Abstract
Objectives
To compare deep overbite treatment using 0.016 × 0.022 nickel-titanium lower reverse curve of Spee archwire (LRCA) or metal anterior bite turbos (ABTs).
Materials and Methods
48 patients with deep overbite malocclusion were randomly allocated into two groups. Group I (age = 18.4 ± 2.8 years, overbite = 5.8 ± 0.6 mm) was treated with LRCA, while Group II (age = 18.2 ± 3.1 years, overbite = 5.2 ± 0.4 mm) was treated with ABTs bonded to the palatal surface of the upper central incisors. Two cephalograms were taken for each patient, at post-alignment stage (T1) and post-leveling stage (T2). The primary outcomes were the anteroposterior and vertical changes of the lower teeth. The secondary outcomes were the effect on upper incisor inclination and the vertical linear changes of upper teeth, to assess the sagittal and vertical skeletal changes, and to compare the duration of overbite correction.
Results
42 of the 48 patients recruited completed the study (21 in each group). At T2, the lower incisors proclined more in Group I (P ≤ .001). Both lower second molars (P ≤ .001) and lower first molars (P = .001) tipped more distally, while the lower first premolar tipped more mesially, in Group I (P < .05). All cusps of both lower molars showed more extrusion in Group II (P < .05) except for the mesial cusp of lower second molars (P = .095). The duration of overbite correction was shorter using the ABTs by 1.7 months (4.85 ± 1.56 and 3.15 ± 0.93 months for Group I and Group II, respectively).
Conclusions
LRCA causes lower incisor proclination with distal tipping of lower molars, while ABTs result in lower posterior tooth extrusion.
Keywords: Deep overbite, Bite turbos, Reverse curve archwires
INTRODUCTION
Correction of deep overbite is among the objectives of orthodontic treatment and is related to stability of the occlusion.1 Numerous methods have been used to treat deep overbite malocclusions. These methods range from removable appliances to fixed appliances with or without orthognathic surgery.2 Nonsurgical treatment options involve incisor intrusion,3 incisor proclination,4 extrusion of the posterior segment,5 or a combination.
Tweed6 described using a continuous single archwire with a reverse curve of Spee (COS) that engaged all mandibular teeth to correct deep overbite. This method was shown to level the COS with a tendency for mandibular premolar and molar extrusion, and incisor intrusion.6,7–9 Another method to correct deep overbite was using a removable or fixed anterior bite plate to disclude the posterior teeth, allowing their passive eruption.10
Although the dental effects of each deep overbite treatment modality was studied previously, no randomized controlled trial compared the skeletal and dental cephalometric changes between nickel-titanium reverse curve archwires (RCA) and anterior bite turbos (ABTs) in two matched groups. The primary purpose of this study was to compare two methods of deep overbite treatment: 0.016 × 0.022-inch nickel-titanium (NiTi) LRCA and ABTs and their effect on changes in the inclination of lower incisors and angular and vertical changes of lower incisors, molars, and premolars. The secondary outcomes were assessment of sagittal and vertical skeletal changes, to measure the change in the inclination of upper incisors and the vertical changes of upper posterior and anterior teeth, and to compare the treatment duration between the two treatment modalities.
MATERIALS AND METHODS
Trial Design and any Changes after Trial Commencement
This single-center study was a two-arm parallel randomized clinical trial with a 1:1 allocation. The methods were not changed after trial initiation.
Participants, Eligibility Criteria, and Settings
This trial was conducted at the Postgraduate Dental Teaching Clinics at Jordan University of Science and Technology. The study was approved by the Institutional Review Board Committee, King Abdullah University Hospital (#106/118/2018).
Inclusion and Extrusion Criteria
Inclusion criteria were: (1) patients with increased overbite (more than half of the lower incisors), (2) mild skeletal discrepancy assessed by patient profile, (3) no missing or extracted teeth in the lower arch except for third molars, (4) patients whose treatment plan did not include extraction of lower teeth and/or any extrusive mechanics (headgear, functional appliance, expansion appliance, and intermaxillary elastics). Exclusion criteria were: (1) patients with an overjet where the placement of anterior bite turbos were not feasible (>6 mm), (2) partially erupted or unerupted lower permanent second molars, (3) previous orthodontic treatment, (4) poor oral hygiene, (5) periodontally compromised teeth.
Oral and written explanations of the purpose of the study were given to all subjects who agreed to participate. Informed consent was signed by the patient or the parent if the patient was under 18 years of age.
Interventions
The orthodontic treatment was carried out by the same orthodontist (E. M.) using fixed appliances with 0.022 × 0.028-inch slot brackets (Victory series, Roth prescription; 3M Unitek, Monrovia, CA, USA). Treatment was started by bonding the upper and lower arches, except for those patients with increased overbite and reduced overjet that made lower incisor bonding not feasible. In those patients, treatment in the lower arch was postponed until the overjet was increased.
After the initial alignment stage, the deep overbite was corrected either using lower 0.016 × 0.022-inch NiTi RCA (Ormco corporation, Kleen Pak System, Glendora, Calif) with a cinch back distal to the lower second permanent molars (Group I) or fixed metal ABTs (Orthodontic Stop And Bite Guide, Morelli, Sorocaba, Brazil) bonded to the middle of the palatal surface of maxillary central incisors (Group II) with 0.016 × 0.022-inch NiTi archwire in the mandibular arch. The upper archwire was 0.019 × 0.025-inch rectangular stainless steel. All patients in both groups were followed up monthly until an average overbite was achieved (one-third or less of the lower incisor crown occluded by the upper incisors).
