Abstract
Background
This study aimed to evaluate the antitumor activity of camrelizumab, an antiprogrammed cell death-1 antibody, in pretreated recurrent or metastatic nasopharyngeal carcinoma (NPC) and to explore predictive biomarkers.
Methods
Patients with recurrent (not amenable to locally curative treatment) or metastatic NPC who had failed at least two lines of chemotherapy were eligible to receive camrelizumab (200 mg intravenously every 2 weeks) for 2 years or until disease progression, intolerable adverse events, withdrawal of consents, or investigator decision. The primary endpoint was objective response rate (ORR) assessed by an independent review committee (IRC). Programmed cell death-ligand 1 (PD-L1) expression was assessed by immunohistochemistry. Other immune-related biomarkers including major histocompatibility complex class I and major histocompatibility complex class II (MHC-II) were assessed by multiplex immunofluorescence staining.
Results
Between August 14, 2018, and December 30, 2019, a total of 156 patients were enrolled. The IRC-assessed ORR was 28.2% (95% CI 21.3% to 36.0%). The median progression-free survival was 3.7 months (95% CI 2.0 to 4.1) per IRC, and the median overall survival was 17.4 months (95% CI 15.2 to 21.9). The ORRs were 35.2% (95% CI 25.3% to 46.1%) vs 19.4% (95% CI 10.4% to 31.4%) in patients with tumor PD-L1 expression of ≥10% and<10%, respectively. Patients with durable clinical benefit (DCB), which was defined as complete response, partial response or stable disease of ≥18 weeks, had higher density of MHC-II+ cell in stroma than patients without DCB (median 868.1 (IQR 413.4–2854.0) cells/mm2 vs median 552.4 (IQR 258.4 to 1242.1) cells/mm2). MHC-II+ cell density did not correlate with PD-L1 expression, and a composite of high stromal MHC-II+ cell density and tumor PD-L1 expression further enriched patients who could benefit from camrelizumab.
Conclusions
Camrelizumab had clinically meaningful antitumor activity in patients with recurrent or metastatic NPC. The composition of both MHC-II+ cell density and PD-L1 expression could result in better patient selection.
Keywords: head and neck neoplasms, immunotherapy
Introduction
Standard first-line treatment for patients with recurrent or metastatic nasopharyngeal carcinoma (R/M-NPC) is platinum-based chemotherapy.1 For patients who failed first-line chemotherapy, treatment options are limited and the prognosis remains dismal, with a median overall survival (OS) of about 12 months.2 Thus, there remains an urgent need for effective salvage treatment in this patient population.
Endemic nasopharyngeal carcinoma (NPC) tumors are characterized by intense infiltration of non-malignant lymphocytes and high expression of programmed cell death-ligand 1 (PD-L1).3 4 These features of NPC render them potentially suitable for immunotherapy. Several antiprogrammed cell death-1 (PD-1) antibodies have demonstrated robust antitumor activity in patients with pretreated R/M-NPC, with an objective response rate (ORR) of 20%–34%.5–8 However, anti-PD-1 antibodies only benefit a subset of patients with R/M-NPC. The predictive value of commonly used biomarkers, such as PD-L1 or tumor mutation burden, is limited for R/M-NPC.6–8 Therefore, identification of novel predictive biomarkers is still of great importance. Recent studies highlight the importance of the antigen presentation mechanism for immunotherapy in several cancers, including melanoma, classic Hodgkin lymphoma and non-small cell lung cancer.9–11 Exome and genome sequencings of primary NPC tumors have found that major histocompatibility complex class I (MHC-I) gene aberrations occur in a third of patients with NPC, which result in loss of corresponding protein expression and are associated with a poor prognosis.12 In addition, basic research reveals that Epstein-Barr virus (EBV) can suppress the expression of major histocompatibility complex class II (MHC-II) genes by downregulation of the MHC class II master transactivator.13 14 However, the significance of MHC-I/MHC-II gene expression in patients with NPC undergoing immunotherapy remains elusive.
In this report, we present results from a phase II pivotal study (Camrelizumab in Previously Treated Recurrent or Metastatic Nasopharyngeal Carcinoma (CAPTAIN)) evaluating the efficacy and safety of camrelizumab (SHR-1210), a humanized IgG4-κ anti-PD-1 monoclonal antibody, for previously treated R/M-NPC. We also investigated the predictive value of potential biomarkers including MHC-I/MHC-II expression, PD-L1 expression and plasma EBV DNA status.
Patients and methods
Study design and patients
The CAPTAIN study is a multicenter, open-label, single-arm, phase II study conducted at eight hospital sites in China (ClinicalTrials.gov identifier: NCT03558191). Eligible patients were aged between 18 and 75 years old, with histopathologically confirmed differentiated or undifferentiated non-keratinizing stage IVb NPC (defined according to the Chinese 2008 staging system for NPC 2017 edition).15 All patients had failed first-line platinum-based chemotherapy (concurrent chemoradiotherapy was considered as a line of systemic treatment as long as disease progressed within 6 months after the end of treatment) and second-line single-agent or combined chemotherapy. Treatment failure was defined as disease progression during or after chemotherapy in recurrent NPC not amenable to locally curative treatment or metastatic setting, and patients who changed treatment due to intolerable toxicities were not allowed. Other eligible criteria included an Eastern Cooperative Oncology Group (ECOG) performance status score of 0 or 1, at least one measurable lesion according to Response Evaluation Criteria in Solid Tumors V.1.1 (RECIST 1.1; lesions located in a previously irradiated area were deemed unmeasurable), a life expectancy of at least 12 weeks, and adequate organ function. Patients were excluded if they underwent chemotherapy or targeted therapy within 4 weeks before study entry or had immune checkpoint inhibitor treatment. Patients with previously treated brain metastases were eligible if they were clinically stable. The full eligibility criteria are described in the online supplemental methods.
