Abstract
Background:
While injury is a leading cause of death and debility in older adults, the relationship between intensity of care and trauma remains unknown. The focus of this analysis is to measure the overall intensity of care delivered to injured older adults during hospitalization.
Methods:
We used Centers for Medicare and Medicaid Services Medicare fee-for-service claims data (2013–2014), to identify ED-based claims for moderate and severe blunt trauma in age-eligible beneficiaries. Medical procedures associated with care intensity were identified using a modified Delphi method. A latent class model was estimated using the identified procedures, ICU length of stay, demographics, and injury characteristics. Clinical phenotypes for each class were explored.
Results:
A total of 683,398 cases were classified as low intensity (73%), moderate (23%), and high intensity care (4%). Greater age and reduced injury severity were indicators of lower intensity, while males, non-whites, and non-fall mechanisms were more common with high intensity. Intubation/mechanical ventilation was an indicator of high intensity and often occurred with at least one other procedure or an extended ICU stay.
Conclusions:
This work demonstrates that although heterogeneous, care for blunt trauma can be evaluated using a single novel measure.
Level of Evidence:
Level III for Prognostic/Epidemiological Studies
Keywords: Latent class analysis, Medicare, Blunt Trauma, Delphi technique, Geriatrics
BACKGROUND
Injury is a leading cause of death and disability among adults over the age of 65.1,2 Each year over 2.7 million Emergency Department (ED) visits and 48,000 deaths due to injury occur in the US alone.3 The system of care developed around trauma - from ambulance services and EDs to intensive care units and rehabilitation centers - reduces injury-related death and disability.4–6 Triage protocols prior to hospital arrival emphasize that older adults have an increased risk of death from injury, yet this population continues to be less likely than younger patients to be transported to a specialized trauma center and has higher rates of morbidity and mortality over the course of their injury.7–9 The acute care of injured older adults is complicated by comorbid conditions, polypharmacy, and pre-existing functional and cognitive impairments.10,11 As a result, higher injury mortality12 and complication rates occur when compared with younger patients with similar injuries.9 Additionally, practice guidelines, available resources, and the existence, or dearth, of specialists, may significantly impact care decisions for injured older adults, especially when it comes to withdrawal of care or end-of-life decision-making.13–20
End-of-life research has shown that patients across a number of diagnoses (e.g., hip fracture, cancer, myocardial infarction) did not see improved outcomes with increased healthcare spending or increased levels of care.14,16,21,22 Even when short-term increases in survival were found, these benefits decreased over time.16 This may not be true in all acute conditions, however, with early, aggressive treatment decreasing mortality in sepsis and stroke patients.23,24 Currently, little evidence exists showing whether trauma patients benefit from a high intensity of care over their hospital course, with existing research focused almost exclusively end-of-life care.25,26 As evidenced by Silber et al. in their evaluation of surgical aggressiveness and outcomes, looking at all patients irrespective of whether or not they are perceived to be near the end of life may provide a different story on the relationship between intensity and survival.27,28 Using this conceptual framework, we therefore set out to estimate the relationship between intensity of care, utilization, and health outcomes in the older adult trauma population.
Current measures of care intensity include days hospitalized, costs, and procedures (e.g., mechanical ventilation, dialysis) performed within the months before death.21,22,29–33 While applicable to patients with chronic and/or terminal illnesses, trauma may require a unique approach. The unplanned nature of injury may result in a greater intensity of care delivered with limited time to plan for the terminal phase of disease.34,35 Additionally, the use of a lookback period when evaluating healthcare utilization has been questioned given that utilization for patients who survive are not estimated and no two patients enter the time period in the same health state.36 The location of intensity on the causal pathway between injury and survival is also unknown, as are the moderating roles of pre-existing conditions and severity of illness. In much the same way Elixhauser37 or Charlson38 provide insight into comorbidities, a “global” classification of intensity could provide insight into the care delivered after injury since each intervention may trigger or prevent future interventions and impact the overall recovery of the patient.
This focus on intensity allowed for expansion beyond care delivered at the “end-of-life” to care delivered after trauma for both survivors and decedents, thus shifting the focus from patients who died to the evaluation of resource utilization in all older adult trauma patients. We developed a metric to categorize intensity of care using procedure codes and patient information available in Medicare claims. We identified the clinical phenotypes for each class of intensity of care and subgroups receiving higher intensity care. We validated these findings in a separate cohort of injured Medicare patients.
METHODS
Data
We used 2013–2014 Medicare Provider Analysis and Review (MedPAR) research identifiable file claims from The Centers for Medicare and Medicaid Services (CMS) to identify inpatient stays. Demographic data was obtained from the CMS Master Beneficiary Summary File, while date of death came from the Enrollment Database. All analyses were conducted using Stata 15 (Stata Corp, College Station, TX). We followed the STROBE checklist for observational studies. This study was approved for expedited review by the Institutional Review Boards at University of Pennsylvania and Thomas Jefferson University.