Outcomes (Primary and Secondary)
Lateral cephalograms were taken for all patients after the alignment stage (T1) and after the leveling stage (T2) using the same machine (ORTHOPHOS XG PLUS, Dentsply Sirona Company, Charlotte, NC, USA). The cephalometric radiographs in JPEG format were imported to FACAD Orthodontic tracing software (Version 3.11.2.1616, Ilexis AB Company, Linköping, Sweden) to perform cephalometric analysis. Calibration of image actual size was made based on the measurement of the x-ray system ruler. Landmark identification was carried out manually on digital images using a mouse-driven cursor.
All cephalometric tracings were done twice by the same investigator (E. M.), and FACAD software calculated the linear and angular measurements. The mean of the two measurements was used in the calculations.
Primary Outcomes
Thirty-six hard tissue and dental landmarks were identified (Figure 1, Table 1), and angular measurements were obtained on each cephalogram (Table 2). To assess the linear dental changes of the mandibular and maxillary teeth, a horizontal reference line (HRL) was determined at T1 (drawn from Sella, 7° below the SN line) and a perpendicular line to the HRL passing through Sella formed the vertical reference line (VRL) (Figure 2).11
Figure 1.
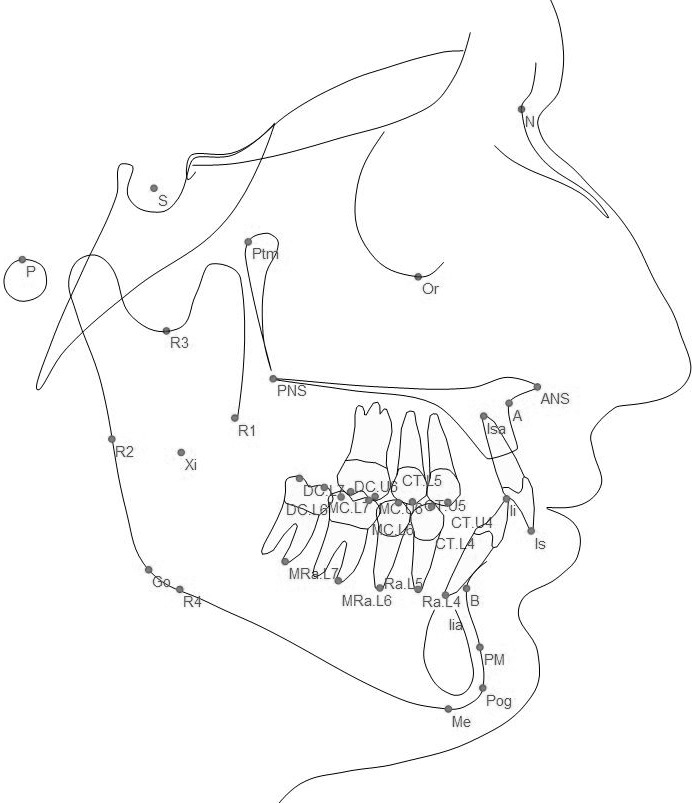
Dental and skeletal cephalometric landmarks.
Table 1.
Definitions of Dental Cephalometric Landmarks
| Dental Landmarks |
Definitions |
| l.s | The incisal tip of the most labially positioned maxillary central incisor |
| l.sa | The root apex of the most labially positioned maxillary central incisor |
| CT.U4 | The cusp tip of the maxillary first premolar |
| CT.U5 | The cusp tip of the maxillary second premolar |
| MC.U6 | The mesial cusp tip of the maxillary first molar |
| DC.U6 | The distal cusp tip of the maxillary first molar |
| L.i | The incisal tip of the most labially positioned mandibular incisor |
| L.ia | The root apex of the most labially positioned mandibular incisor |
| CT.L4 | The cusp tip of the mandibular first premolar |
| Ra.L4 | The root apex of the mandibular first premolar |
| CT.L5 | The cusp tip of the mandibular second premolar |
| Ra.L5 | The root apex of the mandibular second premolar |
| MC.L6 | The mesial cusp tip of the mandibular first molar |
| DC.L6 | The distal cusp tip of the mandibular first molar |
| MRa.L6 | The mesial root apex of the mandibular first molar |
| MC.L7 | The mesial cusp tip of the mandibular second molar |
| DC.L7 | The distal cusp tip of the mandibular second molar |
| MRa.L7 | The mesial root apex of the mandibular second molar |
| Point I | A point on the long axis of the mandibular central incisor, two-thirds of its length from the incisal edge |
Table 2.
