Abstract
Background
Previous studies have shown a negative impact of the COVID-19 pandemic and its associated sanitary measures on mental health, especially among adolescents and young adults. Such a context may raise many concerns about the COVID-19 pandemic long-term psychological effects. An analysis of administrative databases could be an alternative and complementary approach to medical interview-based epidemiological surveys to monitor the mental health of the population. We conducted a nationwide study to describe the consumption of anxiolytics, antidepressants and hypnotics during the first year of the COVID-19 pandemic, compared to the five previous years.
Methods
A historic cohort study was conducted by extracting and analysing data from the French health insurance database between 1 January 2015 and 28 February 2021. Individuals were classified into five age-based classes. Linear regression models were performed to assess the impact of the COVID-19 pandemic period on the number of drug consumers, in introducing an interaction term between time and COVID-19 period.
Results
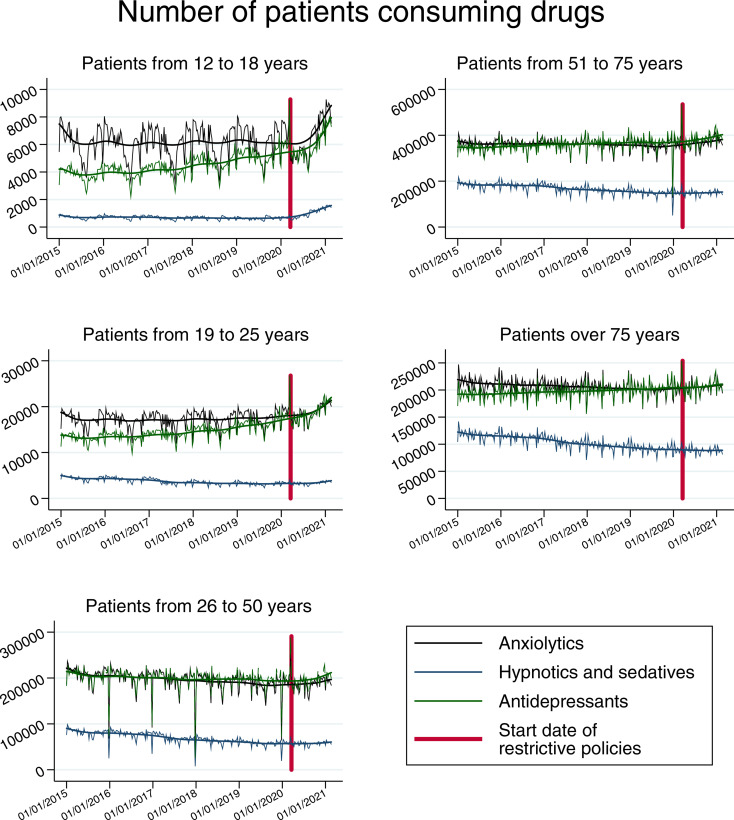
Since March 2020, in all five age groups and all three drug categories studied, the number of patients reimbursed weekly has increased compared to the period from January 2015 to February 2020. The youngest the patients, the more pronounced the magnitude.
Conclusions
Monitoring the consumption of psychiatric medications could be of great interest as reliable indicators are essential for planning public health strategies. A post-crisis policy including reliable monitoring of mental health must be anticipated.
Key words: COVID-19, mental health, pharmacoepidemiology, psychiatry, psychotropic drugs
Introduction
COVID-19 pandemic has now been identified as the cause of death for more than 3 150 000 people in the world, including over 100 000 in France. To deal with such an outbreak and limit the spread of the virus in the population, governments around the world have implemented restrictive policies such as physical distancing or lockdowns, with considerable effects on people's daily lives (Nicola et al., 2020). Evidence from previous epidemics suggests that these health measures can have a negative impact on the mental health of the population (Brooks et al., 2020), rapidly confirmed at the early stage of the COVID-19 pandemic (Wang et al., 2020). In France, as in many countries, studies have also shown an increase in mental health disorders since the start of the pandemic, such as anxiety, depression, posttraumatic stress or suicidal thoughts (Ramiz et al., 2021; Varga et al., 2021; Wathelet et al., 2020). Longitudinal studies are rare and difficult to implement, but some studies tend to show a persistence of high prevalence of severe symptoms of anxiety or depression and an increase in suicidal thoughts after leaving the first confinement (IFOP, 2020; Lu, Li, Lu, & Zhang, 2020). Because of these warning signs and the uncertainties about the long-term effects of the pandemic on mental health, the Lancet's COVID-19 Commission Mental Health Task Force recommends monitoring the mental health of populations over the next few years (Aknin et al., 2021).
