Abstract
OBJECTIVES
Our goal was to examine post hoc patient satisfaction and the decision-making process of choosing a prosthesis for aortic valve replacement (AVR).
METHODS
We surveyed 113 patients who were operated on for AVR at 60–70 years of age, including 74 patients with a mechanical valve (MECH) and 39 with a bioprosthesis (BIO). The study focused on quality of life and the decision pathway in relation to prosthesis choice and valve-related complications. Decisional conflict was defined as the post hoc uncertainty perceived by patients regarding their choice of prosthesis.
RESULTS
The survey was performed at a median of 5.2 (3.2–8.1) years after the AVR. Patients with a biological valve were older (BIO: 68.4 years [66.2–69.4] vs MECH: 63.9 [61.9–66.7]; P < 0.001). Global post hoc satisfaction with prosthesis choice was high in both groups (MECH: 95.9%; BIO: 100%), and 85.1% (MECH) and 92.3% (BIO) of them would repeat their choice. Conflict about their decision was equal (MECH: 30.3%; BIO: 32.6%) for different reasons: MECH patients experienced more anticoagulation-related inconvenience (25.9% vs 0%), fear of bleeding (31.1% vs 0%) and prosthesis noise (26.2% vs 0%), whereas more BIO patients feared prosthesis failure (39.7% vs 17.4%) or reoperation (43.5% vs 18.1%). Active involvement in the decision (odds ratio 0.37, 95% confidence interval 0.16–0.85; P = 0.029) and adequate information about the prosthesis (odds ratio 0.34, 95% confidence interval 0.14–0.86; P = 0.020) decreased the risk of conflict about the decision.
CONCLUSIONS
Although 30% of the responders showed a decisional conflict related to prosthesis-specific interferences, global patient satisfaction with the prosthesis choice for AVR is excellent. Increasing the patient’s involvement in the prosthesis choice through shared accountability and improved information is recommended to decrease the choice-related uncertainty.
Keywords: Valve prosthesis, Aortic valve replacement, Shared decision-making, Quality of life
INTRODUCTION
In absence of the ‘ideal’ heart valve prosthesis, the optimal choice of valve substitute in patients requiring aortic valve replacement (AVR) remains debateable. Mechanical valves are designed to last a lifetime but necessitate the ad vitam intake of oral anticoagulants, so the patient must balance the risk of bleeding or thromboembolic complications due to the limits of the therapeutic regime. Biological valves interfere less with activities of daily life but are prone to structural deterioration over time, inevitably resulting in the need for reoperation in younger patients.
The age of the patient at the time of the AVR has long been considered the principal determinant to guide the choice of prosthesis. The current American Heart Association/American College of Cardiology guidelines propose a mechanical valve as a reasonable option for patients <60 years of age and a biological valve for patients older than 70 years, whereas both types of valves are seen as equivalent alternatives for patients between 60 and 70 years [1]. The European Society of Cardiology statements are in accordance but recommend a bioprosthesis for patients from the age of 65 years [2]. Because several studies reported a lack of survival difference between both types of prostheses, even regardless of lowering the age for the use of biological valves, other features more closely related to quality of life (QoL) and individual patient preferences have been integrated into the decision process for the choice of valve prosthesis [3–5]. Hence, the efficacy of a shared decision-making includes in-depth awareness of the advantages and disadvantages of mechanical and biological valves to increase the participation of the individual patient. In a recent multicentre randomized trial, Korteland et al. [6] investigated the usefulness of an online decision-aid platform to support the valve choice selection process and found that such an additional tool did not alleviate the chance for later decisional conflict, despite improving the informed status and thereby the mental well-being of the individual patient.
The goal of this single-centre study was to evaluate post hoc the decision-making process for choice of valve in patients for whom the outcome of a biological or mechanical prosthesis is expected to be equivocal and therefore are thought to be actively involved in the decision process at the time of the AVR. In addition to the registration of purely medical outcome data, QoL issues and the presence of an eventual decisional conflict regarding prosthesis choice are determined via a survey designed to compare the experiences of patient subgroups with biological and mechanical valve prostheses, respectively.
PATIENTS AND METHODS
All patients who underwent AVR at the age of 60–70 years between January 2007 and December 2017 were eligible for inclusion in this study. Patients undergoing mitral valve replacement or AVR simultaneously with a valve substitute other than a biological or mechanical prosthesis were excluded. After excluding the deceased patients, 260 patients were contacted by phone. Only 123 (47.3%) patients were willing to participate and signed a written informed consent. To reduce the survey response bias, patients whose choice of prosthesis was eventually influenced by the prior intake of anticoagulants (n = 6) or the presence of a contraindication for lifelong anticoagulation (n = 4) were also excluded from analysis, restricting the final study cohort to 113 patients. The study was approved by the ethical committee of the University Hospital of Ghent (trial number 2018/1043) and registered as B670201837230.
