Abstract
The possibility of using three-dimensional reconstructions as an intraoperative aid to thoracic surgeons has not yet been fully explored. With this in mind, we developed a technology based on a three-dimensional virtual model of lungs obtained from lung computed tomography scans, the Hyper-Accuracy Three-Dimensional reconstruction (HA3D™), which aids the surgeon during surgery. We tested this technology while performing a uniportal video-assisted thoracic surgery right upper lobectomy for lung cancer.
Keywords: Lung 3D reconstruction, Intraoperative 3D guidance, HA3D™, 3D, Uniportal video-assisted thoracic surgery, Lung cancer
INTRODUCTION
In thoracic surgery, three-dimensional (3D) reconstructions are mainly utilized in the preoperative setting to improve the anatomical knowledge and the surgical strategy. However, its intraoperative use as an aid to surgeons may be its added value. We have undertaken a step forward in this direction by collaborating in the development of a specific 3D reconstruction of lung computed tomography (CT) images, the Hyper-Accuracy 3D reconstruction (HA3D™; MEDICS, Moncalieri, Turin, Italy), which delivers high standards of 3D anatomical information to interact with during surgery. We report the first use of this technology while performing a uniportal video-assisted thoracic surgery right upper lobectomy (RUL) for an early-stage lung cancer.
CASE REPORT
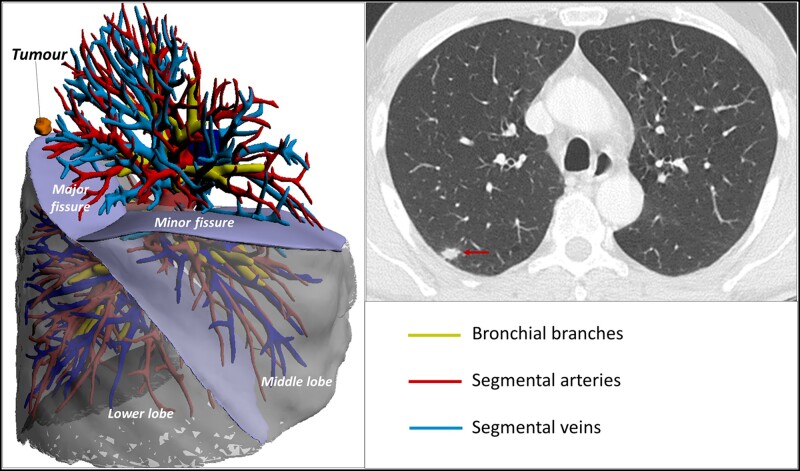
A patient affected by a right upper lobe adenocarcinoma of the lung (cT1b N0 M0) was considered a fit surgical candidate by the lung Multi-Disciplinary Team, based on the preoperative staging work-up (Total Body (TB)-CT scan, positron emission tomography–computed tomography, CT-guided biopsy, bronchoscopy) and functional status (spirometry with dLCO) (Fig. 1). Indication to uniportal video-assisted thoracic surgery RUL was given, which was carried out with the aid of the HA3D™ technology.
Figure 1:
HA3D™ reconstruction of the right lung and axial chest computed tomography scan showing the tumour.
Creating an HA3D™ model
The 3D virtual model of lungs, airways and vasculature was obtained by applying an ISO 13485:2016 certified process (HA3D™, Medics Srl, Turin, Italy) to contrast CT image stacks. Digital Imaging and Communications in Medicine (DICOM) data were processed using an open-source software for image-filtering and pre-processing (3D Slicer, https://www.slicer.org/) and, subsequently, by a commercially available software suite for clinical-grade image segmentation (Mimics Innovation Suite 22, Materialise, Belgium). Hessian-based vesselness filtering and adaptive histogram equalization filters were applied to enhance the contrast of intraparenchymal vessels [1]. The original images were employed for the segmentation of lung parenchyma, airways, tumour and enlarged lymph nodes. The resulting segmentation of these structures from the original dataset was then merged with the vessel segmentation from the filtered images to acquire a final segmentation of the whole lung. In order to better navigate the 3D model during surgery, each major branch origin was made independent on the 3D model.
A web-based application allows the upload of the CT-scan DICOM files together with the surgical specifications (e.g. type of resection planned). In the elaboration process, interaction between surgeons and Medics biomedical engineers is encouraged to meet the specifications required or to provide simulations and measurements based on the needs. Through the same application, surgeons will then be provided a PDF interactive 3D model tailored with the specifications requested (e.g. segmental arteries/veins/bronchi to be sectioned are made independent and marked with a different colour, and/or the presence of large lymph nodes or vascular/bronchial aberrations are made evident).
The PDF model will be visualized simultaneously to the surgical procedure on a side-by-side monitor/computer or with a ‘picture-in-picture’ function on supported screens. An unscrubbed assistant interacts with the model according to the surgeons’ needs (e.g. anatomical details can be zoomed/made transparent, model orientation changed, etc.). The 3D model is usually elaborated within 4–6 h and delivered in 72 h upon receiving the DICOM files.