jitc-2021-003790supp001.pdf (750.6KB, pdf)
Procedures
Enrolled patients received camrelizumab 200 mg intravenously every 2 weeks on 4-week treatment cycles for 2 years or until disease progression, intolerable adverse events (AEs), withdrawal of consents or investigator decision. Radiographical assessments were performed every two cycles according to RECIST 1.1. Patients who were assessed as progressive disease could remain on treatment until confirmed progression assessed 4–6 weeks later. A confirmatory scan was required for the initial complete and partial response (PR) at least 4 weeks later. AEs were graded per the National Cancer Institute Common Terminology Criteria for Adverse Events V.4.03.
Archived or fresh tumor samples were retrieved for immunohistochemical staining of PD-L1 expression in tumor cells with SP142 antibody (Abcam) in a central lab.16 Multiplex immunofluorescence staining of immune-related biomarkers including MHC-I, MHC-II, CD68, CD86, granzyme B, granzyme H, CD8A, IFN-γ, FoxP3, CD19 and CD4 were also conducted in a central lab (online supplemental methods). Plasma EBV DNA level was determined using quantitative reverse transcription PCR method at baseline and every two cycles until disease progression.
Outcomes
The primary endpoint was confirmed ORR per independent review committee (IRC). The secondary endpoints were investigator-assessed ORR, duration of response (DOR), disease control rate (DCR), time to response (TTR), progression-free survival (PFS) and OS. Exploratory analyses were done to investigate the predictive value of PD-L1 expression, other immune-related biomarkers including MHC-I and MHC-II, and plasma EBV DNA level. The definitions of endpoints are present in the online supplemental methods.
Statistical analyses
On the basis of the results from the previous phase I study with camrelizumab in pretreated advanced NPC,8 an ORR of 26% was used to determine the sample size in the present study. In addition, pembrolizumab was approved in patients with head and neck squamous cell carcinoma who had been pretreated with platinum-containing chemotherapy with an ORR of 16%.17 Therefore, 15% was considered the minimum clinically meaningful ORR. Assuming a targeted ORR of 26%, with a one-sided α of 0.025, a sample size of 139 patients was required to provide a 90% power to declare the lower bound of 95% CIs for ORR to exceed 15%. Assuming a dropout rate of 10%, the maximum target sample size estimated was 155 patients.
All patients who received at least one dose of study treatment were included in the efficacy and safety analysis set (full analysis set). The 95% CIs of ORR and DCR were calculated using the Clopper-Pearson method. PFS and OS were plotted using the Kaplan-Meier method, with median and corresponding 95% CIs calculated using the Brookmeyer-Crowley method on a log–log transformation. Median DOR and 95% CI were calculated with the Kaplan-Meier product limit estimate. TTR was summarized descriptively. In addition to response defined by RECIST, we also defined efficacy as durable clinical benefit (DCB, including complete response (CR), PR, and stable disease that lasted ≥18 weeks) or no durable benefit (NDB, including progressive disease and stable disease that lasted <18 weeks). Subgroup analysis was done to investigate the treatment effect of camrelizumab in subgroups according to baseline characteristics. Correlations were examined with the Spearman rank correlation coefficients. Receiver operating characteristic curves that plotted sensitivity and 1 specificity of continuous variables and DCB were assessed by generating the area under the curve (AUC). All statistical analyses were done with SAS V.9.4 or R V.4.0.3.
Results
Patient characteristics and treatment
Between August 14, 2018, and December 30, 2019, 193 patients were screened for eligibility, and a total of 156 patients were enrolled. All enrolled patients received at least one study treatment and were included in efficacy and safety analyses. Patient baseline characteristics are listed in table 1. Most of the patients (84.6%) had an ECOG performance status of 1, and 41.0% of patients had undergone three or more lines of prior therapies. All patients had metastases, and 39.7% of them had metastases in at least three organs. At data cut-off on December 30, 2020, the median follow-up duration was 14.2 months (range 0.7–27.6). A total of 140 patients discontinued study treatment. Of them, 7 patients completed the 2-year camrelizumab treatment, and 109 patients discontinued due to disease progression. Other common reasons for discontinuation were patient decision (13 patients), AEs (5 patients), and investigator decision (3 patients) (online supplemental figure 1).
Table 1.