Analysis of administrative databases is an alternative and complementary approach to medical interview-based epidemiological surveys (Fiest et al., 2014; Filipovic-Pierucci, Samson, Fagot, & Fagot-Campagna, 2017; Townsend, Walkup, Crystal, & Olfson, 2012). Beyond measuring the prevalence or the incidence of mental health disorders, another way to document and monitor the mental health of populations is to study their drug consumption. Some epidemiological studies have shown an increase in the use of substances to cope with psychological difficulties, but data are scarce. In a recent Canadian study including 3027 respondents, a weighted prevalence of 17% of individuals reported an increase in substance use since the start of the pandemic, and 7% an increase in prescription medication use, specifically (Canadian Mental Health Association, 2021). In France, EPI-PHARE has been monitoring the consumption of prescription drugs dispensed in cities in France for the entire French population, using data from the National Health Data System (SNDS). Its last report covers the 6 first months of the COVID-19 pandemic, until 13 September 2020, for a total of 6 months follow-up (Weill et al., 2020). According to this report, two therapeutic classes of drugs for mental disorders – anxiolytics and hypnotics – have seen their consumption and initiation increased persistently during and after confinement. The report concludes that this increase likely reflects the significant psychological impact of the COVID-19 epidemic and its social, occupational and economic consequences.
Of note, the negative effects of the COVID-19 pandemic on mental health vary by age group. Adolescents and young adults seem to be particularly affected by the crisis. The vulnerability of adolescents and young adults to mental health disorders is well-documented (Avenevoli, Swendsen, He, Burstein, & Merikangas, 2015; Merikangas et al., 2010; Observatoire National du Suicide, 2018; WHO, 2014). It is also an age group at risk for the negative effects of pandemic contexts, as observed in previous quarantines (Brooks et al., 2020; Taylor, Agho, Stevens, & Raphael, 2008). Results from more recent studies of the COVID-19 pandemic also point to a greater vulnerability of adolescents and young adults (Mohler-kuo, Dzemaili, Foster, Werlen, & Walitza, 2021; Nearchou, Hennessy, Flinn, Niland, & Subramaniam, 2020; Ramiz et al., 2021; Varga et al., 2021; Wang et al., 2020; Wathelet et al., 2020). To our knowledge, there are no data relating to the psychiatric medications use during the pandemic by age group.
In this national study, we aimed to describe the consumption of psychiatric medications (anxiolytics, antidepressants, hypnotics and sedatives) during the first year of the COVID-19 pandemic, compared to the 5 previous years.
Methods
We conducted a historic cohort study by extracting and analysing data from the French health insurance database, named Système National d'Information Inter-Regimes de l'Assurance Maladie (SNIIRAM) (Moulis et al., 2015), between 1 January 2015 and 28 February 2021.
Data source
The SNIIRAM is a national medico-administrative database, containing data on the reimbursed prescriptions in non-hospital pharmacies, collected anonymously and prospectively for all national health insurance beneficiaries in France (65 million inhabitants).
Study population and data collected
All reimbursed prescriptions of patients above 12 years old affiliated to the Social Security System were retrieved from the SNIIRAM between 1 January 2015 and 28 February 2021.
Three outcomes were considered: the consumption of anxiolytics, antidepressants, and hypnotics or sedatives. Drugs were coded according to the Anatomical Therapeutic Chemical (ATC) Classification System: code N06A or N06C for antidepressants, N05B for anxiolytics and N05C for hypnotics and sedatives (WHOCC, 2021). All routes of administration have been recorded.
Consumers of antidepressant, anxiolytics, and hypnotics and sedatives were identified as patients having received at least one reimbursement for such treatment during the selected week. The rate of new consumers was defined as the difference, before and after the COVID-19 period, of the number of new drug consumers per week, divided by the total number of drug consumers.
Age was also collected, categorized into five classes: 12–18, 19–25, 26–50, 51–75 and above 75 years old.
Statistical analysis
For each considered drug, the evolution of the weekly number of consumers over time was represented graphically.
