Abstract
Respiratory syncytial virus (RSV) is a common seasonal respiratory virus and an important cause of illness among infants, but the burden of RSV disease is not well described among the older population. The objective of this study was to estimate the age‐specific incidence of hospital admission among over 65 s due to respiratory illnesses attributable to RSV in England to inform optimal vaccine and therapeutic interventions.
We used linear multiple regression to examine the effect of changes in weekly counts of respiratory pathogens on the weekly counts of respiratory hospital admissions. The study population was all patients aged 65 years or over admitted to English hospitals between 2nd August 2010 and 30th July 2017.
RSV was estimated to account for a seasonal annual average of 71 (95% CI 52–90) respiratory admissions per 100 000 in adults age 65–74 and 251 (95% CI 186–316) admissions per 100,000 adults age 75+. Pneumococcus was the pathogen responsible for highest annual average respiratory admission with 448 (95% CI 310–587) admissions per 100,000 adults age 65–74 and 1010 (95% CI 527–1493) admissions per 100,000 adults aged 75+.
This study shows that RSV continues to exert a significant burden of disease among older adults in England. These findings will support development of policy for the use of RSV therapeutics and vaccines in this age group.
Keywords: burden of disease, hospital admission, respiratory, respiratory syncytial virus, time series analysis
1. INTRODUCTION
Respiratory syncytial virus (RSV) is a common seasonal respiratory virus and is recognized as an important cause of illness among infants but also increasingly amongst adults. 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 Understanding the impact of RSV on morbidity, mortality, and healthcare usage is important to inform public health policy. However, the burden of RSV disease is not well described among the older population. 10 RSV infection causes a similar clinical syndrome to many other viruses, including influenza; in this age group, 11 there is little routine diagnostic testing for respiratory viruses in many countries including England, and finally patients may present late with complications of infection when the virus is no longer detectable. There are many candidate RSV vaccines and therapeutics in advanced development. 12 , 13 , 14 , 15 Without a clear picture of the impact of RSV, we cannot fully appraise these options.
Existing surveillance data in England show seasonal peaks in RSV infection occurring with regularity usually around November, accompanied by autumn–winter peaks in other respiratory viruses such as influenza. Time series modelling offers tools to understand the role of seasonal respiratory viruses in driving hospital admissions and excess winter deaths due to respiratory disease. Multivariable regression analysis comparing the weekly variation in outcomes such as hospital admissions or primary care consultations, with variation in explanatory factors such as laboratory diagnoses of pathogens, allows us to model the proportion that could be attributable to each factor. Using routine healthcare and laboratory data from national administrative data systems, this approach has been used to measure the burden of seasonal infections such as rotavirus, 16 influenza, 17 , 18 RSV, 19 , 20 , 21 and other respiratory pathogens. 22 , 23 Fleming et al. 19 used influenza and RSV laboratory data between 1995 and 2009 and estimated that in elderly patients, RSV in England was comparable to influenza in terms of the burden of hospital admissions and deaths. Reeves et al. 20 used data on 10 different respiratory pathogens to model the cause‐specific burden of RSV disease in under 5‐year‐olds also in England.
1.1. Objective
The objective of this study was to estimate the age‐specific incidence of hospital admission among over 65 s due to respiratory illnesses attributable to RSV, in order to inform future intervention policies.
2. METHODS
We used linear multiple regression to examine the effect of changes in weekly counts of respiratory pathogens (independent variables) on the weekly counts of respiratory hospital admissions (dependent variable). The study population was all patients aged 65 years or over admitted to English hospitals between 2nd August 2010 and 30th July 2017.
UK laboratory data, including diagnoses of viral infections, is compiled using the Second‐Generation Surveillance System (SGSS). SGSS contains all positive results from diagnostic tests conducted in Public Health England (PHE), National Health Service (NHS), and private microbiology laboratories in England and Wales since 1990. Data collected includes specimen information, test type, patient identifiable information, and laboratory information. To account for repeated testing, identical results within 14 days of each other are grouped as a single episode of infection and assigned a unique organism‐patient‐illness‐episode identifier (OPIE ID). The coverage of SGSS is very high. PHE does not collect data on the ascertainment of RSV tests in SGSS, but studies considering the ascertainment of other clinically significant infections (e.g., blood‐stream infections, methicillin‐resistant Staphylococcus aureus) estimate ascertainment to be approximately 70%–90% and consistent all year round.