Baseline demographics and clinical characteristics
| Characteristic | Patients (N=156) |
| Age (years), median (range) | 48 (23–71) |
| <50 | 93 (59.6) |
| ≥50 | 63 (40.4) |
| Sex | |
| Male | 124 (79.5) |
| Female | 32 (20.5) |
| ECOG performance status | |
| 0 | 24 (15.4) |
| 1 | 132 (84.6) |
| Histology | |
| Undifferentiated non-keratinizing | 118 (75.6) |
| Differentiated non-keratinizing | 15 (9.6) |
| Non-keratinizing | 23 (14.7) |
| Metastases | 156 (100) |
| Metastatic organs (n) | |
| 1 | 37 (23.7) |
| 2 | 57 (36.5) |
| ≥3 | 62 (39.7) |
| PD-L1 expression (%) | |
| <1 | 36 (23.1) |
| ≥1 | 114 (73.1) |
| Unknown | 6 (3.8) |
| Prior lines of therapy | |
| 2 | 92 (59.0) |
| 3 | 41 (26.3) |
| ≥4 | 23 (14.7) |
Data presented as n (%) unless otherwise indicated.
ECOG, Eastern Cooperative Oncology Group; PD-L1, programmed cell death-ligand 1.
Antitumor activity
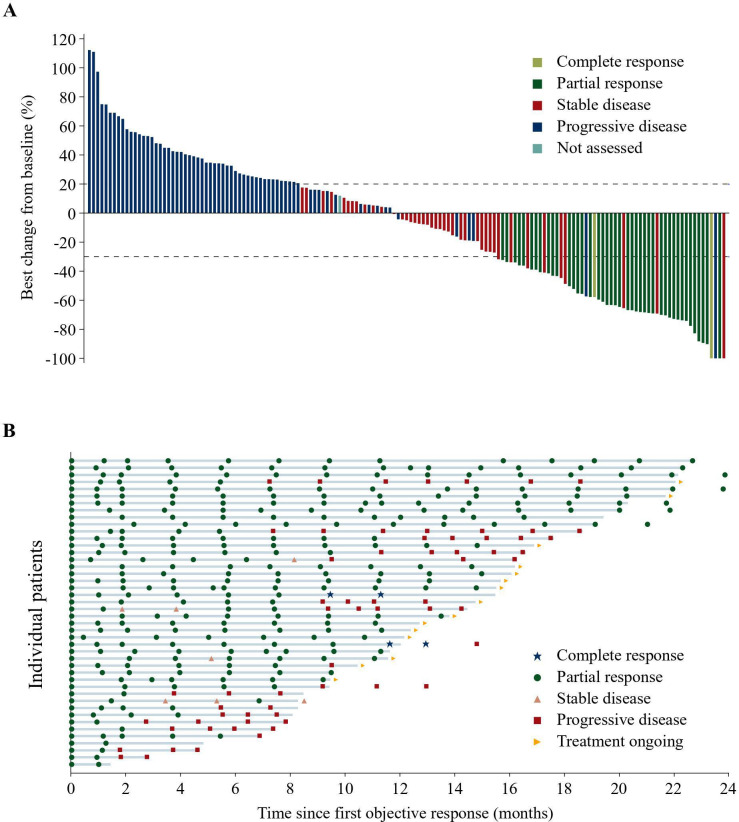
As of data cut-off, two patients (1.3%) achieved CR and 42 (26.9%) had PR per IRC. The ORR reached 28.2% (95% CI 21.3% to 36.0%), and the DCR was 54.5% (95% CI 46.3% to 62.5%). The investigator assessment gave similar results, with an ORR of 23.7% (95% CI 17.3% to 31.2%) (table 2). The change in target lesion in sum of the longest diameters are shown in figure 1A. The median TTR was 8.3 weeks (range 7.3–40.7) per IRC. The response and treatment durations of all responders are shown in figure 1B swimmer plot. Given that 26 (59.1%) of 44 responses remained ongoing, the median DOR was not reached. The median PFS by IRC was 3.7 months (95% CI 2.0 to 4.1), and the median OS was 17.4 months (95% CI 15.2 to 21.9) (figure 2). Objective response to camrelizumab was observed in all subpopulations according to subgroup analysis (online supplemental figure 2).
Table 2.
Antitumor activity according to IRC and investigator in the full analysis set
| Response | Per IRC (N=156) | Per investigator (N=156) |
| Best overall response, n (%) | ||
| CR | 2 (1.3) | 2 (1.3) |
| PR | 42 (26.9) | 35 (22.4) |
| SD | 41 (26.3) | 47 (30.1) |
| PD | 67 (42.9) | 67 (42.9) |
| NA | 4 (2.6) | 5 (3.2) |
| ORR, n (%) (95% CI) | 44 (28.2) (21.3 to 36.0) | 37 (23.7) (17.3 to 31.2) |
| DCR, n (%) (95% CI) | 85 (54.5) (46.3 to 62.5) | 84 (53.8) (45.7 to 61.9) |
| DOR, median (95% CI) | NR (9.5 to NR) | NR (13.0 to NR) |
| TTR (weeks), median (range) | 8.3 (7.3–40.7) | 8.3 (7.1–56.0) |
CR, complete response; DCR, disease control rate; DOR, duration of response; IRC, independent review committee; NA, not assessable; NR, not reached; ORR, objective response rate; PD, progressive disease; PR, partial response; SD, stable disease; TTR, time to response.
Figure 1.
Tumor response assessment according to independent review committee. (A) Best reduction from baseline in sum of the longest diameters of target lesions. (B) Treatment exposure and tumor response of patients who were assessed as complete response or partial response.
Figure 2.