Definitions of the Angular Cephalometric Measurements
| Angular Measurements |
Definitions |
| SNA | The angle formed by the intersection of the S-N line and a line from (N) to (A) point |
| SNB | The angle formed by the intersection of the S-N line and a line from (N) to (B) point |
| ANB | It is the difference between the SNA and SNB angles. |
| Mn-Mx | The angle formed by the intersection of mandibular plane (MP) and maxillary plane (Mx) |
| FH-Mn | The angle formed by the intersection of Frankfurt horizontal plane (FH), and mandibular plane (Mn) |
| UI-Mx | The angle formed by the intersection of a line from the (U.It) to (U.Ia) (the long axis of maxillary central incisor) and maxillary plane (Mx) |
| LI-C.A | The angle formed by the intersection of a line from the (L.1t) to the (L.Ia) (the long axis of mandibular central incisor) and the corpus axis (C.A) |
| L.4-C.A | The angle formed by the intersection of a line from the (CT.L4) to the (Ra.L4) and the corpus axis (C.A) |
| L.5-CA | The angle formed by the intersection of a line from the (CT.L5) to the (Ra.L5) and the corpus axis (C.A) |
| L6-C.A | The angle formed by the intersection of a line from the (MC.L6) to the (MRa.L6) and corpus axis (C.A) |
| L7.-C.A | The angle formed by the intersection of a line from the (MC.L7) to the (MRa.L7) and the corpus axis (C.A) |
Figure 2.
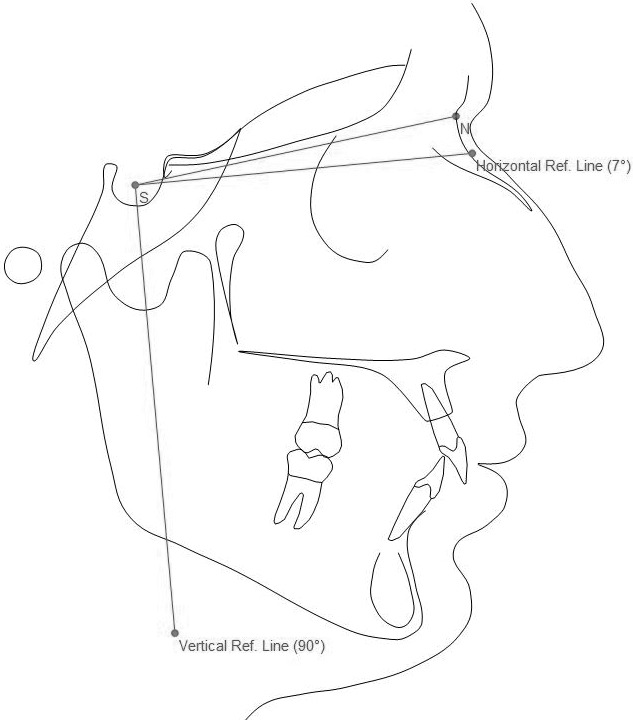
Horizontal and vertical reference lines.
To measure the changes in the mandibular dentition, T1 and T2 lateral cephalometric radiographs were superimposed on the corpus axis at protuberance menti (Pm).12 The change of the position of the lower incisor tip horizontally was determined by drawing perpendicular lines from the lower incisor tips at T1 and T2 to HRL; the linear distance between these two lines measured at the HRL determined the anterioposterior change in the position of the lower incisors (Figure 3). To determine the change in the vertical position of the lower posterior teeth and lower incisor edge, perpendicular lines from each cusp tip at T1 and T2 were drawn to VRL and the linear distance between the two lines was measured at the VRL to determine the vertical change of these teeth (Figure 3).
Figure 3.
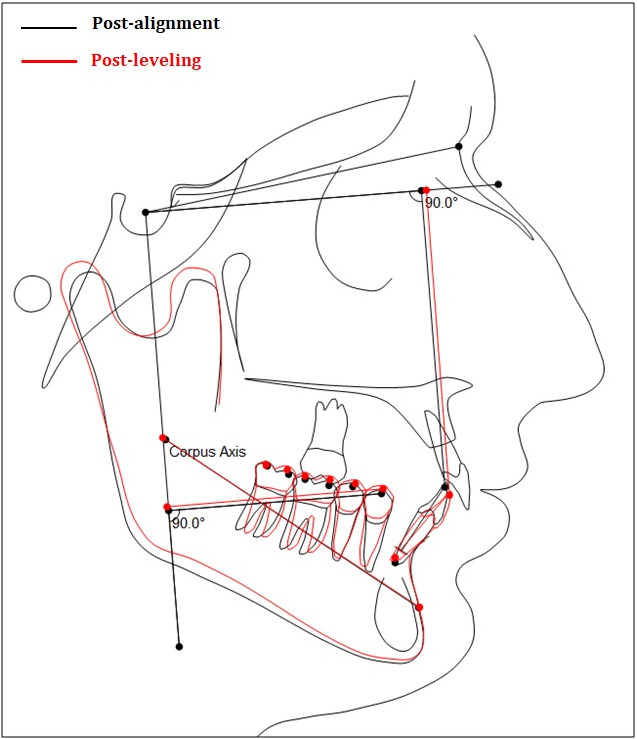
Changes in horizontal and vertical positions of the mandibular teeth.
True vertical movement of the lower incisors was determined by measuring the length of the post-alignment (T1) incisor, then this length was multiplied by 0.66 to determine the position of Point I along the long axis of the tooth, two-thirds of its length from the incisal edge.13 This measurement was then carried out using a transfer line with the same length on the T1 lateral cephalogram and the point was then relocated on the T2 lateral cephalogram. Then the perpendicular lines from these points were drawn to the VRL and the linear distance between the two lines was measured at the VRL to determine the true lower incisor vertical change (Figure 3).
Secondary Outcomes
For the maxillary dental changes, T1 and T2 lateral cephalograms were superimposed according to the Bolton template of maxillary superimposition by using the anterior palatal contour.14 Similar methods as were used to determine changes in the lower arch were applied to determine the change of the vertical and horizontal position of the upper incisor tip and to determine the change in the vertical position of the upper first molar and premolars (Figure 4).