Population
Medicare beneficiaries aged 65 and older, with fee-for-service coverage, and with admission to a U.S. hospital for primary or secondary diagnosis of blunt trauma were included for analysis. For the purposes of our study, blunt trauma is defined as ICD-9-CM codes 800–959, excluding codes 905–909 (late effects of injury), 930–939 (foreign bodies), 940–949 (burns), and 958 (complications of injury).39 Index encounters for injuries admitted through the emergency department for an inpatient stay were included for analysis and transfers to a second hospital were retained if both stays resulted in admissions. Beneficiaries could have more than one injury (case) in the dataset if discharge occurred prior to the second case and both injuries resulted in unique inpatient stays. Injury severity score40 (ISS) was calculated from ICD-9-CM diagnosis codes using the ICDPIC package for Stata 1541 and patients with moderate and severe injuries (ISS ≥ 9) included. Treat-and-release visits were excluded, as were any visits where the patient did not survive to inpatient admission. Cases due to penetrating injuries, poisonings, or drownings were also excluded. All cases meeting inclusion criteria for the study were included with 80% randomized to a development cohort and 20% for validation.
Defining Intensity of Care Using a Modified Delphi Method
A modified Delphi Method42 was used to determine a final set of interventions and procedures (procedures) used to determine intensity of care. An initial list of medical procedures was identified through review of the end-of-life, intensity of care, trauma, and emergency medicine literature. Key informant interviews with trauma, surgical critical care, and emergency medicine physicians, as well as presentations at research meetings to trauma, surgical critical care, and emergency medicine faculty and staff were also completed to solicit feedback on the list for inclusion. Content area experts were then asked to evaluate and provide feedback on which procedures to include in the final metric.
Latent Class Analysis
A latent class model was estimated for the development cohort based on medical procedures, elicited during the modified Delphi, and intensive care unit (ICU) length of stay (LoS). These intensity of care factors were identified from variables documented in MedPAR claims using total ICU days and ICD-9-CM procedure codes. Procedures were identified in both index and transfer admissions for all beneficiaries using ICD-9-CM procedure codes. Each medical procedure was entered into the model as a dichotomous variable (yes/no), with ICU LoS included as three levels to reflect resource utilization seen previously in elderly trauma patients (0 days, 1–7 days, 7+ days).43 The appropriate number of classes were determined using Akaike and Bayesian Information Criteria (AIC and BIC, respectively).44 Non-modifiable beneficiary-level demographic and injury characteristics were then adjusted for in the final model. To allow for assignment of intensity class to all cases, mean values (continuous variables) and most common value (binary variables) were used in place of missing covariates. An additional covariate to identify beneficiaries with imputed data was also included in the model.
Expert adjudication (trauma, surgical critical care, and emergency department clinicians) was used to identify and label the intensity (low, moderate, high, etc.) of each latent class based on the proportion of cases having each procedure and the phenotype derived from cases in that class having had a single or combined set of procedures and/or ICU LoS. Classes were estimated using the development cohort. The latent class model was then calculated for all cases in the validation cohort. Proportions of the validation cohort in each class, as well as procedures, were calculated and compared to the development cohort.
RESULTS
Population
A total of 683,398 unique hospital admissions (652,641 unique beneficiaries) with moderate and severe injury were included in the analysis. Of the total population, 68% (n=441,197) were female, 91% white (n=591,067), and the mean age was 82.5 years (standard deviation (SD): 8.4). Approximately 80% (n=543,154) of cases involved a fall, with motor vehicle crashes accounting for only 3% (n=20,689). The median ISS was 9 (IQR: 9–10), and almost one-fifth (n=131,073) had a head injury with an abbreviated injury score (AIS) of 3 or more. Of all admissions, 30% were treated at a level I/II trauma center, with additional summary statistics for the overall population and stratified by development (80%, n=546,718) and validation (20%, n=136,680) cohorts in Table 1.