Hospital data in England are collected in the Hospital Episode Statistics (HES) database. The HES Admitted Patient Care Database contains information for all patients admitted to all NHS hospitals in England, and all patients treated in private hospitals paid for by the NHS. Data collected includes: clinical information including diagnoses (ICD‐10) and procedures, patient identifiable information, geographical information and administrative information including admission and discharge dates. Each entry in HES relates to an episode of care under a single consultant doctor. A “spell” is defined as the time between the admission and discharge episodes within a hospital, while a “continuous inpatient spell” (CIP) is the time from admission to final discharge, allowing for transfers between hospitals. We have seen a steady increase in healthcare usage in England, related to the ageing population and greater access to healthcare.
2.1. Laboratory data collection
For the laboratory data (SGSS), we selected all records of respiratory pathogens from English laboratories with a specimen date from 2nd August 2010 to 30th July 2017, including all age groups. The list of respiratory pathogens is presented in Table 1, along with the specimen sites and test methods included. We excluded records with the following recorded test methods: antibody detection, electron microscopy, light microscopy, and “unknown.” We checked records for specimen dates and age fields and removed records where this information was missing. We included only the first record for each OPIE ID. We then created tables of weekly counts of each pathogen and visually examined each time series.
TABLE 1.
Pathogens, specimen sites, and test methods included
| Pathogen | ||
|---|---|---|
| Viruses | RSV, influenza A, influenza B, rhinovirus, parainfluenza, human metapneumovirus (hMPV), adenovirus, coxsackievirus, rhinovirus, echovirus, enterovirus | |
| Bacteria | Streptococcus pneumoniae, Haemophilus influenzae, Mycoplasma pneumoniae, Klebsiella pneumoniae, Pseudomonas aeruginosa, Staphylococcus aureus, Streptococcus Group A, Streptococcus Group B, Escherichia coli, Chlamydia trachomatis, Bordetella pertussis, Legionella pneumophila | |
| Specimen sites | Pathogen | |
|---|---|---|
| Upper respiratory | Nose, throat, nasopharyngeal aspirate, per‐nasal, pharyngeal, upper respiratory tract | Viruses & pertussis |
| Lower respiratory | Alveolar lavage, bronchial, endotracheal, lower respiratory tract, lung, sputum, trachea, chest drain, pleural | All pathogens |
| Normally sterile site | Ascitic fluid, blood, cerebrospinal fluid | Bacteria (excluding pertussis) & enterovirus |
| Test method | ||
|---|---|---|
| Antigen detection, culture, and genomic/PCR/LCR detection | ||
2.2. Hospital data collection
For the hospital admissions data (HES), we considered one admission as one continuous inpatient spell (CIP). We selected admissions to English hospitals among patients aged 65 or older, with an admission date from 2nd August 2010 to 30th July 2017, with a primary diagnosis in the first episode of the first spell of a cardio‐respiratory disease (I00‐J99) or urinary tract infection (N39) (control). Only the primary diagnosis of the first episode of the spell was considered to avoid double counting of admissions that had two or more respiratory diagnoses. We cleaned the hospital data, examining the admission dates and age at start of admission and removing any entries where this information was missing. We also examined the admission method and removed any non‐emergency admissions. We counted admissions per week for each of the outcomes in Table 2. We then created tables of weekly counts of each outcome by age group (65–74 and 75+) and visually examined each time series.
TABLE 2.