Figure 4.
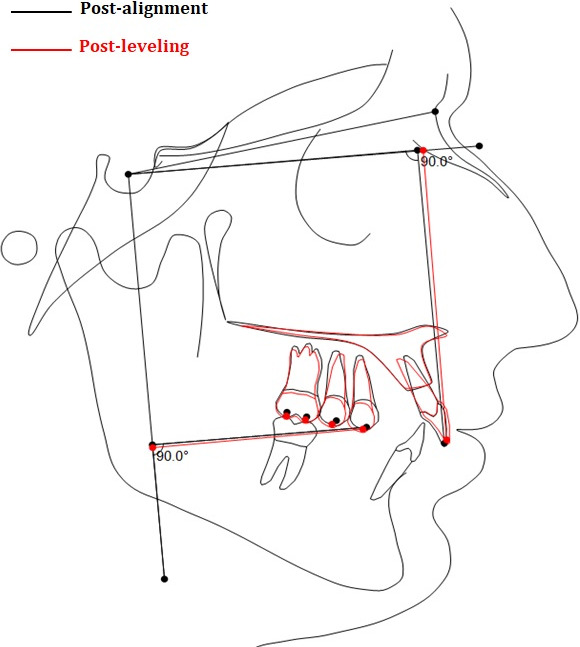
Changes in horizontal and vertical positions of the maxillary teeth.
The anterior lower facial height ratio (LFH) was measured as the distance between the anterior nasal spine and menton, divided by the distance between nasion and menton.15
Sample Size Calculation
Sample size calculation was done using G*power version 3.1.9.4.16 Assuming an effect size (0.8) based on the studies of Alqabandi et al.17 and Akarsu and Ciger18 (mean lower incisor proclination using RCA and ABTs were 6.1 + 3.85 and 5.3 + 5.32, respectively) showed that a total sample size of 42 subjects with a conventional alpha level (0.05) and desired power (1 – β) of 0.80 should be recruited for the study. Six patients were added to compensate for dropouts (attrition rate: 15%).
Randomization
Participants were randomly allocated into two groups. A randomization sequence was created using Excel 2010 (Microsoft, Redmond, WA, USA) with a 1:1 allocation using a random block size of 4. The allocation sequence was concealed from the investigator (E. M.) responsible for assigning participants into the intervention groups in sequentially numbered, opaque, and sealed envelopes. Each patient was asked to pick a sealed envelope to assign the method of intervention.
Blinding
Blinding was not possible during the clinical intervention. Blinding of the investigator was implemented at the data measurement stage by coding all lateral cephalometric radiographs. The LRCA and ABTs were removed before taking the x-rays.
Statistical Analysis
Descriptive and analytic statistics were obtained using Statistical Package for the Social Sciences (SPSS) software, version 25.0 (Chicago, IL, USA). The significance level was P < .05.
The Shapiro-Wilk test revealed a normal distribution of data. Descriptive statistics were calculated for the two groups. T-test was used to compare the two groups for age and post-alignment mean overbite and overjet, while the chi-square test was used to compare gender and classification of malocclusion.
Paired t-test and one-sample t-test were used to determine the significance of the treatment changes within each group. Independent t-tests were used to determine differences in the cephalometric measurements between the two groups.
For method error, 10 random lateral cephalograms were retraced, analyzed, and superimposed a month after the original measurements. The intra-examiner error was assessed using the intraclass correlation coefficient.
RESULTS
Participant Flow
A total of 48 patients were recruited in the study from March to October 2018, with final data collection completed in December 2019. Six patients were excluded (Figure 5).
Figure 5.
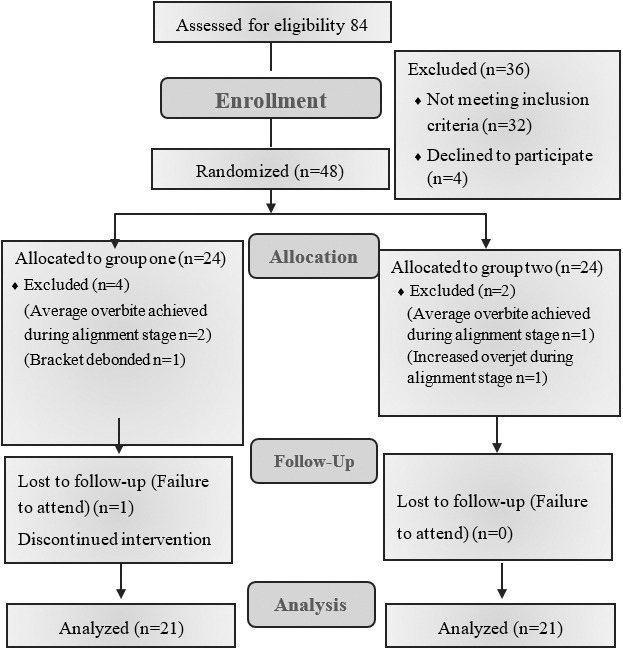
CONSORT flow chart.
Baseline Data
The two groups were matched in age, gender, malocclusion classification, post-alignment means of overbite and overjet, and the Mn-Mx plane angle. (Table 3).
Table 3.
