Abstract
Objectives
To assess the changes in alveolar bone of the mandibular second molars following molar protraction and investigate the factors associated with the alveolar bone changes.
Materials and Methods
Cone-beam computed tomography of 29 patients (mean age 22.0 ± 4.2 years) who had missing mandibular premolars or first molars and underwent molar protraction were reviewed. Alveolar bone level was measured as the distance from the cementoenamel junction at six points, buccal, lingual, mesiobuccal (MB), mesiolingual (ML), distobuccal (DB), and distolingual (DL), of the second molars at pretreatment (T0) and after molar protraction (T1). Factors associated with alveolar bone changes at the distal and mesial of the second molars were assessed.
Results
Mean alveolar bone changes ranged from −1.2 mm (bone apposition) to 0.8 mm (bone resorption). The presence of a third molar impaction at T0 (P < .001), third molar angulation at T0 (P < .001), and Nolla's stage of third molar at T0 (P = .005) were significantly associated with alveolar bone level changes distal to the second molars. Treatment duration (P = .028) was significantly associated with alveolar bone level changes mesial to the second molar.
Conclusions
Patients with impacted third molars, third molars at an earlier stage of development, and mesially angulated third molars at pretreatment may have less alveolar bone resorption distal to the second molars following protraction. Patients with increased treatment time may have reduced alveolar bone resorption mesial to the second molars.
Keywords: Cone-beam computed tomography, Alveolar bone loss, Orthodontic space closure, Molar protraction
INTRODUCTION
Because the mandibular first molar is an early-erupting permanent tooth, it is easily exposed to dental caries or periodontitis, resulting in its being the most frequently missing tooth due to extraction.1 In addition, the mandibular second premolar is one of the most frequently missing teeth congenitally.2,3 Regardless of whether a tooth is missing due to extraction or agenesis, the excess space can be closed orthodontically by molar protraction (Figure 1).4–8 Molar protraction can be challenging for clinicians, but with the aid of temporary anchorage devices (TADs), molars can be more easily protracted to close the space.9–11 When the patient has a third molar in the same quadrant as the missing tooth, it may be aligned along the posterior line of occlusion to replace the missing tooth. As the available space increases posteriorly following molar protraction, impacted third molars may spontaneously erupt and mesialize to attain posterior occlusion.12 However, the amount of spontaneous mesial movement and changes in tooth angulation during eruption vary depending on various factors.12–14
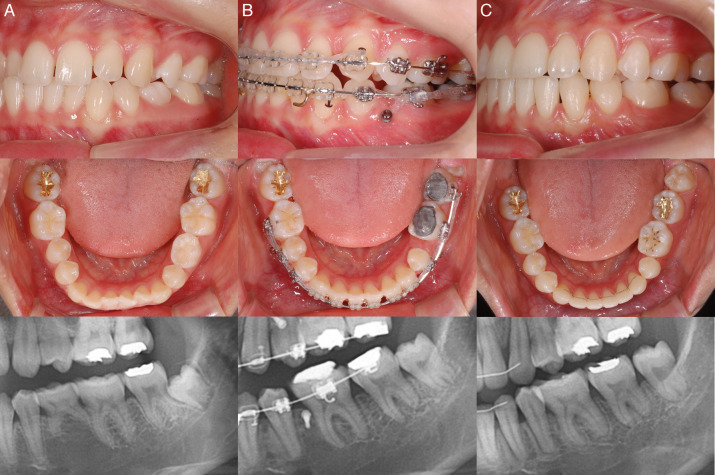
Figure 1.
Protraction of mandibular first and second molars in a patient congenitally missing a second premolar. (A) Before treatment. (B) Protraction using a temporary skeletal anchorage device. (C) After treatment.
When molars are protracted into the edentulous alveolar ridge of an edentulous area, the periodontal health of the protracted tooth might be a concern. A mean of 0.56 ± 0.70 mm of mesial alveolar bone resorption was observed as a result of molar protraction.7 In another study, alveolar bone loss was reported distal to the protracted molar.15 A cone-beam computed tomography (CBCT) study on the alveolar bone level of protracted molars showed slight bone dehiscence at the lingual and buccal alveolar bone crest, compared with those who had space reopening followed by prosthodontic treatment.16 However, only buccal and lingual bone at a cross section passing through the center of the teeth were assessed.
Therefore, the purpose of this study was to (1) assess the alveolar bone level of mandibular second molars at the buccal, lingual, mesial, and distal areas and (2) investigate the factors associated with alveolar bone changes as a result of second molar protraction.
