Abstract
Objectives
To assess speech performance of adult patients undergoing orthodontic treatment with Invisalign.
Materials and Methods
Twenty-four adult patients with Invisalign (Invisalign group: 6 men, 18 women; average age; 34.88 years) and 20 adult patients with fixed labial appliances (fixed group: 5 men, 15 women; average age; 38.85 years) were evaluated. Speech was recorded immediately before delivery of the first set of clear aligners or bonding of labial appliances (T0), immediately after delivery or bonding (T1), and 2 months after delivery or bonding (T2). Speech was evaluated via a combination of three auditory analyses: (1) objective acoustic analysis through digital sonography, (2) semiobjective assessment by six speech and language pathologists, and (3) subjective assessment patient questionnaire.
Results
The objective acoustic analysis showed a statistically significant difference over time from T0 to T1, T1 to T2, and T0 to T2 for Invisalign patients. The semiobjective analysis revealed a significant speech alteration from T0 to T1 and T1 to T2 for both groups, and from T0 to T2 in the Invisalign group. The subjective analysis showed a significant difference between means of Invisalign and fixed group patient perception at both T1 and T2.
Conclusions
Invisalign treatment significantly affected speech, and although patients experience some level of adaptation, speech does not return to normal after 2 months of treatment.
Keywords: Invisalign, Speech
INTRODUCTION
Fixed labial appliances have been the backbone of orthodontics for more than 100 years. Over time, advances in orthodontics have broadened the spectrum of available treatment modalities, including the advent of less visible appliances. This development contributed to a shift in the demographic of the orthodontic patient population to include a higher percentage of adults.1,2 Today, esthetic options for orthodontic treatment include ceramic brackets, lingual braces, and clear aligner therapy (CAT).
Ceramic brackets are less visible, but there are still brackets and wires on the labial surface of the tooth. Lingual braces are considered the most esthetic option3–5 but have been slow to gain popularity in North America due to insufficient training of clinicians.6 This, however, is not the case for another esthetic option: CAT. Clear aligners have gained tremendous momentum in orthodontics, particularly among patients seeking esthetic treatment modalities.
Patients receive information about orthodontic treatment from multiple sources. It is the orthodontist's responsibility to manage patient expectations and provide accurate information to determine what is in the patient's best interest. While esthetics are of great importance, functionality also needs to be considered as it affects patient perceptions and compliance and, thus, treatment outcome. Speech is one of the most commonly affected functions among patients undergoing orthodontic treatment.7 Generally, adults have reduced speech adaptation abilities compared with children due to muscle memory and speech patterns that develop over time.8 With adults comprising a majority of the CAT patient population, orthodontists should be aware of the potential effect on speech. As many adults have jobs and/or social lives where they speak frequently and publicly, speech is of utmost importance. Therefore, it is reasonable to conclude that speech alteration may result in decreased patient compliance.9
Although CAT has been studied for its effectiveness and esthetics, there is little research in the literature evaluating its effect on speech. The few studies that did assess speech alteration in patients undergoing CAT provided insufficient information as they only used methods of subjective nature (patient questionnaire10) or semiobjective (certified speech and language pathologist [SLP] panel11,12). To date, no published studies have objectively evaluated speech performance of patients undergoing CAT.
The purpose of this study was to prospectively assess and compare speech performance of adult patients undergoing orthodontic treatment with Invisalign versus fixed appliances over time. The null hypothesis was that there would be no difference in speech performance between patients undergoing Invisalign and fixed labial appliance treatment.
MATERIALS AND METHODS
A convenience sample was obtained using patients presenting to the orthodontic clinic initiating treatment in one of two modalities—Invisalign (Align Technology, Santa Clara, CA, USA) or labial fixed appliances—who met the inclusion criteria and were willing to participate. The sample population (Invisalign group: 6 men, 18 women, average age 34.88 years) consisted of 24 adult patients who, with their orthodontist, chose Invisalign as their method of treatment. The control population (fixed group: 5 men, 15 women, average age 38.85 years) consisted of 20 adult patients who, with their orthodontist, chose conventional orthodontic therapy with labial fixed appliances as their method of treatment.