Baseline Characteristics of the Subjectsa
|
|
Group I |
Group II |
P Value |
| Gender | .74 | ||
| Male n (%) | 9 (42.8%) | 8 (38.1%) | |
| Female n (%) | 12 (57.1%) | 13 (61.9%) | |
| Age mean ± SD (mm) | 18.4 ± 2.8 | 18.2 ± 3.1 | .98 |
| Post-alignment overbite, mean ± SD (mm) | 5.8 ± 0.6 | 5.2 ± 0.4 | .40 |
| Post-alignment overjet, mean ± SD (mm) | 4.8 ± 0.9 | 4.5 ± 0.7 | .32 |
| Mx-Mn plane angle, mean ± SD (°) | 25.4 ± 6.9 | 22.5 ± 5.5 | .15 |
| Class. of malocclusion, Class 1 n(%) | 12 (57.1%) | 10 (47.6%) | .18 |
| Class 2 div. I n (%) | 5 (23.8%) | 2 (9.5%) | |
| Class 2 div. II n (%) | 4 (19.0%) | 9 (42.8%) |
Class., classification; div., division; Mx-Mn, maxillary-mandibular plane angle; SD, standard deviation.
Primary Outcomes
There was more positive vertical movement of the cusps of both lower molars in Group II (ABTs) (P < .05), except for the mesial cusp of lower second molars (P = .095) and more negative vertical movement of lower incisors in Group I (LRCA) (P = .014).
In Group I, there was more distal tipping of the lower molars and more mesial tipping of the lower first premolar (P < .05). Lower incisor proclination was also greater in Group I (P ≤ .001; Tables 4 and 5).
Table 4.
Means, Standard Deviations, Mean Differences Between Group I and Group II for Cephalometric Linear Measurements of Lower Teeth That Had Occurred Between T1 and T2a
| Variable |
Group I, Mean ± SD (mm) |
Group II, Mean ± SD (mm) |
Mean Diff. (mm) |
Std. Error Mean (mm) |
95% CI of the Diff. (mm) |
P Value |
| MC L.7-V | 0.72 ± 0.68 | 1.05 ± 0.54 | −0.33 | 0.19 | −0.73 to 0.06 | .095 |
| DC L.7-V | −0.83 ± 0.69 | 0.86 ± 0.61 | −1.69 | 0.20 | −2.11 to −1.27 | ≤.001 |
| MC L.6-V | 0.90 ± 0.46 | 1.29 ± 0.46 | −0.39 | 0.14 | −0.68 to −0.09 | .011 |
| DC L.6-V | 0.11 ± 0.81 | 1.15 ± 0.47 | −1.04 | 0.21 | −1.46 to −0.61 | ≤.001 |
| CT L.5-V | 1.02 ± 0.48 | 1.22 ± 0.52 | −0.20 | 0.16 | −0.53 to 0.11 | .219 |
| CT L.4-V | 0.96 ± 0.41 | 1.06 ± 0.31 | −0.10 | 0.11 | −0.33 to 0.13 | .386 |
| LCI-V | −1.94 ± 0.90 | −1.25 ± 0.80 | −0.69 | 0.26 | −1.24 to −0.14 | .014 |
| LCI-H | 0.77 ± 0.64 | 0.86 ± 0.41 | −0.08 | 0.17 | −0.43 to 0.26 | .623 |
| Point I | −1.01 ± 0.80 | −0.28 ± 0.50 | −0.73 | 0.21 | −1.15 to −0.30 | .001 |
| O.B Ch | 4.07 ± 0.69 | 3.87 ± 0.72 | 0.20 | 0.22 | −0.25 to −0.65 | .378 |
CI indicates confidence interval; CT L.4-V, vertical change in the cusp tip of the lower first premolar; CT L.5-V, vertical change in the cusp tip of the lower second premolar; DC L.6-V, vertical change in the distal cusp of the lower first molar; DC L.7-V, vertical change in the distal cusp of the lower second molar; Diff., difference; LCI-H, horizontal change in the lower incisor position; LCI-V, vertical change in the lower incisor position; MC L.6-V, vertical change in the mesial cusp of the lower first molar; MC L.7-V, vertical change in the mesial cusp of the lower second molar; O.B Ch, change of the overbite; Point I, vertical change of the point I; SD, standard deviation; Std., standard.
Table 5.
Means, Standard Deviations, Mean Differences Between Group I and Group II for Cephalometric Angular Measurements of Lower Teeth That Had Occurred Between T1 and T2a
| Variable |
Group I, Mean ± SD (°) |
Group II, Mean ± SD (°) |
Mean Diff. (°) |
Std. Error Mean (°) |
95% CI of the Diff. (°) |
P Value |
| L7-C.A | −7.92 ± 4.56 | 0.71 ± 3.28 | −8.64 | 1.25 | −11.18 to −6.09 | ≤.001 |
| L6-C.A | −2.97 ± 3.21 | 0.88 ± 4.54 | −3.85 | 1.24 | −6.37 to −1.33 | .002 |
| L5-C.A | −0.32 ± 2.83 | 1.18 ± 2.90 | −1.50 | 0.91 | −3.33 to 0.33 | .107 |
| L4-C.A | 3.03 ± 2.61 | 1.05 ± 1.77 | 1.98 | 0.71 | 0.55 to 3.41 | .008 |
| LI-C.A | 5.74 ± 2.56 | 2.82 ± 1.80 | 2.92 | 0.70 | 1.50 to 4.33 | ≤.001 |
CI indicates confidence interval; Diff., difference; L4-C.A, lower first premolar angle to corpus axis; L5-C.A, lower second premolar angle to corpus axis; L6-C.A, lower first molar angle to corpus axis; L7-C.A, lower second molar angle to corpus axis; LI-C.A, lower central incisor angle to corpus axis; SD, standard deviation; Std., standard.