The evolution of the weekly number of consumers over time was analysed using linear regression models. Separate models were performed for each considered drug (anxiolytics, antidepressants, and hypnotics or sedatives) and each age class (12–18, 19–25, 26–50, 51–75 and over 75 years), allowing to check the consistency of the results depending on the considered parameters. For all these models, the dependant variable was the number of consumers per week, and the explanatory variables were time (considered as a continuous covariate) and the COVID-19 period (COVID-19 period being defined as the period starting on 17 March 2020, i.e. the date of the first sanitary confinement in France). An interaction between these two covariates was also considered to assess the effect of the COVID-19 pandemic on drug consumption. If a significant interaction was highlighted, the conditional effect of time depending on COVID-19 period was presented using linear combinations, allowing to assess the average number of new drug consumers per week over time before and during COVID-19.
As a sensitivity analysis, we also performed models including time, COVID-19 period and classes of ages as explanatory covariates, considering all first- and second-order interactions for evaluating the differences of time and COVID-19 period on drug consumption depending on age.
Finally, the relative increase in drug consumption was estimated depending on COVID-19 period using the ratio between the average number of new drug consumers per week and the total number of drug consumers.
The models’ validity was assessed by studying the distribution of residuals. All the tests were two-sided, considering a 0.05 type I error. All the statistical analyses were performed using SAS 9.4 and Stata 14.2 software.
Results
Sample
In 2020, a mean number of 78 715 903 anxiolytics, 30 013 876 hypnotics or sedatives and 80 970 798 antidepressants were reimbursed every week in France. Almost 0.02% of the 12–18-year-olds consumed at least one of those drugs, and 0.06% of the 19–25, 0.28% of the 26–50, 0.75% of the 51–75 and 1.52% of those over 75 years old, based on the population described by the French National Institute for Statistical and Economic Studies (INSEE).
COVID-19 impact
A significant interaction between time and the COVID-19 period was highlighted for all the considered drugs and age groups, except from the specific consumption of antidepressants among patients over 75 years old.
When focusing on anxiolytics, hypnotics and sedatives, the youngest the patients, the more the magnitude of these interactions was pronounced (second-order p value respectively equal to 0.020, <0.001 and 0.101 for anxiolytics, for hypnotics and sedatives and for antidepressants, online Supplementary Table S1). Thus, a very high increase of antidepressants, and hypnotics and anxiolytics was observed across the people aged 12–18 during the pandemic period. For this age group, hypnotics and anxiolytics shifted from a slight decrease to a high increase, while antidepressants, that were already in a slight rising trend, turned to a considerable increase (from +6 to +34 new patient weekly, p < 0.001) (Fig. 1, Table 1).
Fig. 1.
Evolution of weekly drug consumers from 1 January 2015 to 28 February 2021, according to age group and drug considered.
Table 1.
Time effect (number of new consumers per week) before and during COVID-19 pandemic period according to age group and drug considered
| Anxiolytics | Hypnotics and sedatives | Antidepressants | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coef. | 95% CI | p | Coef. | 95% CI | p | Coef. | 95% CI | p | |||||
| 12–18 y | Number of new consumers per week before COVID-19 outbreak | −0.9 | −2.53 | 0.73 | 0.279 | −0.49 | −0.65 | −0.32 | <10−4 | 6.03 | 5.07 | 6.99 | <10−4 |
| Number of new consumers per week during COVID-19 outbreak | 35.72 | 22.28 | 49.15 | <10−4 | 18.46 | 17.08 | 19.85 | <10−4 | 34.48 | 26.59 | 42.38 | <10−4 | |
| Number of consumers on 1 January 2015 | 6226 | 5960 | 6493 | <10−4 | 743 | 715 | 770 | <10−4 | 3570 | 3413 | 3727 | <10−4 | |
| 19–25 y | Number of new consumers per week before COVID-19 outbreak | 1.71 | −0.67 | 4.1 | 0.159 | −5.87 | −6.45 | −5.28 | <10−4 | 14.98 | 13.01 | 16.95 | <10−4 |