Inclusion criteria were ≥18 years old, native English speaker, raised in a monolingual environment, Caucasian, and Class I or Class II malocclusion patients, who were planned for nonextraction treatment. Participants were excluded if they had any other concurrent oral appliance (including but not limited to bite plates, bite turbos, speed bumps), >5 mm overjet, anterior crossbite, anterior open bite, missing teeth, or current speech therapy. Patients with evident speech impairments or documented speech/hearing pathologic conditions (eg, aphasia, cleft lip/palate, hearing loss, voice disorders) were also excluded. Informed consent was obtained from all patients before the start of treatment. The study was reviewed by the Saint Louis University Institutional Review Board and approved (No. 28589).
Bonding attachments and delivering clear aligners/bonding fixed labial appliances was done in both the upper and lower arches at the same appointment for all patients. Clear aligners were changed weekly as directed under the Invisalign treatment sequence. In the fixed labial appliance group, patients had adjustments every 4–6 weeks as is common with a conventional treatment sequence.
Speech performance was evaluated immediately before the delivery of the first set of clear aligners/bonding of labial appliances (T0), immediately after delivery/bonding (T1), and 2 months after delivery/bonding (±1 week) (T2). Articulation was recorded under standardized conditions with a microphone (Fifine Technology, Zhaoqing, GD, China) connected by a USB port to a laptop computer. The following standardized conditions were used for all patients of both groups at each time point: (1) Patient was sitting in an upright position; (2) patient only wore the appliances delivered to them (labial fixed appliances with wires or clear aligners and attachments) intraorally at time of reading (no elastics, wax, etc); (3) patient was in a room with the door closed with minimal background noise; (4) microphone was unobstructed and placed on the table 1 to 2 feet away from the patient's mouth at an angle of 45°; and (5) patient read standardized text (the Grandfather Passage) out loud and was recorded using a software program (Audacity, Version 2.5.0, Audacity Team) for conversion to an mp3 file for upload. The Grandfather Passage is often used to gather a speech sample as it is a brief, phonetically balanced paragraph, containing most sounds in the American English language.13 The passage also provides a validated means of spontaneous, continuous speech assessment to give the SLP evaluators an accurate representation of patient speech.
Speech performance was evaluated via a combination of three analyses: (1) objective acoustic analysis via digital sonography, (2) semiobjective analysis by six SLPs, and (3) subjective analysis through patient questionnaire.
Objective Evaluation of Articulation Via Acoustic Analysis
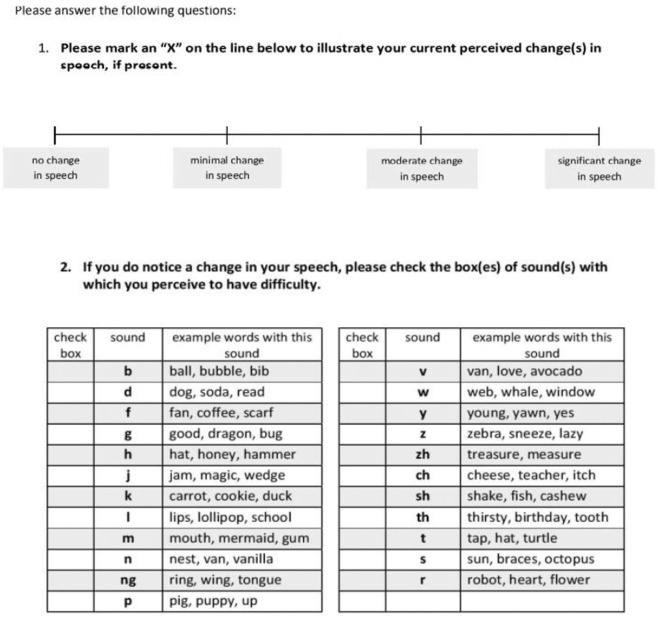
Recordings were uploaded to Praat Software (Version: 6.0.0, github.com/praat/praat, Amsterdam, The Netherlands), a speech analysis software program, to perform acoustic analysis of the /s/ sound in the word “several” via digital sonography (spectrography: recording of frequency, amplitude, and time of a speech signal).14 The /s/ sound was used because the lingua-alveolar fricative is sensitive to morphologic changes in the maxillary incisors and common in most languages globally.15 The word “several” was selected as it was the only word in the Grandfather Passage with an initial /s/ sound that was not a consonant blend, allowing for better isolation and representation of articulation. Wide band spectrography was used to analyze the upper boundary frequency (UBF ; the maximum frequency of the band width of the fricative) of the middle 50 ms of the /s/ sound. Within the spectrogram, the UBF is represented by the maximum grayness or the range of maximum frequency of the band width of the fricative sound (Figure 1).16 Evaluator reliability was validated by repeating each reading three times and averaging the values.