Patient and follow-up data
Demographic and operative data were retrieved from electronic medical records. Follow-up data were gathered from the files of referring cardiologists, with specific focus on the occurrence of valve- and/or anticoagulation-related events. These data were verified at the time of phone contact. Reoperation was noted only if it was for aortic prosthesis-related issues. The follow-up end date was set at September 2019.
Survey data
The survey was designed to evaluate 3 areas: (i) actual health- and valve-related QoL status, (ii) role of the patient-physician relationship in the choice of prosthesis and (iii) post hoc personal assessment of the decision-making process and the perception of decisional conflict interference.
Health quality was assessed by a 36-item short survey, including 8 conditions such as physical and mental health status, social functioning including limitations due to physical/mental dysfunction, vitality, pain and general perception and modifications of personal health status. Assessment was based on the answers to multiple choice questions that were scored on a Likert scale from 1 to 5, where 1 represented bad and 5 represented excellent. The scores were then migrated to a 0–100 scale and collected per item of health well-being. The valve-specific QoL investigation included questions on interferences with the activities of daily life related to the prosthesis itself like noise, regular blood sampling for control of the international normalized ratio and anxiety status regarding specific valve-related complications such as thromboembolism, bleeding and valve failure with the need for reintervention. Only questions completed with a valid answer were included in the analysis.
Decisional conflict as defined by Leblanc et al. [7] reflects the actual personal uncertainty or regret about a definitive choice made between concurrent options. In this study, decisional conflict was confirmed for any post hoc negative perception made by the individual patient that put the original prosthesis choice in doubt. For patients who had a mechanical valve, an additional question asked whether they would have chosen a biological AVR if a reoperation for structural degeneration was amenable to a transcatheter valve implant (TAVI).
Statistical analyses
Normal distribution of continuous data was verified with the Shapiro-Wilk test and shown graphically by a Q–Q plot. Continuous data with normal distribution are expressed by mean value and standard deviation; non-normally distributed data are given as median and interquartile range. Categorical data are expressed by number and percentage. Baseline characteristics of patients with a biological (BIO) or a mechanical (MECH) prosthesis are compared with an unpaired t-test or the Mann–Whitney U-test for continuous variables and with the Fisher exact test for categorical variables. Analysis of valve-related events was based on the Kaplan–Meier product-estimation method, with log-rank analysis for between-group comparisons. To anticipate the potential confounding for differences between populations and/or choice of prosthesis type, data on survey responses are only reported by the descriptive values.
Predictive factors for decisional conflict were analysed by univariable logistic regression analysis and expressed by the odds ratio (OR) and 95% confidence intervals (CIs). Factors achieving a P-value of <0.2 on univariable analysis were entered into a multivariable logistic regression model. Statistical significance was considered for a two-sided P-value <0.05. All statistical tests were performed with SPSS version 25 (IBM corp., Armonk, NY USA).
RESULTS
Patient data
Of the 113 participants, 39 (34.5%) had a biological valve and 74 (65.5%) had a mechanical prosthesis. Patients with a biological prosthesis were older at the time of AVR, with only 12.8% of the patients <65 years compared to 62.2% in the mechanical group (P < 0.001). Various associated diseases were noted, yielding at least 1 comorbidity in 81 (71.7%) patients (biological: 30 [76.9%]—mechanical: 51 [8.9%]; P = 0.268). The majority of patients had AVR for primary aortic valve stenosis (n = 92, 81.4%). All patients and operating characteristics are listed in Table 1.
