Abstract
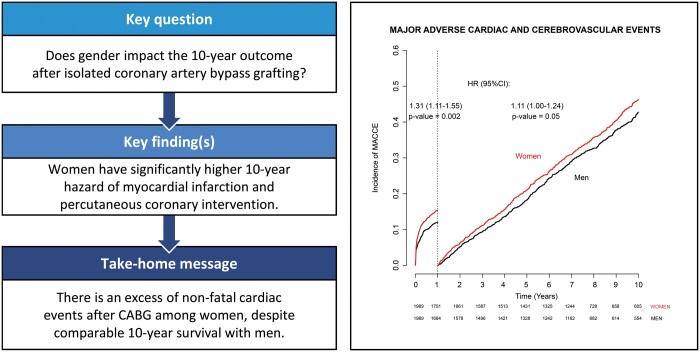
OBJECTIVES
Our goal was to evaluate the impact of gender on the 10-year outcome of patients after isolated coronary artery bypass grafting (CABG) included in the Italian nationwide PRedictIng long-term Outcomes afteR Isolated coronary arTery bypass surgery (PRIORITY) study.
METHODS
The PRIORITY project was designed to evaluate the long-term outcomes of patients who underwent CABG and were included in 2 prospective multicentre cohort studies. The primary end point of this analysis was major adverse cardiac and cerebrovascular events. Baseline differences between the study groups were balanced with propensity score matching and inverse probability of treatment. Time to events was analysed using Cox regression and competing risk analysis.
RESULTS
The study population comprised 10 989 patients who underwent isolated CABG (women 19.6%). Propensity score matching produced 1898 well-balanced pairs. The hazard of major adverse cardiac and cerebrovascular event was higher in women compared to men [adjusted hazard ratio (HR) 1.13, 95% confidence interval (CI) 1.03–1.23; P = 0.009]. The incidence of major adverse cardiac and cerebrovascular event in women was significantly higher at 1 year (HR 1.31, 95% CI 1.11–1.55; P < 0.001) and after 1 year (HR 1.11, 95% CI 1.00–1.24; P = 0.05). Mortality at 10 years in the matched groups was comparable (HR 1.04, 95% CI 0.93–1.16; P = 0.531). Women have significantly a higher 10-year risk of myocardial infarction (adjusted HR 1.40, 95% CI 1.17–1.68; P = 0.002) and percutaneous coronary intervention (adjusted HR 1.32, 95% CI 1.10–1.59; P = 0.003).
CONCLUSIONS
The present study documented an excess of non-fatal cardiac events after CABG among women despite comparable 10-year survival with men. These findings suggest that studies investigating measures of tertiary prevention are needed to decrease the risk of adverse cardiovascular events among women.
Keywords: Coronary artery bypass grafting, Gender, Female, Women
Over the last 2 decades clinicians and policy makers have recognized the need for gender-specific medicine [1].
INTRODUCTION
Over the last 2 decades clinicians and policy makers have recognized the need for gender-specific medicine [1]. Cardiovascular diseases have different patterns in women, although the underlying mechanisms of such differences are far from being completely understood [1–5]. The incidence of cardiovascular diseases is lower in women; nevertheless, their prognosis is poorer after a cardiovascular event [6]. Investigating gender-related differences in patients undergoing coronary artery bypass grafting (CABG) is of cornerstone importance, because existing evidence is still mixed, and a gender-related prognosis after CABG cannot be unequivocally pictured [7–15]. Women have been shown to have worse long-term survival after CABG, although it has been questioned whether the gender itself is a risk factor or outcomes are biased by different risk profiles [9–16]. A recent cohort study showed no increased risk of mortality, stroke, myocardial infarction (MI) and repeat revascularization among women [17], but these opposite outcomes are barely comparable because of the different methods used to control for unbalanced comorbidities between groups [18].
Hence, we have investigated the controversial impact of gender on cardiovascular events after CABG [14, 15, 17] in patients from a nationwide prospective registry who underwent isolated CABG.
MATERIALS AND METHODS
Data sources and study population
The PRedictIng long-term Outcomes afteR Isolated coronary arTery bypass surgery (PRIORITY) project is an observational cohort study merging 2 prospective multicentre studies conducted from 2002 to 2004 (Italian-CABG project, IT-CABG; Supplementary Material) and from 2007 to 2008 (Italian-CABG project 2, IT-CABG II; Supplementary Material) [19–22]. These 2 studies shared the same variables according to the EuroSCORE definition criteria. Data of the 2 studies were collected in the period 2002–2008 for aims falling within the Current Research Activities envisaged for Italian regions, National Health Institute and Universities (art. 5, Legislative Decree 282/99) and therefore the collection and processing of these data does not require the written consent of the participants. Protocols and data on IT-CABG and IT-CABG II are available at https://www.outcomeresearch.it/PROGRESSI/Login.aspx.
