly higher than that in those with dispatcher-assisted conventional CPR with rescue breaths – 22.0% (8381/38 139) vs. 19.1% (873/4570), P < 0.001. Accordingly, although most of the bystanders in the DA-CPR groups may be untrained individuals, receiving DA-CPR with chest-compression-only CPR would contribute to bring the same association effect on initial shockable rhythm and favourable outcomes as bystander CPR without dispatcher assistance. However, further precise analyses are required to demonstrate whether dispatcher-assisted compression-only CPR is associated with increased odds of an initial shockable rhythm and favourable outcomes compared with DA-CPR with the conventional manoeuvre.
During the study period, the proportion of DA-CPR to all bystander CPR significantly increased from 69.1% (7799/11 289) to 74.0% (9342/12 627, P < 0.0001). This may be attributed to the increase in the quality of dispatchers’ ability to deliver CPR instruction following recognition of cardiac arrest due to the continuous quality improvement project in Japan [16,28]. Of patients who did not receive bystander CPR, 69.8% (38 225/54 785) of bystanders were not offered CPR instruction owing to a lack of recognition of cardiac arrest by the dispatcher. To reduce this rate, further efforts should focus on increasing the early recognition of cardiac arrest so that CPR instruction can be offered by the dispatcher to bystanders. A recent Parisian study [29] report a unique method (hand-on-belly) to detect OHCA based on details provided by a caller over the phone. This new method of recognition of cardiac arrest over the phone may help increase the early recognition of OHCA.
Unfortunately, during the study period, 27.9% (16 560/59 269) of bystanders did not perform CPR despite the dispatcher’s offer of CPR instructions, although the rate has been improving compared with those seen in previous studies in Japan (49.6% in 2005) [16]. The reasons for not performing CPR may include the increased age of bystanders, fear or panic, or unwillingness to touch the patient’s body. To minimise this rate, further efforts are required to encourage bystanders over the phone to perform CPR.
Limitations
The present study has some limitations. First, accurate collapse-to-rhythm-analysis times were not measured in this study, and they might have been underestimated because they were measured as the time from collapse to EMS-initiated CPR. Second, the number of patients with rhythm conversion from shockable to unshockable rhythms, and vice versa, before EMS arrival were unknown. These unmeasured factors may modify the present results. Third, the study analysed data collected using standard procedures from a large nationwide population; however, because of the retrospective observational design, uncontrolled confounders could not be excluded. The present study lacked data on preexisting comorbidities, the location of cardiac arrest, the quality of bystander- and EMS-initiated CPR, and in-hospital treatments. Other limitations are common to epidemiological studies, including ascertainment bias and lack of data integrity and validity. The relevance of present results to other communities with different emergency care systems [2,30] is not known. Similar studies in other countries would help validate present results.
Conclusion
DA-CPR after OHCA had the same independent association with the likelihood of an initial shockable rhythm, 1-month survival, and neurologically intact survival as bystander CPR without dispatcher assistance.
Acknowledgements
Special appreciation is extended to the FDMA for their generous cooperation in maintaining the database.
Japan Society for the Promotion of Science (grant-in-aid for scientific research (B) grant no. 20H202271, (C) grant no. 18K09999 and (C) grant no. 21K10324).
Conflicts of interest
There are no conflicts of interest.
Supplementary Material
Footnotes
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website (www.euro-emergencymed.com).