Figure 1.
Wide band spectrogram of the English word “several” spoken by a subject for evaluation of the isolated /s/ sound.
Semiobjective Speech Assessment by Speech Professionals
Audio recordings were uploaded to an encrypted server. The panel of six speech professionals was chosen based on willingness to participate and certification as an SLP. SLPs performed independent, blinded auditory evaluations on each recording by indicating alteration in speech production and speech intelligibility. Evaluator reliability was validated by repeating recordings of 10% of the sample. A 4-point Likert scale was used to evaluate alteration in speech production: 4 = severely altered speech production, 3 = moderately altered speech production, 2 = mildly altered speech production, and 1 = normal speech production. If the speech professionals indicated that they perceived an alteration in speech production, they were asked to provide commentary on specific sound productions altered and additional pertinent information. Speech intelligibility was also evaluated to determine comprehensibility of patient speech. This was indicated by a score of 0, indicating unintelligible speech, or 1, indicating intelligible speech.
Subjective Speech Evaluation by Patient Questionnaire
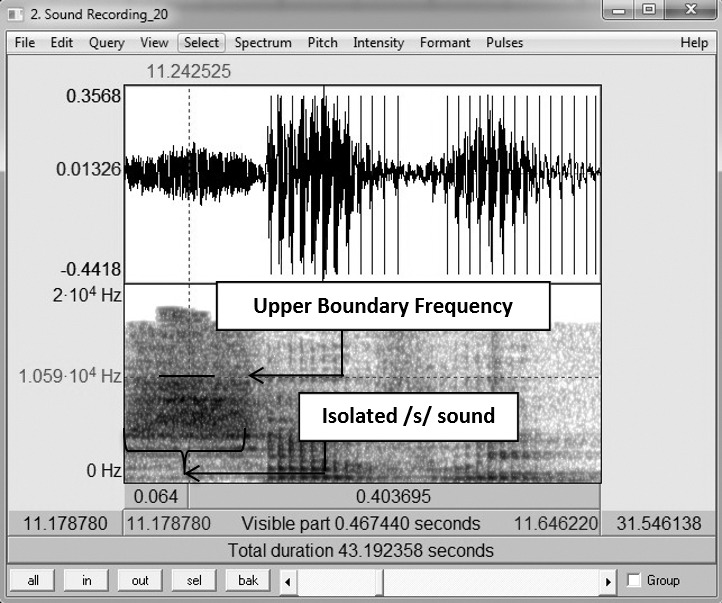
A standardized questionnaire (Figure 2) was given to the patient at each time point with the following questions:
Figure 2.
Patient questionnaire.
"Please mark an “X” on the line below to illustrate your current perceived change(s) in speech, if present."
A visual linear scale (100 mm) was provided with the following answer choices: no change in speech, minimal change in speech, moderate change in speech, and significant change in speech.
“If you do notice a change in your speech, please check the box(es) of sound(s) with which you perceive to have difficulty."
A table with all of the phonemes in the American English language, along with sample words for each, was provided for patients.