Follow-up information was obtained by a record linkage with the National Hospital Discharged Records database and the Tax Registry Information System, provided by the Italian Ministry of Health through a collaboration with the Italian National Program for Outcome Evaluation. The methods used for record linkage among databases were described previously [23]. Data on patients death and date of death are available only from the beginning of 2004; therefore, patients enrolled in the IT-CABG study prior to 1 January 2004 were excluded from the present analysis. Follow-up was truncated at 10 years after the intervention.
Outcomes
The main outcome of this study was any major adverse cardiac and cerebrovascular event (MACCE, defined as all-cause mortality, rehospitalization for acute MI, rehospitalization for repeat revascularization with percutaneous coronary intervention PCI or CABG, and rehospitalization for stroke) at 10 years. Secondary outcomes were all-cause mortality, rehospitalization for acute MI, rehospitalization for repeat revascularization with PCI or CABG and re-recovery for stroke. All end points are described by administrative rather than clinical definitions and are identified through the administrative codes of re-recovery.
Data analysis
To overcome the selection bias related to the observational nature of the study, we used a propensity score approach [24]. The probability of a woman undergoing isolated CABG was generated by a non-parsimonious logistic regression model including the 23 variables listed in Table 1. The logit of the resulting propensity score was used for one-to-one matching of men and women using the greedy matching algorithm (calliper 0.01 of the standard deviation of the logit of the propensity score). The balance between the matched groups was evaluated with standardized differences. We also tested weighing regression models with propensity scores as a balancing method in order to confirm the results of propensity score matching. The inverse probability of treatment weight (IPTW) was defined as the inverse of the probability of receiving the treatment that the patient received. The end points were then studied with time-to-event models that were weighted for the IPTW and the IPTW-weighted Kaplan–Meier estimators and log-rank test. Propensity score weighting has the advantage of permitting the use of all the subjects in the 2 treatments groups for the outcome analysis compared to propensity score matching.
Table 1:
Baseline characteristics and operative data of the study groups before and after propensity score matching
| Overall series |
Propensity score matched groups |
||||||
|---|---|---|---|---|---|---|---|
| Baseline characteristics and operative data | Women (N = 2150) | Men (N = 8839) | P-value | Women (N = 1989) | Men (N = 1989) | Mean standardized difference | P-value |
| Age (years), mean (SD) | 70.5 (8.8) | 66.3 (9.5) | <0.001 | 70.2 (8.8) | 69.9 (8.6) | 0.0259 | 0.405 |
| Creatinine >2 mg/dl, n (%) | 91 (4.2) | 415 (4.7) | 0.389 | 86 (4.3) | 71 (3.6) | 0.0373 | 0.254 |
| Dialysis, n (%) | 15 (0.7) | 72 (0.8) | 0.676 | 15 (0.8) | 10 (0.5) | 0.0294 | 0.423 |
| Diabetes on drug treatment, n (%) | 918 (42.7) | 2627 (29.8) | <0.001 | 845 (42.5) | 828 (41.6) | 0.0172 | 0.607 |
| Neurological dysfunction,an (%) | 44 (2.1) | 159 (1.8) | 0.478 | 37 (1.9) | 31 (1.6) | 0.0223 | 0.541 |
| Previous stroke, n (%) | 71 (3.3) | 299 (3.4) | 0.889 | 65 (3.3) | 44 (2.2) | 0.0597 | 0.05 |
| Systolic PA pressure > 60 mmHg, n (%) | 5 (0.2) | 36 (0.4) | 0.323 | 5 (0.3) | 3 (0.2) | 0.0203 | 0.726 |
| Chronic pulmonary disease,an (%) | 139 (6.5) | 892 (10.1) | <0.001 | 135 (6.8) | 10.8 (5.4) | 0.0546 | 0.090 |
| Cancer, n (%) | 16 (0.7) | 102 (1.2) | 0.108 | 14 (0.7) | 12 (0.6) | 0.0122 | 0.845 |
| Extracardiac arteriopathy,an (%) | 407 (18.9) | 1771 (20.1) | 0.252 | 392 (19.7) | 350 (17.6) | 0.0534 | 0.10 |
| Cirrhosis, n (%) | 6 (0.3) | 24 (0.3) | 0.999 | 5 (0.3) | 3 (0.2) | 0.0186 | 0.726 |
| Unstable angina, n (%) | 663 (30.9) | 2244 (25.4) | <0.001 | 611 (30.7) | 610 (30.8) | −0.0011 | 0.999 |