Outcome groups and ICD 10 codes, demonstrating hierarchy
| Outcome | ICD 10 codes |
|---|---|
| • Cardiorespiratory disease | I00–J99 |
| • Respiratory disease | J00–J99 |
| • Influenza and pneumonia | J09–J18 |
| • Bronchitis, bronchiolitis and unspecified LRTI | J20–J22, J40 |
| • Chronic respiratory disease | J41–J47 |
| • Urinary tract infection (control) | N39 |
2.3. Data analysis
We included RSV in all models along with three “time variables”: (1) a secular trend (to account for an overall increase in admissions over the seven‐year study period), (2) a 1‐year period term (to account for unmeasured seasonal factors that contribute to hospital admissions), and (3) a categorical season term (to account for any step changes in testing practice and influenza activity by season), all three of which we found to improve the models. Then, we used a backward stepwise approach, starting with all pathogens then removing first those pathogens with negative coefficients (starting with the most negative) due to biological implausibility, then those with positive coefficients that did not contribute significantly to the model (starting with the coefficient with the largest p value). We assessed the effect of a lag of up to 4 weeks, first for RSV, then for the other remaining pathogens (starting with the coefficient with the smallest p value), checking the effect on each model and selecting the overall best lag for each pathogen to apply to all models. We explored the interaction between RSV and influenza A with pneumococcus and the removal of pneumococcus. We did not split influenza A into H1 and H3 subtypes as subtype data was not available. We assessed model fit using the Akaike information criterion (AIC) and the coefficient of determination (R 2). We fitted models to the control data using the same three “time variables” and same lag as other models.
We interpreted the coefficients for each pathogen as the number of admissions attributable to each case of infection. We calculated the number of weekly admissions attributable to each pathogen by multiplying the number of cases of each infection in the laboratory database by the coefficient for that pathogen, so for RSV in week n (RSVn), where β 1 is the model coefficient for RSV, the RSV attibutable admissions in week n is given by:
We calculated the upper and lower 95% confidence intervals by multiplying the number of cases by the upper and lower confidence interval estimates of the coefficients. We calculated the overall and seasonal number of admissions attributable to each pathogen by taking the sum of weekly admissions. We calculated the seasonal rate of admissions based on the average Office for National Statistics mid‐year population estimates for the 2 years either side of the season. We plotted time series showing the actual and expected weekly admissions, and the weekly admissions attributable to each pathogen. We conducted the analysis using R version 4.0.2.
2.4. Ethical statement
SGSS is held by PHE under existing information governance policies. HES is accessed by PHE under existing information governance policies. All data is anonymized.
3. RESULTS
We identified 4,254,927 hospital admissions with a cardio‐respiratory diagnosis (I00‐J99) for inclusion in the study and 1,092,778 laboratory records including 39,219 cases of RSV.
All 10 models included a secular trend, a one‐year period term, a categorical season term and weekly counts of RSV, influenza A, HMPV, and pneumococcus. Five models also included parainfluenza and three included group A streptococcus. We found model fit improved overall with a lag of 3 weeks for RSV, and 1 week for HMPV. Adding an interaction between RSV and pneumococcus led to a negative coefficient for RSV, and adding an interaction between influenza A and pneumococcus did not improve the model fit. Removal of pneumococcus gave a poorer model fit and did not significantly change the respiratory admission rates for the other pathogens. Figures 1 and 2 below show model fit for two models: respiratory admissions (J00–J99) in 65–74 years and in 75+ years, with the weekly admissions predicted by the model and the weekly proportion attributable to each pathogen predicted by the model, along with the actual admissions.
FIGURE 1.
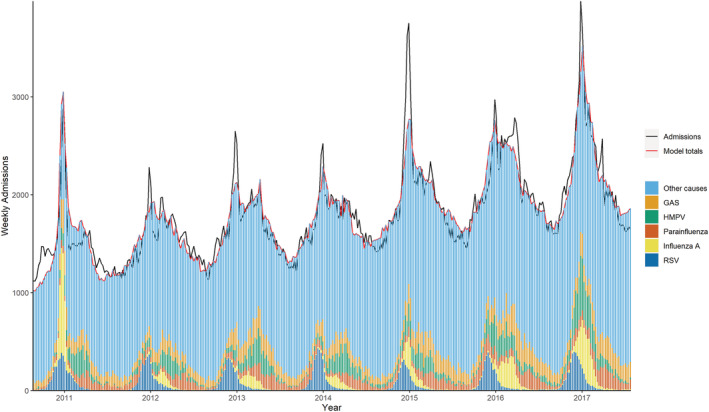
Weekly observed and predicted respiratory (J00–J99) admissions attributable to each pathogen, age 65–74
FIGURE 2.