Table 1:
Patient and operative data
| All patients | Biological prosthesis | Mechanical prosthesis | P-value | |
|---|---|---|---|---|
| Number | 113 | 39 | 74 | |
| Age (years), median (IQR) | 65.7 (62.7–68.4) | 68.4 (66.2–69.4) | 63.9 (61.9–66.7) | <0.001 |
| Gender, male, n (%) | 83 (73.5) | 30 (76.9) | 53 (61.7) | 0.656 |
| Comorbidities, n (%) | ||||
| Coronary artery disease | 46 (40.7) | 19 (48.7) | 27 (36.5) | 0.232 |
| Congestive heart failure | 6 (5.4) | 3 (7.9) | 3 (4.1) | 0.410 |
| Chronic atrial fibrillation | 15 (13.3) | 4 (10.3) | 11 (14.8) | 0.492 |
| Peripheral vascular disease | 3 (2.7) | 0 (0.0) | 3 (4.1) | 0.549 |
| Cerebrovascular disease | 7 (6.4) | 2 (5.3) | 5 (7.0) | 1.000 |
| Liver disease | 4 (5.0) | 2 (7.7) | 2 (3.7) | 0.507 |
| Chronic renal failure | 7 (6.3) | 5 (14.2) | 2 (2.7) | 0.054 |
| Chronic obstructive lung disease | 5 (4.6) | 2 (5.4) | 3 (4.2) | 1.000 |
| Diabetes mellitus | 18 (18.8) | 8 (23.5) | 10 (16.1) | 0.419 |
| Arterial hypertension | 70 (66.0) | 21 (60.0) | 49 (69.0) | 0.389 |
| Indication for AVR | 0.164 | |||
| Degenerative disease | 64 (57.7) | 23 (62.2) | 41 (55.4) | |
| Endocarditis | 8 (7.2) | 4 (10.8) | 4 (5.4) | |
| Bicuspid disease | 38 (34.2) | 9 (24.3) | 29 (29.2) | |
| Rheumatic disease | 2 (1.8) | – | 2 (2.7) | |
| Marfan disease | 1 (0.9) | 1 (2.7) | – | |
| Prior cardiac surgery | 18 (16.1) | 7 (18.4) | 11 (14.9) | 0.786 |
| Associated procedure | 47 (41.6) | 15 (38.5) | 32 (43.2) | 0.417 |
| CABG | 39 (36.4) | 15 (39.5) | 24 (34.8) | |
| MV repair | 3 (2.8) | – | 3 (4.3) | |
| TV repair | 1 (0.9) | – | 1 (1.4) | |
| Ascending aorta replacement | 4 (3.7) | – | 4 (5.8) | |
AVR: aortic valve replacement; CABG: coronary artery bypass grafting; IQR: interquartile range; MV: mitral valve; TV: tricuspid valve.
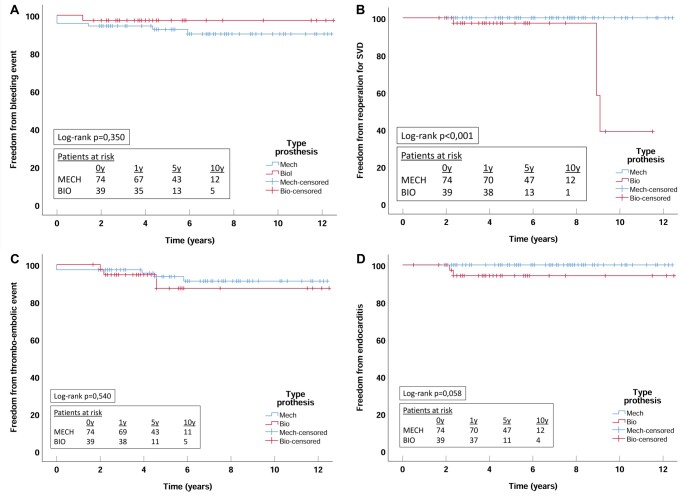
Prosthesis-related events
The median time between AVR and the survey was 5.2 (3.2–8.1) years and was significantly shorter for patients with biological valves compared to those with a mechanical prosthesis (BIO 3.9 years [2.6–5.5]; MECH 6.2 years [4.1–8.2]; P = 0.003). Within this follow-up period, at least 1 valve-related event each was observed in 19 (16.8%) patients, including thromboembolism with transient neurological injury (BIO n = 3 [7.7%]; MECH n = 5 [7.0%]), clinically relevant bleeding (BIO n = 1 [2.8%]; MECH n = 6 [8.6%]), endocarditis (BIO n = 2 [5.1%]; MECH n = 0) and reoperation for structural prosthesis degeneration (BIO n = 4 [10.3%]; MECH n = 0). The time-dependent freedom from valve- and/or anticoagulation-related complications as shown by the Kaplan–Meier plots (Fig. 1A–D) revealed a significant difference for structural degeneration only in patients with a bioprosthesis (log-rank P < 0.001), all of whom underwent successful surgical redo AVR. Because 1 patient with endocarditis of a biological valve was reoperated on, the freedom from aortic valve-related reoperation was significantly lower in the BIO group (log-rank P < 0.001; Fig. 2).