| Recent myocardial infarction,an (%) | 592 (27.5) | 2180 (24.7) | 0.006 | 536 (26.9) | 497 (25.0) | 0.0440 | 0.169 |
| Left ventricular ejection fraction < 30%, n (%) | <0.01? | −0.0335 | 0.787 | ||||
| 30–50% | 776 (36.8) | 3296 (38.1) | 730 (36.7) | 709 (35.6) | |||
| <30% | 68 (3.2) | 454 (5.3) | 65 (3.3) | 66 (3.3) | |||
| Previous CABG, n (%) | 23 (1.1) | 200 (2.3) | <0.001 | 22 (1.1) | 19 (1.0) | 0.0146 | 0.754 |
| Previous cardiac surgery excluding CABG, n (%) | 16 (0.7) | 84 (1.0) | 0.444 | 14 (0.7) | 19 (0.9) | −0.0183 | 0.719 |
| Haemodynamic instability,bn (%) | 119 (5.6) | 468 (5.3) | 0.672 | 103 (5.2) | 101 (5.1) | 0.0045 | 0.943 |
| Recent ventricular arrhythmia,cn (%) | 50 (2.3) | 201 (2.3) | 0.878 | 48 (2.4) | 50 (2.5) | −0.0065 | 0.919 |
| Cardiogenic shock, n (%) | 18 (0.8) | 66 (0.7) | 0.688 | 13 (0.7) | 13 (0.7) | 0.0000 | 0.999 |
| Emergency procedure,an (%) | 78 (3.6) | 326 (3.7) | 0.944 | 73 (3.7) | 68 (3.4) | 0.0132 | 0.732 |
| Off-pump surgery | 605 (28.1) | 2378 (26.9) | 0.256 | 562 (28.3) | 530 (26.6) | −0.0358 | 0.271 |
| Bilateral internal mammary artery grafting | 408 (19.0) | 2169 (24.5) | <0.001 | 405 (20.4) | 424 (21.3) | −0.0239 | 0.482 |
Defined according to the EuroSCORE criteria.
Preoperative inotropic support or intra-aortic balloon pump.
Preoperative ventricular tachycardia or ventricular fibrillation.
CABG: coronary artery bypass grafting; PA: pulmonary artery; SD: standard deviation.
Long-term end points were analysed with time-to-event non-parametric and semiparametric methods. Time-to-event distributions were analysed separately accordingly to the type of primary event. Time-to-death and time-to-MACCE were modelled with the grouped frailty semiparametric Cox model, accounting for heterogeneity among centres with a random-intercept parameter as previously described. Grouped frailty semiparametric Fine and Gray models were used in competing risk analysis for time to rehospitalization for MI, PCI, CABG and/or stroke with death as the competing risks [25–27]. The selection of variables for the Cox models was performed by a forward stepwise regression (probability of stay = 0.10; probability of entry = 0.05). The selection of variables for the Fine Gray models was performed by a forward stepwise regression with the Akaike information criterion as selection criteria. Hazards proportionality and time-dependent effects were checked with the analysis of Schoenfeld residuals, the Kolmogorov–Smirnov test and the Cramér–von Mises test.
The time dependency of the treatment effect was approached with landmark analysis, applying Kaplan–Meier analysis and Cox regression to evaluate end points in women and men at specific times. The cut-offs were chosen on the basis of visual inspection of the scaled Schoenfeld residuals and the Kaplan–Meier curves.
Two-sided statistics were performed with a significance level of 0.05. Analyses were performed with R language [R 4.0.3; R Development Core Team (2020). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria].
RESULTS
The IT-CABG and IT-CABG II studies enrolled a total of 11 538 patients since January 2004 and had administrative data available for linkage. The record linkage of administrative and clinical data sets led to links of 95.2% of patients; the final study cohort comprised 10 989 patients with complete baseline clinical characteristics, operative data and administrative follow-up. Of these patients, 2150 (19.6%) were women. The follow-up time was 86 005 patient-years (median 7.9 years; 69 746 patient-years in the male group and 16 259 patient-years in the female group).
Propensity score matching produced well-balanced pairs of 1898 patients as confirmed by diagnostic plots (see Supplementary Material, Fig. S1). Table 1 shows the baseline characteristics of the unmatched and matched groups. In the unmatched cohort, women were significantly older at the time of surgery, had a higher rate of diabetes and unstable angina and less frequently received bilateral internal mammary artery grafts.