| Number of new consumers per week during COVID-19 outbreak | 55.92 | 36.31 | 75.54 | <10−4 | 15.08 | 10.27 | 19.9 | <10−4 | 87.12 | 70.91 | 103.33 | <10−4 | |
| Number of consumers on 1 January 2015 | 17 034 | 16 644 | 17 423 | <10−4 | 4538 | 4443 | 4634 | <10−4 | 12 446 | 12 124 | 12 768 | <10−4 | |
| 26–50 y | Number of new consumers per week before COVID-19 outbreak | −102.14 | −133.43 | −70.85 | <10−4 | −116.5 | −128.02 | −104.98 | <10−4 | −52.56 | −82.79 | −22.33 | 0.001 |
| Number of new consumers per week during COVID-19 outbreak | 214.52 | −42.7 | 471.75 | 0.102 | 123.77 | 29.09 | 218.45 | 0.011 | 247.11 | −1.38 | 495.61 | 0.051 | |
| Number of consumers on 1 January 2015 | 210 570 | 205 460 | 215 679 | <10−4 | 85 355 | 83 475 | 87 236 | <10−4 | 206 572 | 201 636 | 211 508 | <10−4 | |
| 51–75 y | Number of new consumers per week before COVID-19 outbreak | −43.93 | −85.49 | −2.37 | 0.038 | −174.34 | −195.5 | −153.18 | <10−4 | 100.85 | 60.41 | 141.29 | <10−4 |
| Number of new consumers per week during COVID-19 outbreak | 520 | 178.36 | 861.64 | 0.003 | 160.33 | −13.58 | 334.25 | 0.071 | 486.18 | 153.72 | 818.63 | 0.004 | |
| Number of consumers on 1 January 2015 | 366 345 | 359 558 | 373 132 | <10−4 | 191 529 | 188 075 | 194 984 | <10−4 | 345 589 | 338 985 | 352 194 | <10−4 | |
| >75 y | Number of new consumers per week before COVID-19 outbreak | −50.15 | −69.47 | −30.83 | <10−4 | −125.52 | −136.93 | −114.11 | <10−4 | 49.56 | 32.05 | 67.07 | <10−4 |
| Number of new consumers per week during COVID-19 outbreak | 189.71 | 30.88 | 348.53 | 0.019 | 40.72 | −53.06 | 134.5 | 0.394 | 100.9 | −43.06 | 244.86 | 0.169 | |
| Number of consumers on 1 January 2015 | 213 733 | 210 578 | 216 888 | <10−4 | 121 007 | 119 144 | 122 870 | <10−4 | 190 597 | 187 737 | 193 456 | <10−4 | |
The number of new consumers per week before COVID-19 outbreak corresponds to the time effect of the linear model. The number of new consumers per week during COVID-19 outbreak corresponds to the linear combination between time effect and interaction between time effect and COVID-19 period. Finally, the number of consumers on 1 January 2015 corresponds to the intercept.
For the 19–25 age group, the same increase was observed in all drugs considered, with a higher increase trend after March 2020 for anxiolytics and antidepressants, and a shift from a slight decrease to an increase for hypnotics.
For either the 26–50, the 51–75 and the above 75 age groups, the decreasing trend in anxiolytics and hypnotics observed since 2015 was converted into an important increase in the weekly number of consumers (p < 0.001). A similar effect was observed for antidepressants in the 26–50 age group.
On the contrary, for the 51–75 age group and above, antidepressant's consumers were increasing in the population, a rise that became more important after the implementation of restrictive sanitary measures.
The rate of new drugs consumers due to the COVID-19 period was dependent on the considered drugs and age groups. For antidepressants, the increase in the number of consumers was, respectively, five and four times higher among the 12–18 and 19–25 compared to the 26–50. For anxiolytics, this inflation was, respectively, four and two times higher among the 12–18 and 19–25 compared to the 26–50. Finally, the increase of hypnotics' users was, respectively, nine and 1.6 times higher among the 12–18 and 19–25 compared to the 26–50 (Table 2).
Table 2.
Rate of new drug consumers per week due to the COVID-19 pandemic according to age group and drug considered
| Anxiolytics | Hypnotics and sedatives | Antidepressants | |
|---|---|---|---|
| 12–18 | 0.59%, CI 95% (0.37–0.81%) | 2.55%, CI 95% (2.36–2.74%) | 0.80%, CI 95% (0.57–1.02%) |
| 19–25 | 0.32%, CI 95% (0.20–0.44%) | 0.46%, CI 95% (0.35–0.57%) | 0.58%, CI 95% (0.45–0.71%) |
| 26–50 | 0.15%, CI 95% (0.02–0.28%) | 0.28%, CI 95% (0.17–0.40%) | 0.15%, CI 95% (0.02–0.27%) |
| 51–75 | 0.15%, CI 95% (0.06–0.25%) | 0.17%, CI 95% (0.08–0.27%) | 0.11%, CI 95% (0.01–0.21%) |
| >75 | 0.11%, CI 95% (0.03–0.19%) | 0.14%, CI 95% (0.06–0.22%) | 0.03%, CI 95% (−0.05 to 0.11%) |
CI 95%, 95% confidence interval.