MATERIALS AND METHODS
This retrospective study was approved by the Institutional Review Board of Korea University Anam Hospital (IRB 2018AN1657). Treatment records of orthodontic patients with excess space caused by extraction of the mandibular first molar (L-6) or congenital absence of the mandibular second premolar with a retained deciduous molar (L-E) in which the space was orthodontically closed through molar protraction with the use of TADs from 2010 to 2019 were reviewed for the study. The inclusion criteria were as follows: (1) closure of L-6 and L-E spaces through molar protraction, (2) second molar roots aligned perpendicular to the occlusal plane and parallel with the adjacent teeth at the time of space closure, (3) third molars erupted and aligned into occlusion at the end of treatment, (4) healthy periodontium at the start of treatment, and (5) those who agreed and underwent CBCT before and after treatment. The exclusion criteria were (1) malformation of the third molar root, (2) missing third molars, (3) history of previous orthodontic treatment, (4) incisor crowding of >3 mm, (5) incisor protrusion, and (6) generalized periodontitis.
After leveling and alignment, molar protraction was performed by using a 0.018-inch slot molar tube. Sliding mechanics were used in the 0.016 × 0.022-inch stainless steel wire. A TAD was placed mesial to the edentulous space, and protraction force (100–120 g) was applied using elastomeric chains. When a TAD failed, it was replaced in the interdental space mesial to the second premolar or first premolar in cases of missing L-6 or L-E, respectively. Due to the play between the bracket slot and the wire, mesial tipping of the molars may occur when a protraction force is applied. Therefore, V-bends were placed in the wire to minimize mesial tipping. In cases of L-E space, extraction of the deciduous molar was carried out after leveling and alignment.
Patients underwent CBCT (Implagraphy, Vatech, Korea) at pretreatment (T0) and after the full eruption and alignment of the third molars following second molar protraction (posttreatment, T1). The parameters were as follows: tube voltage 60–90 kV, tube current 10 mAs, voxel size 0.2 mm, field of view (FOV) 16 × 8.5 cm, and a scan time of 24 seconds. After importing the CBCT images into the Invivo software (version 5.0, San Diego, Calif), CBCTs acquired at T0 and T1 were superimposed at the lower cortical border of the mandibular body to measure the amount of second molar protraction and change in angulation (Figure 2).17 The amount of second molar protraction was assessed by measuring the distance between the second molar root furcation at T0 and T1 (Figure 2A). The angulation changes of the second molar from T0 to T1 were measured by using the long axis of the second molar: the line connecting the central fossa and the root furcation (Figure 2B).
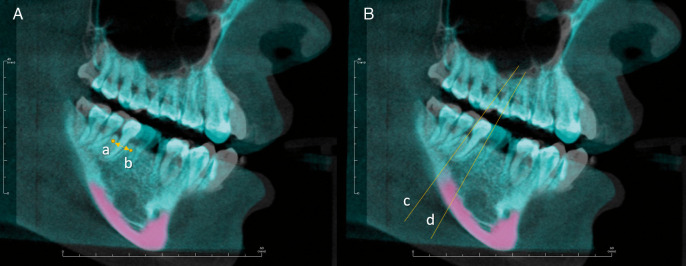
Figure 2.
Cone-beam computed tomographic images acquired at T0 and T1 were superimposed at the lower cortical border of the mandibular body (pink). (A) Amount of second molar protraction (distance between points a and b) and (B) change in angulation (angle between lines c and d) were measured.
For measurement of the alveolar bone level, the CBCTs were reoriented along the posterior occlusal plane and the long axis of the second molar. The sagittal reference plane was defined as the plane passing through the mesial and distal points of the second molar crown and the root furcation. Alveolar bone level was defined as the shortest distance from the most apical alveolar bone to the cementoenamel junction along the long axis (Figure 3) and was measured at six points: buccal, lingual, mesiobuccal (MB), mesiolingual (ML), distobuccal (DB), and distolingual (DL), on the second molar (Figure 4). The mesial and distal bone levels were measured in the sagittal section view, parallel to the mesiodistal axis of the crown. The ML and DL bone levels were measured in a sagittal section halfway from the central groove to the lingual surface (Figure 4A,D). The MB and DB bone levels were measured in a sagittal section halfway from the central groove to the buccal surface (Figure 4A,B). The buccal and lingual bone levels were measured in the coronal section view, perpendicular to the mesiodistal axis of the crown (Figure 4A,C).