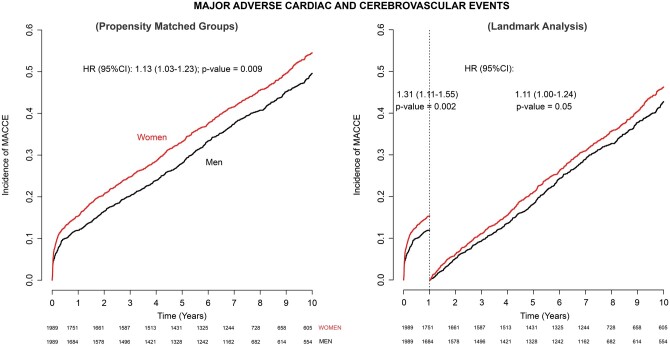
Major adverse cardiac and cerebrovascular events
The crude incidence of MACCE at 10 years in the propensity score matched cohorts was 50.6% (1006 events) for women and 45.8% (911) for men [adjusted hazard ratio (HR) 1.13, 95% confidence interval (CI) 1.03–1.23; P = 0.009]. The estimate of random parameter θ for heterogeneity among centres was 0.012 (P = 0.087). Although the proportional hazards assumption was granted in the model, the analysis of the Kaplan–Meier curves suggested a different HR before and after the first year. A landmark analysis with the cut-off at 1 year was performed (Fig. 1). In the first year after the operation, the incidence of MACCE in women was significantly higher compared to that in men (HR 1.31, 95% CI 1.11–1.55; P < 0.001). Women were also associated with an increased incidence of MACCEs after 1 year (HR 1.11, 95% CI 1.00–1.24; P = 0.05).
Figure 1:
Left panel: cumulative incidence of major adverse cardiac and cerebrovascular events at 10 years in the propensity score matched groups with landmarking at 1 year (right panel). CI: confidence interval; HR: hazard ratio.
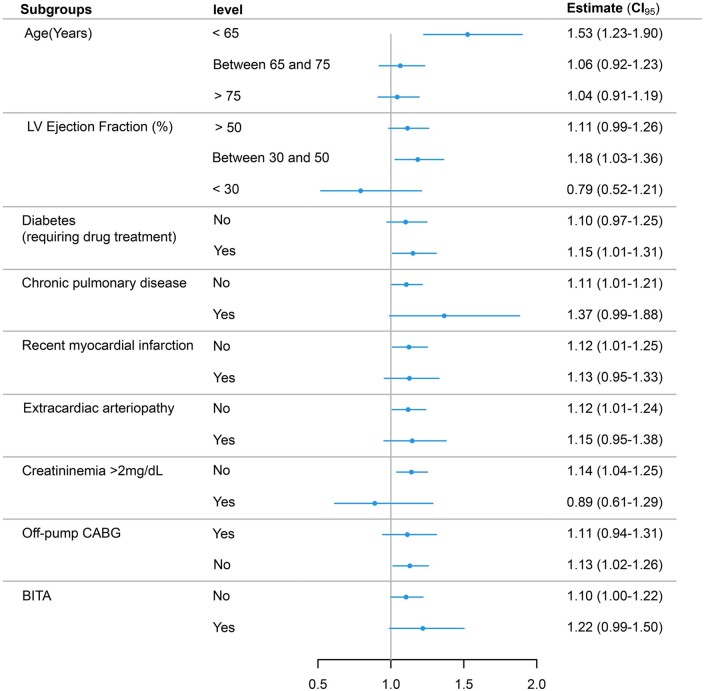
Results of subgroup analysis with interaction testing for the primary end point are presented in Fig. 2. The hazard of MACCE was significantly higher for women younger than 65 years and for lower risk profiles, women being at an increased risk in the absence of most comorbidities such as diabetes, pulmonary disease and recent MI.
Figure 2:
Subgroup analysis for major adverse cardiac and cerebrovascular events. BITA: bilateral internal thoracic artery; CABG: coronary artery bypass grafting; CI: confidence interval; LV: left ventricle.
The use of IPTW adjusted the wider difference in the unmatched groups (Supplementary Material, Fig. S2) to a level comparable to that of propensity score matched cohorts (adjusted HR 1.13, 95% CI 1.09–1.18; P < 0.001, Table 2).
Table 2:
Adjusted risk estimates for adverse events at 10 years in women compared to men according to propensity score matching and propensity score weighting analyses
| Outcomes | PS matched analysis (HR, 95% CI) | P-value | PS weighting analysis (HR, 95% CI) | P-value |
|---|---|---|---|---|
| MACCE | 1.13 (1.03–1.23) | 0.009 | 1.13 (1.09–1.18) | <0.001 |
| All-cause mortality | 0.99 (0.89–1.11) | 0.921 | 0.97 (0.91–1.01) | 0.210 |
| Percutaneous coronary intervention | 1.32 (1.10–1.59) | 0.003 | 1.28 (1.11–1.47) | <0.001 |
| Myocardial infarction | 1.40 (1.17–1.68) | 0.002 | 1.34 (1.17–1.54) | <0.001 |
| Stroke | 1.00 (0.81–1.24) | 0.748 | 0.95 (0.80–1.10) | 0.550 |
CI: confidence interval; HR: hazard ratio; MACCE: major adverse cardiac and cerebrovascular event; PS: propensity score.