Figure 1:
Kaplan–Meier plots of valve-related events. (A) Freedom from bleeding. (B) Freedom from reoperation for structural valve deterioration. (C) Freedom from thromboembolic event. (D) Freedom from endocarditis. BIO: bioprosthesis; MECH: mechanical valve; y: year; SVD: structural valve deterioration.
Figure 2:
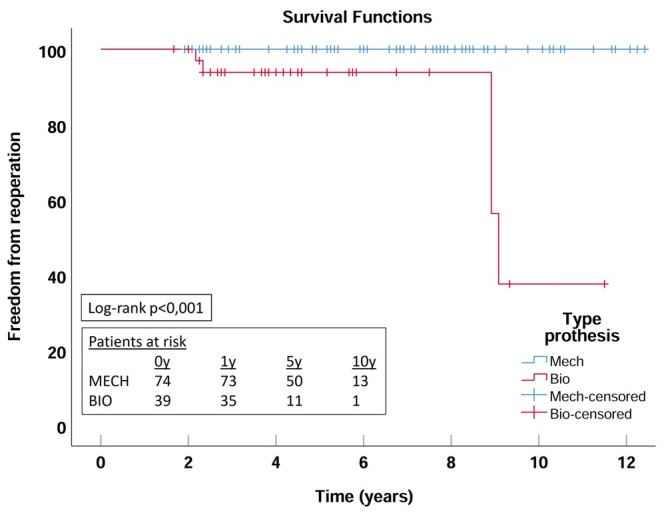
Kaplan–Meier plot of aortic valve-related reoperation. BIO: bioprosthesis; MECH: mechanical valve; y: year.
QoL evaluation
The median age at the time of the survey was 71.9 years (70.4–73.6) for patients in the BIO group and 70.8 years (67.1–73.6) for the patients in the MECH group (P = 0.083). The overall health status was estimated as good to excellent, more frequently in the MECH than in the BIO group (75.3% vs 57.5%) and was associated with a better mental health perception in the MECH group. The mental health score corresponding to good/excellent was 90.4% in MECH group but by only 77.1% in the BIO group. QoL data are listed in Table 2. Valve-specific interference with QoL was observed in both populations, yielding mainly features related to anticoagulation drug intake and the eventual risk of bleeding events in the MECH group and anxiety for future prosthesis failure and eventual reoperation in the BIO group (Table 3).
Table 2:
Quality of life survey results
| All patients (n = 113) | Biological prosthesis (n = 39) | Mechanical prosthesis (n = 74) | |
|---|---|---|---|
| Physical scale | |||
| Physical functioning | 89 (72–100) | 82 (55–100) | 90 (65–100) |
| Social functioning | 100 (90–100) | 100 (90–100) | 100 |
| Role limitations (physical) | 90 (65–100) | 69 (30-100) | 100 (65–100) |
| Mental scale | |||
| Mental well-being | 91 (73–100) | 88 (62–100) | 93 (78–100) |
| Vitality | 89 (71–100) | 77 (57–95) | 89 (67–100) |
| Body pain | 100 (74–100) | 100 (82–100) | 100 (64–100) |
| General health | 81 (51–96) | 75 (54–98) | 81 (47–96) |
| Anxiety, depression | 75 (50–97) | 50 (24–74) | 75 (49–94) |
Data are represented by median (interquartile range).
Table 3:
Valve-specific interference with quality of life
| All patients (n = 113) | Biological prosthesis (n = 39) | Mechanical prosthesis (n = 74) | |
|---|---|---|---|
| Are you afraid of prosthesis failure? | |||
| No | 90 (79.6) | 26 (60.6) | 64 (86.3) |
| Yes | 23 (20.4) | 13 (39.4) | 10 (13.7) |
| Are you afraid of a need for valve reoperation? | |||
| No | 82 (72.6) | 22 (56.4) | 68 (81.1) |
| Yes | 31 (27.4) | 17 (43.6) | 14 (18.9) |
| Are you afraid of valve-related complications? | |||
| No | 90 (79.6) | 31 (79.5) | 59 (79.7) |
| Yes | 23 (20.4) | 8 (20.5) | 15 (20.3) |
| Are you afraid of eventual bleeding complications due to anticoagulant medication? | |||
| No | – | NA | 57 (77.0) |
| Yes | – | NA | 17 (23.0) |
| Are the regular blood samplings and medical visits disturbing? | |||
| No | – | NA | 60 (81.1) |
| Yes | – | NA | 14 (18.9) |
| Is the valve noise disturbing? | |||
| No | – | NA | 56 (75.6) |
| Yes | – | NA | 18 (24.3) |
Data are represented by n (%).