Discussion
Since the introduction of restrictive sanitary measures in France, in particular the first lockdown in March 2020, the number of patients weekly reimbursed for either anxiolytics, sedatives or antidepressants have increased compared to the period going from January 2015 to February 2020. This increase was noticed across the five age groups of interest, and for all the three drug categories investigated. However, the magnitude of the increase was not the same across age groups. The age groups under 26 years old were those for which the increase in consumption was the most important, notably for antidepressants. In addition, the proportion of new consumers has grown more importantly in the youngest population.
Our results relating to the increase in the consumption of psychotropic drugs with the pandemic are congruent with the few data available on such topics, such as the one provided by the Canadian Mental Health Association (Canadian Mental Health Association, 2021) and the French project EPI-PHARE (Weill et al., 2020). These findings also converge with medical interview-based or web-based epidemiological studies reporting a high prevalence of mental health disorders, persisting even after the lifting of the first confinement (IFOP, 2020; Lu et al., 2020). While there is no study about medication use among adolescents and young adults during the pandemic period, our results converge with studies reporting the disastrous effects of the pandemic on their mental health (Mohler-kuo et al., 2021; Nearchou et al., 2020; Wathelet et al., 2020).
Interestingly, epidemiological studies focusing on mental health disorders reported a decrease in prevalence rates of mental health disorders after the first confinement was lifted (without reaching their previous levels, however), which is not congruent with the continuous increase in reimbursed prescriptions (Aknin et al., 2021). Epidemiological studies of mental health disorders suffer from limitations inherent in their designs, such as selection bias related to non-responders, or classification bias related to self-administered screening scales (instead of diagnostic assessment by clinicians). Moreover, the investment making it possible to carry out such studies is extremely heavy and their reproducibility over time is not really conceivable. Conversely, the use of medico-administrative databases allows close monitoring of populations by means of reproducibility at low cost.
Monitoring the consumption of psychiatric medications could be of great interest during health crises with important repercussions on individuals' mental health. Reliable indicators are essential to describe a health phenomenon, plan public health strategies and evaluate interventions. However, studies evaluating the psychological repercussions of the COVID-19 pandemic are mostly based on medical interviews or self-administrated questionnaire, use different methodologies, include different samples, and, therefore, lead to results not closely comparable and not easily reproducible from one time to another (Filipovic-Pierucci et al., 2017). Even if estimating the prevalence of mental disorders (such as depression) using medico-administrative databases often lead to an underestimation (Filipovic-Pierucci et al., 2017), monitoring over time can provide valuable information.
For example, using the Norwegian Prescription Database, it has been shown that patients who died by suicide were dispensed more psychotropic medications than the general population, including antidepressants, anxiolytics and hypnotics, suggesting a higher severity of the depression experienced prior to dying by suicide (Reneflot, Kaspersen, Hauge, & Kalseth, 2019). Although prescribing habits may vary over time and space, the increase in treatment dispensations probably reflects improved access to adequate treatment or a deterioration in the mental health of the population, circumstances invite us to monitor these indicators and to develop algorithms to describe and even predict mental health disorders through a pharmaco-epidemiological approach (Bezin et al., 2017). Monitoring this particular mental issue through a pandemic can help in targeting post-crisis priority policies. For example, as mental health was already an issue for children, adolescents and young adults in France as in many countries before COVID-19 (Avenevoli et al., 2015; Merikangas et al., 2010), and because of a major increase of drugs through the pandemic, it is very likely that without a major focus on such an issue, this rise will not stop.