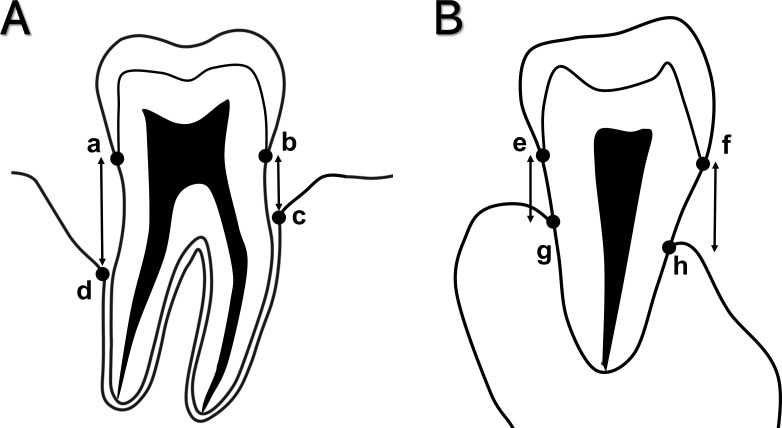
Figure 3.
Measurement of alveolar bone level of the mandibular second molars. (A) Mesial bone level (mm): shortest distance from the most apical point of the mesial alveolar bone to the cementoenamel junction (CEJ) measured along the long axis (bc). Distal bone level (mm): Shortest distance from the most apical point of the distal alveolar bone to the CEJ along the long axis (ad). (B) Buccal bone level (mm): shortest distance from the most apical point of the buccal alveolar bone to the CEJ along the long axis (fh). Lingual bone level (mm): shortest distance from the most apical point of the lingual alveolar bone to the CEJ along the long axis (eg).
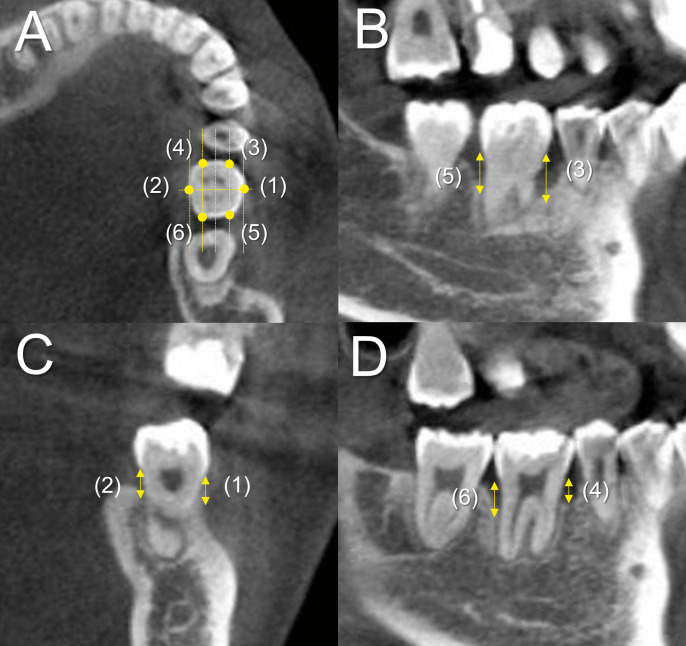
Figure 4.
(A) After reorientation, the alveolar bone level was measured at six points: buccal (1), lingual (2), mesiobuccal (MB; 3), mesiolingual (ML; 4), distobuccal (DB; 5), and distolingual (DL; 6), on the second molar. (B) The MB and DB bone level were measured in the sagittal plane halfway from the central groove to the buccal surface. (C) The buccal and lingual bone levels were measured in the coronal plane perpendicular to the mesiodistal axis of the crown and bisecting the second molar crown. (D) The ML and DL bone level were measured in the sagittal plane halfway from the central groove to the lingual surface.
The buccolingual thickness of the edentulous ridge of the missing space was measured at T0. Ridge thickness was measured in a plane parallel to the occlusal plane and passing through the second molar root furcation at the center of the missing space. Angulations of the second and third molars at T0 were measured relative to the mandibular plane, defined as a line tangent to the lower border of the mandibular body.
