Abstract
Regional analgesia has been introduced successfully into the postoperative pain management after total knee arthroplasty, reducing pain scores, opioid use and adverse effects.
Combination of regional analgesia techniques is associated with better pain management and lower side effects than single regional techniques.
Adductor canal block provides good analgesia and considerably lower detrimental effect in muscular strength than femoral nerve block, enhancing surgical recovery.
Infiltration techniques may have equivalent analgesic effect than epidural analgesia and peripheral nerve blocks, however there should be awareness of dose dependent toxicity.
Novel long-acting local anesthetics role for regional analgesia is still to be determined, and will require larger randomized trials to support its advantage over traditional local anesthetics.
Cite this article: EFORT Open Rev 2021;6:1181-1192. DOI: 10.1302/2058-5241.6.210045
Keywords: blocks, regional analgesia, Total Knee Arthroplasty
Introduction
Total knee arthroplasty (TKA) is a widely used method to treat end-stage osteoarthritis and other disabling knee conditions, and its demand is expected to increase to more than 1 million procedures by the year 2030 in the United States.1-3 Therefore, increasing value of TKA has been an area of enhanced interest.3 Among the changes in practice in the last decade, we have seen a steady decrease in hospital length of stay (LOS), and a shift towards outpatient surgery.3,4 In 2018 the U.S. Centers for Medicare & Medicaid Services (CMS) finalized the 2018 Medicare Outpatient Payment System rule that removed TKA from the Medicare inpatient-only list of procedures. Altogether, the safety and general feasibility of cost-effective strategies across different TKA patient populations constitutes an area of increased interest and value.5 One of the facets that continues to require improvement is the relatively high incidence of postoperative severe pain, ranging from 10 to 36%, which produce dissatisfaction among patients after TKA, and increased hospital utilization.6,7
Different anesthetic approaches and combinations such us general anesthesia (GA), neuroaxial anesthesia (epidural or spinal) and/or peripheral nerve blocks have been used in TKA. GA, historically, has been associated to high rates of postoperative nausea, vomit and delirium.8 On the other hand, neuroaxial anesthesia reduces nausea, vomiting, cardiovascular and pulmonary complications and overall mortality when compared to GA.9,10 Regional analgesia (RA) have been used to optimize pain management during the postoperative phase of TKA.11 Most RA techniques use local anesthetics (LA), in lower concentration than anesthesia methods, to reduce pain and produce the least possible impairment in mobility.12 Increased interest in RA has been mainly due to its improvement of pain management with relevant reduction in opioids consumption due to its opioid-sparing effect, decrease risk of addiction and opioid crisis.13 Furthermore, RA can decrease opioid side effects such as urinary retention, constipation, nausea, vomiting, ventilatory depression and sedation which have resulted in lower LOS.14 RA expanded its versatility when ultrasound improved the accuracy of LA administration.15 Also, its role in decreasing risk of complications and LOS related to immobilization makes RA an ideal method for orthopaedic surgical procedures.16 RA facilitates physical therapy by reducing postoperative pain. However, some techniques may reduce motor function which in turn can delay recovery times.
This review article will serve as a guide of classic and novel regional analgesic techniques used in the early postoperative period after TKA, comparing and discussing advantages and disadvantages among them in addition to present promising advances in this area. For the purpose of this review, we address anesthetic techniques as part of the intraoperative management and analgesic techniques as a component of multimodal analgesia for the perioperative care after TKA.
Anesthesia for TKA
TKA has been performed under two main anesthetic techniques: I) GA; and II) neuroaxial anesthesia. The use of intravenous and inhaled anesthetics drugs in GA, in addition to eliminating pain and consciousness, also prevents motor repose, autonomic and cardiovascular reflexes.17 On the other hand, neuroaxial anesthesia utilizes local anesthetics to block sensory and motor nerves following a caudal direction from the spinal level the anesthetic was injected, with variable impact on autonomic nervous system.18 Overall there are two main approaches to neuroaxial anesthesia used in TKA: A) Subarachnoid (intrathecal) anesthesia in which the needle is inserted at the subarachnoid space at L4/L5 lumbar interspace to administer opioids or LA; and B) Epidural anesthesia where epidural space is targeted by the needle. Unlike the subarachnoid space, the epidural space is septated and it contains fat, lymphatics, veins and nerve roots.19 This non-continuous space may facilitate partial or unilateral effect during epidural anesthesia.20
Controversial results have been published comparing GA and neuroaxial anesthesia. While some authors found advantages in neuroaxial anesthesia over GA such as reduction in short-term complications21 including less blood transfusion22 and surgical site infections23, others failed to find differences other than lower LOS on neuroaxial anesthesia.24 In addition, epidural techniques are associated with higher incidence of urinary retention, pruritus and hypotension, compared to anesthetic regional techniques.25 Its higher incidence of side effects along with its technical complexity compared to spinal block, makes epidural anesthesia prone to obsolescence for TKA. A recent nationwide database study found that patients who undergo total joint arthroplasty with spinal anesthesia experience fewer 30-day complications and were less likely to have a non-home discharge than those with GA.10 A large 2019 meta-analysis named the International Consensus on Anaesthesia-Related Outcomes after Surgery group (ICAROS), which analyzed 94 studies comparing neuroaxial vs GA in hip and knee arthroplasty, suggests the use of neuroaxial anesthesia for knee arthroplasty based on reduction in infections, deep venous thrombosis, blood transfusions, pulmonary and renal complications; evidence level: low, weak recommendation.26
Regional Analgesia for TKA
Postoperative pain management contributes greatly to achieve enhanced recovery after surgery (ERAS) goals.27 Recognition of the sensory innervation of the knee plays a key factor on regional analgesia, discussed in Table 1. Regional analgesia uses different nerve block techniques as part of the multimodal analgesia arsenal to favor ERAS.28Techniques are presented in two different chronologic groups: 1) Classic Techniques; and 2) Novel Techniques.