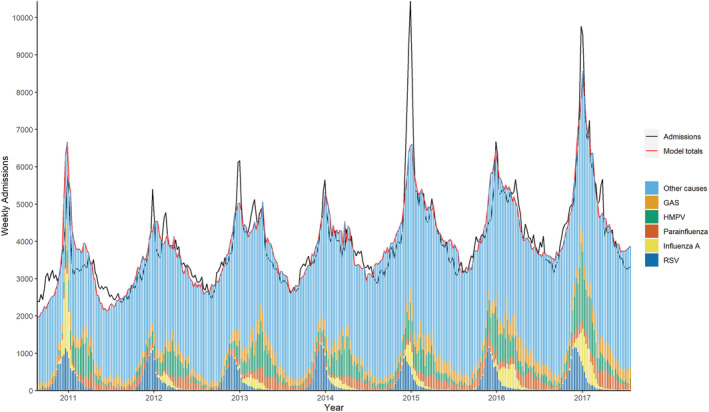
Weekly observed and predicted respiratory (J00–J99) admissions attributable to each pathogen, age 75+
Table 3 shows data from the same two models (respiratory admissions (J00–J99) in 65–74 years and in 75+ years) with the mean seasonal rate of admissions attributable to each pathogen. The highest rate of admissions in both age groups was attributable to pneumococcus, with a seasonal average of 448 (310–587) admissions per 100 000 adults age 65–74 and 1010 (527–1493) admissions per 100 000 adults aged 75+. RSV was estimated to account for a seasonal average of 71 (52–90) respiratory admissions per 100 000 adults age 65–74 and 251 (186–316) admissions per 100 000 adults age 75+. The mean seasonal rate of admissions for RSV was significantly higher than influenza A for adults age 75+.
TABLE 3.
Mean seasonal respiratory (J00–J99) admissions attributable to each pathogen by age group
| Organism | Age group | Admissions(mean) | Admissions(95 CI) | Rate/100,000(mean) | Rate(95% CI) |
|---|---|---|---|---|---|
| Pneumococcus | 65–74 | 22 610 | 15 626–29 595 | 448 | 310–587 |
| 75+ | 43 641 | 22 779–64 503 | 1010 | 527–1493 | |
| HMPV | 65–74 | 5023 | 3554–6492 | 99 | 70–128 |
| 75+ | 16 781 | 12 387–21 174 | 387 | 286–488 | |
| GAS | 65–74 | 4815 | 912–8718 | 95 | 18–172 |
| 75+ | ‐ | ‐ | ‐ | ‐ | |
| RSV | 65–74 | 3565 | 2632–4498 | 71 | 52–90 |
| 75+ | 10 808 | 7997–13 620 | 251 | 186–316 | |
| Parainfluenza | 65–74 | 2540 | 358–4722 | 50 | 7–93 |
| 75+ | 6784 | 142–13 427 | 157 | 3–310 | |
| Influenza A | 65–74 | 2273 | 1721–2824 | 45 | 34–56 |
| 75+ | 5141 | 3564–6718 | 119 | 82–155 |
Figure 3 shows time series data from the same two models (respiratory admissions (J00–J99) in 65–74 years and in 75+ years), showing the seasonal trend in the RSV attributable respiratory (J00–J99) admission rate attributable by age group. There was no significant change in admission rate over the study period.
FIGURE 3.