Kaplan-Meier curves per independent review committee in the full analysis set. (A) Progression-free survival. (B) Overall survival.
Biomarker analyses
Tumor PD-L1 expression was assessed in 150 patients. Among these patients, 114 were PD-L1+ (defined as PD-L1 positive staining on ≥1% of tumor cells) and 36 were PD-L1–. The ORR was comparable between PD-L1+ and PD-L1– patients (29.8% (95% CI 21.6% to 39.1%) vs 25.0% (95% CI 12.1% to 42.2%) (online supplemental table 1). However, the ORR was higher in patients with high PD-L1 expression (88 patients, defined as PD-L1 positive staining on ≥10% of tumor cells) than those with low PD-L1 expression (62 patients, 35.2% (95% CI 25.3% to 46.1%) vs 19.4% (95% CI 10.4% to 31.4%)). In addition, we also observed longer median PFS (3.9 months (95% CI 2.7 to 7.8) vs 2.8 months (95% CI 1.8 to 3.8)) and median OS (19.9 months (95% CI 17.5 to not reached) vs 14.2 months (95% CI 10.6 to 17.5)) in patients with high PD-L1 expression than those with low PD-L1 expression.
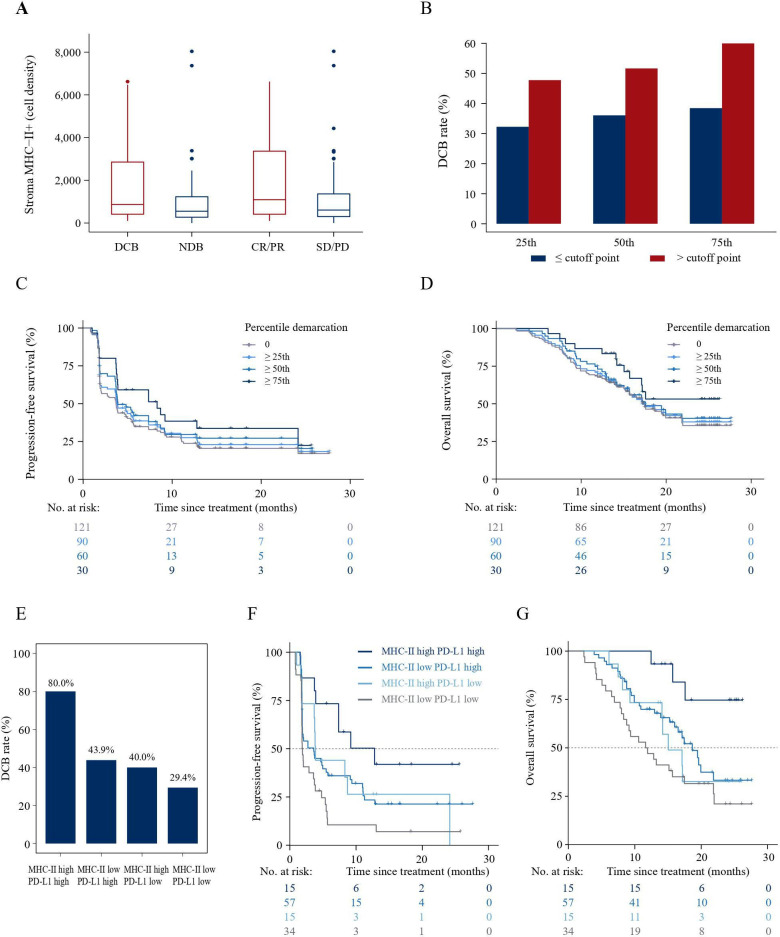
Multiplex immunofluorescence staining was done in 121 patients (online supplemental figure 3). No significant associations were observed between immune-related biomarkers with clinical outcomes in terms of objective response or DCB except for density of MHC-II+ cells in the stroma (online supplemental figure 4). Patients with DCB or objective response had higher density of stromal MHC-II+ cells than patients without DCB (median 868.1 (IQR 413.4–2854.0] cells/mm2 vs median 552.4 (IQR 258.4–1242.1) cells/mm2) or objective response (median 1091.8 (IQR 409.0–3411.7) cells/mm2 vs median 605.5 (IQR 298.0–1391.3) cells/mm2, respectively; figure 3A). We then examined how increasing cut-off points of MHC-II cell densities affected response to camrelizumab treatment. When MHC-II+ cell density was stratified into increasing quartiles, DCB rate, PFS and OS improved with increasing MHC-II+ cell density, especially in those with cell density above 75th percentile (>1538.0 cells/mm2, figure 3B–D). Higher DCB rates (60.0% vs 38.5%), longer median PFS (8.3 months (95% CI 3.7 to 24.1) vs 2.1 months (95% CI 1.9 to 3.7)), and improved median OS (not reached (95% CI 15.7 to not reached) vs 16.5 months (95% CI 12.8 to 19.6]) were observed in patients with stromal MHC-II+ cell density above versus below the 75th percentile.
Figure 3.