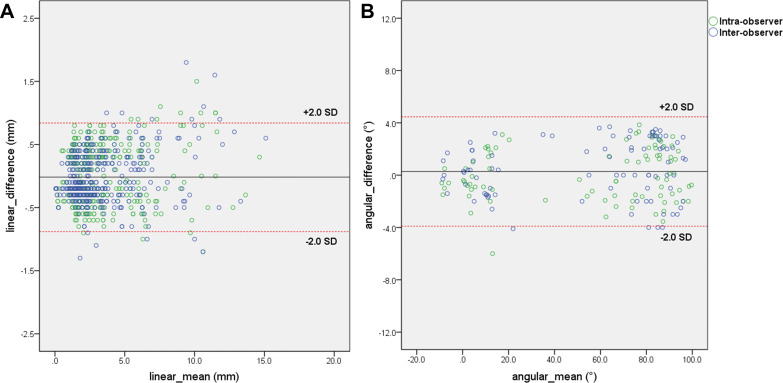
Repeated measurements on all participants were conducted by the same investigator (Dr J-Y Jung) and a second investigator (Dr Kim) after approximately 4 weeks. Intra- and interobserver reliability was evaluated using the Bland–Altman test.
Statistical Analysis
SAS software (version 9.4; SAS Institute, Inc., Cary, NC) was used for all statistical analyses. After calculating descriptive statistics, Fisher's exact test was used to investigate the difference in the distribution of third molar impaction and the missing tooth between males and females. Linear mixed model analyses were conducted to compare the alveolar bone changes and investigate factors associated with alveolar bone changes. Statistical significance was set at a P value of less than .05.
RESULTS
The intra- and interobserver reliabilities for all linear and angular measurements are shown as a Bland–Altman plot (Figure 5). The mean linear error was −0.02 ± 0.43 mm; the mean angular error was 0.28° ± 2.09°.
Figure 5.
(A) Bland–Altman plot for linear measurement errors and (B) the angular measurement errors. The green plot indicates intraobserver differences, and the blue plot indicates interobserver differences.
A total of 29 patients (8 males and 21 females; mean age 22.0 ± 4.2 years) were included. Age, treatment time, Nolla developmental stage of the third molar at T0, number of patients per missing tooth (L-6 or L-E), and number of patients with impacted or erupted third molars at T0 is displayed in Table 1. The second molar was protracted by 7.8 ± 3.8 mm as measured at the furcation. The mean angulation change of the second molar was 3.7° ± 9.6°, with positive values indicating uprighting.
Table 1.
Patient Characteristics at Pretreatment (T0)a
|
|
Male (n = 8) |
Female (n = 21) |
Total (n = 29) |
P
|
| Age, y | 21.9 ± 4.0 | 22.0 ± 4.4 | 22.0 ± 4.2 | .999 |
| Treatment time, y | 3.0 ± 0.8 | 2.9 ± 0.5 | 2.9 ± 0.6 | .720 |
| Nolla_T0, n | 8.6 ± 2.2 | 8.8 ± 1.8 | 8.7 ± 1.9 | .943 |
| Missing tooth, n, L-6 | 7 | 16 | 23 | .647 |
| L-E | 1 | 5 | 6 | |
| Third molar impaction at T0, n | 5 | 11 | 16 | .697 |
| Third molar eruption at T0, n | 3 | 10 | 13 |
L-6, mandibular first molar; L-E, mandibular second premolar with retained deciduous molar; Nolla_T0, Nolla developmental stage of third molar.
The mean alveolar bone levels of the second molars at T0 and T1 are displayed in Table 2. Significant alveolar bone changes were observed at the lingual, DB, DL, and ML of the second molar (Table 2).
Table 2.
Alveolar Bone Level of Mandibular Second Molars at Pretreatment (T0) and Posttreatment (T1) using Cone-Beam Computed Tomographya
| Location |
Time |
Mean ± SD, mm |
Alveolar Bone Change (T1–T0), mm |
95% CI |
P* |
| B | T0 | 2.2 ± 1.5 | 0.4 | (−0.2, 0.9) | .231 |
| T1 | 2.5 ± 1.6 | ||||
| L | T0 | 1.9 ± 1.2 | 1.1 | (0.5, 1.6) | .001 |
| T1 | 3.0 ± 1.3 | ||||
| DB | T0 | 3.9 ± 2.3 | −1.2 | (−1.7, −0.6) | <.001 |
| T1 | 2.7 ± 1.8 | ||||
| MB | T0 | 2.2 ± 1.2 | 0.5 | (−0.04, 1.1) | .071 |
| T1 | 2.7 ± 1.2 | ||||
| DL | T0 | 3.2 ± 1.9 | −0.8 | (−1.4, −0.2) | .008 |
| T1 | 2.4 ± 1.0 | ||||
| ML | T0 | 2.0 ± 1.1 | 0.8 | (0.2, 1.4) | .010 |
| T1 | 2.8 ± 1.3 |
Alveolar bone change, estimated difference of alveolar bone level from T0 to T1, derived from the linear mixed model (T1–T0). Positive values indicate bone resorption. B, buccal; DB, distobuccal; DL, distobuccal; L, lingual; MB, mesiobuccal; ML, mesiobuccal.