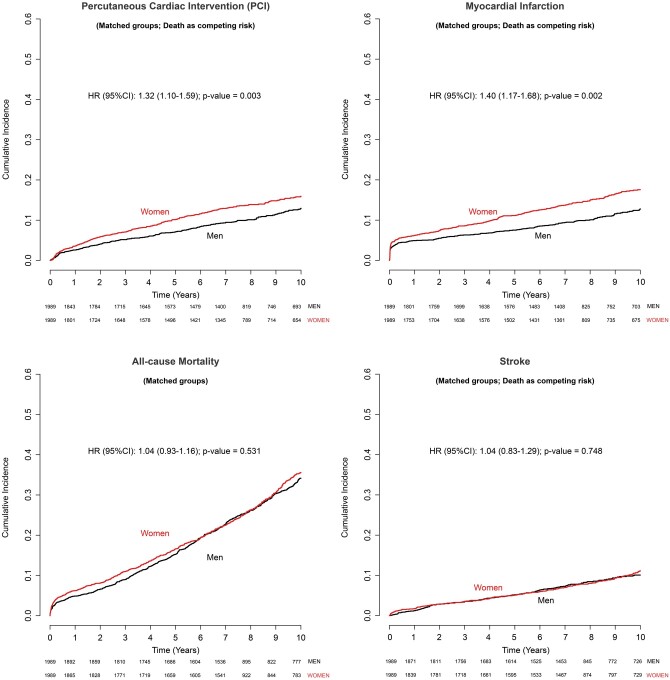
Ten-year mortality, myocardial infarction, stroke and repeat revascularization
The risk of each secondary outcome is shown in Fig. 3 and Table 2. Mortality at 10 years was comparable in the propensity score matched cohorts (HR 1.04, 95% CI 0.93–1.16; P = 0.531) (Table 2). Taking into account the differences in baseline risk profile balanced the excess of mortality in women evident in the unmatched groups (Supplementary Material, Fig. S4), also confirmed by IPTW adjustment (Table 2 and Supplementary Material, Fig. S4).
Figure 3:
Cumulative incidence function of PCI, myocardial infarction, all-cause death and stroke at 10 years in the propensity score matched groups. CI: confidence interval; HR: hazard ratio; PCI: percutaneous coronary intervention.
Gender has no effect on the incidence of stroke at 10 years in the propensity score matched cohorts (HR 1.04, 95% CI 0.83–1.29; P = 0.748) as well as in overall series (Supplementary Material, Fig. S5).
The cumulative incidence of MI was significantly higher in women in the unmatched groups (Gray’s test, P < 0.001, Supplementary Material, Fig. S6). This excess of risk in women was mitigated by propensity score matching; nonetheless it remains significant, with a 40% higher hazard of MI compared to men (adjusted HR 1.40, 95% CI 1.17–1.68; P = 0.002). Heterogeneity among centres was 0.012 (θ = 0.080; P < 0.001).
The risk of PCI at 10 years was higher in women than in men (adjusted HR 1.32, 95% CI 1.10–1.59; P = 0.003). For this end point, balancing with both propensity score matching and weighting gave a consistently higher risk of PCI compared to that of the unweighted cohort (Supplementary Material, Fig. S7).
Repeat CABG was necessary in only 12 patients at follow-up (4 in men, 8 in women) with no difference between the study groups (Gray’s test, P = 0.400; HR 1.87, 95% CI 0.57–6.13; P = 0.30).
DISCUSSION
The present study showed that (i) women have an increased adjusted risk of MI and repeat PCI at 10 years and (ii) the risk of death and stroke at 10 years is comparable in men and women.
Understanding the gender-based differences in the late outcomes after CABG is a core issue of the PRIORITY project because evidence on long-term outcomes is still controversial, and new insight into the specific risks for women is vital for encouraging health care decision makers to develop specific programs on tertiary prevention after CABG and educate women on issues of gender-related prognosis.