Table 1.
Characteristics of US Medicare beneficiaries with hospital admission for primary or secondary diagnosis of blunt trauma, 2013 – 2014
| Total | Development Cohort | Validation Cohort | |
|---|---|---|---|
|
| |||
| Unique Admissions, n (%) | 683,398 (100.0) | 546,718 (80.0) | 136,680 (20.0) |
|
| |||
| Unique Beneficiaries, n (%) | 652,641 (95.5) | 526,682 (96.3) | 135,391 (99.1) |
|
| |||
| Beneficiary Characteristics a | |||
| Sex, n (%) | |||
| Female | 441,197 (67.6) | 356,284 (67.7) | 91,443 (67.5) |
| Male | 211,444 (32.4) | 170,284 (32.3) | 43,948 (32.5) |
| Race, n (%) | |||
| White | 591,067 (90.6) | 476,865 (90.5) | 122,775 (90.7) |
| Black | 29,760 (4.6) | 24,021 (4.6) | 6,134 (4.5) |
| Other | 31,814 (4.9) | 25,796 (4.9) | 6,482 (4.8) |
| Age in years, mean (SD) | 82.5 (8.4) | 82.5 (8.3) | 82.5 (8.3) |
| Elixhauser Comorbidity Score, median (IQR) | 3 (2 – 4) | 3 (2 – 4) | 3 (2 – 4) |
|
| |||
| Injury Characteristics b | |||
| Injury Severity Score, median (IQR) | 9 (9 – 10) | 9 (9 – 10) | 9 (9 – 10) |
| Max Abbreviated Injury Score, mean (SD) | 3.0 (0.7) | 3.0 (0.7) | 3.0 (0.7) |
| Abbreviated Injury Score Head 3+, n (%) | 131,073 (19.2) | 104,809 (19.2) | 26,264 (19.2) |
| Mechanism of Injury, n (%) | |||
| Fall | 543,154 (79.5) | 434,783 (79.5) | 108,371 (79.3) |
| Motor Vehicle Crash | 20,689 (3.0) | 16,519 (3.0) | 4,170 (3.1) |
| Other | 49,439 (7.2) | 39,573 (7.2) | 9,866 (7.2) |
| Missing | 70,116 (10.3) | 55,843 (10.2) | 14,273 (10.4) |
| Treated at Level I/II Trauma Center, n (%) | 204,359 (30.9) | 163,508 (30.9) | 40,851 (31.0) |
| Distance to Nearest Trauma Center in miles, median (IQR) | 13.4 (5.9 – 33.6) | 13.4 (5.9 – 33.7) | 13.4 (5.9 – 33.5) |
Beneficiary characteristics are calculated based on the total number of unique beneficiaries
Injury characteristics are calculated based on the total number of unique admissions for moderate and severe injury
Modified Delphi Method
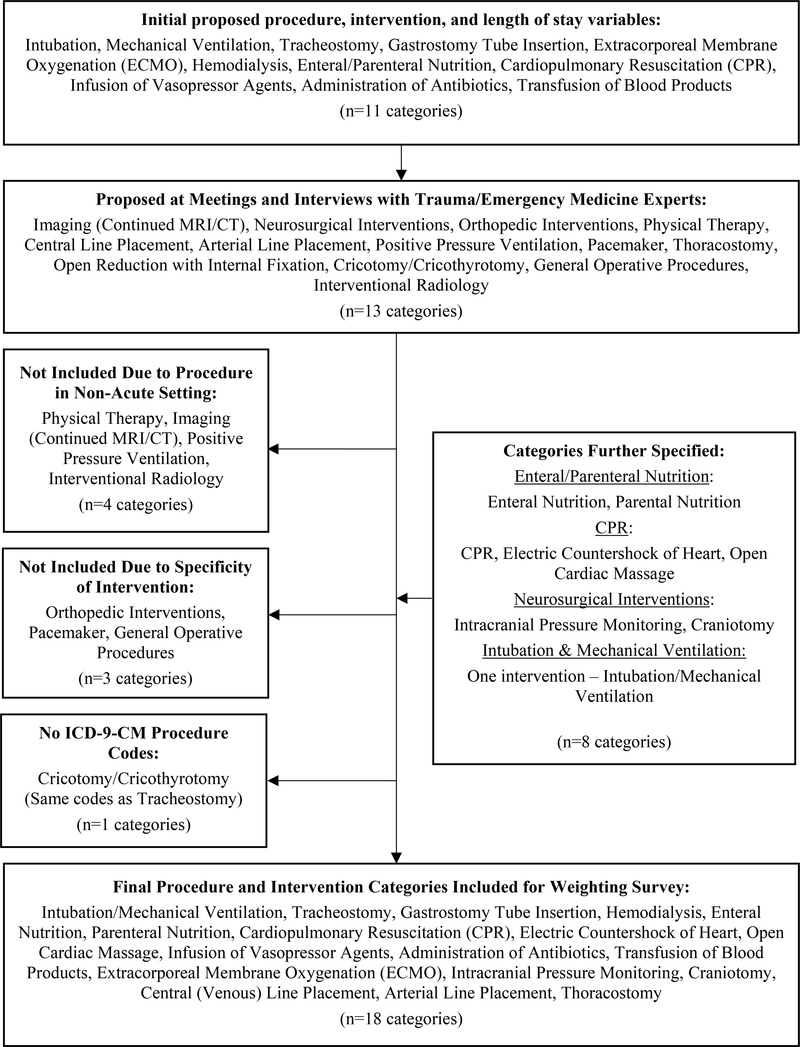
Eleven categories of medical procedures were initially identified, focused mainly on life-sustaining interventions. This list was presented to approximately 50 trauma, surgical critical care, and emergency medical professionals over the course of three separate, regularly scheduled research meetings. Eight additional categories of procedures were proposed for inclusion, ranging from surgical interventions to surveillance measures and rehabilitation. A final list of 18 intervention and procedure categories were identified (Figure 1 with ICD-9-CM procedure codes in Supplemental Table 1).
Figure 1.
Inclusion and exclusion of interventions/procedures for Latent Class Analysis
Latent Class Analysis
Using the Akaike and Bayesian Information Criterion, three classes were assigned based on inclusion of the 18 procedures and ICU LoS using the development cohort (AIC: 27824.28, BIC: 28514.09) (Supplemental Table 2), and demographic and injury characteristics were then incorporated into the three-class model. Of the 546,718 unique cases in the development cohort final model, 73% were assigned to class 1, 23% to class 2, and 3% to class 3 (n= 401,040, 127,025, and 18,653, respectively.) Independent expert adjudication by two critical care physicians assigned high intensity of care to the class with the lowest proportion of cases, low intensity to the largest group, and moderate to the remaining class based on underlying commonalities in procedures, ICU length of stay, demographics, and injury characteristics.
Transfusion of blood products had the highest proportion of patients in the low intensity class, while intubation/mechanical ventilation, dialysis, craniotomy, and venous catheter placement were highest in the moderate. All other interventions and procedures had the highest proportion of beneficiaries in the high intensity class (Table 2). No ICU admission was most common in low intensity class (n=390,943), with 1–7 days highest for moderate intensity beneficiaries, and almost an equal number of moderate and high intensity beneficiaries having greater than seven days length of ICU stay.
Table 2.