References
- 1.Goto Y, Maeda T, Nakatsu-Goto Y. Neurological outcomes in patients transported to hospital without a prehospital return of spontaneous circulation after cardiac arrest. Crit Care 2013; 17:R274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Javaudin F, Penverne Y, Montassier E. Organisation of prehospital care: the French experience. Eur J Emerg Med 2020; 27:404–405. [DOI] [PubMed] [Google Scholar]
- 3.Panchal AR, Bartos JA, Cabañas JG, Donnino MW, Drennan IR, Hirsch KG, et al. Part 3: adult basic and advanced life support: 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2020; 142:S366–S468. [DOI] [PubMed] [Google Scholar]
- 4.Hasselqvist-Ax I, Riva G, Herlitz J, Rosenqvist M, Hollenberg J, Nordberg P, et al. Early cardiopulmonary resuscitation in out-of-hospital cardiac arrest. N Engl J Med 2015; 372:2307–2315. [DOI] [PubMed] [Google Scholar]
- 5.Kragholm K, Wissenberg M, Mortensen RN, Hansen SM, Malta Hansen C, Thorsteinsson K, et al. Bystander efforts and 1-year outcomes in out-of-hospital cardiac arrest. N Engl J Med 2017; 376:1737–1747. [DOI] [PubMed] [Google Scholar]
- 6.Soar J, Maconochie I, Wyckoff MH, Olasveengen TM, Singletary EM, Greif R, et al. 2019 International consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations: summary from the basic life support; advanced life support; pediatric life support; neonatal life support; education, implementation, and teams; and first aid task forces. Circulation 2019; 140:e826–e880. [DOI] [PubMed] [Google Scholar]
- 7.Panchal AR, Berg KM, Cabañas JG, Kurz MC, Link MS, Del Rios M, et al. 2019 American Heart Association focused update on systems of care: dispatcher-assisted cardiopulmonary resuscitation and cardiac arrest centers: an update to the American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2019; 140:e895–e903. [DOI] [PubMed] [Google Scholar]
- 8.Lee SY, Hong KJ, Shin SD, Ro YS, Song KJ, Park JH, et al. The effect of dispatcher-assisted cardiopulmonary resuscitation on early defibrillation and return of spontaneous circulation with survival. Resuscitation 2019; 135:21–29. [DOI] [PubMed] [Google Scholar]
- 9.Japanese Circulation Society Resuscitation Science Study Group. Chest compression-only bystander cardiopulmonary resuscitation in the 30:2 compression-to-ventilation ratio era: nationwide observational study. Circ J 2013; 77:2742–2750. [DOI] [PubMed] [Google Scholar]
- 10.Ro YS, Shin SD, Lee YJ, Lee SC, Song KJ, Ryoo HW, et al. Effect of dispatcher-assisted cardiopulmonary resuscitation program and location of out-of-hospital cardiac arrest on survival and neurologic outcome. Ann Emerg Med 2017; 69:52–61.e1. [DOI] [PubMed] [Google Scholar]
- 11.Kim MW, Kim TH, Song KJ, Shin SD, Kim CH, Lee EJ, Kim K. Comparison between dispatcher-assisted bystander CPR and self-led bystander CPR in out-of-hospital cardiac arrest (OHCA). Resuscitation 2021; 158:64–70. [DOI] [PubMed] [Google Scholar]
- 12.Hagihara A, Onozuka D, Shibuta H, Hasegawa M, Nagata T. Dispatcher-assisted bystander cardiopulmonary resuscitation and survival in out-of-hospital cardiac arrest. Int J Cardiol 2018; 265:240–245. [DOI] [PubMed] [Google Scholar]
- 13.Ambulance Service Planning Office of Fire and Disaster Management Agency of Japan. Effect of first aid for cardiopulmonary arrest [in Japanese]. http://www.fdma.go.jp/neuter/topics/kyukyukyujo_genkyo/h29/01_kyukyu.pdf. [Accessed January 11, 2019].
- 14.Japan Resuscitation Council CPR Guidelines Committee. 2010 Japanese guidelines for emergency care and cardiopulmonary resuscitation. 2011. Tokyo: Health Shuppansha; (in Japanese). [Google Scholar]
- 15.Japan Resuscitation Council CPR Guidelines Committee. 2015 Japanese guidelines for emergency care and cardiopulmonary resuscitation (in Japanese). 2016.Igaku-Shoin; [Google Scholar]
- 16.Takahashi H, Sagisaka R, Natsume Y, Tanaka S, Takyu H, Tanaka H. Does dispatcher-assisted CPR generate the same outcomes as spontaneously delivered bystander CPR in Japan? Am J Emerg Med 2018; 36:384–391. [DOI] [PubMed] [Google Scholar]
- 17.Status of EMS and Rescue. Annual report of Fire and Disaster Management Agency (FDMA). www.fdma.go.jp/.../items/tuchi2804/pdf/280425_kyu36.pdf. [Accessed March 27, 2021].