NA: not applicable.
Results of decision-making process for valve choice
The majority of patients in both groups mentioned that the final decision on valve choice was made by the physician; however, the choice was usually made with the agreement of the patient him- or herself (Table 4).
Table 4:
Patient involvement in the decision-making process of valve choice
| All patients (n = 113) | Biological valve (n = 39) | Mechanical valve (n = 74) | |
|---|---|---|---|
| Are you aware of different kinds of valve prostheses? | |||
| No | 10 (8.8) | 3 (7.6) | 7 (9.5) |
| Yes | 103 (91.2) | 36 (92.3) | 67 (90.5) |
| Do you know the advantages and disadvantages of valve prosthesis? | |||
| No | 32 (28.3) | 13 (33.3) | 19 (25.7) |
| Yes but insufficiently | 9 (8.0) | 4 (10.3) | 5 (6.8) |
| Yes | 72 (63.7) | 22 (56.4) | 50 (67.7) |
| Have you been involved in the prosthesis choice by your physician? | |||
| No | 45 (39.8) | 13 (33.4) | 32 (43.2) |
| Yes but insufficiently | 13 (11.5) | 4 (10.2) | 9 (12.2) |
| Yes | 55 (48.7) | 22 (56.4) | 33 (44.6) |
| Did you had enough information to support your valve choice? | |||
| No | 11 (9.8) | 4 (10.3) | 7 (9.4) |
| Yes but insufficiently | 12 (10.6) | 4 (10.3) | 8 (10.8) |
| Yes | 90 (79.6) | 31 (79.4) | 59 (79.8) |
| Has the information on the kind of valve been given appropriately? | |||
| No | 21 (18.6) | 8 (20.5) | 13 (17.6) |
| Yes | 92 (81.4) | 31 (79.5) | 61 (82.4) |
| Do you find it important to be involved in the valve choice? | |||
| No | 20 (17.7) | 5 (12.8) | 15 (20.3) |
| Not really | 38 (33.6) | 15 (38.5) | 23 (31.1) |
| Yes | 55 (48.7) | 19 (48.7) | 36(48.6) |
| Who should make the choice of valve prosthesis? | |||
| Only the patient | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Mainly the patient | 1 (0.9) | 1 (2.6) | 0 (0.0) |
| Both physician and patient | 40 (35.4) | 12 (30.8) | 28 (37.8) |
| Mainly the physician | 33 (29.1) | 15 (38.4) | 17 (23.0) |
| Only the physician | 40 (35.4) | 11 (28.2) | 29 (39.2) |
| Was the decision of valve choice made by the physician, followed by your agreement? | |||
| No | 10 (8.8) | 2 (5.1) | 8 (10.8) |
| Yes | 103 (91.2) | 37 (94.9) | 66 (89.2) |
| Are you satisfied with your actual valve prosthesis? | |||
| No | 3 (2.7) | 0 (0.0) | 3 (4.1) |
| Yes | 110 (97.3) | 39 (100.0) | 71 (95.9) |
| Would you choose the same valve again? | |||
| No | 15 (13.3) | 3 (7.6) | 11 (14.9) |
| Yes | 98 (86.7) | 36 (92.3) | 63 (85.1) |
Data are given by n (%).
In general, 97.3% of the patients were satisfied post hoc with the choice of prosthesis, and 86.7% said they would make the same choice again, regardless of the prosthesis type. There were no differences in patient information status or decision involvement between both types of valve choices. Patient satisfaction was altered by the occurrence of valve-related events in 2 out of the 10 patients in the BIO group, i.e. in 2 patients requiring reoperation for structural valve deterioration. In the MECH group, all patients who experienced a valve-specific complication confirmed their original choice. However, 3 patients in the MECH group pointed to another prosthesis choice unrelated to any valve-related event, mainly for reasons of interference with QoL.
When considering patient involvement in the decision-making process, 79.6% of the entire cohort confirmed that they felt they were well-informed about the specific features that supported their choice (MECH: 79.8%; BIO: 79.4%). The availability of a digital information platform to guide the valve choice before AVR was felt to be helpful by 29.4% of the study cohort (MECH: n = 22, 29.7%; BIO: n = 10, 25.6%). Only half of the patients confirmed the absolute importance of being personally involved in the decision-making process (MECH: 48.6%; BIO: 48.7%). Patients in the MECH group were asked whether having the additional knowledge that structural failure of a bioprosthesis may be treatable by TAVI affected their post hoc decision. Fourteen patients (18.8%) agreed that they would prefer a biological prosthesis, whereas 58 (78.4%) patients confirmed their original choice of a mechanical valve. Twelve (16.2%) patients were not able to give a definitive answer.