Statistical Analysis
Data were analyzed with IBM SPSS Statistics 24.0 statistical analysis software (SPSS Inc, Chicago, Ill). The null hypothesis was that there would be no significant difference between the groups. P was set at <.05 for significant changes. The sample size of 44 patients was certified for the UBF variable, which resulted in a standard deviation mean of 0.48 and 0.55 with averages of 11.52 and 11.48, for the Invisalign and Fixed groups, respectively, and with a maximum difference between the averages of 0.46. To verify the consistency of the sample size, a probability of 95% (P = .05) and a value of Zα/2 = 1.96 and Zβ = 0.84 were considered, resulting in a sample size of 19.7, which was equivalent to 20 patients for each group. Independent sample t-test and Mann-Whitney U-test were used to determine differences between groups at T0, T1, and T2. Due to sample sizes, sample distribution was assumed to be normal for both groups.
Paired t-test and Wilcoxon signed-rank test were used to compare changes among time points within each group. Equal variances were assumed based on Levene's test.
To assess the reliability of SLPs, 10% of the recordings (n = 13) were randomly selected to be evaluated a second time by each SLP panelist. High intraobserver reliability was tested with Cronbach's alpha. Interobserver reliability was assumed based on all speech professionals having SLP certification.
RESULTS
Objective Evaluation of Articulation Via Acoustic Analysis
At the evaluation time points, there were no significant differences in means between the Invisalign and Fixed groups in the articulation of the /s/ sound with respect to the mean UBF (Table 1). However, there was a statistically significant difference over time from T0 to T1 (P < .01), T1 to T2 (P = .01), and T0 to T2 (P = .02) for Invisalign patients (Table 2).
Table 1.
Descriptive Data and Independent Sample t-Tests From Objective, and Subjective Analysis of Invisalign and Fixed Groups at T0, T1, and T2 a,b
|
|
Invisalign Group (n = 24) |
Fixed Group (n = 20) |
P Value |
||||||
| Min |
Max |
Mean |
SD |
Min |
Max |
Mean |
SD |
||
| Upper boundary frequency (MHz) | |||||||||
| T0 | 10.72 | 12.73 | 11.68 | 0.46 | 10.37 | 12.38 | 11.55 | 0.55 | .42 |
| T1 | 10.37 | 12.21 | 11.36 | 0.50 | 10.37 | 12.12 | 11.44 | 0.55 | .64 |
| T2 | 10.55 | 12.3 | 11.53 | 0.48 | 10.37 | 12.3 | 11.45 | 0.56 | .62 |
| Patient perception of speech alteration (mm) | |||||||||
| T1 | 4.67 | 86.67 | 43.83 | 18.84 | 6.0 | 68.33 | 30.78 | 21.16 | .04* |
| T2 | 6.0 | 66.0 | 36.14 | 16.42 | 0 | 32.00 | 21.52 | 11.89 | <.01** |
Max indicates maximum; min, minimum; SD, standard deviation.
Speech alteration of all patients at T0 was used as baseline and therefore assumed to be 0.
Significant by the Student's t-test at P < .05.
Significant by the Student's t-test at P < .01.
Table 2.
Paired t-Tests From Objective and Subjective Analysis of Invisalign and Fixed Groups at T0, T1, and T2 a
|
|
Invisalign Group (n = 24) |
Fixed Group (n = 20) |
||||
| Mean |
SD |
P Value |
Mean |
SD |
P Value |
|
| Upper boundary frequency (MHz) | ||||||
| T0 × T1 | –0.31 | 0.37 | <.01** | –0.11 | 0.37 | .19 |
| T1 × T2 | 0.16 | 0.27 | .01* | 0.01 | 0.32 | .89 |
| T0 × T2 | –0.15 | 0.29 | .02* | –1.39 | 0.51 | .06 |
| Patient perception of speech alteration (mm) | ||||||
| T1 × T2 | 39.99 | 17.91 | .02* | 26.15 | 17.58 | 0.30 |
SD indicates standard deviation.
Significant by the Student's t-test at P < .05.
Significant by the Student's t-test at P < .01.