Women with severe coronary artery disease requiring surgical revascularization hold a different risk profile compared to men [14–17] because they are older and have a higher burden of comorbidities such as diabetes, hypertension and cerebrovascular disease [12–16]. The reasons for these disparities are to be found in biological sex differences as well as in the observed gender bias resulting in a delay in the diagnosis and treatment among women [9, 27]. Our data are partially consistent with previous findings because women were older in the PRIORITY cohort, but comorbidities were differently distributed in men and women, i.e. diabetes and unstable angina were prevalent among women whereas pulmonary disease, depressed ventricular function and previous CABG were more frequent among men. Interestingly, our data corroborate the evidence of treatment disparity because women were less likely to receive bilateral internal mammary arteries [17, 28]. Hence, considering this potential confounding factor together with appropriate methods for adjustment is critical to avoid misleading outcomes and inferences. In observational cohort and retrospective studies, which represent the majority of evidence in this field of research, the methods for balancing for baseline differences are mainly regression modelling and models based on propensity scores. If no attempts are made to balance the gender groups by their different baseline characteristics, outcomes will be biased and not interpretable.
In gender-based cardiovascular medicine, the risk of misleading results is clear in the analysis of long-term survival. Different study designs and methodological approaches as well as diverse enrolling periods have led to controversial findings. A recent large retrospective cohort study demonstrated a higher risk of 8-year mortality after isolated CABG in women, but adjustment for confounding factors was not performed, except for age-standardized mortality [8]. Still, the increased risk profile in the female cohort introduced bias in survival analysis. The risk adjustment by balancing methods over-rides the higher long-term mortality among women [17]. We corroborated this outcome by showing that the excess deaths at 10 years in women was related to their different preoperative risk profiles. In the present study, women did not have an increased risk of stroke as also observed in prior studies [14–17].
The main finding of this study is the higher incidence of MACCEs among women, which persisted despite extensive risk adjustment. The 10-year risk of MACCE is higher in the first year but remains significant afterwards and accounted for a 40% higher risk of MI and 32% higher risk of PCI for women compared to men. The 10-year cumulative incidence of both myocardial and PCI was independent of baseline characteristics and of the use of bilateral internal mammary arteries. The latter finding raises concerns about the possible amelioration of gender disparities by bilateral internal mammary artery grafting that was documented in prior studies [29]. Our results are in contrast with those of a large cohort study by Dalén et al. [17], which showed that gender was not a risk factor for MI and PCI. However, these results should be considered with caution because the association between gender and repeat revascularization held non-proportional hazards; also, the Kaplan–Meier curves for MI suggest a time-varying HR that cannot be summarized by the Cox-semiparametric HR. Indeed, when the Cox modelling shows a departure from the constancy of the HR, it cannot be used to summarize outcomes. Consequently, researchers need to move to time-varying models or to a landmark analysis. The study by Dalén et al. [17] had other potential drawbacks such as the high proportion of missing values for some relevant variables and the fact that imputation can fail to manage a high proportion of missing data. Moreover, results can be also modified by the lack of adjustment for the centre effect with frailty models as well as the choice of not to treat PCI and MI in a competing risk framework.
Investigation of the causes underlying a gender bias in the risk of MI and of repeat revascularization with PCI was not the goal of our observational study. Women have a higher prevalence of small-vessel disease, and revascularization could be less effective in them than in men [6]. The gender bias in tertiary prevention could be responsible for the worse results among women [30]. Biological differences may account for a different pattern of coronary artery disease and influence the natural course of disease after CABG [1].
Limitations and strengths
Our study is limited by its observational nature. Second, no inferences can be drawn on the causes of higher incidence of late MI and repeat revascularization with PCI among women because no data were available on the severity of coronary artery disease, completeness of revascularization and adequacy and adherence to post-surgery medical treatment. Third, a risk of bias in evaluating men and women may still be present for confounders that were not available in the database. Finally, this study has the limitations related to the administrative follow-up, with generic administrative data on diagnosis and procedures of re-recovery but no precise clinical information.
This study was designed to focus on the ‘real world’ and on the relationship between gender and the 10-year outcomes after isolated CABG. The strength of this study is the completeness of preoperative clinical information on such a large number of patients and the advantages of administrative follow-up. In fact, there were no patients lost to follow-up, and retrieval data on late outcome was independent of participating researchers and clinicians.
CONCLUSIONS
The present study documented an excess of non-fatal cardiac events after CABG among women, despite comparable 10-year survival with men. These findings suggest that studies investigating measures of tertiary prevention as well as deeper evaluations of treatment disparities between genders are needed to decrease the risk of adverse cardiovascular events among women.
SUPPLEMENTARY MATERIAL
Supplementary material is available at ICVTS online.
Funding
The PRIORITY study was supported by the Italian Ministry of Health by a grant from the Finalized Research [WFR GR-2013-02359264]. The study was carried out in collaboration with the Italian National Agency for Regional Healthcare Services as part of the Italian National Results Evaluation Program.