Proportion of development cohort cases in each latent class with intervention or procedure of interest
| Low Intensity | Moderate Intensity | High Intensity | Totala | |
|---|---|---|---|---|
|
| ||||
| Proportion in Class, n (%) | 401,040 (74.28) | 127,025 (23.23) | 18,653 (3.41) | 546,718 (100.00) |
|
| ||||
| Interventions/Procedures, n (%) | ||||
| Intubation/Mechanical Ventilation | 0 (0.00) | 16,959 (50.60) | 16,557 (49.40) | 33,516 (6.13) |
| Tracheostomy | 0 (0.00) | 0 (0.00) | 3,770 (100.00) | 3,770 (0.69) |
| Gastrostomy Tube Placement | 1 (<0.1) | 2,571 (37.39) | 4,306 (62.61) | 6,877 (1.26) |
| Hemodialysis | 18 (0.06) | 18,872 (68.07) | 8,834 (31.86) | 27,724 (5.07) |
| Enteral Nutrition | 0 (0.00) | 1,653 (30.38) | 3,788 (69.62) | 5,441 (1.00) |
| Parenteral Nutrition | 0 (0.00) | 891 (49.12) | 923 (50.88) | 1,814 (0.33) |
| CPR | 0 (0.00) | 697 (20.34) | 2,729 (79.66) | 3.426 (0.63) |
| Electric Countershock of Heart | 104 (8.04) | 558 (43.12) | 632 (48.84) | 1,294 (0.24) |
| Open Cardiac Massage | 0 (0.00) | 0 (0.00) | 43 (100.00) | 43 (0.01) |
| Vasopressors | 0 (0.00) | 679 (27.57) | 1,784 (72.43) | 2,463 (0.45) |
| Administration of Antibiotics | 2,604 (60.39) | 1,218 (28.25) | 490 (11.36) | 4,312 (0.79) |
| Transfusion of Blood Products | 103,333 (69.48) | 36,273 (24.39) | 9,113 (6.13) | 148,719 (27.20) |
| ECMO | 0 (0.00) | 93 (43.06) | 123 (56.94) | 216 (0.04) |
| ICP Monitoring | 0 (0.00) | 535 (38.94) | 839 (61.06) | 1,374 (0.25) |
| Craniotomy | 0 (0.00) | 1,180 (68.01) | 555 (31.99) | 1,735 (0.32) |
| Central Venous Catheterization | 405 (3.37) | 6,913 (57.45) | 4,715 (39.18) | 12,033 (2.20) |
| Arterial Line Placement | 0 (0.00) | 1,694 (24.93) | 5,101 (75.07) | 6,795 (1.24) |
|
| ||||
| ICU Length of Stay, n (%) | ||||
| No ICU Stay | 390,943 (83.17) | 68,868 (14.65) | 10,234 (2.18) | 470,045 (85.98) |
| ICU Stay ≤7 Days | 10,097 (15.46) | 52,423 (80.26) | 2,800 (4.29) | 65,320 (11.95) |
| ICU Stay >7 Days | 0 (0.00) | 5,734 (50.51) | 5,619 (49.49) | 11,353 (2.08) |
Percentages are row percentages for intensity classes and percentage of total cohort in total column
Phenotypes
Of the ten most common phenotypes for cases in the high intensity class, all included intubation/mechanical ventilation (I/MV), and this intervention combined with dialysis, transfusion of blood products, and/or ICU length of stay greater than 7 days accounted for over 5% of all cases receiving high intensity care (Table 3). For those with low intensity of care, no procedures (of the 18 measured) and no ICU stay was most common. An ICU stay of 1–7 days accounted for approximately 23% of beneficiaries in the moderate class, with another 20% having no procedures or ICU stay. Table 4 shows the differences in demographics and injury characteristics between the classes.
Table 3.
Phenotypes of cases by intensity of care class for the development cohort
| Phenotype Rank | Low Intensity | % | Moderate Intensity | % | High Intensity | % |
|---|---|---|---|---|---|---|
|
| ||||||
| 1 | No Interventions/Procedures or ICU Stay | 286,139 (71.35) | ICU Stay 1–7 Days | 28,718 (22.61) | Intubation/Mechanical Ventilation (I/MV), Dialysis, Transfusion of Blood Products (Blood) | 386 (2.07) |
| 2 | Blood | 99,103 (24.71) | No Procedures or ICU Stay | 25,373 (19.97) | I/MV, Dialysis, ICU stay >7 days (ICU>7) | 300 (1.61) |
| 3 | ICU Stay 1–7 Days | 7,242 (1.81) | Blood, ICU Stay 1–7 Days | 10,433 (8.21) | I/MV, CPR | 298 (1.60) |
| 4 | Blood, ICU 1–7 Days | 2,827 (0.70) | Dialysis | 6,997 (5.51) | I/MV, Dialysis, Arterial Line Placement | 284 (1.52) |
| 5 | Thoracostomy | 2,407 (0.60) | Blood | 6,892 (5.43) | I/MV, Blood, ICU>7 | 263 (1.41) |
| 6 | Antibiotics Administration | 1,584 (0.39) | I/MV | 6,082 (4.79) | I/MV, Dialysis, Blood, ICU>7 | 249 (1.33) |
| 7 | Blood, Antibiotics Administration | 980 (0.24) | Dialysis, Blood | 4,331 (3.41) | I/MV, Blood, Venous Catheter Placement | 226 (1.21) |
| 8 | Venous Catheter Placement | 221 (0.06) | I/MV, ICU Stay 1–7 Days | 2,730 (2.15) | I/MV, Arterial Line Placement | 193 (1.03) |
| 9 | Blood, Thoracostomy | 191 (0.05) | ICU >7, Blood | 2,435 (1.92) | I/MV, ICU>7 | 188 (1.01) |
| 10 | Blood, Venous Catheter | 184 (0.05) | Thoracostomy | 2,329 (1.83) | I/MV, Dialysis | 182 (0.98) |
Table 4.