Semiobjective Speech Assessment by Speech Professionals
The mean rating showed significant increases to 1.58 (Invisalign group) and 1.39 (fixed group) at T1 (P = .02), indicating significant deterioration in articulation immediately after appliance delivery (Table 3). Mean ratings then decreased to 1.44 for the Invisalign and 1.23 for the fixed group at T2 (P < .01), suggesting a decrease in speech alteration from T1 and, thus, adaptation to the appliance. There was significant speech alteration from T0 to T1 (P < .01), T1 to T2 (P = .03), and T0 to T2 (P < .01) in the Invisalign group. However, there was significant speech alteration from T0 to T1 (P < .01) and T1 to T2 (P = .01) in the fixed group (Table 4). Overall, from before appliance delivery (T0) to 2 months with the appliance (T2), there was a significant increase in means for Invisalign patients, suggesting that, even though Invisalign patients showed signs of adaptation, overall they still had speech articulation errors 2 months after the start of treatment. Although the same general trend existed for the fixed group, the difference was not statistically significant when T0 and T2 were compared. These trends can be observed through the table of SLP evaluation of speech alteration (Table 5) and the bar graph depicting frequencies (Figures 3 and 4).
Table 3.
Mann-Whitney U-Test Results of SLP Analysis of Invisalign and Fixed Groups at T0, T1, and T2 a
|
|
Invisalign Group (n = 24) |
Fixed Group (n = 20) |
P Value |
||||||
| Min |
Max |
Mean |
SD |
Min |
Max |
Mean |
SD |
||
| T0 | 1 | 2 | 1.08 | 0.27 | 1 | 2 | 1.18 | 0.40 | .24 |
| T1 | 1 | 4 | 1.58 | 0.65 | 1 | 4 | 1.39 | 0.62 | .02** |
| T2 | 1 | 3 | 1.44 | 0.51 | 1 | 3 | 1.23 | 0.46 | <.01** |
Max indicates maximum; min, minimum; SD, standard deviation; SLP, speech and language pathologist.
Significant by the Student's t-test at P < .01.
Table 4.
Wilcoxon Signed-Rank Test Results of Speech and Language Pathologist Analysis of Speech Alteration of Invisalign and Fixed Groups at T0, T1, and T2
|
|
Invisalign Group (n = 24) |
Fixed Group (n=20) |
||
| z Value |
P Value |
z Value |
P Value |
|
| T0 × T1 | –6.6635 | <.01** | –3.6303 | <.01** |
| T1 × T2 | –2.1533 | .03* | –2.4569 | .01* |
| T0 × T2 | –5.9384 | <.01** | –1.4085 | .15 |
Significant by the Student's t-test at P < .05.
Significant by the Student's t-test at P < .01.
Table 5.
Frequency of Semiobjective Speech Assessment: Speech and Language Pathologist Evaluation of Speech Alteration of Invisalign and Fixed Groups at T0, T1, and T2
|
|
Invisalign Group (n = 24) |
Fixed Group (n = 20) |
||||
| T0 |
T1 |
T2 |
T0 |
T1 |
T2 |
|
| Speech alteration | ||||||
| Normal | 91.7 | 50.7 | 56.3 | 83.3 | 67.5 | 78.3 |
| Mildly altered | 8.3 | 41.7 | 43.1 | 15.8 | 26.7 | 20.0 |
| Moderately altered | 0 | 6.9 | 0.7 | 0.8 | 5.0 | 1.7 |
| Severely altered | 0 | 0.7 | 0 | 0 | 0.8 | 0 |
| Speech intelligibility | ||||||
| Intelligible | 100 | 100 | 100 | 100 | 100 | 100 |
| Unintelligible | 0 | 0 | 0 | 0 | 0 | 0 |
Figure 3.
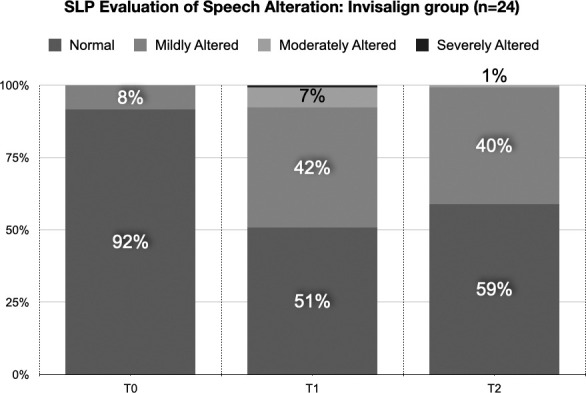
SLP evaluation of speech production of Invisalign group over time.