HA3D™ during surgery
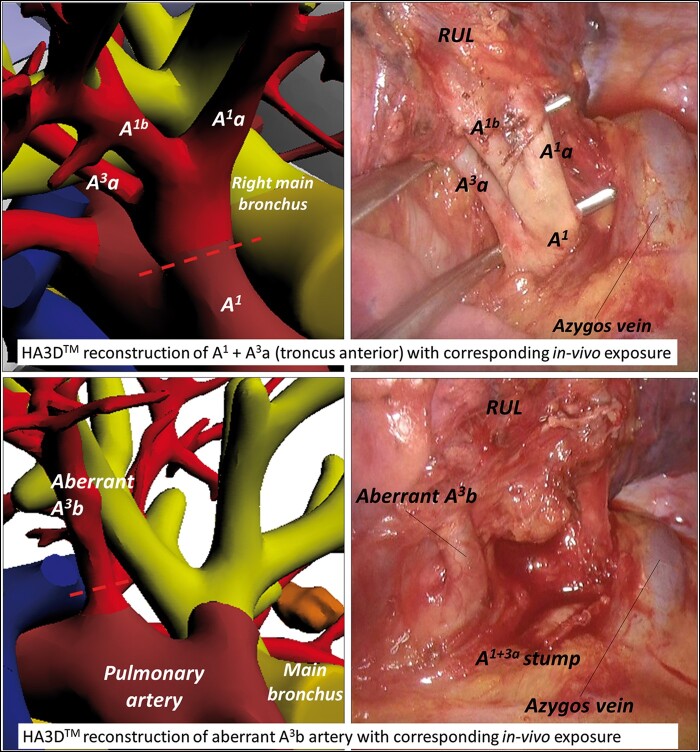
Following its creation through the steps described previously, the customised 3D model for this case was displayed on a side-by-side monitor and managed by an unscrubbed assistant. The troncus anterior of the pulmonary artery (PA) with subsegments A1a + A1b and A3a were exposed by dissection and subsequently divided prior verification through interaction with the 3D model (Fig. 2). Once divided, the same was then excluded from the 3D model, allowing an explicit vision of the remaining anatomy, which clearly distinguished an anatomical variation of A3b originating from the main PA, posterior to A1 and anterior to A2 (Fig. 2). Following the troncus anterior dissection, A3b was isolated and safely dissected after confirming its relationships with the surrounding structures by rotation of the 3D model and by excluding the vessel to clearly identify the ascending PA branch (A2), which was located more posteriorly. The 3D reconstruction yielded a distinctive identification of the RUL vein, which we divided and excluded from the model after distinctive identification of the middle lobe vein (V4 + 5). Interaction with the model showed that the RUL bronchus could have been safely taken before A2 due to the position of the latter. Its relationship with the arterial stumps, the interlobar lymph nodes e and the ascending PA branch (A2) were clearly distinguishable with the reconstruction and allowed a safe bronchial division after test-inflating the remaining lung. A2 with its subsegmental branches (A2a + A2b) was then manifested and dissected and the RUL was accomplished by completing the fissures by staplers.
Figure 2:
HA3D™ reconstruction of A1 + A3a and aberrant A3b artery.
COMMENT
The HA3D™ delivers a high-quality 3D model which features customizable characteristics, such as a 360° rotation on all axes, a zoom in/out option, a selective exclusion/inclusion and transparency of parenchyma, vascular/bronchial (sub-)segments and the study of lung fissures. Several of these characteristics are shared by other competitors (e.g. Visible Patient™, Strasbourg, France) and similar technologies have been previously described intraoperatively [1, 2]. However, its added value is a unique operative workflow focalized on reproducing, prior to surgery, the surgical plan based on the surgical steps that the surgeon will likely face intraoperatively, and deliver a tailored 3D reconstruction which is reproducible during surgery.
Our test determined the utility of using the HA3D™ intraoperatively, evidencing a very close to reality virtual navigation throughout the procedure, providing a clear advantage in the proceeding of the lobectomy, warranting precision, safety and confidence throughout the dissection.
Conflict of interest: none declared.
Reviewer information
Interactive CardioVascular and Thoracic Surgery thanks Clemens Aigner, Hasan Fevzi Batirel and the other anonymous reviewers for their contribution to the peer review process of this article.
REFERENCES
- 1. Seguin-Givelet A, Grigoroiu M, Brian E, Gossot D.. Planning and marking for thoracoscopic anatomical segmentectomies. J Thorac Dis 2018;10:S1187–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sardari Nia P, Olsthoorn JR, Heuts S, Maessen JG.. Interactive 3D reconstruction of pulmonary anatomy for preoperative planning, virtual simulation, and intraoperative guiding in video-assisted-thoracoscopic lung surgery. Innovations (Phila) 2019;14:17–26. [DOI] [PubMed] [Google Scholar]