Characteristics of cases by intensity of care class for the development cohort
| Low Intensity | Moderate Intensity | High Intensity | |
|---|---|---|---|
|
| |||
| Demographics | |||
| Sex, n (%) | |||
| Female | 297,235 (74.12) | 65,236 (51.36) | 7,827 (41.96) |
| Male | 103,805 (25.88) | 61,789 (48.64) | 10,826 (58.04) |
| Race, n (%) | |||
| White | 370,231 (92.32) | 108,982 (85.80) | 15,860 (85.03) |
| Non-White | 30,809 (7.68) | 18,043 (14.20) | 2,793 (14.97) |
| Age in years, mean (SD) | 83.26 (8.22) | 80.94 (8.30) | 78.26 (7.91) |
| Elixhauser Comorbidity Score, median (IQR) | 3 (2 – 4) | 4 (2 – 5) | 3 (2 – 5) |
| Discharge Disposition | |||
| Home | 72,054 (17.97) | 32,271 (25.41) | 1,121 (6.01) |
| Rehabilitation Facility | 56,619 (14.12) | 15,797 (12.44) | 1,914 (10.26) |
| Death/Hospice | 14,817 (3.69) | 18,015 (14.18) | 8,158 (43.74) |
| Skilled Nursing Facility | 248,383 (61.93) | 58,133 (45.77) | 6,948 (37.25) |
| Other | 9,167 (2.29) | 2,809 (2.21) | 512 (2.74) |
|
| |||
| Injury Characteristics | |||
| Injury Severity Score, median (IQR) | 9 (9 – 9) | 13 (9 – 16) | 14 (9 – 18) |
| Max Abbreviated Injury Score, mean (SD) | 2.92 (0.60) | 3.34 (0.72) | 3.39 (0.76) |
| Abbreviated Injury Score Head 3+, n (%) | 37,148 (9.26) | 58,953 (46.41) | 8,708 (46.68) |
| Mechanism of Injury, n (%) | |||
| Fall | 335,662 (83.70) | 89,476 (70.44) | 9,645 (51.71) |
| Other | 65,378 (16.30) | 37,549 (29.56) | 9,008 (48.29) |
| Index Treatment at Level I/II Trauma Center, n (%) | 101,667 (25.35) | 51,624 (40.64) | 10,217 (54.77) |
| Distance to Nearest Trauma Center in miles, median (IQR) | 15.50 (6.41 – 33.11) | 12.95 (5.66 – 28.14) | 14.08 (5.08 – 30.45) |
| Urban residential zip code | 338,488 (84.40) | 110,626 (87.09) | 15,758 (84.48) |
| Missing one or more variables, n (%) | 34,144 (8.51) | 9,220 (7.26) | 1,588 (8.51) |
As intensity increased, the proportion of cases that were male and white decreased. The median ISS of the high intensity class was 14 (IQR 9–18) compared with 9 (9–9) in low and 13 (9–16) in moderate. In the high intensity class, fewer injuries were caused by falls (n=9,645, 52% vs n=89,476, 70% in moderate; 335,662, 84% in low), and a greater proportion of cases (55% vs 41% and 25%, respectively) were initially triaged to trauma centers for treatment. Death or discharge to hospice was highest in the high intensity cohort (n=8,158 44%), while discharge to a skilled nursing facility was highest in the low intensity cohort (n=248,3838, 62%).
Validation
The class assignment in the validation cohort was similar to that in the development cohort. Of the 136,680 beneficiaries, 3% (n=4,658) were assigned to the high intensity class, with 24% (n=32,536) to moderate and the remainder to low (Supplemental Table 3). The proportion of cases with each procedure were the same as in the development cohort with limited procedures present in the low intensity cohort (antibiotics, transfusions, catheterization) and short (≤7 Days) or no ICU stay. The exception of electric countershock of the heart, which had a higher proportion of cases (59%, n=203) assigned to the moderate intensity class (development cohort: 43%, n=558).
DISCUSSION
Using a variety of interventions and procedures combined with demographic and injury information available in Medicare data, we found that approximately 4% of older adults with moderate or severe blunt trauma received high intensity care. We identified commonalities between cases, even given the heterogeneity of injury and care delivered. The combination of interventions, procedures, and length of ICU stay defined the high intensity of care class with greater precision than a sum of the number of procedures, suggesting that the type of care may play more of a role than the total procedure count.