Figure 4.
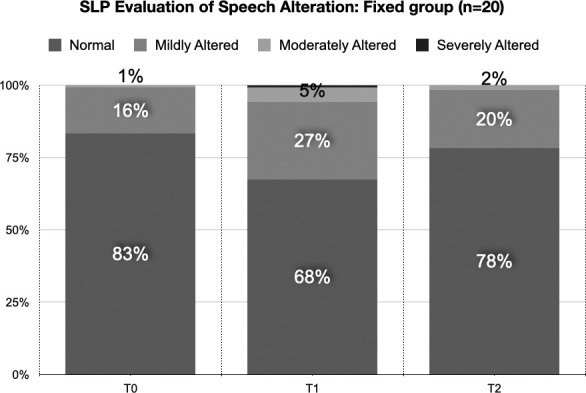
SLP evaluation of speech production of Fixed group over time.
Subjective Speech Evaluation by Patient Questionnaire
Speech alteration of all patients at T0 was used as the baseline and, therefore, assumed to be 0. At T1, Invisalign patients reported sentiments on their speech alteration with a mean rating of 43.83 (corresponding to a moderate change in speech) compared with the fixed group of 30.78 (indicating a minimal change in speech). At T2, mean ratings decreased to 36.14 (minimal to moderate change in speech) for Invisalign and 21.52 (no change to minimal change in speech) for the fixed group. There was a significant difference between means of Invisalign and fixed group patient perceptions at both T1 and T2 (T1: P = .04; T2: P < .01) (Table 1). From T1 to T2, patients on average reported a decrease in speech alteration severity; however, the difference between T1 and T2 for both groups was not statistically significant, indicating that, although patients perceived adaptation or improvement in their speech, it was not statistically significant (Table 2). The sounds reported most frequently by patients as being affected were /s,z,zh,sh,th,ch/ in the Invisalign group and /s,th,f/ in the fixed group (Table 6).
Table 6.
Frequency (%) of Perceived Affected Sounds Reported by Patients on Questionnaire (Subjective Analysis)
|
|
Invisalign Group (n = 24) |
Fixed Group (n = 20) |
||
| T1 |
T2 |
T1 |
T2 |
|
| /s/ | 79.17 | 79.17 | 60 | 30 |
| /z/ | 45.83 | 50 | 10 | 5 |
| /zh/ | 45.83 | 37.50 | 15 | 25 |
| /sh/ | 41.67 | 45.83 | 15 | 20 |
| /th/ | 41.67 | 45.83 | 30 | 25 |
| /ch/ | 25.00 | 37.50 | 15 | 15 |
| /b/ | 16.67 | 0 | 0 | 0 |
| /j/ | 16.67 | 20.83 | 0 | 0 |
| /d/ | 12.50 | 12.50 | 0 | 5 |
| /n/ | 12.50 | 4.17 | 5 | 0 |
| /v/ | 12.50 | 0 | 10 | 10 |
| /l/ | 8.33 | 25.00 | 15 | 5 |
| /t/ | 8.33 | 8.33 | 5 | 0 |
| /w/ | 8.33 | 4.17 | 5 | 10 |
| /r/ | 8.33 | 4.17 | 5 | 0 |
| /m/ | 8.33 | 0 | 10 | 5 |
| /ng/ | 8.33 | 0 | 0 | 10 |
| /f/ | 4.17 | 8.33 | 30 | 15 |
| /g/ | 4.17 | 8.33 | 0 | 0 |
| /y/ | 4.17 | 4.17 | 0 | 5 |
| /k/ | 4.17 | 0 | 0 | 0 |
| /p/ | 4.17 | 0 | 5 | 0 |
| /h/ | 0 | 0 | 0 | 5 |
DISCUSSION
For the Invisalign group, the objective analysis demonstrated that there was a significant alteration in speech immediately after delivery of the aligners, and, though some speech recovery occurred over time, there was still significant speech alteration from the appliance compared with baseline (Table 2). This speech change noted over time from T0 to T2 was shown by a significant drop in the mean UBF (Table 2). A comparison with the literature showed a similar reduction in the UBF of the fricative /s/ sound in patients undergoing orthodontic treatment with lingual appliances.15 This similarity suggested that both aligners and lingual appliances created a similar pathomechanism to alter speech as the contact area of the tongue shifts based on the presence of an appliance on the lingual surface.