Table 1.
Sensory Innervation of the Knee
| Compartment | Nerves | Considerations | Joint Supply | Cutaneous Supply |
|---|---|---|---|---|
| Anterior | Femoral nerve | Crosses behind the inguinal ligament and lateral to the femoral artery and provides branches to innervate each muscular component of the quadriceps muscle (Vastus Medialis, intermedious and lateralis branches) | The vastus medialis to the medial collateral ligament, The vastus lateralis branches end at the quadriceps tendon without innervating the capsule of the knee | The vastus medialis to the superomedial aspect, The vastus Intermedius to the anterosuperior aspect of the knee |
| Common fibular nerve | Provides articular (genicular) branches to knee, lateral superior, lateral inferior, recurrent. | Inferolateral capsule of the knee joint, proximal tibiofibular joint | Lateral aspect of the knee | |
| Saphenous nerve | Cutaneous branch of the Femoral nerve Runs into the adductor canal |
Infrapatellar Branch Descending Branch Antero inferior capsule of knee joint |
Medial and inferior aspect of the knee | |
| Posterior | Tibial nerve | Branch of the Sciatic nerve, provides the posterior articular nerve. | Articular (genicular) branches to knee medial superior, medial inferior, middle and capsular branches | Medial portion of the capsule, retinaculum, collateral ligaments of knee joint proximal and distal tibiofibular joint |
| Obturator nerve | Originates two main branches: anterior and posterior | Posterior branch to joint capsule, cruciate ligaments and synovial membrane | Anterior branch to medial aspect and mid-thigh | |
| Plexuses | Contributors to the plexus | Sensory innervation | ||
| Peripatellar | Femoral nerve: medial, intermediate, lateral femoral cutaneous nerves Saphenous nerve: infrapatellar branch Retinacular nerves: medial (terminal branch of nerve to vastus medius), lateral (direct branch of sciatic nerve) Nerve to vastus intermedius | Skin anterior, superior, inferior, medial and lateral to patella; retinacula; collateral ligaments and capsule of knee joint | ||
| Subsartorial | Saphenous nerve: infrapatellar branch Obturator nerve: anterior division Medial femoral cutaneous nerve Nerve to vastus medius | Cutaneous to medial side of knee, retinaculum, collateral ligaments and capsule of knee joint | ||
| Popliteal | Tibial nerve Sciatic nerve Obturator nerve | Retinaculum, anterior and posterior cruciate ligaments, collateral ligaments and capsule of knee joint | ||
Adapted from Pulsed radiofrequency of the composite nerve supply to the knee joint as a new technique for relieving osteoarthritic pain: a preliminary report. Pain Physician.2014;17(6):493-506.
Classic Techniques
Neuroaxial Analgesia
This method uses LA or opiates through a subarachnoid or epidural access to relief pain after TKA, applying single shot or continuous (catheter) technique. Continuous subarachnoid analgesia is associated with better hemodynamic stability, pain management, and less nausea and vomit than single shot technique in lower limb surgery29. Single shot epidural analgesia is limited to brief pain relief (<6 hours)25 compared to 48 hours with standard epidural catheters and 6 weeks with tunneled epidural catheters30.Neuroaxial techniques are frequently associated with hypotension, urinary retention and pruritus25; major complications such as spinal infections, bleeding, nerve damage, wrong route and cardiovascular collapse and respiratory depression have to be considered30
One metanalysis found no difference on analgesic effect in neuroaxial techniques compared to peripheral nerve blocks for TKA.31 However, neuroaxial analgesia was associated with higher incidence of hypotension, urinary retention, nausea and vomiting.31 On the other hand, researchers found that local infiltration provides better analgesia management than either subarachnoid32 or epidural analgesia33 for TKA. In favor of reducing opioid use, epidural analgesia provides superior pain control than intravenous opioids.34,35 Advantages, disadvantages and contraindications of postoperative regional analgesic techniques for TKA are discussed in Table 2.
Table 2.
Regional Analgesia for TKA
| Analgesic Procedure | Advantages | Disadvantages | Contraindications |
|---|---|---|---|
| Intrathecal analgesia | • Relatively easy technique • Bilateral analgesic effect for bilateral TKA |
• Effect in sympathetic innervation (urinary retention and hypotension ) • Respiratory depression related to intrathecal opioid use • Pruritus • Unnecessary bilateral block • Risk of infection and nerve damage • Delays mobilization |
• Elevated intracranial pressure • Infection on the injection site • Risk of hypotension (hypovolemia) • Thrombocytopenia or coagulopathy |
| Femoral nerve block | • Easy access with or without ultrasound guidance • Excellent analgesia • Good predictable course of catheter with ultrasound guidance |
• Delays mobilization • High risk of falls |
• Patient inability to positioning • Allergy to LAs • Preexisting coagulopathies (endogenous or iatrogenic) • Active infection on the injection site • If no USG guidance, anatomic anomalies • affecting physical • landmarks identification • Pre-existing neuropathies affecting the distribution of the block |
| Sciatic nerve block (posterior) | • Analgesia on the posterior aspect of the knee • Adjuvant effect on anterior compartment blocks |
• Relatively deep block • Requires prone/ semiprone position • Delays mobilization |
|
| Adductor canal block (ACB) |
• Allows early mobilization and recovery time • Continuous technique provides the highest analgesic effect73 • Higher opioid-sparing effect than LAI78,79 • Easy ultrasound guide access68 |
• Tunneling is required in some cases | |
| iPACK | • Adjuvant analgesic effect on ACB • Analgesia on the posterior aspect of the knee • Minimal impact on mobilization |
• Limited to single shot technique • Short analgesic effect • Risk of foot drop |
|
| Local anesthetic infiltration (LAI) | • Easy intraoperative administration • Adjuvant analgesic effect • Minimal impact on mobilization |
• Increased risk of toxicity101
• Short analgesic effect • Risk of infections with intraarticular catheter |
|
| Genicular nerve block | • No risk of toxicity (no LA use) | • Requires Fluoroscopic and trained staff • USG guidance still in investigation • Scarce clinical evidence |
• Bleeding diathesis • Infection at the site |
| Cryoanalgesia | • No risk of toxicity (no LA use) | • Unpredictable analgesic duration • Risk of permanent sensory and motor block • Scarce clinical evidence |
• Raynaud syndrome • Cryoglubulinemia • Bleeding disorders • Active infection on the injection site120 |
Comparison among postoperative analgesic techniques for TKA. All thechniques are rarely associated with infectious complications. Neuroaxial procedures are related with 1.1- 2.5 infections per 100.000 neuroaxial blocks. Risk factors of infectious complications in peripheral nerve blocks are: ICU hospitalization, duration of catheter more than 48 hrs, lack of antibiotic prophilaxis, catheters in the femoral region and number of catheter dressing changes are considered risk factors of infectious complications in peripheral nerve blocks.