P for difference between T0 and T1 according to the linear mixed model analysis.
According to univariate analysis, third molar impaction, third molar angulation at T0, and Nolla stage of third molar at T0 were significantly associated with the changes in alveolar bone level (Table 3). Patients with impacted third molars with mesial angulation at T0 and those at lower Nolla stage were likely to have less alveolar bone resorption at the distal of the second molars as a result of protraction. Age, sex, a missing tooth (L-6 or L-E), second molar angulation at T0, treatment duration, and ridge thickness were not significant as predictors of distal alveolar bone changes. In the multivariable analysis, only third molar angulation and Nolla stages were significant as predictors. In predicting alveolar bone changes at ML and MB of the second molar, treatment duration was the only significant factor; a longer treatment time was associated with less alveolar bone resorption (Table 4).
Table 3.
Factors Associated With Changes (T0–T1) in Alveolar Bone Level Distobuccal (Δ7DB) and Distolingual (Δ7DL) to the Second Molarsa
| Variable |
Univariate Analysis |
Multivariate Analysis |
||||
| Beta |
95% CI |
P
|
Beta |
95% CI |
P
|
|
| Location | ||||||
| Δ7DB | 0 | |||||
| Δ7DL | −0.355 | (−1.038, 0.328) | .297 | |||
| Age | −0.105 | (−0.264, 0.053) | .185 | |||
| Sex | ||||||
| F vs M (Ref) | −0.674 | (−2.173, 0.825) | .365 | |||
| Missing tooth | ||||||
| L-E vs L-6 (Ref) | 0.070 | (−1.606, 1.746) | .933 | |||
| Impaction | ||||||
| 1 vs 0 (Ref) | 2.367 | (1.359, 3.375) | <.001 | |||
| 7MP_T0 | −0.060 | (−0.158, 0.037) | .215 | |||
| 8MP_T0 | −0.092 | (−0.125, −0.059) | <.001 | −.080 | (−0.101, −0.026) | <.001 |
| Nolla_T0 | −0.477 | (−0.798, −0.156) | .005 | −.277 | (−0.501, 0.085) | .027 |
| Treatment time | −0.017 | (−0.115, 0.082) | .734 | |||
| Ridge thickness | 0.163 | (−0.098, 0.423) | .205 | |||
| Movement 7 | 0.093 | (−0.107, 0.293) | .346 | |||
| Angulation 7 | 0.014 | (−0.065, 0.094) | .714 | |||
Δ, change in alveolar bone level from pretreatment to posttreatment (T0–T1); 7MP_T0, second molar angulation measured to the mandibular plane at pretreatment; 8MP_T0, third molar angulation measured to the mandibular plane at pretreatment; F, female; impaction, third molar impaction at pretreatment (1, impacted; 0, nonimpacted); L-6, missing first molar; L-E, missing second premolar with retained deciduous molar; M, male; Nolla, Nolla stage of the third molar at pretreatment; Ref, reference; ridge thickness, thickness of edentulous alveolar ridge at pretreatment.
Table 4.