According to the SLP panel evaluation, there was significant speech alteration between T0 and T1 and between T1 and T2 in both the Invisalign and fixed groups. This suggested that speech professionals observed a significant change in speech immediately after appliance delivery but that there was also significant recovery over time. Overall, from before appliance delivery to 2 months with the appliance (T0 to T2), there was a significant increase in means for Invisalign patients (P < .01), suggesting that, even though patients showed adaptation, overall, they still had speech articulation errors 2 months after the start of treatment. Although the same general trend existed for the fixed group from T0 to T2, the difference was not statistically significant (Table 3).
SLPs were asked to list specific sound productions altered, if any, along with important comments. Most comments were associated with patients in the Invisalign group. The most frequent comment among all Invisalign® patients was a “lisp.” Specifically, the panel overwhelmingly identified the /s,z,zh,sh,th,ch/ sounds as those that were primarily distorted by Invisalign and the /s,th,f/ sounds as those primarily distorted by fixed labial appliances. Speech of the Invisalign group was often described as “slushy” and “distorted,” and that it seemed like patients spoke at a “slowed rate.” Additionally, “breaking of the consonant air flow” was frequently noted for Invisalign patients by SLPs. This concept was also demonstrated in a study with lingual brackets, as the tongue tip encountered an unfamiliar appliance.17
Previous studies found similar results but were limited based on study design. Some limitations included only performing subjective10 or semiobjective analyses,11 having shorter follow-up times,11 evaluating a different language,10 and using lingual braces as the control group10 rather than labial braces.
The use of three different methods of speech evaluation in the current study ensured the reliability of the results by largely dismissing bias that could result from patient- or investigator-related misinterpretation. In this way, the objective sonography method allowed verification that the speech changes observed/reported with the other methods were not simply opinion based. In addition, the following factors contributed to the validity of this study: (1) By selecting a passage that included every sound in the American English language (the Grandfather Passage), all sounds were included in the analysis by SLPs and patients; (2) the passage also provided a validated means of spontaneous, continuous speech assessment for a more accurate representation of actual speech versus isolated words in a list; (3) unlike other studies with shorter follow-up times (1 day),11 this study performed an evaluation at a follow-up of 2 months (T2), providing a better representation of patient speech adaptation over time; and (4) a linear visual analog scale was used in the patient questionnaire to allow open-ended responses.
However, there were some limitations in the current study. First, a convenience sample was obtained. Patients were selected by their willingness to participate along with meeting the inclusion criteria; selection was not random. Second, patient compliance with aligners and duration of daily wear may have affected speech adaptation but was not taken into account. Third, the linear/ruler set-up of the patient questionnaire response, along with the categorical nature and the order of answers, may have cognitively influenced how the patient answered the questions. Similarly, the questionnaire for the speech professionals was limited as it included categorical answer choices. Fourth, the objective analysis selective evaluation of the /s/ sound limited the extent to which the findings could be generalized. Although the /s/ sound was chosen based on a variety of factors, including it being a lingua-alveolar fricative, sensitive to morphologic changes in the maxillary incisors and common in most languages globally,15 it was not representative of all speech. Additionally, the 2 month period used in this study may not have been sufficient to show the full extent of speech adaptation. Further study is needed to evaluate for a longer period of time.
CONCLUSIONS
Invisalign clear aligner orthodontic treatment significantly affects speech and, although patients experience some level of adaptation, speech does not return to baseline after 2 months of treatment.