Three in one Block
Described by Winnie et al.36, its original purpose was to block the lumbar plexus retrogradely using high amounts of LA (>20ml). This technique uses a single shot local anesthetic to target the 3 main nerve branches from the lumbar plexus: femoral, lateral femoral cutaneous, and obturator nerves. Moreover, Rosenblatt37 described that a catheter can be placed into the femoral sheath to extend the analgesic effect during the postoperative period. There is a lack of evidence comparing three in one block on its two variations: single shot and continuous administration of LA. However, it is well documented that a single shot administration of LA can provide a sensitive block for more than 24 hours.38 Additionally, one shot three in one block reduces morphine consumption after knee surgery.39,40
Three in one catheter was promoted due to its similar analgesic effect and lower risk when compared to epidural catheter. Three in one block is an alternative to avoid classic side effects related to epidural analgesia.41 The use of catheter in three in one block allows continuous administration of the local anesthetics, increasing the analgesic effect in the femoral or saphenous nerves.42
There are few studies comparing three in one block against other regional analgesic techniques. Besides, none of them were for knee surgeries. Comparisons were made in femur fractures surgeries. One study compared three in one block vs fascia iliaca block which uses an anterior approach variation of the femoral nerve and the lateral femoral cutaneous nerve. Researchers found that both techniques provide adequate analgesia but fascia iliaca block presented faster and more uniform nerve blockade.43
Nowadays, one in three block is not frequently used as before. One of the causes is its non- homogeneous effect in all three main lumbar plexus branches. Studies have shown just a 4% success rate in terms of achieving the obturator nerve block, relating to the poor analgesic effect on the medial aspect of the knee.44 In fact, researchers proposed to change the term of this technique to two in one block due to its almost no effect in the obturator nerve. Also, the unpredictability of the course of the catheter placed without ultrasound guidance decreases its success rate.45
Femoral nerve Block
Described in 195246, femoral nerve block (FNB) can provide sufficient analgesia to the anterior aspect of the thigh including motor blockade of the muscles in the anterior compartment. It can be combined with sciatic and obturator nerve block to allow anesthesia for knee surgeries. FNB was initially performed blindly, by inserting a needle 1-1.5 cm laterally to the femoral artery pointing it to the midpoint of the inguinal ligament. In recent years clinicians prefer to use ultrasonography (USG) to enhance technique accuracy.47
FNB can be performed as a single anesthetic shot or using a catheter for continuous analgesia. Several meta-analyses comparing single shot vs. continuous FNB have contradictory findings. While some declare lower morphine consumption48 and lower pain scores after TKA in the continuous method49, others found no difference with the single-shot method.50,51 Elderly patients may benefit from the combination of FNB and GA. One study reported decreasing intraoperative and postoperative analgesic use, recovery and extubation times in patients with advanced ages who underwent TKA under GA plus FNB.52 When compared against epidural analgesia, FNB has no impact on the sympathetic innervation and produces less incidence of urinary retention.53
On the other hand, this method has substantial effect on mobility. Researchers have found that FNB, single shot or catheter, decreases the motor strength of the quadriceps muscle, increases recovery time and risk of falls compared to adductor canal block (ACB) 54,55. Moreover, there is no difference in pain control between FNB and ACB.56,57 However, FNB showed superior analgesic effect against local infiltration. On a randomized control trial, 194 patients received FNB or infiltration for TKA, the FNB group had significantly lower amount of opioid use compared to the infiltration group.58
Sciatic Nerve Block
The classic posterior approach was first described in 1923 by Labat. There have been several other variations described, some are the anterior approach, parasacral and subgluteal modifications. Nowadays, ultrasound guided sciatic nerve block is commonly used. USG identifies the sciatic nerve in between the greater trochanter and the ischial tuberosity, the nerve lies over quadratus femoris beneath the gluteus maximus. SNB is more a complement than an absolute analgesic resource for knee surgeries. SNB contribute with analgesic effect to the posterior aspect of the knee where FNB has no influence. Evidence shows that SNB increases the analgesic effect during the first 12 postoperative hours in patients who received FNB for TKA59, but also can deteriorates postoperative mobilization.60 Researchers have made efforts to predict the need of SNB as additional pain management in those patients who received FNB for TKA61. Factors associated with a higher probability of postoperative SNB requirements were: younger age, lower BMI, depression, short surgical procedures under peripheral nerve blocks and infiltration anesthesia.
SNB has also been compared to local infiltrations when an additional block to FNB is needed for TKA. Some authors have claimed better analgesic effect, reduction on opioid use, nausea and vomiting events for the combination of FNB plus SNB in comparison to FNB plus local infiltrations.62,63 Although, some other investigators found no difference in pain control between these two strategies64. In addition, SNB can be used in combination with ACB. Investigators found lower postoperative pain scores at rest and in movement when ACB plus SNB technique was compared to ACB alone65.