Without a current gold standard, the use of a modified Delphi method allowed for development of a single metric for assessment of care intensity. Prior work by Lilley, et. al., and Barnato, et. al., have shown the association between many of the procedures we evaluated and intensity of care.16,45 However, these measures have not been applied to an older adult blunt trauma population, and the lack of a composite measure, especially one that can be used with administrative and claims data, means that the evaluating intensity beyond the measurement of individual procedures continues to be limited. The use of both latent class analysis to identify unique groups and the classes identified in this paper offer a starting point for evaluating intensity of care in younger populations, those with penetrating trauma, and other trauma subgroups given its flexibility to adapt to the data provided. Given this, our metric can be applied to hospital quality benchmarking to evaluate the effectiveness of high intensity care delivered throughout hospital admission. This builds on prior trauma risk adjustment models that look at in-hospital mortality and its drivers.46,47 A composite measure of intensity may help provide a more comprehensive understanding of how the case-mix of trauma patients, and the care delivered at both trauma and non-trauma centers throughout the US, drive quality outcomes such as in-hospital and 30-day mortality. However, understanding the causal pathway between intensity and mortality may also require further exploration of the role of patient level factors (pre-existing conditions, patient preferences), hospital-level factors (service lines, norms), and community-level factors (availability of services, resources).
Beneficiaries who received higher intensity care were more likely to be male, non-white, and younger. These findings are similar to those seen in other patient cohorts near the end of life31 and suggest that underlying demographic differences persist in the care level delivered to those who are severely ill.26,48 Medicare beneficiaries with higher intensity of care were also less likely to have a fall as their mechanism of injury, suggesting that while falls may make up over two-thirds of injury in older adults,3 other mechanisms may make a greater contribution to increased care requirements and utilization of services. Additionally, while beneficiaries in the lower two intensity classes still received a number of the procedures of interest, including ICU stays, these were limited and tended to reflect procedures commonly seen as less aggressive (e.g., dialysis, blood products). Hospital-level analyses may highlight additional drivers of variability and provide insight into the impact programming plays in overall intensity of care, including the use of geriatric consultations and palliative care programs.49,50 Additionally, exploration of whether differences in intensity is a result of early mortality, less severe injury, or other beneficiary-level factors is required.
Limitations and Next Steps
This study used administrative and claims data resulting in predefined data points and limited our ability to fully determine some aspects of care intensity including administration and duration of medication, timing or duration of interventions or procedures, distinguishing services delivered for acute need versus chronic conditions, and patient/family/surrogate decisions surrounding care. However, the use of claims data, and specifically CMS data, allows for capture of standardized information on all beneficiaries providing a representative picture of intensity of care across the United States. This dataset enabled us to create a measure of intensity that utilized readily available data to measure intensity of care at the administrative level instead of requiring time-consuming and expensive approaches, such as electronic health record abstraction. A second limitation is that cases may only receive procedures for which they have an indication, (e.g., dialysis for those with kidney failure). However, given the focus on moderate and severely injured older adults, each beneficiary is “at risk” for all procedures beginning at the time of their injury, especially given the possibility of complications or decline in health status. We chose to measure an overall intensity of care, as opposed to intensity of care adjusted for indication for each procedure, to allow for determination of the total care delivered for each case allowing differences in the type, count, and combination of procedures.
Conclusions
This study measured the intensity of care delivered to older adults with blunt trauma. Using 18 interventions and procedures, along with intensive care unit length of stay, we were able to assign Medicare beneficiaries to low, moderate, and high intensity classes, and estimate their probability of receiving high intensity care. The inclusion of intubation/mechanical ventilation was a key component of high intensity care, and it was often combined with additional interventions and procedures, as well as days in the intensive care unit. This metric can be used to assess variability in care intensity at the hospital level and to estimate the association of high intensity care with patient-level outcomes.
Supplementary Material
Acknowledgements
We thank David Buckler, MUSA, and David Karp, MUSA, for assistance with developing the trauma cohort from the 2013 and 2014 CMS claims data.
Source of Funding: The data source for this study was funded by the Agency for Healthcare Research and Quality (R01HS023614-01) and the NHLBI (R01HL141841-01) (PI: Carr). Dr. Holena was supported by NIH training award K08HL131995. The contents of this study are solely the responsibility of the authors and do not necessarily reflect the views of the Agency for Healthcare Research and Quality, the National Institutes of Health, or the U.S. Department of Health and Human Services.
Footnotes
Conflicts of Interest: While conducting this research Dr. Carr spent a portion of his time as the Director of the Emergency Care Coordination Center in the US Department of Health & Human Services. These contents are solely the responsibility of the authors and do not necessarily reflect the views of the U.S. Department of Health and Human Services.
Meeting Presentations: A portion of this work was presented at the 2019 Academy Health Annual Research Meeting.
References
- 1.Sise RG, Calvo RY, Spain DA, Weiser TG, Staudenmayer KL. The epidemiology of trauma-related mortality in the United States from 2002 to 2010. J Trauma Acute Care Surg. 2014;76(4):913–919; discussion 920. [DOI] [PubMed] [Google Scholar]
- 2.Corso P, Finkelstein E, Miller T, Fiebelkorn I, Zaloshnja E. Incidence and lifetime costs of injuries in the United States. Inj Prev. 2006;12(4):212–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.CDC. Injury Prevention & Control: Data & Statistics (WISQARSTM: Web-based Injury Statistics Query and Reporting System). 2015.