Secondary Outcomes
The upper central incisors showed more proclination, horizontal (advancement) and vertical (intrusion) movements in Group II (P = .001, P < .001, and P = .05, respectively). There was no significant difference between the two groups regarding the vertical movement of the upper posterior teeth (Table 6). Comparing the skeletal changes, only the LFH ratio increased significantly more in Group II (P = .002) (Table 7). The duration of leveling was significantly shorter (by 1.7 months) in Group II (Table 8).
Table 6.
Means, Standard Deviations, Mean Differences Between Group I and Group II for Cephalometric Angular and Linear Measurements of Upper Teeth That Had Occurred Between T1 and T2a
| Variable |
Group I, Mean ± SD |
Group II, Mean ± SD |
Mean Diff. |
Std. Error Mean |
95% CI of the Diff. |
P Value |
| UI-Mx (°) | 0.37 ± 0.58 | 1.47 ± 1.22 | −1.09 | 0.30 | −1.71 to −0.47 | .001 |
| UCI-V (mm) | 0.02 ± 0.07 | −0.43 ± 0.63 | 0.43 | 0.14 | 0.16 to 0.74 | .005 |
| UCI-H (mm) | 0.07 ± 0.16 | 0.63 ± 0.38 | −0.53 | 0.08 | −0.74 to −0.37 | ≤.001 |
| MC U.6-V (mm) | 0.04 ± 0.05 | 0.08 ± 0.07 | −0.04 | 0.02 | −0.08 to −0.01 | .055 |
| DC U.6-V (mm) | 0.05 ± 0.05 | 0.08 ± 0.07 | −0.01 | 0.02 | −0.07 to 0.01 | .700 |
| CT U.5-V (mm) | 0.04 ± 0.05 | 0.08 ± 0.07 | −0.04 | 0.02 | −0.07 to 0.01 | .117 |
| CT U.4-V (mm) | 0.07 ± 0.06 | 0.07 ± 0.08 | −0.01 | 0.02 | −0.04 to 0.04 | .879 |
CI indicates confidence interval; CT U.4-V, vertical change in the cusp tip of the upper first premolar; CT U.5-V, vertical change in the cusp tip of the upper second premolar; DC U.6-V, vertical change in the distal cusp of the upper first molar; Diff., difference; MC U.6-V, vertical change in the mesial cusp of the upper first molar; SD, standard deviation; Std., standard; U.C.I-H, horizontal change in the upper incisor position; U.C.I-V, vertical change in the upper incisor position; UI-Mx, upper central incisor angle to the maxillary plane.
Table 7.
Means, Standard Deviations, Mean Differences Between Group I and Group II for Cephalometric Skeletal Measurements That Had Occurred Between T1 and T2a
| Variable |
Group I, Mean ± SD |
Group II, Mean ± SD |
Mean Diff. |
Std. Error Mean |
95% CI of the Diff. |
P Value |
| SNA (°) | −0.11 ± 1.49 | 0.18 ± 0.70 | −0.28 | 0.19 | −0.67 to 0.10 | .256 |
| SNB (°) | 0.18 ± 1.11 | 0.20 ± 0.57 | −0.02 | 0.28 | −0.58 to 0.54 | .456 |
| ANB (°) | −0.23 ± 0.91 | −0.04 ± 0.63 | −0.19 | 0.24 | −0.69 to 0.31 | .438 |
| Mx-Mn (°) | 0.22 ± 0.59 | 0.69 ± 0.89 | −0.47 | 0.24 | −0.96 to 0.01 | .067 |
| FH-Mn (°) | 0.15 ± 0.47 | 0.42 ± 0.49 | −0.27 | 0.15 | −0.57 to −0.03 | .085 |
| LFH (%) | −0.09 ± 0.54 | 0.41 ± 0.42 | −0.51 | 0.15 | −0.82 to −0.19 | .002 |
CI indicates confidence interval; Diff., difference; FH-Mn indicates Frankfort mandibular plane angle; LFH, lower facial height; Mx-Mn, maxillary-mandibular plane angle; SD, standard deviation; Std., standard.
Table 8.
Mean and Standard Deviation of the Treatment Duration From T1-T2 in Both Groups and the Mean Difference Between Them
| Group, Duration (mo) |
Mean ± SD |
Mean Diff. |
P Value |
| Group I | 4.85 ± 1.56 | 1.7 | ≤ .001 |
| Group II | 3.15 ± 0.93 |
Diff. indicates difference; SD, standard deviation.
Method Error
The intraclass correlation coefficients ranged from 0.927 to 0.992, indicating reproducible measurements and reliable data.
DISCUSSION
For a reliable comparison of treatment changes, basic demographic characteristics such as age, gender, post-alignment overbite, overjet, classification of the malocclusion, and Mn-Mx plane angle were evaluated to examine the compatibility of the two groups. This reduced any possible confounding effects of those factors.