Conflict of interest: Fabio Barili reports receiving consulting fees from Abbott, outside the scope of the present work. All other authors declared no conflict of interest.
Author contributions
Fabio Barili: Conceptualization; Formal analysis; Methodology; Visualization; Writing—original draft. Paola D’Errigo: Data curation; Methodology; Writing—review & editing. Stefano Rosato: Data curation; Investigation; Methodology; Resources; Writing—review & editing. Fausto Biancari: Resources; Supervision; Validation; Writing—review & editing. Marco Forti: Investigation; Methodology; Software; Writing—review & editing. Eva Pagano: Conceptualization; Resources; Validation; Visualization; Writing –review & editing. Alessandro Parolari: Methodology; Project administration; Supervision; Validation; Writing—review & editing. Mara Gellini: Validation; Visualization; Writing—original draft; Writing—review & editing. Gabriella Badoni: Investigation; Methodology; Visualization; Writing—review & editing. Fulvia Seccareccia: Conceptualization; Methodology; Writing—original draft; Writing—review & editing.
Reviewer information
Interactive CardioVascular and Thoracic Surgery thanks the anonymous reviewer(s) for their contribution to the peer review process of this article.
Supplementary Material
ABBREVIATIONS
- CABG
Coronary artery bypass grafting
- CI
Confidence interval
- HR
Hazard ratio
- IPTW
Inverse probability of treatment weight
- MACCEs
Major adverse cardiac and cerebrovascular events
- MI
Myocardial infarction
- PCI
Percutaneous coronary intervention
- PRIORITY
PRedictIng long-term Outcomes afteR Isolated coronary arTery bypass surgery
REFERENCES
- 1. Mauvais-Jarvis F, Bairey MN, Barnes PJ, Brinton RD, Carrero JJ, DeMeo DL. et al. Sex and gender: modifiers of health, disease, and medicine. Lancet 2020;396:565–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Roger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD, Brown TM, et al. ; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2011 update: a report from the American Heart Association. Circulation 2011;123:e18–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ventura-Clapier R, Dworatzek E, Seeland U, Kararigas G, Arnal JF, Brunelleschi S. et al. Sex in basic research: concepts in the cardiovascular field. Cardiovasc Res 2017;113:711–24. [DOI] [PubMed] [Google Scholar]
- 4. Kane AE, Howlett SE.. Differences in cardiovascular ageing in men and women. Adv Exp Med Biol 2018;1065:389–411. [DOI] [PubMed] [Google Scholar]
- 5. O'Neil A, Scovelle AJ, Milner AJ, Kavanagh A.. Gender/sex as a social determinant of cardiovascular risk. Circulation 2018;137:854–64. [DOI] [PubMed] [Google Scholar]
- 6. Mosca L, Barrett-Connor E, Wenger NK.. Sex/gender differences in cardiovascular disease prevention: what a difference a decade makes. Circulation 2011;124:2145–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Puskas JD, Kilgo PD, Kutner M, Pusca SV, Lattouf O, Guyton RA, Off-pump techniques disproportionately benefit women and narrow the gender disparity in outcomes after coronary artery bypass surgery. Circulation 2007;116(suppl I):I192–9. [DOI] [PubMed] [Google Scholar]
- 8. Johnston A, Mesana TG, Lee DS, Eddeen AB, Sun LY.. Sex differences in long term survival after major cardiac surgery: a population-based cohort study. J Am Heart Assoc 2019;8:e013260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sun L, Tu J, Bader Eddeen A, Liu P.. Prevalence and long-term survival after coronary artery bypass grafting in men and women with heart failure and preserved versus reduced ejection fraction. J Am Heart Assoc 2018;7:e008902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Arif R, Farag M, Gertner V, Szabo G, Weymann A, Veres G. et al. Female gender and differences in outcome after isolated coronary artery bypass graft surgery: does age play a role? PLoS One 2016;11:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Blankstein R, Ward R, Arnsdorf M, Jones B, Lou Y, Pine M.. Female gender is an independent predictor of operative mortality after coronary artery bypass graft surgery: contemporary analysis of 31 midwestern hospitals. Circulation 2005;112:I323–7. [DOI] [PubMed] [Google Scholar]
- 12. Alam M, Bandeali S, Kayani W, Ahmad W, Shahzad S, Jneid H. et al. Comparison by meta-analysis of mortality after isolated coronary artery bypass grafting in women versus men. Am J Cardiol 2013;112:309–17. [DOI] [PubMed] [Google Scholar]