Factors Associated With Changes (T0–T1) in Alveolar Bone Level Mesiobuccal (Δ7MB) and Mesiolingual (Δ7ML) to the Second Molarsa
| Variable |
Univariate Analysis |
Multivariable Analysis |
|||||
| Beta |
95% CI |
P
|
Beta |
95% CI |
P
|
||
| Location | |||||||
| Δ7MB | 0 | ||||||
| Δ7ML | −.238 | (−0.885, 0.409) | .458 | ||||
| Age | −.041 | (−0.124, 0.043) | .329 | ||||
| Sex | |||||||
| F vs M (Ref) | .249 | (−0.539, 1.037) | .523 | ||||
| Missing tooth | |||||||
| L-E vs L-6 (Ref) | .815 | (−0.007, 1.636) | .052 | ||||
| Impaction | |||||||
| 1 vs 0 (Ref) | .264 | (−0.446, 0.974) | .453 | ||||
| 7MP_T0 | .014 | (−0.038, 0.067) | .587 | ||||
| 8MP_T0 | .002 | (−0.022, 0.027) | .854 | ||||
| Nolla_T0 | −.166 | (−0.346, 0.015) | .070 | −.122 | −0.319 | 0.074 | .211 |
| Treatment time | .053 | (0.006, 0.101) | .028 | .029 | −0.026 | 0.084 | .293 |
| Ridge thickness | .068 | (−0.131, 0.267) | .480 | ||||
| Movement 7 | .050 | (−0.006, 0.200) | .063 | .060 | −0.046 | 0.167 | .255 |
| Angulation 7 | −.009 | (−0.052, 0.035) | .688 | ||||
Δ, change in alveolar bone level from pretreatment to posttreatment (T0–T1); 7MP_T0, second molar angulation measured to the mandibular plane at pretreatment; 8MP_T0, third molar angulation measured to the mandibular plane at pretreatment; angulation 7, angular changes of the second molar from T0 to T1; F, female; impaction, third molar impaction at pretreatment (1, impacted; 0, nonimpacted); L6, missing first molar; LE, missing second premolar with retained deciduous molar; M, male; movement 7, amount of protraction of the second molar from T0 to T1; Nolla, Nolla stage of third molar at pretreatment; Ref, reference; ridge thickness, thickness of the edentulous alveolar ridge at pretreatment.
DISCUSSION
As a result of molar protraction, most patients showed favorable alveolar bone support. Alveolar bone changes after treatment were also not associated with the amount of protraction. Patients who had a narrower alveolar ridge in the edentulous area did not show decreased bone support following protraction. The results were in agreement with previous studies that concluded that moving teeth into edentulous ridges resulted in minimal changes to the periodontal tissues.18–20 A CBCT study also showed that regeneration of the alveolar bone was possible when there was bodily movement of a tooth into an edentulous ridge.21 Stepovich19 compared alveolar bone changes after molar protraction and concluded that buccolingual alveolar bone formation occurred. However, dos Santos et al.16 showed that orthodontic space closure led to greater bone loss in the buccolingual crestal bone than opening an edentulous first molar space for prosthodontic treatment.
The change in the distal alveolar bone level was associated with the developmental stage of the third molar, third molar angulation, and the presence of third molar impaction at pretreatment. Patients with impacted third molars that were mesially angulated and at an earlier stage of development at pretreatment had less bone resorption after protraction. The results were in agreement with previous studies15,22,23 which reported that the angulation of the third molar was associated with the distal alveolar bone level of the second molar. The estimated changes (T1-T0) in alveolar bone level for DB and DL were −1.2 mm (P < .001) and −0.8 mm (P = .008), indicating bone apposition; this was in contrast to the other sites of the alveolar bone that showed bone resorption. This could be explained by the presence of the impacted third molar, as patients with impacted third molars at T0 (n = 16) showed 2.4 ± 2.0 mm and 1.8 ± 1.8 mm of bone apposition of the DB and DL alveolar bone, respectively. In contrast, patients with erupted third molars at T0 showed alveolar bone resorption of 0.4 ± 1.6 mm and 0.4 ± 0.6 mm at the DB and DL alveolar bone, respectively. It has been known that the dental follicle plays a major role in tooth eruption and the coronal part of the dental follicle controls the osteoclastic activity of the adjacent alveolar bone, while the basal part of the dental follicle involves bone formation.24,25 Therefore, increased bone metabolism around the erupting third molar may have affected the alveolar bone changes observed in the distal area.
The mesial alveolar bone change was associated with the total treatment time; a longer treatment time was associated with less alveolar bone resorption. A number of factors may be associated with increased treatment time, such as mesially tipped second molars at pretreatment, protraction force, age, and the buccolingual width of the edentulous ridge. Hom and Turley20 reported that, among 12 adult patients whose edentulous space in the posterior area of the mandible was closed, 5 patients showed bone apposition while 7 showed bone resorption of the mesial alveolar bone. Among the current patients, there were no cases showing bone apposition at the mesial of the second molar. Kondo et al.26 reported that mesial tipping movement of the maxillary molars led to greater crestal bone resorption; therefore, bodily protraction of the molars may be associated with minimal bone resorption on the mesial side.
Due to the retrospective nature of the current study, factors associated with oral hygiene and periodontal indices that could affect the alveolar bone level could not be gathered. A further prospective study may be required to determine the effects of periodontal care on alveolar bone changes as a result of molar protraction. Also, for the current study, CBCTs were taken at the end of treatment rather than after protraction. Therefore, factors related to the leveling of the adjacent teeth may have affected the outcome of the study.