The initial lateral cephalometric radiographs were taken only after the alignment stage to reduce the risk of exposure of participants to ionizing radiation. Previous studies concluded that, for most patients, the clinical examination supplemented with study models and photographs provided adequate information for orthodontic treatment planning, and cephalometric radiographs did not make a significant difference to the treatment decisions.19,20 The need for pretreatment cephalometric images in this study was minimized by restricting the sample to cases with Class I or mild Class II malocclusions. Although during the alignment stage, the overbite is usually reduced due to incisor proclination, this was not evaluated, as it was not one of the study aims. Taking the lateral cephalograms after the completion of alignment eliminated any changes that could have occurred at this stage and made studying the effects of leveling more accurate.
Only one RCA was used to correct the deep overbite because the aim was to study the effect of 0.016 × 0.022-in NiTi archwire. Additionally, using stainless steel RCA would have added another variable (the amount of reverse curve) as preformed stainless steel RCAs were not available.
Primary Outcomes
Deep overbite correction using RCA led to incisor proclination. This was in agreement with previous studies,3,6,7,17 which confirmed that, when using reverse curve archwires to open the bite, the incisors became more proclined.
There were variations in the average proclination of lower incisors that were reported in other previous studies.3,6,7,9,17 This might have been due to the use of different archwire dimensions, the use of the mandibular plane as a reference line, and that previous studies reported the overall changes in lower incisor inclination rather than the effect of arch leveling alone.
Evaluation of the data obtained from the change in lower incisor inclination to the corpus axis after correction of the deep overbite using ABTs revealed a statistically significant increase in inclination by an average of 2.28°. This was in agreement with Lindauer et al.21 and Akarsu and Ciger,18 who found that there was an average proclination of the lower incisor by a mean of 5.5° and 3°, respectively, when an anterior bite plate was used to correct overbite.
As a consequence of the proclination, the lower incisor incisal edge moved apically and horizontally in both groups. Since the lower central incisor proclined more in Group I, the incisal edge also moved more apically and horizontally. To determine if there was true intrusive movement that occurred during the treatment, the vertical change of the point I was measured. More true intrusion was observed in cases treated with LRCA than cases treated with ABTs (1 mm vs 0.28 mm, respectively); this difference was statistically significant but clinically was not a significant change.
The exact vertical movement of each cusp tip of the lower posterior teeth was determined. As the distal cusp of the lower second molar was intruded in Group I and extruded in Group II, there was an average of 1.69 mm difference between the two groups (P = ≤.001). The mesial and the distal cusps of the lower first molar was extruded more in Group II than Group I by a mean difference of 0.39 mm and 1.04 mm, respectively (P < .05). There was no significant difference in the extrusive movement of the mesial cusp of the lower second molar, or of the lower second and first premolars between the two groups (P > .05).
Similar to the current study results, Mitchell and Stewart4 reported that, in cases treated with reverse curve archwires, when the lower second molar was banded, it intruded on average by 0.7 mm, while the first molar was extruded up to 0.8 mm. Also, in that study, there was extrusion of the lower second premolar by 1.1 mm on average, and of the lower first premolar by 0.6 mm.
Secondary Outcomes
The two cephalograms at T1 and T2 were superimposed on the maxillary vault to observe any changes that would happen in the upper arch especially when ABTs were used. In both groups, the mean vertical changes of the upper posterior teeth showed no significant difference between the two groups except for the change of the upper central incisor, in which there was more proclination, vertical and horizontal movement of the incisal edge in Group II compared to Group I after leveling (P ≤ .05).
Lindauer et al.21 reported in their study that the acrylic anterior bite plate caused a mean increase of 6.6° in axial inclination of the upper incisors to the Sella-Nasion plane. That was a greater effect than in the current study, but the incisal edge moved apically by 0.4 mm, which was the same amount as in the current study. The reason that Lindauer et al.21 reported more upper incisor proclination might have been because the anterior acrylic bite plate covered more palatal surface area and, thus, may have produced more forward tipping force.
Regarding skeletal changes, only the LFH ratio showed a significant increase (P = .002) in Group II compared to Group I, but the actual difference was very small, an average of 0.15%. This may be explained as having been due to more extrusive movement of the lower posterior teeth in Group II.
In Group II, the duration needed to open the overbite was faster by 1.7 months compared to the time required in Group I (4.85 months for Group I and 3.15 months for Group II). The difference was statistically significant. However, since the duration of the overall orthodontic treatment is usually 24 to 30 months, the clinical significance of this reduction is questionable.
Limitations
Blinding could not be implemented during the intervention.
Only one dimension and type of reverse curve archwire was used.
Generalizability
The results were limited to deep overbite cases treated using one reverse curve archwire type and dimension (0.016 × 0.022-inch NiTi).
CONCLUSIONS
Both 0.016 × 0.022 NiTi LRCA and ABTs were effective in deep overbite correction.
Lower incisors in cases treated with 0.016 × 0.022 NiTi RCA demonstrated more proclination than cases treated with ABTs.
1 mm of absolute intrusion of the lower incisor was noted in cases treated with 0.016 × 0.022 NiTi RCA compared to 0.28 mm in cases treated with ABTs.
Lower first and second molars showed significant distal tipping when the overbite was corrected using 0.016 × 0.022 NiTi RCA.
Greater lower posterior tooth extrusion and a greater increase in the lower facial height ratio were noted in cases treated with ABTs than cases treated with 0.016 × 0.022 NiTi RCA.
The duration of the overbite correction stage of treatment was shorter when ABTs were used to treat cases with deep overbite.