- 4.Van Aalst JA MJJ, Yates KH, Miller RS, Bass SM. Severely Injured Geriatric Patients Return to Independent Living:: A Study of Factors Influencing Function and Independence. J. Trauma Acute Care Surg. 1991;31(8):1096–1102. [PubMed] [Google Scholar]
- 5.Chalfin DB, Trzeciak S, Likourezos A, Baumann BM, Dellinger RP, group D-Es. Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med. 2007;35(6):1477–1483. [DOI] [PubMed] [Google Scholar]
- 6.Grossman M, Scaff DW, Miller D, Reed J 3rd, Hoey B, Anderson HL 3rd. Functional outcomes in octogenarian trauma. J Trauma. 2003;55(1):26–32. [DOI] [PubMed] [Google Scholar]
- 7.Nakamura Y, Daya M, Bulger EM, Schreiber M, Mackersie R, Hsia RY, Mann NC, Holmes JF, Staudenmayer K, Sturges Z, et al. Evaluating Age in the Field Triage of Injured Persons. Ann. Emerg. Med. 2012;60(3):335–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chang DC, Bass RR, Cornwell EE, Mackenzie EJ. Undertriage of elderly trauma patients to state-designated trauma centers. Arch Surg. 2008;143(8):776–781; discussion 782. [DOI] [PubMed] [Google Scholar]
- 9.Richmond TS, Kauder D, Strumpf N, Meredith T. Characteristics and outcomes of serious traumatic injury in older adults. J Am Geriatr Soc. 2002;50(2):215–222. [DOI] [PubMed] [Google Scholar]
- 10.Neideen T, Lam M, Brasel KJ. Preinjury beta blockers are associated with increased mortality in geriatric trauma patients. J Trauma. 2008;65(5):1016–1020. [DOI] [PubMed] [Google Scholar]
- 11.Hwang U, Morrison RS. The geriatric emergency department. J Am Geriatr Soc. 2007;55(11):1873–1876. [DOI] [PubMed] [Google Scholar]
- 12.Rogers FB, Osler TM, Shackford SR, Morrow PL, Sartorelli KH, Camp L, Healey MA, Martin F. A population-based study of geriatric trauma in a rural state. J Trauma. 2001;50(4):604–609; discussion 609–611. [DOI] [PubMed] [Google Scholar]
- 13.Truog RD, Campbell ML, Curtis JR, Haas CE, Luce JM, Rubenfeld GD, Rushton CH, Kaufman DC, American Academy of Critical Care M. Recommendations for end-of-life care in the intensive care unit: a consensus statement by the American College [corrected] of Critical Care Medicine. Crit Care Med. 2008;36(3):953–963. [DOI] [PubMed] [Google Scholar]
- 14.Angus DC, Barnato AE, Linde-Zwirble WT, Weissfeld LA, Watson RS, Rickert T, Rubenfeld GD, Robert Wood Johnson Foundation ICUE-O-LPG. Use of intensive care at the end of life in the United States: an epidemiologic study. Crit Care Med. 2004;32(3):638–643. [DOI] [PubMed] [Google Scholar]
- 15.Baggs JG, Schmitt MH, Prendergast TJ, Norton SA, Sellers CR, Quinn JR, Press N. Who is attending? End-of-life decision making in the intensive care unit. J Palliat Med. 2012;15(1):56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barnato AE, Chang CC, Farrell MH, Lave JR, Roberts MS, Angus DC. Is survival better at hospitals with higher “end-of-life” treatment intensity? Med Care. 2010;48(2):125–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carr BG, Bowman AJ, Wolff CS, Mullen MT, Holena DN, Branas CC, Wiebe DJ. Disparities in access to trauma care in the United States: A population-based analysis. Injury. 2017;48(2):332–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Larochelle MR, Rodriguez KL, Arnold RM, Barnato AE. Hospital staff attributions of the causes of physician variation in end-of-life treatment intensity. Palliat Med. 2009;23(5):460–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gordy S, Klein E. Advance directives in the trauma intensive care unit: Do they really matter? Int J Crit Illn Inj Sci. 2011;1(2):132–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ishihara KK, Wrenn K, Wright SW, Socha CM, Cross M. Advance directives in the emergency department: too few, too late. Acad Emerg Med. 1996;3(1):50–53. [DOI] [PubMed] [Google Scholar]
- 21.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 2: health outcomes and satisfaction with care. Ann Intern Med. 2003;138(4):288–298. [DOI] [PubMed] [Google Scholar]
- 22.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 1: the content, quality, and accessibility of care. Ann Intern Med. 2003;138(4):273–287. [DOI] [PubMed] [Google Scholar]
- 23.Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M, Early Goal-Directed Therapy Collaborative G. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345(19):1368–1377. [DOI] [PubMed] [Google Scholar]
- 24.Hacke W, Donnan G, Fieschi C, Kaste M, von Kummer R, Broderick JP, Brott T, Frankel M, Grotta JC, Haley EC Jr., et al. Association of outcome with early stroke treatment: pooled analysis of ATLANTIS, ECASS, and NINDS rt-PA stroke trials. Lancet. 2004;363(9411):768–774. [DOI] [PubMed] [Google Scholar]
- 25.Lilley EJ, Scott JW, Weissman JS, Krasnova A, Salim A, Haider AH, Cooper Z. End-of-Life Care in Older Patients After Serious or Severe Traumatic Brain Injury in Low-Mortality Hospitals Compared With All Other Hospitals. JAMA Surg. 2018;153(1):44–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cooper Z, Rivara FP, Wang J, MacKenzie EJ, Jurkovich GJ. Racial disparities in intensity of care at the end-of-life: are trauma patients the same as the rest? J Health Care Poor Underserved. 2012;23(2):857–874. [DOI] [PubMed] [Google Scholar]