Although CBCTs were not performed as a routine imaging procedure for all orthodontic patients, patients who were included in the study had CBCTs taken before and after treatment in addition to the panoramic radiographs. For future patients who are at a greater risk for alveolar bone loss as a result of molar protraction, CBCTs with a smaller FOV to include only the molar protraction area may be indicated.
CONCLUSIONS
Molar protraction to close an edentulous posterior space leads to changes in the alveolar bone level that are clinically acceptable.
Various risk factors for alveolar bone loss in the mesial and distal alveolar bone should be considered.
Mandibular molar protraction may be considered as an alternative treatment to conventional prosthetic treatment for missing second premolars or first molars in young adults.
ACKNOWLEDGMENT
This research did not receive any specific grant funding from agencies in the public, commercial, or not-for-profit sectors.
REFERENCES
- 1.Meskin LH, Brown LJ. Prevalence and patterns of tooth loss in U.S. employed adult and senior populations, 1985-86. J Dent Educ . 1988;52:686–691. [PubMed] [Google Scholar]
- 2.Ide M, Kuriyama C, Takeuchi C, et al. The prevalence of congenitally missing permanent teeth in Japanese children: a survey conducted in south-west area of Kanto district. Pediatr Dent J . 2011;21:24–30. [Google Scholar]
- 3.Gracco ALT, Zanatta S, Forin Valvecchi F, Bignotti D, Perri A, Baciliero F. Prevalence of dental agenesis in a sample of Italian orthodontic patients: an epidemiological study. Prog Orthod . 2017;18:33. doi: 10.1186/s40510-017-0186-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baik UB, Kook YA, Bayome M, Park JU, Park JH. Vertical eruption patterns of impacted mandibular third molars after the mesialization of second molars using miniscrews. Angle Orthod . 2016;86:565–570. doi: 10.2319/061415-399.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baik UB, Chun YS, Jung MH, Sugawara J. Protraction of mandibular second and third molars into missing first molar spaces for a patient with an anterior open bite and anterior spacing. Am J Orthod Dentofacial Orthop . 2012;141:783–795. doi: 10.1016/j.ajodo.2010.07.031. [DOI] [PubMed] [Google Scholar]
- 6.Baik UB, Kim MR, Yoon KH, Kook YA, Park JH. Orthodontic uprighting of a horizontally impacted third molar and protraction of mandibular second and third molars into the missing first molar space for a patient with posterior crossbites. Am J Orthod Dentofacial Orthop . 2017;151:572–582. doi: 10.1016/j.ajodo.2016.01.019. [DOI] [PubMed] [Google Scholar]
- 7.Kim SJ, Sung EH, Kim JW, Baik HS, Lee KJ. Mandibular molar protraction as an alternative treatment for edentulous spaces: focus on changes in root length and alveolar bone height. J Am Dent Assoc . 2015;146:820–829. doi: 10.1016/j.adaj.2015.04.025. [DOI] [PubMed] [Google Scholar]
- 8.Baik UB, Park JH, Kook YA. Correction of bimaxillary protrusion after extraction of hopeless mandibular posterior teeth and molar protraction. J Clin Orthod . 2017;51:353–359. [PubMed] [Google Scholar]
- 9.Chhibber A, Upadhyay M. Anchorage reinforcement with a fixed functional appliance during protraction of the mandibular second molars into the first molar extraction sites. Am J Orthod Dentofacial Orthop . 2015;148:165–173. doi: 10.1016/j.ajodo.2015.02.029. [DOI] [PubMed] [Google Scholar]
- 10.Kyung SH, Choi JH, Park YC. Miniscrew anchorage used to protract lower second molars into first molar extraction sites. J Clin Orthod . 2003;37:575–579. [PubMed] [Google Scholar]
- 11.Nagaraj K, Upadhyay M, Yadav S. Titanium screw anchorage for protraction of mandibular second molars into first molar extraction sites. Am J Orthod Dentofacial Orthop . 2008;134:583–591. doi: 10.1016/j.ajodo.2006.09.055. [DOI] [PubMed] [Google Scholar]