Acknowledgments
ACKNOWLEDGMENTS
Funding
This study was funded by Jordan University of Science and Technology.
REFERENCES
- 1.Bergersen EO. A longitudinal study of anterior vertical overbite from eight to twenty years of age. Angle Orthod . 1988;58:237–256. doi: 10.1043/0003-3219(1988)058<0237:ALSOAV>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 2.Sadowsky C, Sellke T. Management of overbite by controlling incisor and molar movements. Semin Orthod . 2000;6:43–49. [Google Scholar]
- 3.Mitchell DL, Stewart WL. Documented leveling of the lower arch using metallic implants for reference. Am J Orthod . 1973;63:526–532. doi: 10.1016/0002-9416(73)90165-6. [DOI] [PubMed] [Google Scholar]
- 4.Ball JV, Hunt N. The effect of Andresen, Harvold, and Begg treatment on overbite and molar eruption. Eur J Orthod . 1991;13:53–58. doi: 10.1093/ejo/13.1.53. [DOI] [PubMed] [Google Scholar]
- 5.Schudy FF. The control of vertical overbite in clinical orthodontics. Angle Orthod . 1968;38:19–39. doi: 10.1043/0003-3219(1968)038<0019:TCOVOI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 6.Dake ML, Sinclair PM. A comparison of the Ricketts and Tweed-type arch leveling techniques. Am J Orthod Dentofacial Orthop . 1989;95:72–78. doi: 10.1016/0889-5406(89)90138-8. [DOI] [PubMed] [Google Scholar]
- 7.Weiland FJ, Bantleon HP, Droschl H. Evaluation of continuous arch and segmented arch leveling techniques in adult patients. Am J Orthod Dentofacial Orthop . 1996;110:647–652. doi: 10.1016/s0889-5406(96)80042-4. [DOI] [PubMed] [Google Scholar]
- 8.Carcara S, Preston CB, Jureyda O. The relationship between the curve of Spee, relapse, and the Alexander discipline. Semin Orthod . 2001;7:90–99. [Google Scholar]
- 9.Bernstein RL, Preston CB, Lampasso J. Leveling the curve of Spee with a continuous archwire technique: a long term cephalometric study. Am J Orthod Dentofacial Orthop . 2007;131:363–371. doi: 10.1016/j.ajodo.2005.05.056. [DOI] [PubMed] [Google Scholar]
- 10.Hemley S. Bite plates, their application and action. Am J Orthod Oral Surg . 1938;24:721–736. [Google Scholar]
- 11.Al-Nimri KS, Hazza'a AM, Al-Omari RM. Maxillary incisor proclination effect on the position of point A in Class II division 2 malocclusion. Angle Orthod . 2009;79:880–884. doi: 10.2319/082408-447.1. [DOI] [PubMed] [Google Scholar]
- 12.Ricketts RM. A principle of arcial growth of the mandible. Angle Orthod . 1972;42:368–386. doi: 10.1043/0003-3219(1972)042<0368:APOAGO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 13.Greig D. Bioprogressive therapy: overbite reduction with the lower utility arch. Br J Orthod . 1983;10:214–216. doi: 10.1179/bjo.10.4.214. [DOI] [PubMed] [Google Scholar]
- 14.Proffit WR, Sarver DM, Ackerman JL. Diagnosis and treatment planning. In: Proffit WR, HW Fields, Sarver DM, editors. Contemporary Orthodontics 5th ed. St. Louis, MO: Elsevier/Mosby; 2013. 197. [Google Scholar]
- 15.Johnston DJ, Hunt O, Johnston CD, Burden DJ, Stevenson M, Hepper P. The influence of lower face vertical proportion on facial attractiveness. Eur J Orthod . 2005;27:349–354. doi: 10.1093/ejo/cji023. [DOI] [PubMed] [Google Scholar]
- 16.Erdfelder E, Faul F, Buchner A. GPOWER: a general power analysis program. Behav Res Methods Instrum Comput . 1996;28:1–11. [Google Scholar]
- 17.Alqabandi AK, Sadowsky C, Begole EA. A comparison of the effects of rectangular and round archwires in leveling the curve of Spee. Am J Orthod Dentofacial Orthop . 1999;116:522–529. doi: 10.1016/s0889-5406(99)70183-6. [DOI] [PubMed] [Google Scholar]
- 18.Akarsu B, Ciger S. Evaluation of the effects of fixed anterior biteplane treatment on the dental and skeletal structures and masticatory muscles in patients with deep bite. J Hacettepe Fac Dent . 2010;34:10–22. [Google Scholar]
- 19.Han UK, Vig KW, Weintraub JA, Vig PS, Kowalski CJ. Consistency of orthodontic treatment decisions relative to diagnostic records. Am J Orthod Dentofacial Orthop . 1991;100:212–219. doi: 10.1016/0889-5406(91)70058-5. [DOI] [PubMed] [Google Scholar]
- 20.Devereux L, Moles D, Cunningham SJ, McKnight M. How important are lateral cephalometric radiographs in orthodontic treatment planning. Am J Orthod Dentofacial Orthop . 2011;13:175–181. doi: 10.1016/j.ajodo.2010.09.021. [DOI] [PubMed] [Google Scholar]
- 21.Lindauer SJ, Lewis SM, Shroff B. Overbite correction and smile aesthetics. Semin Orthod . 2005;11:62–66. [Google Scholar]