- 18.Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L, et al.; International Liaison Committee on Resuscitation; American Heart Association; European Resuscitation Council; Australian Resuscitation Council; New Zealand Resuscitation Council; Heart and Stroke Foundation of Canada; InterAmerican Heart Foundation; Resuscitation Councils of Southern Africa; ILCOR Task Force on Cardiac Arrest and Cardiopulmonary Resuscitation Outcomes. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa). Circulation 2004; 110:3385–3397. [DOI] [PubMed] [Google Scholar]
- 19.Hulleman M, Zijlstra JA, Beesems SG, Blom MT, van Hoeijen DA, Waalewijn RA, et al. Causes for the declining proportion of ventricular fibrillation in out-of-hospital cardiac arrest. Resuscitation 2015; 96:23–29. [DOI] [PubMed] [Google Scholar]
- 20.Granfeldt A, Wissenberg M, Hansen SM, Lippert FK, Lang-Jensen T, Hendriksen OM, et al. Clinical predictors of shockable versus non-shockable rhythms in patients with out-of-hospital cardiac arrest. Resuscitation 2016; 108:40–47. [DOI] [PubMed] [Google Scholar]
- 21.Lin YN, Chang SS, Wang LM, Chi HT, Ueng KC, Tsai CF, et al. Prehospital predictors of initial shockable rhythm in out-of-hospital cardiac arrest: findings from the Taichung sudden unexpected death registry (THUNDER). Mayo Clin Proc 2017; 92:347–359. [DOI] [PubMed] [Google Scholar]
- 22.Polentini MS, Pirrallo RG, McGill W. The changing incidence of ventricular fibrillation in Milwaukee, Wisconsin (1992-2002). Prehosp Emerg Care 2006; 10:52–60. [DOI] [PubMed] [Google Scholar]
- 23.Renkiewicz GK, Hubble MW, Wesley DR, Dorian PA, Losh MJ, Swain R, Taylor SE. Probability of a shockable presenting rhythm as a function of EMS response time. Prehosp Emerg Care 2014; 18:224–230. [DOI] [PubMed] [Google Scholar]
- 24.Rea TD, Eisenberg MS, Culley LL, Becker L. Dispatcher-assisted cardiopulmonary resuscitation and survival in cardiac arrest. Circulation 2001; 104:2513–2516. [DOI] [PubMed] [Google Scholar]
- 25.Tanigawa K, Iwami T, Nishiyama C, Nonogi H, Kawamura T. Are trained individuals more likely to perform bystander CPR? An observational study. Resuscitation 2011; 82:523–528. [DOI] [PubMed] [Google Scholar]
- 26.Teo MHN, Wong WEJ, Daniel PCN, Kweh RHC, Ho RYJ, Koh JH, et al. The use of dispatcher assistance in improving the quality of cardiopulmonary resuscitation: a randomised controlled trial. Resuscitation 2019; 138:153–159. [DOI] [PubMed] [Google Scholar]
- 27.Spelten O, Warnecke T, Wetsch WA, Schier R, Böttiger BW, Hinkelbein J. Dispatcher-assisted compression-only cardiopulmonary resuscitation provides best quality cardiopulmonary resuscitation by laypersons: a randomised controlled single-blinded manikin trial. Eur J Anaesthesiol 2016; 33:575–580. [DOI] [PubMed] [Google Scholar]
- 28.Tanaka Y, Taniguchi J, Wato Y, Yoshida Y, Inaba H. The continuous quality improvement project for telephone-assisted instruction of cardiopulmonary resuscitation increased the incidence of bystander CPR and improved the outcomes of out-of-hospital cardiac arrests. Resuscitation 2012; 83:1235–1241. [DOI] [PubMed] [Google Scholar]
- 29.Derkenne C, Jost D, Thabouillot O, Briche F, Travers S, Frattini B, et al.; Paris Fire Brigade Cardiac Arrest Task Force. Improving emergency call detection of Out-of-Hospital Cardiac Arrests in the Greater Paris area: efficiency of a global system with a new method of detection. Resuscitation 2020; 146:34–42. [DOI] [PubMed] [Google Scholar]
- 30.Mikkelsen S, Lassen AT. The Danish prehospital system. Eur J Emerg Med 2020; 27:394–395. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.