Some limitations should be considered while interpreting the results. First, the statistical model used can be discussed, as it could be considered as non-optimal according to the complexity of the prescription rates' evolution over time, because of seasonal and annual variations superimposed on non-linear long evolutions. However, an arbitrage between technicality and clarity favoured the choice of a linear regression model, correctly fitted to the data. Second, some confounders may be missing in the model. Indeed, it is a descriptive analysis of the evolution of drug consumption as a function of time and age only. However, since this is a national-based analysis, it is unlikely that other factors (independent of the consequences of the pandemic) varied considerably over the same period. Third, although we used international classifications to group the drugs, it may mask some specific trends for a particular drug. Four, the SNIIRAM database collects treatments delivered but not consumed (which they would overestimate) nor the diagnosis of mental health disorders [which they would undoubtedly underestimate due to the low recourse to adequate treatment in the event of a health disorder mental (Alonso et al., 2004)]. Finally, reimbursements for children and adolescents are complex to identify given the possibility of several rights' holder.
Conclusion
In France, since mid-March and the first sanitary lockdown implemented to deal with COVID-19 outbreak, the weekly number of new antidepressants, anxiolytics, sedative and hypnotics consumers increases as compared with the trend from 2015 to 2020. This increase is higher for children, adolescents and young adults than for the age ranges above 26 years old. In order to study the long-term effects of the pandemic on the mental health of populations, monitoring using administrative database should be encouraged.
Acknowledgements
None.
Author contribution
Conception: ML, MW, AL, JFH. Planning: ML, MW, AL, JFH. Carrying out: ML, JFH. Analysing: ML, MW, AL, BG, JFH. Writing up: ML, MW, JFH. Revising it critically for important intellectual content: ML, MW, AL, ER, BG, JFH. Final approval of the version to be published: ML, MW, AL, ER, BG, JFH.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Ethical standards
As this research does not involve human participants but administrative database, informed consent and ethical committee submission were not applicable to this study.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S0033291721004839.
click here to view supplementary material
Data
The data that support the findings of this study are available on request from the corresponding author, ML.
Conflict of interest
None.
References
- Aknin, L., Neve, J.-E. D., Dunn, E., Fancourt, D., Goldberg, E., Helliwell, J., … Amour, Y. B. (2021). Mental health during the first year of the COVID-19 pandemic: a review and recommendations for moving forward. PsyArXiv. 10.31234/osf.io/zw93g. [DOI] [PMC free article] [PubMed]
- Alonso, J., Angermeyer, M. C., Bernert, S., Bruffaerts, R., Brugha, T. S., Bryson, H., … Vollebergh, W. A. M. (2004). Psychotropic drug utilization in Europe: Results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatrica Scandinavica, Supplement, 109(420), 55–64. 10.1111/j.1600-0047.2004.00331.x. [DOI] [PubMed] [Google Scholar]
- Avenevoli, S., Swendsen, J., He, J. P., Burstein, M., & Merikangas, K. R. (2015). Major depression in the national comorbidity survey – adolescent supplement: Prevalence, correlates, and treatment. Journal of the American Academy of Child and Adolescent Psychiatry, 54(1), 37–44.e2. 10.1016/j.jaac.2014.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bezin, J., Duong, M., Lassalle, R., Droz, C., Pariente, A., Blin, P., & Moore, N. (2017). The national healthcare system claims databases in France, SNIIRAM and EGB: Powerful tools for pharmacoepidemiology. Pharmacoepidemiology and Drug Safety, 26(8), 954–962. 10.1002/pds.4233. [DOI] [PubMed] [Google Scholar]
- Brooks, S. K., Webster, R. K., Smith, L. E., Woodland, L., Wessely, S., Greenberg, N., & Rubin, G. J. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet, 395, 912–920. Lancet Publishing Group. 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canadian Mental Health Association. (2021). Mental health impacts of Covid-19: Wave 2.
- Fiest, K. M., Jette, N., Quan, H., St Germaine-Smith, C., Metcalfe, A., Patten, S. B., & Beck, C. A. (2014). Systematic review and assessment of validated case definitions for depression in administrative data. BMC Psychiatry, 14(1), 289. 10.1186/s12888-014-0289-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filipovic-Pierucci, A., Samson, S., Fagot, J. P., & Fagot-Campagna, A. (2017). Estimating the prevalence of depression associated with healthcare use in France using administrative databases. BMC Psychiatry, 17(1), 1. 10.1186/s12888-016-1163-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IFOP. (2020). Les Français et le suicide.