Clinical features and association of MHC-II+ cell density and PD-L1 expression with response to immunotherapy. (A) Cell density of stromal MHC-II+ cells among patients with DCB versus NDB, and among patients with CR and PR versus SD and PD. (B) DCB rate in patients with increasing cut-off points of MHC-II+ cell densities. (C) PFS in patients with stromal MHC-II+ cell densities above each percentile. (D) OS in patients with stromal MHC-II+ cell densities above each percentile. (E) The proportion of patients with DCB among patient groups defined by a composite variable of PD-L1 expression (≥10% vs <10%) and density of MHC-II+ cells in stroma (above vs below 75th percentile). (F) PFS among patient groups defined by a composite variable of PD-L1 expression (≥10% vs <10%) and density of MHC-II+ cells in stroma (above vs below 75th percentile). (G) OS among patient groups defined by a composite variable of PD-L1 expression (≥10% vs <10%) and density of MHC-II+ cells in stroma (above vs below 75th percentile). CR, complete response; DCB, durable clinical benefit; MHC-II, major histocompatibility complex class II; NDB, no durable benefit; OS, overall survival; PD, progressive disease; PD-L1, programmed cell death-ligand 1; PFS, progression-free survival; PR, partial response; SD, stable disease.
No correlation was found between PD-L1 expression and MHC-II+ cell density (Spearman p=−0.1027, online supplemental figure 5). PD-L1 expression and MHC-II+ cell density demonstrated similar predictive value on the likelihood of DCB (PD-L1 AUC 0.586, MHC-II+ AUC 0.637; online supplemental figure 6). When considered as a composite variable, patients with high PD-L1 expression level (positive staining on ≥10% of tumor cells) and high density of stromal MHC-II+ cells (above 75th percentile) were associated with the highest DCB rate, while patients with the presence of only one variable showed lower DCB rates, and the DCB rate was the lowest in patients with neither variable (figure 3E). Of note, the same trend was also observed when analyzing the association of this composite variable with PFS and OS (figure 3F, G, and online supplemental table 2).
At last, a higher proportion of patients with baseline negative plasma EBV DNA (39 patients) achieved objective response than those with positive plasma EBV DNA (117 patients, 41.0% vs 23.9%). The median PFS was longer in patients with negative EBV DNA status than patients with positive EBV DNA status (6.0 vs 2.7 months). The median OS was 22.7 vs 16.5 months, respectively (online supplemental table 3). Tumor burden analysis showed that patients with baseline positive plasma EBV DNA level had a longer mean (SD) diameter of target lesions compared with patients with negative plasma EBV DNA (64.3 (40.0) mm vs 40.9 (24.8 mm). Dynamic change of plasma EBV DNA level from baseline to the first post treatment assessment was also assessed during the study. Patients with ≥50% EBV DNA level decrease showed higher ORR (42.9% vs 6.8%) and longer median PFS (5.5 vs 1.9 months) than those with <50% decrease (online supplemental table 4).
Safety
AEs of any grade occurred in 155 (99.4%) of 156 patients. Of them, 52 patients (33.3%) had grade ≥3 AEs. Grade ≥3 treatment-related adverse events (TRAEs) were reported in 24 patients (15.4%, table 3), with the most common being increased gamma-glutamyltransferase (3.2%), anemia (3.2%), reactive capillary endothelial proliferation (RCEP, 1.9%), and increased alanine aminotransferase (1.9%). A treatment-related death resulting from disease progression was reported. Discontinuation of camrelizumab as a result of TRAE occurred in two patients (1.3%), and dose interruption due to TRAEs was reported in 19 patients (12.2%). Grade 3 immune-mediated AEs were reported in seven patients (4.5%), being RCEP (1.9%), increased alanine aminotransferase (1.9%), increased aspartate aminotransferase (0.6%), anemia (0.6%), and pneumonitis (0.6%). No grade 4 and 5 immune-mediated AEs occurred.
Table 3.
Treatment-related adverse events with all grades occurring in ≥5% of all patients
| Events | Patients (N=156) | |
| All grades | Grade ≥3 | |
| RCEP | 140 (89.7) | 3 (1.9) |
| Anemia | 43 (27.6) | 5 (3.2) |
| Hypothyroidism | 38 (24.4) | 0 |
| Aspartate aminotransferase increased | 37 (23.7) | 2 (1.3) |
| Fever | 34 (21.8) | 0 |
| Alanine aminotransferase increased | 27 (17.3) | 3 (1.9) |
| Asthenia | 27 (17.3) | 0 |
| Cough | 27 (17.3) | 0 |
| Pruritus | 22 (14.1) | 0 |
| Blood thyroid-stimulating hormone increased | 21 (13.5) | 0 |
| White blood cell count decreased | 19 (12.2) | 1 (0.6) |
| Proteinuria | 18 (11.5) | 0 |
| Hypoalbuminemia | 15 (9.6) | 0 |
| Productive cough | 13 (8.3) | 0 |
| Thyroxine-free decreased | 13 (8.3) | 0 |
| Rash | 12 (7.7) | 1 (0.6) |
| Blood creatinine increased | 12 (7.7) | 0 |
| Gamma-glutamyltransferase increased | 10 (6.4) | 5 (3.2) |
| Neutrophil count decreased | 10 (6.4) | 0 |
| Blood alkaline phosphatase increased | 8 (5.1) | 2 (1.3) |
| Occult blood positive | 8 (5.1) | 0 |
| Decreased appetite | 8 (5.1) | 0 |
Data presented as n (%).