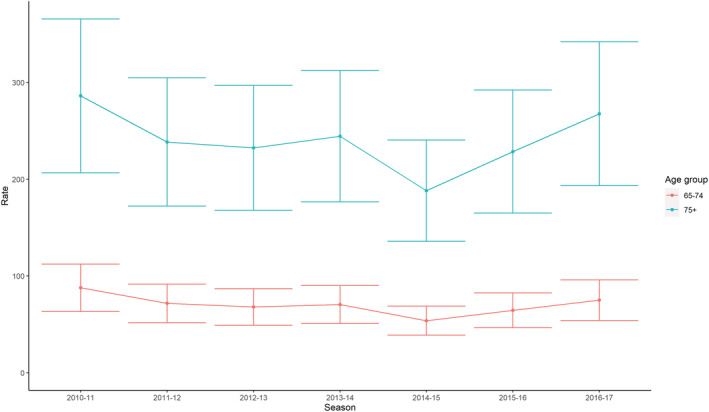
RSV attributable respiratory (J00–J99) admission rate by season and age group, 95% CI
Table 4 combines data from all 10 models with the mean seasonal RSV attributable admissions for each outcome by age group and diagnostic code. For each outcome, the admission rate was higher in the 75+ age group.
TABLE 4.
Mean seasonal RSV attributable admissions by diagnosis and age group, England, 2010–2017
| Admission group | Age group | Admissions(mean) | Admissions(95% CI) | Rate/100,000(mean) | Rate/100,000(95% CI) |
|---|---|---|---|---|---|
| Cardiorespiratory disease I00–J99 | 65–74 | 3062 | 2093–4032 | 61 | 42–80 |
| 75+ | 9978 | 6989–12 967 | 232 | 162–301 | |
| Respiratory disease J00–J99 | 65–74 | 3565 | 2632–4498 | 71 | 52–90 |
| 75+ | 10 808 | 7997–13 620 | 251 | 186–316 | |
| Influenza and Pneumonia J09–J18 | 65–74 | 1263 | 874–1653 | 25 | 17–33 |
| 75+ | 5073 | 3621–6524 | 118 | 84–151 | |
| Bronchitis J20–J22, J40 | 65–74 | 599 | 417–781 | 12 | 8–16 |
| 75+ | 2506 | 1828–3183 | 58 | 42–74 | |
| Chronic respiratory disease J41–J47 | 65–74 | 1569 | 1174–1964 | 31 | 23–39 |
| 75+ | 2711 | 2085–3336 | 63 | 48–77 | |
| Urinary disease | 65–74 | ‐ | ‐ | ‐ | ‐ |
| 75+ | 510 | 11–1009 | 12 | 0–23 |
4. DISCUSSION
This study found that RSV disease among adults in England aged 65–74 and 75+ accounted for an average annual hospital admission rate of 71 and 251 per 100 000 respectively. The yearly burden remained stable over the seven‐year study period from 2010 to 2017. The RSV burden was greater than influenza A and parainfluenza, similar to HMPV and GAS and greatly exceeded by pneumococcus. Among the specific respiratory subdiagnoses, influenza and pneumonia were the most common RSV attributable admission, followed by bronchitis and chronic respiratory disease. This study used nationally representative data sets and examined the full range of known pathogens likely to account for seasonal respiratory admissions.
Comparing these results with Fleming's analysis, 19 we find no statistically significant differences, noting the wide confidence intervals in both studies, though point estimates did vary somewhat. This study found a lower rate of respiratory disease in the 65–74 age group at 71 (52–90) compared to Fleming's 86 (62–101), and a slightly higher rate in the 75+ group at 251 (186–316)
Although the primary objective of the study was to assess RSV burden, the methodology does provide evidence of the impact of other pathogens in this age‐group notably pneumococcus, HMPV, GAS and parainfluenza. There are limitations inherent in this study methodology. The observation that RSV explained some urinary disease in the over 75's, albeit with very wide confidence intervals, despite the observation that urinary disease has no particular seasonality, indicates the limitations of this methodology, and also points to the complexity of causal factors contributing to respiratory admissions in the elderly. The model makes the reasonable assumption of a linear, additive relationship between different pathogens. We may argue whether a proportion of the pneumococcus admissions are secondary to RSV or other viruses and therefore potentially partially preventable with future RSV intervention strategies. Only invasive isolates of pneumococcus were included so the burden estimate is likely correct. The laboratory testing data includes all age groups and settings. We were unable to distinguish between tests done in hospital and the community, and most of the testing was done in children, which may explain the lagged peak in admissions in the elderly as reflecting a sequential pattern of infection across the age groups perhaps combined with delayed onset of complications such as secondary bacterial infection. We did not split influenza A into H1 and H3 subtypes but experience from Cromer et al. suggested this would not improve the model. 17 We did not include smoothing as is this is primarily a descriptive technique. The model retains periodic terms to account for unmeasured seasonal factors. Future studies could perhaps be strengthened by combining infectious disease data with environmental data such as air quality and temperature. A recent study 24 used linked data on positive and negative RSV test results and hospital admissions to develop a predictive model of RSV attributable hospital admissions in under 5's, which gave an overall very similar estimate of disease burden as with linear regression among the same population. A similar approach could be used to study disease burden in the elderly.