Adductor Canal Block
Van der Wal et al. in 1993, described ACB as a transartorial approach, using landmarks to block the saphenous nerve.66 Unlike FNB, this technique achieves more sensorial than motor block. The Adductor canal (AC) contains distal branches of the femoral nerve such as the saphenous nerve, the obturator nerve as well as sensory and motor branches for the quadriceps muscle. Nowadays, ultrasound is commonly used to identify the AC (Fig.1).67 In supine position, the leg is externally rotated and the probe is positioned at the midpoint of the thigh on its medial aspect. The superficial femoral artery is used as a reference, the AC is located anterolaterally to the artery. The needle is advanced and a particular “pop” indicates that the tip pierced the vastoadductor membrane, which is the roof of the adductor canal. A single dose of local anesthetic is injected or a catheter is placed. In practice, clinicians prefer tunneling the AC catheter due to its proximity to the surgical field. Although, tunneling the AC catheter may increase the time of the procedure, it decreases the risk of intraoperative dislodgement.68
Figure 1.
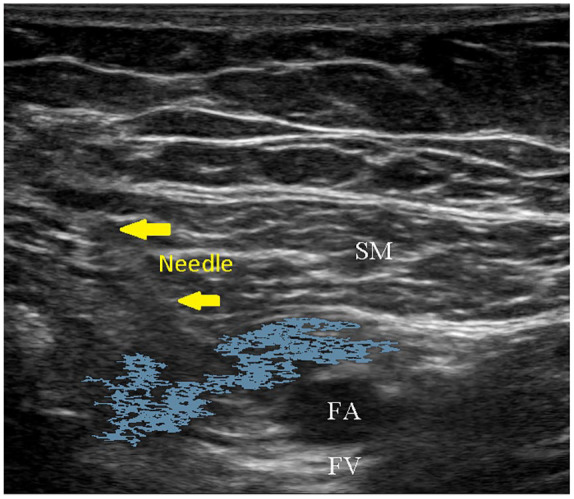
Adductor canal block. The needle (yellow arrows) is injecting local anesthetic (blue area) which is spreading into the adductor canal. In the proximities, the superficial femoral artery (FA) is anterior to the superficial femoral vein (FV). The Sartorius muscle (SM) is more superficial.
ACB’s main advantage over previous techniques is its low impact on muscular strength. Numerous publications show that ACB has less detrimental effect on the quadriceps strength compared to FNB. In particular, ACB is associated with earlier mobilization and recovery times with equivalent pain scores compared to FNB.57,69,70 Similarly, researchers found that ACB in volunteers reduced 8% of quadriceps strength compared to 49% in FNB.71 A recent meta-analysis found that continuous ACB deteriorates less the quadriceps strength compared to continuous FNB and it is associated with better rehabilitation outcomes.72 Moreover, researchers have compared single shot ACB and ACB catheter. Multiple studies show that continuous ACB provides better analgesia, less postoperative opioid use and shorter rehabilitation periods compared to single-shot ACB 73-76. However, some others found that the superiority of ACB catheter over ACB single-shot was only presented after the second postoperative day when presumably the single dose of LA has worn off72,77. Other advantages have also been described for ACB. ACB presents less postoperative opioid consumption than local infiltrations technique after TKA; however, both provide equivalent pain control and impact on muscle strength.78,79 A recent meta-analysisreviewed a substantial number of randomized controlled trials comparing different RA techniques for TKA.80 Continuous ACB showed a solid superiority over other techniques, results are summarized in Table 3.
Table 3.
Comparison of Regional Analgesia techniques in TKA
|
Comparision A vs B |
Rest VAS at 24 h |
Rest VAS At 48h |
Total OMEQC |
ROM |
|---|---|---|---|---|
| ACB vs PAI | A≃B | A≃B | A>>>B* | A≃B |
| ACB + PAI vs PAI | A>>B* | A≃B | A>>>B* | A>>>B* |
| ACB + PAI vs ACB | A>>B* | A≃B | A≃B | A≃B |
| cACB vs ACB | A>>B* | A>>>B* | A>>>B* | A>>>B* |
| LB vs PAI | A≃B | A≃B | A≃B | A≃B |
Comparasion of weighted mean difference (WMD) (accumulative differences of studies weighted by the sample size) of studies with the same clinical outcomes and interventions. Two posoperative analgesic strategies (A vs B) after TKA were compared. Evaluating visual analoge scale (VAS) at rest, 24h and 48h posoperatively, total oral morphine equivalents consumption (OMEQC) and Range of Motion (ROM) are explained as no difference (A≃ B), small superoirity (A>B), moderate superiority (A>>B), large superiority (A>>>B) by the magnitude of the WND ( 0, 0-0.2, 0.2-0.8, >0.8 respectivily). ACB, adductor canal block; cACB, continuous adductor canal block; PAI, periarticular infiltration; LB, Liposomal Bupivacaine.
p value was <0.05
Adapted from Journal of Clinical Anesthesia Volume 68, February 2021, 11009.
Novel Techniques
Infiltration between the popliteal artery and capsule of knee (iPACK) block
iPACK block was developed by Sinha in 2012. The aim of iPACK block is to control the pain at the posterior aspect of the knee after TKA without causing foot drop.81 This technique can block important genicular nerves such as articular branches of tibial and common peroneal nerves, posterior branches of the obturator nerve, and medial genicular nerve.82 The needle is inserted in a trajectory from anteromedial to posterolateral at the distal metaphyseal level of the femur in between the shaft of the femur and the popliteal artery (Fig. 2).83 iPACK block is used mostly in conjunction with FNB and its advantages are still been studied. Multiple researchers suggest that iPACK block can enhance the analgesic effect, lower opioid consumption, and ambulation time of ACB. 84-87 iPACK block was found to be superior to periarticular infiltrations when it was required to improve the effect of ACB.88 Authors have reported a low incidence of foot drop after iPACK block89, hypothetically due to spread of the LA to the tibial and peroneal nerves. There are some concerns regarding the trajectory of the needle; for example, some authors intuit an unintentional saphenous nerve injury related to its thinness, which makes it difficult to identify even with the use of USG.90
Figure 2.