RCEP, reactive capillary endothelial proliferation.
Discussion
In this study, camrelizumab monotherapy demonstrated promising antitumor activity in patients with pretreated R/M-NPC, with an ORR of 28.2%, a median PFS of 3.7 months and a median OS of 17.4 months. The safety profile of camrelizumab was manageable, with no new safety signals identified.
Several previous studies had investigated anti-PD-1 monotherapy in patients with R/M-NPC who failed platinum-based chemotherapy. Pembrolizumab showed an ORR of 25.9% among 27 patients with PD-L1 positive NPC in the KEYNOTE-028 study.5 Nivolumab showed an ORR of 20.5% in 44 patients with pretreated NPC in the NCI-9742 study.6 In the POLARIS-02 study (Toripalimab in Previously Treated Recurrent or Metastatic Nasopharyngeal carcinoma: A Phase II Clinical Trial), among 92 patients with NPC who failed at least two lines of chemotherapy, the ORR was 23.9%, and the median PFS and OS were 2.0 and 15.1 months, respectively.7 Our previous phase I study demonstrated an ORR of 34% and a median PFS of 5.6 months.8 Collectively, these findings strongly support the critical role of anti-PD-1 antibody monotherapy in chemotherapy-refractory patients with R/M-NPC.
Optimal biomarker to select patients who will benefit most from immunotherapy remains lacking in NPC. The predictive value of PD-L1, the most extensively studied biomarker for anti-PD-1 or anti-PD-L1 therapies, was inconclusive in NPC. In the NCI-9742 study, nivolumab provided a numerically higher ORR among patients with PD-L1+ tumors (≥1%) than those with PD-L1− tumors (33% vs 13%), but the difference was not significant, which could be due to the relatively small sample size (18 vs 23 patients).6 In the POLARIS-02 study with 190 patients,7 the ORRs were 27.1% and 19.4% in patient populations with PD-L1+ and PD-L1− R/M-NPC, and the difference still did not reach statistical significance either. By setting a higher threshold (>25%), the difference in ORR (38.1% vs 19.3%), PFS (median, 7.2 vs 1.9 months) and OS (median, unreached vs 15.1 months) among patients with a PD-L1 expression above or below the threshold enlarged. However, none of the differences were statistically significant. Recently, a phase III study reported that pembrolizumab monotherapy did not improve the OS compared with chemotherapy in patients with pretreated R/M-NPC.18 Of note, in a subgroup of patients with PD-L1 combined positive score of ≥10, the OS benefit was observed with chemotherapy versus pembrolizumab.18 In the present study, the ORR among patients with tumor PD-L1 expression level of ≥1% or <1% (29.8% vs 25.0%) was comparable. When using a higher threshold (≥10%), we observed higher ORR and improved median PFS and OS in patients with high PD-L1 expression than those with low PD-L1 expression. These results suggest that PD-L1 expression has certain predictive utility in NPC. However, further studies are needed to explore the optimal cut-off value, assays and scoring methods of PD-L1.
In the present study, we also examined the association of other immune-related biomarkers with outcome after camrelizumab therapy. We found that high density of MHC-II+ cell in the stroma was associated with improved DCB rate, longer median PFS and OS. Of note, there was no strong correlation between density of MHC-I+ cell nor CD8+ cell with clinical outcome. Our findings were consistent with previous studies. Roemer et al11 reported that 92% (11 of 12 patients) of patients with classic Hodgkin lymphoma who had membranous MHC-II expression on tumor cells reached CR to nivolumab, whereas the majority of patients who achieved CR had tumors that were negative for β2M and MHC-I.11 Consistent result was reported by Johnson et al, in which two independent cohorts of melanoma patients were treated with anti-PD-1 or anti-PD-L1 antibodies, and MHC-II positivity in tumor cells was significantly associated with better ORR, PFS and OS.10 Emerging evidence from basic research also highlight the important role of MHC-II antigen presentation pathway in immunotherapy. As MHC-II could bind to a higher diversity of tumor antigens as compared with MHC-I,19 20 tumor neoantigens were largely recognized by MHC-II.21 22 Importantly, there was no correlation between the expression of MHC-II and PD-L1, and a composite of MHC-II+ and PD-L1 expression further enriched patients who would benefit from camrelizumab. Of note, as these biomarker analyses were not prespecified, these findings should be validated in the future.
Pretreatment and the dynamic change of plasma EBV DNA level during radiotherapy, chemoradiotherapy, or chemotherapy have been established as a robust predictive biomarker in NPC.23–25 In the present study, the predictive value of pretreatment and dynamic change of plasma EBV DNA was assessed in patients undergoing immunotherapy. At baseline, patients with negative EBV DNA level had higher ORR and longer median PFS compared with patients with positive EBV DNA level. Notably, in our trial, a positive correlation between tumor load and baseline plasma EBV DNA level was observed. Therefore, we assumed that the prognostic value of plasma-negative EBV DNA may be due to the low shedding of EBV DNA into circulation. Furthermore, patients with ≥50% decrease in EBV DNA level from baseline to the first post-treatment assessment also had improved outcome than those with <50% decrease in EBV DNA level. Our findings were consistent with data in the PLOARIS-02 study,7 which further confirmed the value of plasma EBV DNA as a reliable predictor for clinical efficacy in patients with R/M-NPC receiving immunotherapy. Since almost all endemic NPCs are associated with EBV infection,26–28 whether the clinical outcomes of camrelizumab could be extrapolated to the non-endemic regions still needs further investigation.