4.1. Conclusion and recommendations
This study shows that RSV continues to exert a significant burden of disease among older adults in England. This confirms the importance of RSV as a cause of hospital admissions among the elderly. There is also evidence of an on‐going burden due to pneumococcus and potentially important burden of HMPV in this age group. There is more work required using a range of analytical approaches including data linkage. These findings will support development of policy for the use of RSV therapeutics and vaccines in this age group, as these products become available and licensed for use.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
DISCLAIMER
The views expressed in this article are those of the authors and are not necessarily those of Public Health England or the Department of Health and Social Care.
AUTHOR CONTRIBUTIONS
Ashley Sharp: Data curation; formal analysis; investigation; methodology; visualization. Mehdi Minaji: Formal analysis; investigation; methodology. Nikolaos Panagiotopoulos: Formal analysis; investigation; methodology. Rachel Reeves: Conceptualization; methodology; supervision. Andre Charlett: Formal analysis; methodology; supervision. Richard Pebody: Conceptualization; formal analysis; investigation; methodology; supervision.
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1111/irv.12910.
Sharp A, Minaji M, Panagiotopoulos N, Reeves R, Charlett A, Pebody R. Estimating the burden of adult hospital admissions due to RSV and other respiratory pathogens in England. Influenza Other Respi Viruses. 2022;16(1):125-131. doi: 10.1111/irv.12910
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- 1. Bosco E, Van Aalst R, McConeghy KW, et al. Estimated cardiorespiratory hospitalizations attributable to influenza and respiratory syncytial virus among long‐term care facility residents. JAMA Netw Open. 2021;4(6):e2111806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Branche AR, Saiman L, Walsh EE, et al. Incidence of respiratory syncytial virus infection among hospitalized adults, 2017‐2020. Clin Infect Dis. 2021. [DOI] [PubMed] [Google Scholar]
- 3. Jackson ML, Scott E, Kuypers J, Nalla AK, Roychoudury P, Chu HY. Epidemiology of respiratory syncytial virus across five influenza seasons among adults and children one year of age and older‐Washington State, 2011/2012‐2015/2016. J Infect Dis. 2021;223(1):147‐156. [DOI] [PubMed] [Google Scholar]
- 4. Lee N, Smith S, Zelyas N, et al. Burden of noninfluenza respiratory viral infections in adults admitted to hospital: analysis of a multiyear Canadian surveillance cohort from 2 centres. Cmaj. 2021;193(13):E439‐e446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Prasad N, Newbern EC, Trenholme AA, et al. The health and economic burden of respiratory syncytial virus associated hospitalizations in adults. PLoS One. 2020;15(6):e0234235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Shi T, Denouel A, Tietjen AK, et al. Global disease burden estimates of respiratory syncytial virus‐associated acute respiratory infection in older adults in 2015: a systematic review and meta‐analysis. J Infect Dis. 2020;222(Suppl 7):S577‐s583. [DOI] [PubMed] [Google Scholar]