Decisional conflict
Equal numbers in both groups said they had a decisional conflict (MECH: 30.3%; BIO: 32.6%) but for different reasons. This conflict was frequently related to prosthesis-specific issues: fear that the prosthesis would fail (BIO: 39.7%; MECH: 17.4%) and of eventual reoperation (BIO: 43.5%; MECH: 18.1%) in the BIO group, whereas fear of bleeding problems (MECH: 31.1%; BIO: 0%), regular blood sampling and medical visits (MECH: 25.9%; BIO: 0%) and valve noise (MECH: 26.2%; BIO: 0%) were common reasons in the MECH group.
Univariable analysis of predictive risk factors for decisional conflict demonstrated that active involvement in the decision process (OR 0.37, 95% CI 0.16–0.85; P = 0.029) and providing sufficient prosthesis information to the patient (OR 0.34, 95% CI 0.14–0.86; P = 0.020) decreased the risk of decisional conflict (Table 5). No independent predictors were retained in the multivariable analysis.
Table 5:
Risk factor analysis of decisional conflict by logistic regression analysis
| Risk factors | Univariable analysis |
Multivariable analysis |
||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P-value | OR | 95% CI | P-value | |
| Type of prosthesis (BIO versus MECH) | 1.16 | 0.53–2.35 | 0.707 | |||
| Age at surgery | 0.99 | 0.89–1.13 | 0.920 | |||
| Follow-up duration | 1.02 | 0.81–1.16 | 0.953 | |||
| Age at survey | 1.01 | 0.92–1.10 | 0.903 | |||
| Involvement in prosthesis choice | 0.37 | 0.16–0.85 | 0.029 | 0.94 | 0.05–19.17 | 0.709 |
| Informative status on prosthesis choice | 0.34 | 0.14–0.86 | 0.020 | 0.99 | 0.04–7.82 | 0.275 |
| Valve-related event | 1.38 | 0.51–3.70 | 0.527 | |||
OR: odds ratio; CI: confidence interval; BIO: bioprosthesis; MECH: mechanical valve.
DISCUSSION
This survey on the decisional pathway for prosthesis choice in patients at an age when biological or mechanical valve substitutes are proposed as equivalent options for AVR demonstrated that >90% were finally satisfied with the chosen prosthesis, regardless of any interference from valve-specific features or clinical events. The perception of the overall QoL was good to excellent in most patients, yet it was estimated at a lower level in patients with a biological valve. Specifically, features such as physical health, vitality and emotional perception of anxiety were less well perceived in patients with a biological prosthesis; however, these patients were generally older. It is conceivable that in this older population, health complaints other than cardiac-related issues dominated their overall well-being when they took the survey. Korteland et al. [8] found that the perception of physical health after AVR was certainly inferior compared to that of the general population, but the perception of mental health appeared to be superior. This paradox was explained by a shift in internal standards that can be experienced after a life-threatening event such as cardiac surgery. Otherwise, Kottmaier et al. noticed the same QoL in patients with mechanical or biological AVR. Hence, anxiety and avoidance behaviours were more frequently observed in patients with a mechanical valve, promoted by factors that constantly affect daily life, such as valve sounds and anticoagulation checks. The fact that these events were equally experienced by the patients’ partners strengthened the adverse impact of these emotions [9]. Approximately one-fourth to one-fifth of the patients worried about valve-specific interferences with one’s QoL. The negative perception in patients with a mechanical prosthesis of valve noise, of disturbance from regular anticoagulation-related blood samplings and medical visits, as well as the fear of structural failure in patients with biological valves is notably higher in our study than in the series of Korteland et al. [8]. Interestingly, 14–18% of the patients with a mechanical prosthesis admitted being afraid of valve failure and of the subsequent need for reoperation. One assumes that this deviation in perception might be due to different or incompletely understood information regarding the chosen prosthesis. In line with this observation, a substantial number of patients who chose a mechanical valve acknowledged that they would change their original choice to a biological prosthesis in light of the growing possibility of treating a failing bioprosthesis with a TAVI. This option should now be included in the shared decision process.