- Lu, P., Li, X., Lu, L., & Zhang, Y. (2020). The psychological states of people after Wuhan eased the lockdown. PLoS ONE, 15(11), e0241173. 10.1371/journal.pone.0241173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas, K. R., He, J. P., Burstein, M., Swanson, S. A., Avenevoli, S., Cui, L., … Swendsen, J. (2010). Lifetime prevalence of mental disorders in U.S. adolescents: Results from the national comorbidity survey replication-adolescent supplement (NCS-A). Journal of the American Academy of Child and Adolescent Psychiatry, 49(10), 980–989. 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohler-kuo, M., Dzemaili, S., Foster, S., Werlen, L., & Walitza, S. (2021). Stress and mental health among children/adolescents, their parents, and young adults during the first COVID-19 lockdown in Switzerland. International Journal of Environmental Research and Public Health, 18(9), 4668. 10.3390/ijerph18094668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moulis, G., Lapeyre-Mestre, M., Palmaro, A., Pugnet, G., Montastruc, J. L., & Sailler, L. (2015). French health insurance databases: What interest for medical research? Revue de Medecine Interne, 36, 411–417. Elsevier Masson SAS. 10.1016/j.revmed.2014.11.009. [DOI] [PubMed] [Google Scholar]
- Nearchou, F., Hennessy, E., Flinn, C., Niland, R., & Subramaniam, S. S. (2020). Exploring the impact of covid-19 on mental health outcomes in children and adolescents: A systematic review. International Journal of Environmental Research and Public Health, 17, 1–19. MDPI AG. 10.3390/ijerph17228479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicola, M., Alsafi, Z., Sohrabi, C., Kerwan, A., Al-Jabir, A., Iosifidis, C., … Agha, R. (2020). The socio-economic implications of the coronavirus pandemic (COVID-19): A review. International Journal of Surgery, 78, 185–193. Elsevier Ltd. 10.1016/j.ijsu.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Observatoire National du Suicide. (2018). Suicide: Enjeux éthiques de la prévention, singularités du suicide à l'adolescence.
- Ramiz, L., Contrand, B., Rojas Castro, M. Y., Dupuy, M., Lu, L., Sztal-Kutas, C., … Lagarde, E. (2021). A longitudinal study of mental health before and during COVID-19 lockdown in the French population. Globalization and Health, 17, 29. 10.1186/s12992-021-00682-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reneflot, A., Kaspersen, S. L., Hauge, L. J., & Kalseth, J. (2019). Use of prescription medication prior to suicide in Norway. BMC Health Services Research, 19(1), 1–8. 10.1186/s12913-019-4009-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor, M. R., Agho, K. E., Stevens, G. J., & Raphael, B. (2008). Factors influencing psychological distress during a disease epidemic: Data from Australia's first outbreak of equine influenza. BMC Public Health, 8(1), 347. 10.1186/1471-2458-8-347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Townsend, L., Walkup, J. T., Crystal, S., & Olfson, M. (2012). A systematic review of validated methods for identifying depression using administrative data. Pharmacoepidemiology and Drug Safety, 21(Suppl. 1), 163–173. 10.1002/pds.2310. [DOI] [PubMed] [Google Scholar]
- Varga, T. V., Bu, F., Dissing, A. S., Elsenburg, L. K., Bustamante, J. J. H., Matta, J., … Rod, N. H. (2021). Loneliness, worries, anxiety, and precautionary behaviours in response to the COVID-19 pandemic: A longitudinal analysis of 200000 Western and Northern Europeans. The Lancet Regional Health – Europe, 2, 100020. 10.1016/j.lanepe.2020.100020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, C., Pan, R., Wan, X., Tan, Y., Xu, L., Ho, C. S., … Ho, R. C. (2020). Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health, 17. 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wathelet, M., Duhem, S., Vaiva, G., Baubet, T., Habran, E., Veerapa, E., … D'Hondt, F. (2020). Factors associated with mental health disorders among university students in France confined during the COVID-19 pandemic. JAMA Network Open, 3(10), e2025591. 10.1001/jamanetworkopen.2020.25591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weill, A., Drouin, J., Desplas, D., Cuenot, F., Dray-Spira, R., & Zureik, M. (2020). Usage des médicaments de ville en France durant l’épidémie de la Covid-19 – point de situation jusqu'au 13 septembre 2020.
- WHO. (2014). Données et statistiques sur le suicide.
- WHOCC. (2021). Guidelines for ATC classification and DDD assignment 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S0033291721004839.
click here to view supplementary material
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author, ML.