Conclusions
Camrelizumab had encouraging clinical activity in patients with heavily pretreated R/M-NPC with manageable safety profile. The composition of both MHC-II+ cell density and PD-L1 expression could result in better patient selection, which should be validated in future studies.
jitc-2021-003790supp002.pdf (1.2MB, pdf)
Acknowledgments
We are grateful to all patients and their families and all members of the collaborative group in this trial. We thank Shuwen Biotech (Deqing, China) for immunofluorescence staining analyses. We would also like to acknowledge Qing Shen (Jiangsu Hengrui Pharmaceuticals) for contributions to biomarker analysis and interpretation. Medical writing support was provided by Yanwen Wang (Jiangsu Hengrui Pharmaceuticals) according to Good Publication Practice Guidelines.
Footnotes
Presented at: Part of this work was presented as an oral presentation at the 2020 European Society for Medical Oncology Virtual Congress, September 19–21, 2020; and the European Society for Medical Oncology Asia Virtual Congress 2020, November 20–22, 2020.
Contributors: LZ, JZ, WFa, and YZ contributed to study design and conception; YY, TZ, XC, JL, JP, XH, LL, YS, WFe, JX, KY, QY, QZ, DH, YS, GH, PL, LS, QL, LZ, WFa, and YZ contributed to patient recruitment and data acquisition; BZ contributed to statistical analysis and interpretation of the data. XQ contributed to interpretation of the data. YY, BZ, and XQ wrote the initial manuscript. All authors read and approved the final manuscript.
Funding: This work was supported by Jiangsu Hengrui Pharmaceuticals Co., Ltd; Chinese National Natural Science Foundation Project (numbers 81972556 and 82072558); and Medical Scientific Research Foundation of Guangdong Province (number C2018062).
Competing interests: BZ, XQ, and JZ are employees of Jiangsu Hengrui Pharmaceuticals. All other authors declare no competing interests.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. The data that support the findings of this study are available from the corresponding author upon reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
The study was conducted in accordance with the International Conference on Harmonization Good Clinical Practice guidelines and the Declaration of Helsinki. The study protocol and all amendments were approved by the independent ethics committee at each site. All patients gave written informed consent.
References
- 1.National Comprehensive Cancer Network . NCCN clinical practice guidelines in oncology: head and neck cancers. Vesion 2, 2020. Available: https://www.nccn.org/professionals/physician_gls/pdf/head-and-neck.pdf [DOI] [PubMed]
- 2.Prawira A, Oosting SF, Chen TW, et al. Systemic therapies for recurrent or metastatic nasopharyngeal carcinoma: a systematic review. Br J Cancer 2017;117:1743–52. 10.1038/bjc.2017.357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Larbcharoensub N, Mahaprom K, Jiarpinitnun C, et al. Characterization of PD-L1 and PD-1 expression and CD8+ tumor-infiltrating lymphocyte in Epstein-Barr virus-associated nasopharyngeal carcinoma. Am J Clin Oncol 2018;41:1204–10. 10.1097/COC.0000000000000449 [DOI] [PubMed] [Google Scholar]
- 4.Zhang J, Fang W, Qin T, et al. Co-expression of PD-1 and PD-L1 predicts poor outcome in nasopharyngeal carcinoma. Med Oncol 2015;32:86. 10.1007/s12032-015-0501-6 [DOI] [PubMed] [Google Scholar]
- 5.Hsu C, Lee S-H, Ejadi S, et al. Safety and antitumor activity of pembrolizumab in patients with programmed death-ligand 1-positive nasopharyngeal carcinoma: results of the KEYNOTE-028 study. J Clin Oncol 2017;35:4050–6. 10.1200/JCO.2017.73.3675 [DOI] [PubMed] [Google Scholar]
- 6.Ma BBY, Lim W-T, Goh B-C, et al. Antitumor activity of nivolumab in recurrent and metastatic nasopharyngeal carcinoma: an international, multicenter study of the mayo clinic phase 2 consortium (NCI-9742). J Clin Oncol 2018;36:1412–8. 10.1200/JCO.2017.77.0388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang F-H, Wei X-L, Feng J, et al. Efficacy, safety, and correlative biomarkers of Toripalimab in previously treated recurrent or metastatic nasopharyngeal carcinoma: a phase II clinical trial (POLARIS-02). J Clin Oncol 2021;39:704–12. 10.1200/JCO.20.02712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fang W, Yang Y, Ma Y, et al. Camrelizumab (SHR-1210) alone or in combination with gemcitabine plus cisplatin for nasopharyngeal carcinoma: results from two single-arm, phase 1 trials. Lancet Oncol 2018;19:1338–50. 10.1016/S1470-2045(18)30495-9 [DOI] [PubMed] [Google Scholar]