Despite overall satisfaction with valve choice, still one-third of the patients expressed some degree of post hoc decisional conflict, dominated by valve-specific interferences related to either type of prosthesis. This result corresponded to a decisional conflict rate of 31–34% in a Dutch study designed to examine the effect of implementing an on-line patient decision aid on the magnitude of this personal conflict [6]. However, cautious interpretation of this comparison is needed because the method used to quantify decisional conflict, based on an extensive 16-item questionnaire, might be more appropriate in their study. In addition, the presence of decisional conflict was studied preoperatively in relation to aortic and mitral valve replacements in a cohort of patients who were 22–82 years of age, 2 conditions that can contribute to the arbitrariness of the final prosthesis choice. In contrast, our data reflect a perception at some point after AVR and, in the meantime, may have been influenced by real-life interferences from valve-specific drawbacks.
This perception of uncertainty has commonly been associated with the information status of the individual patient. The findings of this study justify the use of enhanced efforts and means to help patients choose a prosthesis prior to a surgical procedure, often psychologically perceived as disabling. Better informed patients who are actively involved in the decision-making process are significantly less likely to experience decisional conflict after the operation. However, in a multicentre randomized trial, Korteland et al. failed to show a benefit of using a digital decision aid in decreasing the incidence of preoperative decisional conflict about the prosthesis choice. Although patients acknowledged that they were better informed, their level of uncertainty was not alleviated, regardless of the reduction of anxiety and improved mental well-being before the surgery [6]. Hence, our results indirectly indicate that the on-going uncertainty about a decision such as prosthesis choice depends on factors other than those related to the psychological resilience of the individual patient rather than to the completeness and adequacy of information. Nonetheless, these results underscore that the decision-making process for prosthesis choice should ideally integrate a shared and objective overview of the potential degree of interference of each valve type in the patient’s QoL and should be performed by >1 physician before elective AVR is scheduled, regardless of whether the physician is the patient’s cardiologist, cardiac surgeon or general practitioner. Therefore, the heart team approach, as currently recommended, should preferentially be combined with active patient participation in order to optimize the decisional pathway of the individual patient affected by valvular heart disease.
Another aspect skewing the comparison among studies performed in different countries concerns the differences in health educational profiles. Whereas the Dutch study [6] revealed that most patients favoured a decision-making process with equally shared responsibility between patient and physician, more than half of the patients in our survey mentioned that the final decision is best made by the physician. One-third of the patients even admitted to being insufficiently aware of the main differences between the valves, thereby explaining their motivation to rely principally on the surgeon for the choice of valve. These observations need to be considered from the perspective of the wide variability in culture and health care education among countries. Previous research in that area confirmed that the mode of care was primarily patient-centered in the Dutch society, in contrast to a more disease-centered and possibly a more paternalistic attitude towards the practice of medicine in our country [10, 11]. This observation indicates that the results from our study are not generalizable to or comparable to those from other countries and perhaps not even to other centres within our country.
Limitations
This study is a single-centre evaluation of a decision process reviewed 2–12 years after the operation, in a patient population undergoing AVR at an age when personal involvement was thought to be fully integrated. However, this study has some bias related to a disappointingly low response rate, potentially including only responses of patients who still felt emotionally linked to the cardiac procedure. Moreover, the broad time range since the AVR might be associated with a certain level of recall bias. The impact of this additional variability on the results remains difficult to determine and can only be limited by scrutinizing and empowering the survey response at well-defined time intervals after AVR in a prospectively motivated patient cohort.
The selection of a patient study subgroup restricted to the age range of 60 to 70 years and confined to an equivocal choice of a biological or mechanical prosthesis for AVR is not fully in accordance with the actual guidelines. Although this issue may be centre specific, precluding generalizability, we feel confident that the results represent the individual patient’s post hoc evaluation of his own perception of valve choice.
The different follow-up times of the patients who had biological and mechanical AVR at the time the survey was conducted might have influenced the responses regarding QoL and decisional conflict. Within this limited follow-up time, the number of valve-related events was low, precluding a significant effect of these complications on the post hoc satisfaction rate. In particular for patients with biological valves, it is conceivable that a longer time span since AVR, associated with an increasing risk for valve failure, might alter the decisional conflict rate in that group.
In addition, this kind of interrogation is perhaps valid for a selected patient population within a well-defined era, but it is possible that the derivations from this study will change over time due to the increased gathering of digital information in actual generations of patients.
CONCLUSION
In this survey, patient satisfaction and the eventual presence of decisional conflict regarding the valve prosthesis after AVR have been investigated in a specific patient cohort in whom age at the time of the operation was the predominant factor in the decision tree. A decisional conflict was noted in one-third of the patients and was mainly related to valve-specific issues such as fear of valve failure in patients with a biological valve and fear of bleeding, valve noise or anticoagulation-linked inconveniences in patients with a mechanical prosthesis. However, enhanced information and active involvement in the decision process at the time of the AVR appear to decrease the adverse perception or uncertainty of the individual patient of having perhaps made the inappropriate valve choice. Despite this uncertainty, >90% of the responders expressed post hoc satisfaction with the initial valve choice, even reconfirming their initial choice.