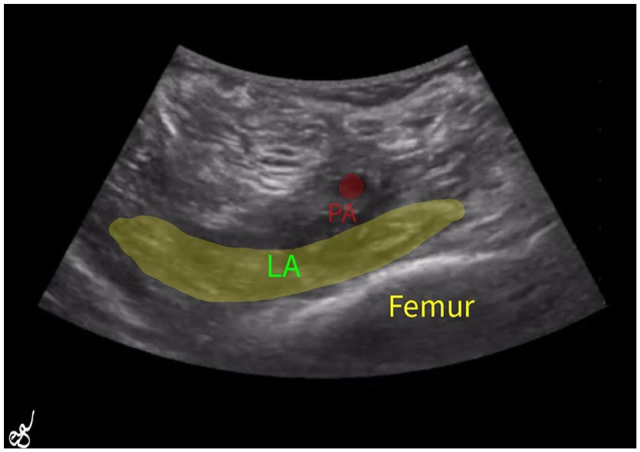
iPACK. The local anesthetic is distributed transversally between the Popliteal Artery (PA) and the Femur.
Local Anesthetic Infiltration (LAI)
This technique consists of a systematic intraoperative administration of LA in the periarticular and intraarticular tissues of the knee. There is no consensus to guide the best use of LAI91, often surgeons perform this technique using plain LA or combination of analgesic medications. Generally, the cocktail comprehends a high volume (150-170 mL) of a mixture of 0.2% ropivacaine or 0.125% levobupivacaine plus ketorolac and epinephrine.92 The systematic injection occurs in 3 phases during a period of 1 hour to decrease risk of toxicity. First, the posterior capsule is infiltrated with the mix, then deep tissues around the medial and lateral collateral ligaments and wound edges; and subsequently, the subcutaneous tissue is injected. Also, an intraarticular catheter can be placed for additional administration of LA during the postoperative period. Researchers have seen better short term pain control when the intraarticular catheter was inserted compared to single-shot LAI.93 However, the same researchers suggest considering the risk of infection related to the intraarticular catheter. Compression bandage plays a key factor to extend the analgesic effect of LAI.94.
Several meta-analyses have compared the efficacy of LAI against other postoperative analgesic strategies. LAI is associated with superior analgesic effect than epidural analgesia33 with lower incidence of nausea and vomiting and a wider range of articular motion.95 In the case of FNB, there was a similar effect in pain control compared to LAI.96 Importantly, periarticular infiltration technique was superior to FNB in avoiding muscle weakness.97 Other studies have questioned the benefit to adding LAI to the ACB. While some have found benefit in the combination to reduce pain and opioid consumption98, others have not seen a clinical difference.99 Reports about complications related to this technique point to the dose and speed in which the infiltrations were administrated 92,100. A high dose of adrenaline in LAI given in a short period of time can cause high blood pressure with ST and T wave alterations.100
Genicular Nerve Block
This method uses radiofrequency ablation (RFA) of the genicular nerves (knee joint nerves). Although, RFA was primarily investigated to cure intractable pain due to advanced cancer in the '60s101 and to treat pain from the spinal facet joints since the '70s102, nowadays is also used for non-surgical treatment in advanced osteoarthritis of the knee.103 Most recent applications include postoperative chronic pain management after TKA.104 With fluoroscopic guidance, pain physicians use needles to target the periosteal areas at the superior lateral, superior medial, inferior medial borders of the knee. A high-frequency current travels throughout the needle until its tip where it causes neurolysis to the surrounded nerves.103
Despite its wide use in other areas, there is limited evidence supporting RFA for pain management after TKA. One of the first cases reported is a 48-year-old male with persistent severe pain after TKA, using both fluoroscopic and ultrasound guidance, the genicular block was performed. The patient reported significant improvement in pain scores; muscular strength and range of motion at 3 months follow up.105 Later on, similar results were described in another case report 104. A recent study showed promising results in the use of ultrasound to guide the genicular nerve block for TKA.106 One randomized clinical trial compared the genicular nerve block against local anesthetic and corticoid therapy in patients with persistent pain after TKA107. Similar pain reduction and improvement in physical function were obtained in both groups, portraying genicular nerve block with RFA as an alternative to conventional treatment. However, more studies are needed to fully include this technique as an option for postoperative pain management after TKA.
Long-acting Anesthetics
Pain after TKA is directly associated with low mobilization which in turn is related to high morbidity and prolonged hospital stay.108 Pain management needs to be assured during the postoperative period for a considerable time after TKA. Consequently, duration of the action of LA is one of the key features in RA for TKA. LA with high affinity for proteins present longer anesthetic effect. Lipid solubility is another factor associated with prolonged anesthetic effect. Lipid-soluble LA can remain longer in the proximity of the neural membranes in a more continual release.109 Also, adjuvants increase the duration of LA; some of them are alpha 2 agonists, steroids, magnesium and the vasoconstrictors. Ropivacaine and bupivacaine are the two most frequently used long-acting LA. In recent years the liposomal version of bupivacaine has drawn the attention of physicians due to its promising longer effect. Performance of different LA is illustrated in Table 4.110
Table 4.