- 9.Thompson JC, Davis C, Deshpande C, et al. Gene signature of antigen processing and presentation machinery predicts response to checkpoint blockade in non-small cell lung cancer (NSCLC) and melanoma. J Immunother Cancer 2020;8:e000974. 10.1136/jitc-2020-000974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Johnson DB, Estrada MV, Salgado R, et al. Melanoma-specific MHC-II expression represents a tumour-autonomous phenotype and predicts response to anti-PD-1/PD-L1 therapy. Nat Commun 2016;7:10582. 10.1038/ncomms10582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Roemer MGM, Redd RA, Cader FZ, et al. Major histocompatibility complex class II and programmed death ligand 1 expression predict outcome after programmed death 1 blockade in classic Hodgkin lymphoma. J Clin Oncol 2018;36:942–50. 10.1200/JCO.2017.77.3994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li YY, Chung GTY, Lui VWY, et al. Exome and genome sequencing of nasopharynx cancer identifies NF-κB pathway activating mutations. Nat Commun 2017;8:14121. 10.1038/ncomms14121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li D, Qian L, Chen C, et al. Down-regulation of MHC class II expression through inhibition of CIITA transcription by lytic transactivator Zta during Epstein-Barr virus reactivation. J Immunol 2009;182:1799–809. 10.4049/jimmunol.0802686 [DOI] [PubMed] [Google Scholar]
- 14.Lin J-H, Lin J-Y, Chou Y-C, et al. Epstein-Barr virus LMP2A suppresses MHC class II expression by regulating the B-cell transcription factors E47 and PU.1. Blood 2015;125:2228–38. 10.1182/blood-2014-08-594689 [DOI] [PubMed] [Google Scholar]
- 15.Chinese Nasopharyngeal Carcinoma Clinical Staging Committee . Chinese nasopharyngeal carcinoma staging system 2017 edition (expert consensus on revised 2008 staging system for nasopharyngeal carcinoma). Chin J Radia Oncol;26:1119–24. [Google Scholar]
- 16.Gaule P, Smithy JW, Toki M, et al. A quantitative comparison of antibodies to programmed cell death 1 ligand 1. JAMA Oncol 2017;3:256–9. 10.1001/jamaoncol.2016.3015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.KEYTRUDA® (Pembrolizumab) [Prescribing Information]. Available: https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/125514s088lbl.pdf
- 18.Chan A, Lee V, Hong R. Results of KEYNOTE-122: A phase III study of pembrolizumab (pembro) monotherapy vs chemotherapy (chemo) for platinum-pretreated, recurrent or metastatic (R/M) nasopharyngeal carcinoma (NPC) [Oral presentation]. Europ Soc Med Oncol Congress 2021. [Google Scholar]
- 19.Axelrod ML, Cook RS, Johnson DB, et al. Biological consequences of MHC-II expression by tumor cells in cancer. Clin Cancer Res 2019;25:2392–402. 10.1158/1078-0432.CCR-18-3200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Johnson AM, Bullock BL, Neuwelt AJ, et al. Cancer cell-intrinsic expression of MHC class II regulates the immune microenvironment and response to anti-PD-1 therapy in lung adenocarcinoma. J Immunol 2020;204:2295–307. 10.4049/jimmunol.1900778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kreiter S, Vormehr M, van de Roemer N, et al. Mutant MHC class II epitopes drive therapeutic immune responses to cancer. Nature 2015;520:692–6. 10.1038/nature14426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alspach E, Lussier DM, Miceli AP, et al. MHC-II neoantigens shape tumour immunity and response to immunotherapy. Nature 2019;574:696–701. 10.1038/s41586-019-1671-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liu L-T, Tang L-Q, Chen Q-Y, et al. The prognostic value of plasma Epstein-Barr viral DNA and tumor response to neoadjuvant chemotherapy in advanced-stage nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys 2015;93:862–9. 10.1016/j.ijrobp.2015.08.003 [DOI] [PubMed] [Google Scholar]
- 24.Chan ATC, Hui EP, Ngan RKC, et al. Analysis of plasma Epstein-Barr virus DNA in nasopharyngeal cancer after chemoradiation to identify high-risk patients for adjuvant chemotherapy: a randomized controlled trial. J Clin Oncol 2018:3091–100. 10.1200/JCO.2018.77.7847 [DOI] [PubMed] [Google Scholar]
- 25.You R, Liu Y-P, Lin M, et al. Relationship of circulating tumor cells and Epstein-Barr virus DNA to progression-free survival and overall survival in metastatic nasopharyngeal carcinoma patients. Int J Cancer 2019;145:2873–83. 10.1002/ijc.32380 [DOI] [PubMed] [Google Scholar]
- 26.Stelow EB, Wenig BM. Update from the 4th edition of the World Health Organization classification of head and neck tumours: nasopharynx. Head Neck Pathol 2017;11:16–22. 10.1007/s12105-017-0787-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tsao S-W, Tsang CM, To K-F, et al. The role of Epstein-Barr virus in epithelial malignancies. J Pathol 2015;235:323–33. 10.1002/path.4448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hau PM, Lung HL, Wu M, et al. Targeting Epstein-Barr virus in nasopharyngeal carcinoma. Front Oncol 2020;10:600. 10.3389/fonc.2020.00600 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
jitc-2021-003790supp001.pdf (750.6KB, pdf)
jitc-2021-003790supp002.pdf (1.2MB, pdf)
Data Availability Statement
Data are available upon reasonable request. The data that support the findings of this study are available from the corresponding author upon reasonable request.