Despite the tendency of many patients to rely on the superior knowledge and responsibility of the physician, primarily the surgeon, it is mandatory to exert greater efforts to encourage active patient participation in the decision-making process of choosing a prosthesis before valve surgery in order to improve the individual patient’s awareness of the consequences of the shared decision.
Conflict of interest: none declared.
Author contributions
Laure Bryssinck: Data curation; Investigation; Methodology. Siel De Vlieger: Data curation; Formal analysis; Investigation; Methodology. Katrien François: Supervision; Writing—review & editing. Thierry Bové: Conceptualization; Formal analysis; Methodology; Validation; Writing—original draft; Writing—review & editing.
Reviewer information
Interactive CardioVascular and Thoracic Surgery thanks Takuya Fujikawa, Clarence Pienteu Pingpoh, Kevin M. Veen and the other, anonymous reviewer(s) for their contribution to the peer review process of this article.
ABBREVIATIONS
- AVR
Aortic valve replacement
- CIs
Confidence intervals
- OR
Odds ratio
- QoL
Quality of life
- TAVI
Transcatheter valve implant
REFERENCES
- 1. Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, Fleisher LA. et al. 2017 AHA/ACC Focused Update of the 2014 AHA/ACC Guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2017;135:e1159–e95. [DOI] [PubMed] [Google Scholar]
- 2. Baumgartner H, Falk V, Bax JJ, De Bonis M, Hamm C, Holm PJ. et al. ; ESC Scientific Document Group 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J 2017;38:2739–91. [DOI] [PubMed] [Google Scholar]
- 3. Chiang YP, Chikwe J, Moskowitz AJ, Itagaki S, Adams DH, Egorova NN.. Survival and long-term outcomes following bioprosthetic vs mechanical aortic valve replacement in patients aged 50 to 69 years. JAMA 2014;312:1323–9. [DOI] [PubMed] [Google Scholar]
- 4. Roumieh M, Ius F, Tudorache I, Ismail I, Fleissner F, Haverich A. et al. Comparison between biological and mechanical aortic valve prostheses in middle-aged patients matched through propensity score analysis: long-term results. Eur J Cardiothorac Surg 2015;48:129–36. [DOI] [PubMed] [Google Scholar]
- 5. Glaser N, Jackson V, Holzmann MJ, Franco-Cereceda A, Sartipy U.. Aortic valve replacement with mechanical vs. biological prostheses in patients aged 50-69 years. Eur Heart J 2016;37:2658–67. [DOI] [PubMed] [Google Scholar]
- 6. Korteland NM, Ahmed Y, Koolbergen DR, Brouwer M, de Heer F, Kluin J. et al. Does the use of a decision aid improve decision making in prosthetic heart valve selection? A multicenter randomized trial. Circulation Cardiovasc Quality Outcomes 2017;10:e003178. [DOI] [PubMed] [Google Scholar]
- 7. LeBlanc A, Kenny DA, O'Connor AM, Legare F.. Decisional conflict in patients and their physicians: a dyadic approach to shared decision-making. Med Decis Making 2009;29:61–8. [DOI] [PubMed] [Google Scholar]
- 8. Korteland NM, Top D, Borsboom GJ, Roos-Hesselink JW, Bogers AJ, Takkenberg JJ.. Quality of life and prosthetic aortic valve selection in non-elderly adult patients. Interact CardioVasc Thorac Surg 2016;22:723–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kottmaier M, Hettich I, Deutsch MA, Badiu C, Krane M, Lange R. et al. Quality of life and anxiety in younger patients after biological versus mechanical aortic valve replacement. Thorac Cardiovasc Surg 2017;65:198–205. [DOI] [PubMed] [Google Scholar]
- 10. Grol R, de Maeseneer J, Whitfield M, Mokkink H.. Disease-centred versus patient-centred attitudes: comparison of general practitioners in Belgium, Britain and The Netherlands. Fam Pract 1990;7:100–3. [DOI] [PubMed] [Google Scholar]
- 11. Grol R, Whitfield M, De Maeseneer J, Mokkink H.. Attitudes to risk taking in medical decision-making among British, Dutch and Belgian general practitioners. Brit J Gen Practice 1990;40:134–6. [PMC free article] [PubMed] [Google Scholar]