- 27.Silber JH, Kaestner R. Response to Commentaries on Silber et al.: Aggressive Treatment Styles and Surgical Outcomes. Health Serv Res. 2010;45(6):1908–1911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Silber JH, Kaestner R, Even-Shoshan O, Wang Y, Bressler LJ. Aggressive treatment style and surgical outcomes. Health Serv Res. 2010;45(6 Pt 2):1872–1892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Barnato AE, Farrell MH, Chang CC, Lave JR, Roberts MS, Angus DC. Development and validation of hospital “end-of-life” treatment intensity measures. Med Care. 2009;47(10):1098–1105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Earle CC, Neville BA, Landrum MB, Souza JM, Weeks JC, Block SD, Grunfeld E, Ayanian JZ. Evaluating claims-based indicators of the intensity of end-of-life cancer care. Int J Qual Health Care. 2005;17(6):505–509. [DOI] [PubMed] [Google Scholar]
- 31.Miesfeldt S, Murray K, Lucas L, Chang CH, Goodman D, Morden NE. Association of age, gender, and race with intensity of end-of-life care for Medicare beneficiaries with cancer. J Palliat Med. 2012;15(5):548–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Thorpe KE, Howard DH. The rise in spending among Medicare beneficiaries: the role of chronic disease prevalence and changes in treatment intensity. Health Aff (Millwood). 2006;25(5):w378–388. [DOI] [PubMed] [Google Scholar]
- 33.Wong SP, Kreuter W, O’Hare AM. Treatment intensity at the end of life in older adults receiving long-term dialysis. Arch Intern Med. 2012;172(8):661–663; discussion 663–664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.The SUPPORT Principal Investigators. A controlled trial to improve care for seriously ill hospitalized patients. The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT). JAMA. 1995;274(20):1591–1598. [PubMed] [Google Scholar]
- 35.Murray SA, Kendall M, Boyd K, Sheikh A. Illness trajectories and palliative care. BMJ. 2005;330(7498):1007–1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bach PB, Schrag D, Begg CB. Resurrecting treatment histories of dead patients: a study design that should be laid to rest. JAMA. 2004;292(22):2765–2770. [DOI] [PubMed] [Google Scholar]
- 37.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. [DOI] [PubMed] [Google Scholar]
- 38.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. [DOI] [PubMed] [Google Scholar]
- 39.MacKenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, Salkever DS, Scharfstein DO. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354(4):366–378. [DOI] [PubMed] [Google Scholar]
- 40.Baker SP, O’Neill B, Haddon W Jr., Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14(3):187–196. [PubMed] [Google Scholar]
- 41.ICDPIC: Stata module to provide methods for translating International Classification of Diseases (Ninth Revision) diagnosis codes into standard injury categories and/or scores [computer program]. Boston College Department of Economics; 2009. [Google Scholar]
- 42.Humphrey-Murto S, Varpio L, Wood TJ, Gonsalves C, Ufholz LA, Mascioli K, Wang C, Foth T. The Use of the Delphi and Other Consensus Group Methods in Medical Education Research: A Review. Acad Med. 2017;92(10):1491–1498. [DOI] [PubMed] [Google Scholar]
- 43.Taylor MD, Tracy JK, Meyer W, Pasquale M, Napolitano LM. Trauma in the elderly: intensive care unit resource use and outcome. J Trauma. 2002;53(3):407–414. [DOI] [PubMed] [Google Scholar]
- 44.Nylund K, Asparouhov T, Muthen B. Deciding on the number of classes in latent class analysis and growth mixed modeling: A monte carlo simulation study. Struct. Equ. Model 2007;14(4). [Google Scholar]
- 45.Lilley EJ, Williams KJ, Schneider EB, Hammouda K, Salim A, Haider AH, Cooper Z. Intensity of treatment, end-of-life care, and mortality for older patients with severe traumatic brain injury. J Trauma Acute Care Surg. 2016;80(6):998–1004. [DOI] [PubMed] [Google Scholar]
- 46.Wiebe DJ, Holena DN, Delgado MK, McWilliams N, Altenburg J, Carr BG. The Pennsylvania Trauma Outcomes Study Risk-Adjusted Mortality Model: Results of a Statewide Benchmarking Program. Am Surg. 2017;83(5):445–452. [PMC free article] [PubMed] [Google Scholar]
- 47.Newgard CD, Fildes JJ, Wu LL, Hemmila MR, Burd RS, Neal M, Mann NC, Shafi S, Clark DE, Goble S, et al. Methodology and Analytic Rationale for the American College of Surgeons Trauma Quality Improvement Program. J Am Coll Surgeons. 2013;216(1):147–157. [DOI] [PubMed] [Google Scholar]
- 48.Hicks CW, Hashmi ZG, Velopulos C, Efron DT, Schneider EB, Haut ER, Cornwell EE 3rd, Haider AH. Association between race and age in survival after trauma. JAMA Surg. 2014;149(7):642–647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lilley EJ, Lee KC, Scott JW, Krumrei NJ, Haider AH, Salim A, Gupta R, Cooper Z. The impact of inpatient palliative care on end of life care among older trauma patients who die after hospital discharge. J Trauma Acute Care Surg. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Olufajo OA, Tulebaev S, Javedan H, Gates J, Wang J, Duarte M, Kelly E, Lilley E, Salim A, Cooper Z. Integrating Geriatric Consults into Routine Care of Older Trauma Patients: One-Year Experience of a Level I Trauma Center. J Am Coll Surg. 2016;222(6):1029–1035. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.