REFERENCES
- 1.Rosvall MD, Fields HW, Ziuchkovski J, Rosenstiel SF, Johnston WM. Attractiveness, acceptability, and value of orthodontic appliances. Am J Orthod Dentofacial Orthop . 2009;135:276.e1–76.e12. doi: 10.1016/j.ajodo.2008.09.020. [DOI] [PubMed] [Google Scholar]
- 2.Lew KK. Attitudes and perceptions of adults towards orthodontic treatment in an Asian community. Community Dent Oral Epidemiol . 1993;21:31–35. doi: 10.1111/j.1600-0528.1993.tb00715.x. [DOI] [PubMed] [Google Scholar]
- 3.Gorman J. Treatment of adults with lingual orthodontic appliances. Dent Clin North Am . 1988;32:589–620. [PubMed] [Google Scholar]
- 4.Poon KC, Taverne AA. Lingual orthodontics: a review of its history. Aust Orthod J . 1998;15:101–104. [PubMed] [Google Scholar]
- 5.Hohoff A, Stamm T, Kühne N, et al. Effects of a mechanical interdental cleaning device on oral hygiene in patients with lingual brackets. Angle Orthod . 2003;73:579–587. doi: 10.1043/0003-3219(2003)073<0579:EOAMIC>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 6.Phan X, Ling PH. Clinical limitations of Invisalign. J Can Dent Assoc . 2007;73:263–266. [PubMed] [Google Scholar]
- 7.Auluck A. Lingual orthodontic treatment: what is the current evidence base? J Orthod . 2013;40(supp1):s27–s33. doi: 10.1179/1465313313Y.0000000073. [DOI] [PubMed] [Google Scholar]
- 8.Crystal D. A Little Book of Language. UNS New Haven, CT: Yale University Press; 2010. [Google Scholar]
- 9.Doll GM, Zentner A, Klages U, Sergl HG. Relationship between patient discomfort, appliance acceptance and compliance in orthodontic therapy. J Orofac Orthop . 2000;61:398–413. doi: 10.1007/pl00001908. [DOI] [PubMed] [Google Scholar]
- 10.Nedwed V, Miethke R-R. Motivation, acceptance and problems of Invisalign patients. J Orofac Orthop . 2005;66:162–173. doi: 10.1007/s00056-005-0429-0. [DOI] [PubMed] [Google Scholar]
- 11.Arreghini A, Beretta A, Lombardo L, Almoni C, Siciliani G. Assessment of phonetic alterations in patients treated with F22 aligners. J Aligner Orthod . 2018;2:21–29. [Google Scholar]
- 12.Pogal-Sussman-Gandia CB, Tabbaa S, Al-Jewair T. Effects of Invisalign® treatment on speech articulation. Int Orthod . 2019;17:513–518. doi: 10.1016/j.ortho.2019.06.011. [DOI] [PubMed] [Google Scholar]
- 13.Ogar J, Willock S, Baldo J, et al. Clinical and anatomical correlates of apraxia of speech. Brain Lang . 2006;97:343–350. doi: 10.1016/j.bandl.2006.01.008. [DOI] [PubMed] [Google Scholar]
- 14.Hohoff A, Seifert E, Ehmer U, Lamprecht-Dinnesen A. Articulation in children with Down's syndrome. J Orofac Orthop . 1998;59:220–228. doi: 10.1007/BF01579166. [DOI] [PubMed] [Google Scholar]
- 15.Runte C, Lawerino M, Dirksen D, et al. The influence of maxillary central incisor position in complete dentures on/s/sound production. J Prosthet Dent . 2001;85:485–495. doi: 10.1067/mpr.2001.114448. [DOI] [PubMed] [Google Scholar]
- 16.Hohoff A, Seifert E, Fillion D, Stamm T, Heinecke A, Ehmer U. Speech performance in lingual orthodontic patients measured by sonography and auditory analysis. Am J Orthod Dentofacial Orthop . 2003;123:146–152. doi: 10.1067/mod.2003.12. [DOI] [PubMed] [Google Scholar]
- 17.Sinclair P, Cannito M, Goates L, Solomos L, Alexander C. Patient responses to lingual appliances. J Clin Orthod . 1986;20:396. [PubMed] [Google Scholar]