- 13. Filardo G, Hamman B, Pollock B, da Graca B, Sass D, Phan T. et al. Excess short-term mortality in women after isolated coronary artery bypass graft surgery. Open Heart 2016;3:e000386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Nicolini F, Vezzani A, Fortuna D, Contini G, Pacini D, Gabbieri D. et al. Gender differences in outcomes following isolated coronary artery bypass grafting: long-term results. J Cardiothorac Surg 2016;11:10–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Guru V, Fremes S, Austin P, Blackstone E, Tu J.. Gender differences in outcomes after hospital discharge from coronary artery bypass grafting. Circulation 2006;113:507–16. [DOI] [PubMed] [Google Scholar]
- 16. Ter WJ, van Straten AHM, Houterman S, Soliman-Hamad MA.. Sex difference in coronary artery bypass grafting: preoperative profile and early outcome. J Cardiothorac Vasc Anesth 2019;33:2679–84. [DOI] [PubMed] [Google Scholar]
- 17. Dalén M, Nielsen S, Ivert T, Holzmann MJ, Sartipy U.. Coronary artery bypass grafting in women 50 years or younger. J Am Heart Assoc 2019;8:e013211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Blackstone EH. Comparing apples and oranges. J Thorac Cardiovasc Surg 2002;123:8–15. [DOI] [PubMed] [Google Scholar]
- 19. Barili F, Rosato S, D'Errigo P, Parolari A, Fusco D, Perucci CA. et al. Impact of off-pump coronary artery bypass grafting on long-term percutaneous coronary interventions. J Thorac Cardiovasc Surg 2015;150:902–9.e1–6. [DOI] [PubMed] [Google Scholar]
- 20. Seccareccia F, Perucci CA, D'Errigo P, Arcà M, Fusco D, Rosato S. et al. The Italian CABG Outcome Study: short-term outcomes in patients with coronary artery bypass graft surgery. Eur J Cardiothorac Surg 2006;29:56–62. [DOI] [PubMed] [Google Scholar]
- 21. D'Errigo P, Tosti ME, Fusco D, Perucci CA, Seccareccia F; Research group, Italian CABG Outcome Study. Use of hierarchical models to evaluate performance of cardiac surgery centres in the Italian CABG outcome study. BMC Med Res Methodol 2007;7:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. D'Errigo P, Seccareccia F, Rosato S, Manno V, Badoni G, Fusco D. et al. Comparison between an empirically derived model and the EuroSCORE system in the evaluation of hospital performance: the example of the Italian CABG Outcome Project. Eur J Cardiothorac Surg 2008;33:325–33. [DOI] [PubMed] [Google Scholar]
- 23. Rosato S, D'Errigo P, Badoni G, Fusco D, Perucci CA, Seccareccia F.. Comparison between administrative and clinical databases in the evaluation of cardiac surgery performance. G Ital Cardiol 2008;9:569–78. [PubMed] [Google Scholar]
- 24. Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res 2011;46:399–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Putter H, Fiocco M, Geskus RB.. Tutorial in biostatistics: competing risks and multi-state models. Stat Med 2007;26:2389–430. [DOI] [PubMed] [Google Scholar]
- 26. Barili F, Barzaghi N, Cheema FH, Capo A, Jiang J, Ardemagni E. et al. An original model to predict intensive care unit length-of stay after cardiac surgery in a competing risk framework. Int J Cardiol 2013;168:219–25. [DOI] [PubMed] [Google Scholar]
- 27. Reis SE, Holubkov R, Conrad SA, Kelsey SF, Sharaf BL, Reichek N. et al. Coronary microvascular dysfunction is highly prevalent in women with chest pain in the absence of coronary artery disease: results from the NHLBI WISE study. Am Heart J 2001;141:735–41. [DOI] [PubMed] [Google Scholar]
- 28. Jacobs AK, Kelsey SF, Brooks MM, Faxon DP, Chaitman BR, Bittner V. et al. Better outcome for women compared with men undergoing coronary revascularization: a report from the Bypass Angioplasty Revascularization Investigation (BARI). Circulation 1998;98:1279–85. [DOI] [PubMed] [Google Scholar]
- 29. Kurlansky PA, Traad EA, Galbut DL, Singer S, Zucker M, Ebra G.. Coronary bypass surgery in women: a long-term comparative study of quality of life after bilateral internal mammary artery grafting in men and women. Ann Thorac Surg 2002;74:1517–25. [DOI] [PubMed] [Google Scholar]
- 30. Peters SAE, Muntner P, Woodward M.. Sex differences in the prevalence of, and trends in, cardiovascular risk factors, treatment, and control in the United States, 2001 to 2016. Circulation 2019;139:1025–35. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.