Local Anesthetics Performance in Peripheral Nerve Blocks
|
Anesthetic |
Onset (minutes) | Duration of Anesthesia (hours) | Duration of Analgesia (hours) | Toxicity considerations* |
|---|---|---|---|---|
| 2% lidocaine | 10 - 20 | 2 - 5 | 3 - 8 | High CNS toxicity in neuroaxial anesthesia |
| 1.5% mepivacaine | 10 - 20 | 2 - 5 | 3 - 10 | |
| 0.2% ropivacaine | 15 - 30 | n/a | 5 - 16 | Lower myotoxicity |
| 0.5% ropivacaine | 15 - 30 | 4 - 12 | 5 - 24 | |
| 0.25% bupivacaine | 15 - 30 | n/a | 5 - 26 | Higher myotoxicity, neurotocicity and cardiotoxicity (tachycardia and ventricular fibrilation) Chondrotoxic |
| 0.5% bupivacaine (+epi) | 15 - 30 | 5 - 15 | 6 - 30 |
Reactions to Local Anesthetics (LA) are rare and mostly are secundary to intravascular administration or absortion. Local toxicity (myotoxicity and neurotocicity) differ among LAs, bupivacaine > procaine > tetracaine >ropivacaine. Systemic reactions include, neurotoxicity(agitation,dizziness, myoclonic responses, nistagmus,disartria, muscle contractures, perioral parestesias, metallic taste,tinnitus, speech disorders, tonic-clonic seizures,respiratory depression (hypoxia, acidosis) and coma) and cardiotoxicity (tachycardia, hypertension (initially),hypotension and bradycardia (severe toxicity),miocardial depression and low cardiac output associated with arrhythmias (PR prolongation, branch blocks, ventricular ectopia, ventricular tachycardia, ventricularfibrilation, torsade de pointes, sinus arrest,asystole)
Adapted from Hadzic's Peripheral Nerve Blocks and Anatomy for Ultrasound-Guided Regional Anesthesia, 2nd 2. Local Anesthetics: Clinical Pharmacology and Rational Selection Jeff Gadsden
Pharmaceutic companies have modified bupivacaine in order to improve its performance. Levobupivacaine is less neurotoxic and cardiotoxic due to modifications made in the original structure of bupivacaine; but at the same time, it preserves its original potency and effect.111 Liposomal bupivacaine (Exparel; bupivacaine liposome injectable suspension, Pacira Pharmaceuticals, Inc., Parsippany, NJ, USA) uses a multivesicular configuration to reduce the speed of degradation of bupivacaine (Fig. 3); in consequence, its analgesic duration is longer than plain bupivacaine achieving 72 hours of analgesia. The Food and Drug Administration (FDA) approved liposomal bupivacaine for intraoperative infiltrations and interscalene brachial plexus block.112
Figure 3.
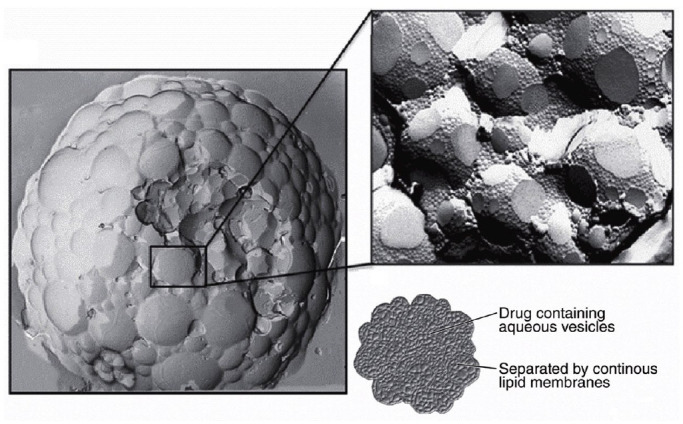
—A) Scanning electron micrographic image of DepoFoam with bupivacaine; B) diagram representing the polyhedral, nonconcentric aqueous chambers filled with medication (with permission from Pacira Pharmaceuticals, Inc.).
A recent narrative review concluded that the current evidence does not support the routine use of liposomal bupivacaine over standard LA for postoperative pain management.113 Specifically for TKA, liposomal bupivacaine has been studied both in peripheral nerve blocks and LAI analgesic techniques with controversial results. Some researchers found that liposomal bupivacaine is associated with high analgesic effectiveness in peripheral better pain scores at later time, reduction in morphine consumption and less nausea than plain bupivacaine for articular infiltrations.114 Similarly, a recent meta-analysis showed that periarticular injection with liposomal bupivacaine is associated with faster functional recovery but no difference in pain scores was seen when compared with FNB.115 However, another meta-analysis compared liposomal bupivacaine in periarticular injections for TKA with traditional LAs and found no clinical difference in pain reduction neither opioid consumption116. Although, the authors acknowledge the lack of studies with comparable procedures, which may limit their conclusions. Similarly, No clinical advantage was found when liposomal bupivacaine was compared to ropivacaine in ACB for TKA.117
Most recently, an investigational drug called HTX-011 (Heron Therapeutics, Inc. San Diego, CA, USA) has been studied. It is composed of bupivacaine and meloxicam in a bioerodible polymer. The purpose to include meloxicam is to decrease local inflammation to maintain a more physiological pH locally and decrease peripheral sensitization.118 HTX-011 is directly applied around periarticular tissues not using a needle. Although, this Drug has not FDA approval, a phase 2b trial in total knee arthroplasty has finished. The researchers found superior reduction in pain scores in patients who received HTX-011 during TKA compared to periarticular injections with plain bupivacaine during the first 72 hours after surgery119.