- 12.De-la-Rosa-Gay C, Valmaseda-Castellón E, Gay-Escoda C. Spontaneous third-molar eruption after second-molar extraction in orthodontic patients. Am J Orthod Dentofacial Orthop . 2006;129:337–344. doi: 10.1016/j.ajodo.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 13.Baik UB, Kang JH, Lee UL, Vaid NR, Kim YJ, Lee DY. Factors associated with spontaneous mesialization of impacted mandibular third molars after second molar protraction. Angle Orthod . 2020;90:181–186. doi: 10.2319/050919-322.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baik UB, Bayome M, Abbas NH, Park JH, Lee UL, Kim YJ. Factors associated with spontaneous angular changes of impacted mandibular third molars as a result of second molar protraction. Am J Orthod Dentofacial Orthop . 2019;156:178–185. doi: 10.1016/j.ajodo.2018.08.024. [DOI] [PubMed] [Google Scholar]
- 15.Baik UB, Choi HB, Kim YJ, Lee DY, Sugawara J, Nanda R. Change in alveolar bone level of mandibular second and third molars after second molar protraction into missing first molar or second premolar space. Eur J Orthod . 2019;41:513–518. doi: 10.1093/ejo/cjz001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Santos P, Herrera Sanches FS, Ferreira MC, de Almeida A, Janson G, Garib D. Movement of mandibular molar into edentulous alveolar ridge: a cone-beam computed tomography study. Am J Orthod Dentofacial Orthop . 2017;151:907–913. doi: 10.1016/j.ajodo.2016.10.024. [DOI] [PubMed] [Google Scholar]
- 17.Ruellas ACdO, Yatabe MS, Souki BQ, Benavides E, Nguyen T, Luiz RR, Franchi L, Cevidanes LHS. 3D mandibular superimposition: comparison of regions of reference for voxel-based registration. PLoS One . 2016;11:e0157625. doi: 10.1371/journal.pone.0157625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lindskog-Stokland B, Hansen K, Ekestubbe A, Wennström JL. Orthodontic tooth movement into edentulous ridge areas—a case series. Eur J Orthod . 2013;35:277–285. doi: 10.1093/ejo/cjr029. [DOI] [PubMed] [Google Scholar]
- 19.Stepovich ML. A clinical study on closing edentulous spaces in the mandible. Angle Orthod . 1979;49:227–233. doi: 10.1043/0003-3219(1979)049<0227:ACSOCE>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 20.Hom BM, Turley PK. The effects of space closure of the mandibular first molar area in adults. Am J Orthod . 1984;85:457–469. doi: 10.1016/0002-9416(84)90085-x. [DOI] [PubMed] [Google Scholar]
- 21.Gündüz E, Rodriguez-Torres C, Gahleitner A, Heissenberger G, Bantleon HP. Bone regeneration by bodily tooth movement: dental computed tomography examination of a patient. Am J Orthod Dentofacial Orthop . 2004;125:100–106. doi: 10.1016/j.ajodo.2003.03.007. [DOI] [PubMed] [Google Scholar]
- 22.Tolstunov L, Brickeen M, Kamanin V, Susarla SM, Selvi F. Is the angulation of mandibular third molars associated with the thickness of lingual bone? Br J Oral Maxillofac Surg . 2016;54:914–919. doi: 10.1016/j.bjoms.2016.06.005. [DOI] [PubMed] [Google Scholar]
- 23.You TM, Ban BH, Jeong JS, Huh J, Doh RM, Park W. Effect of premolar extraction and presence of the lower third molar on lower second molar angulation in orthodontic treatment. Oral Surg Oral Med Oral Pathol Oral Radiol . 2014;118:278–283. doi: 10.1016/j.oooo.2014.05.002. [DOI] [PubMed] [Google Scholar]
- 24.Marks SC, Jr, Cahill DR, Wise GE. The cytology of the dental follicle and adjacent alveolar bone during tooth eruption in the dog. Am J Anat . 1983;168:277–289. doi: 10.1002/aja.1001680303. [DOI] [PubMed] [Google Scholar]
- 25.Marks SC, Jr, Cahill DR. Regional control by the dental follicle of alterations in alveolar bone metabolism during tooth eruption. J Oral Pathol . 1987;16:164–169. doi: 10.1111/j.1600-0714.1987.tb02060.x. [DOI] [PubMed] [Google Scholar]
- 26.Kondo T, Hotokezaka H, Hamanaka R, et al. Types of tooth movement, bodily or tipping, do not affect the displacement of the tooth's center of resistance but do affect the alveolar bone resorption. Angle Orthod . 2017;87:563–569. doi: 10.2319/110416-794.1. [DOI] [PMC free article] [PubMed] [Google Scholar]