- 7. Shi T et al. The etiological role of common respiratory viruses in acute respiratory infections in older adults: a systematic review and meta‐analysis. J Infect Dis. 2020;222(Supplement_7):S563‐s569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tin Tin Htar M, Yerramalla MS, Moïsi JC, Swerdlow DL. The burden of respiratory syncytial virus in adults: a systematic review and meta‐analysis. Epidemiol Infect. 2020;148:e48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Tong S, Amand C, Kieffer A, Kyaw MH. Incidence of respiratory syncytial virus related health care utilization in the United States. J Glob Health. 2020;10(2):020422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Johnson EK, Sylte D, Chaves SS, et al. Hospital utilization rates for influenza and RSV: a novel approach and critical assessment. Popul Health Metr. 2021;19(1):31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Zambon MC, Stockton JD, Clewley JP, Fleming DM. Contribution of influenza and respiratory syncytial virus to community cases of influenza‐like illness: an observational study. Lancet. 2001;358(9291):1410‐1416. [DOI] [PubMed] [Google Scholar]
- 12. Domachowske JB, Anderson EJ, Goldstein M. The future of respiratory syncytial virus disease prevention and treatment. Infect Dis Ther. 2021;10(Suppl 1):47‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Higgins D, Trujillo C, Keech C. Advances in RSV vaccine research and development—a global agenda. Vaccine. 2016;34(26):2870‐2875. [DOI] [PubMed] [Google Scholar]
- 14. Nam HH, Ison MG. Respiratory syncytial virus infection in adults. BMJ. 2019;366:l5021. [DOI] [PubMed] [Google Scholar]
- 15. Stephens LM, Varga SM. Considerations for a respiratory syncytial virus vaccine targeting an elderly population. Vaccines (Basel). 2021;9(6):624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ryan MJ, Ramsay M, Brown D, Gay NJ, Farrington CP, Wall APG. Hospital admissions attributable to rotavirus infection in England and Wales. J Infect Dis. 1996;174(Suppl 1):S12‐S18. [DOI] [PubMed] [Google Scholar]
- 17. Cromer D, Van Hoek AJ, Jit M, Edmunds WJ, Fleming D, Miller E. The burden of influenza in England by age and clinical risk group: a statistical analysis to inform vaccine policy. J Infect. 2014;68(4):363‐371. [DOI] [PubMed] [Google Scholar]
- 18. Pitman RJ, Melegaro A, Gelb D, Siddiqui MR, Gay NJ, Edmunds WJ. Assessing the burden of influenza and other respiratory infections in England and Wales. J Infect. 2007;54(6):530‐538. [DOI] [PubMed] [Google Scholar]
- 19. Fleming DM, Taylor RJ, Lustig RL, et al. Modelling estimates of the burden of respiratory syncytial virus infection in adults and the elderly in the United Kingdom. BMC Infect Dis. 2015;15(1):443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Reeves RM, Hardelid P, Gilbert R, Warburton F, Ellis J, Pebody RG. Estimating the burden of respiratory syncytial virus (RSV) on respiratory hospital admissions in children less than five years of age in England, 2007‐2012. Influenza Other Respi Viruses. 2017;11(2):122‐129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Taylor S, Taylor RJ, Lustig RL, et al. Modelling estimates of the burden of respiratory syncytial virus infection in children in the UK. BMJ Open. 2016;6(6):e009337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Dolk FCK, De Boer PT, Nagy L, et al. Consultations for influenza‐like illness in primary care in the Netherlands: a regression approach. Value Health. 2021;24(1):11‐18. [DOI] [PubMed] [Google Scholar]
- 23. Morbey RA, Elliot AJ, Harcourt S, et al. Estimating the burden on general practitioner services in England from increases in respiratory disease associated with seasonal respiratory pathogen activity. Epidemiol Infect. 2018;146(11):1389‐1396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Reeves RM, Hardelid P, Panagiotopoulos N, Minaji M, Warburton F, Pebody R. Burden of hospital admissions caused by respiratory syncytial virus (RSV) in infants in England: a data linkage modelling study. J Infect. 2019;78(6):468‐475. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