Cryoanalgesia
Cryoanalgesia, also called cryoneurolysis, is a method to temporarily block nerves through very low temperatures. It was first described in 1961 using a probe with liquid nitrogen to create ice crystals which in turn produced severe endoneural edema disrupting neural conduction.120 Nowadays, more complex and narrow-gauge probes using N2O or CO2 create an ice-ball with temperatures ranging from −70°C to −90°C to ablate the nerves reversely. Duration of the block is unpredictable due to the factors involved (temperature, time of exposure and nerve diameter) but usually is count in weeks or months. There is few clinical evidence about the use of cryoanalgesia in TKA. Five patients (Three with knee surgery and two with shoulder surgery) received cryoanalgesia postoperatively and the pain scores and opioid use was recorded. All patients described pain scores no more than 2 on a 0-10 scale and opioid consumption was lower compared to historic controls.121 Furthermore, one retrospective study found that the addition of cryoanalgesia to the standard multimodal pain management five days before TKA reduces significantly length of stay and opioid consumption postoperatively.122 Although, cryoanalgesia does not represent systemic toxicity, the risk of complete sensory and motor block along with its uncertain effect time may limit its use.
In summary, RA has been successfully incorporated into the postoperative analgesic arsenal for TKA. Evidence supports its roll to improve analgesic management and decrease opioids use. Chronologically, a more caudal approach has been developed in order to selectively target sensitive nerve branches and avoid motor impact. Although, some techniques are associated with deleterious effect on mobilization, novel techniques apparently bypass this disadvantage but still more evidence is needed to fully implement them. Combination of RA techniques can improve the analgesic effect. Pharmaceutics have also made efforts to improve the performance of LAs. New LAs have been promoted as longer duration drugs than previous ones but requires further proof with large randomized clinical trials. Cryoanalgesia is still unpredictable and represents an undiscovered field.
Conclusion
Orthopedic procedures, including TKA, demands a multimodal analgesic approach. This need to provide a diversified pain management comprises an advancement in the field, increasing interest and value in new analgesic techniques to improve patients’ outcomes and satisfaction.
Acknowledgments
We thank Dr. Ece Yamak Altinpulluk for donating the iPACK block ultrasound, seen in Figure 2.
Footnotes
ICMJE Conflict of interest statement: The authors declare no conflict of interest relevant to this work.
OA licence text: This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Price AJ, Alvand A, Troelsen A, et al. Knee replacement. Lancet. 2018;392:1672-1682. [DOI] [PubMed] [Google Scholar]
- 2. Inacio MCS, Paxton EW, Graves SE, Namba RS, Nemes S. Projected increase in total knee arthroplasty in the United States - an alternative projection model. Osteoarthritis Cartilage. 2017;25:1797-1803. [DOI] [PubMed] [Google Scholar]
- 3. Siddiqi A, Warren JA, McLaughlin J, et al. Demographic, Comorbidity, and Episode-of-Care Differences in Primary Total Knee Arthroplasty. J Bone Joint Surg [Am]. 2021;103-A:227-234. [DOI] [PubMed] [Google Scholar]
- 4. Cleveland Clinic OME Arthroplasty Group. Understanding the main predictors of length of stay after total hip arthroplasty: patient-related or procedure-related risk factors? J Arthroplasty. 2021;36:1663-1670.e4 [DOI] [PubMed] [Google Scholar]
- 5. Anis HK, Strnad GJ, Klika AK, Zajichek A, Spindler KP, Barsoum WK, Higuera CA, Piuzzi NS. Developing a personalized outcome prediction tool for knee arthroplasty. J Bone Joint Surg [Br]. 2020;102-B:1183-1193. [DOI] [PubMed] [Google Scholar]
- 6. Kim DH, Pearson-Chauhan KM, McCarthy RJ, Buvanendran A. Predictive Factors for Developing Chronic Pain After Total Knee Arthroplasty. J Arthroplasty. 2018;33:3372-3378. [DOI] [PubMed] [Google Scholar]
- 7. Elmallah RK, Chughtai M, Khlopas A, et al. Pain Control in Total Knee Arthroplasty. J Knee Surg. 2018;31:504-513. [DOI] [PubMed] [Google Scholar]
- 8. Turnbull ZA, Sastow D, Giambrone GP, Tedore T. Anesthesia for the patient undergoing total knee replacement: current status and future prospects. Local Reg Anesth. 2017;10:1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rodgers A, Walker N, Schug S, et al. Reduction of postoperative mortality and morbidity with epidural or spinal anaesthesia: results from overview of randomised trials. BMJ. 2000;321:1493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Warren J, Sundaram K, Anis H, et al. Spinal Anesthesia Is Associated With Decreased Complications After Total Knee and Hip Arthroplasty. J Am Acad Orthop Surg. 2020;28:e213-e221. [DOI] [PubMed] [Google Scholar]
- 11. Bauer MC, Pogatzki-Zahn EM, Zahn PK. Regional analgesia techniques for total knee replacement. Curr Opin Anaesthesiol. 2014;27:501-506. [DOI] [PubMed] [Google Scholar]
- 12. Columb M, Gall I. Minimum local analgesic concentration of local anaesthetics. Contin Educ Anaesth Crit Care Pain. 2010;10:114-116. [Google Scholar]
- 13. Lee BH, Kumar KK, Wu EC, Wu CL. Role of regional anesthesia and analgesia in the opioid epidemic. Reg Anesth Pain Med. 2019;44:rapm-2018-100102. [DOI] [PubMed] [Google Scholar]
- 14. Liu Q, Chelly JE, Williams JP, Gold MS. Impact of peripheral nerve block with low dose local anesthetics on analgesia and functional outcomes following total knee arthroplasty: a retrospective study. Pain Med. 2015;16:998-1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wahal C, Kumar A, Pyati S. Advances in regional anaesthesia: A review of current practice, newer techniques and outcomes. 2018;62(2):94-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Stein BE, Srikumaran U, Tan EW, Freehill MT, Wilckens JH. Lower-extremity peripheral nerve blocks in the perioperative pain management of orthopaedic patients: AAOS exhibit selection. J Bone Joint Surg [Am]. 2012;94-A:1-13. [DOI] [PubMed] [Google Scholar]
- 17. Bischoff P, Rundshagen I. Awareness under general anesthesia. Dtsch Arztebl Int. 2011;108:1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Olawin AM, J MD. Spinal Anesthesia. StatPearls. Treasure Island, Florida: StatPearls Publishing; 2020. [Google Scholar]
- 19. Hogan QH. Lumbar epidural anatomy. A new look by cryomicrotome section. Anesthesiology. 1991;75:767-775. [DOI] [PubMed] [Google Scholar]
- 20. Hogan Q. Distribution of solution in the epidural space: examination by cryomicrotome section. Reg Anesth Pain Med. 2002;27:150-156. [DOI] [PubMed] [Google Scholar]
- 21. Pugely AJ, Martin CT, Gao Y, Mendoza-Lattes S, Callaghan JJ. Differences in short-term complications between spinal and general anesthesia for primary total knee arthroplasty. J Bone Joint Surg [Am]. 2013;95-A:193-199. [DOI] [PubMed] [Google Scholar]
- 22. Mauermann WJ, Shilling AM, Zuo Z. A comparison of neuraxial block versus general anesthesia for elective total hip replacement: a meta-analysis. Anesth Analg. 2006;103:1018-1025. [DOI] [PubMed] [Google Scholar]
- 23. Park YB, Chae WS, Park SH, Yu JS, Lee SG, Yim SJ. Comparison of Short-Term Complications of General and Spinal Anesthesia for Primary Unilateral Total Knee Arthroplasty. Knee Surg Relat Res. 2017;29:96-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Johnson RL, Kopp SL, Burkle CM, et al. Neuraxial vs general anaesthesia for total hip and total knee arthroplasty: a systematic review of comparative-effectiveness research. Br J Anaesth. 2016;116(:163-176. [DOI] [PubMed] [Google Scholar]
- 25. Choi PT, Bhandari M, Scott J, Douketis J. Epidural analgesia for pain relief following hip or knee replacement. Cochrane Database Syst Rev. 2003;3:CD003071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Memtsoudis SG, Cozowicz C, Bekeris J, et al. Anaesthetic care of patients undergoing primary hip and knee arthroplasty: consensus recommendations from the International Consensus on Anaesthesia-Related Outcomes after Surgery group (ICAROS) based on a systematic review and meta-analysis. Br J Anaesth. 2019;123:269-287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kehlet H. Postoperative pain, analgesia, and recovery—bedfellows that cannot be ignored. 2018;159:S11-S16. [DOI] [PubMed] [Google Scholar]
- 28. Chitnis SS, Tang R, Mariano ER. The role of regional analgesia in personalized postoperative pain management. Korean J Anesthesiol. 2020;73:363-371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Maurer K, Bonvini JM, Ekatodramis G, Serena S, Borgeat A. Continuous spinal anesthesia/analgesia vs. single-shot spinal anesthesia with patient-controlled analgesia for elective hip arthroplasty. Acta Anaesthesiol Scand. 2003;47:878-883. [DOI] [PubMed] [Google Scholar]
- 30. Saltzman BM, Dave A, Young A, Ahuja M, Amin SD, Bush-Joseph CA. Prolonged Epidural Infusion Improves Functional Outcomes Following Knee Arthroscopy in Patients with Arthrofibrosis after Total Knee Arthroplasty: A Retrospective Evaluation. J Knee Surg. 2016;29:40-46. [DOI] [PubMed] [Google Scholar]
- 31. Gerrard AD, Brooks B, Asaad P, Hajibandeh S, Hajibandeh S. Meta-analysis of epidural analgesia versus peripheral nerve blockade after total knee joint replacement. Eur J Orthop Surg Traumatol. 2017;27:61-72. [DOI] [PubMed] [Google Scholar]
- 32. McCarthy D, McNamara J, Galbraith J, Loughnane F, Shorten G, Iohom G. A comparison of the analgesic efficacy of local infiltration analgesia vs. intrathecal morphine after total knee replacement: A randomised controlled trial. Eur J Anaesthesiol. 2019;36:264-271. [DOI] [PubMed] [Google Scholar]
- 33. Liu X, Zhang H, Zhang H, Guo M, Gao Y, Du C. Local infiltration vs epidural analgesia for postoperative pain control after total knee or hip arthroplasty: A meta-analysis of randomized controlled trials. Medicine (Baltimore). 2020;99:e22674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Block BM, Liu SS, Rowlingson AJ, Cowan AR, Cowan JA, Jr, Wu CL. Efficacy of postoperative epidural analgesia: a meta-analysis. JAMA. 2003;290:2455-2463. [DOI] [PubMed] [Google Scholar]
- 35. Mahoney OM, Noble PC, Davidson J, Tullos HS. The effect of continuous epidural analgesia on postoperative pain, rehabilitation, and duration of hospitalization in total knee arthroplasty. Clin Orthop Relat Res. 1990;260:30-37. [PubMed] [Google Scholar]
- 36. Winnie AP, Ramamurthy S, Durrani Z. The inguinal paravascular technic of lumbar plexus anesthesia: the “3-in-1 block”. Anesth Analg. 1973;52:989-996. [PubMed] [Google Scholar]
- 37. Rosenblatt RM. Continuous femoral anesthesia for lower extremity surgery. Anesth Analg. 1980;59:631-632. [PubMed] [Google Scholar]
- 38. Marhofer P, Oismüller C, Faryniak B, Sitzwohl C, Mayer N, Kapral S. Three-in-one blocks with ropivacaine: evaluation of sensory onset time and quality of sensory block. Anesth Analg. 2000;90:125-128. [DOI] [PubMed] [Google Scholar]
- 39. de Lima E, Souza R, Correa CH, Henriques MD, de Oliveira CB, Nunes TA, Gomez RS. Single-injection femoral nerve block with 0.25% ropivacaine or 0.25% bupivacaine for postoperative analgesia after total knee replacement or anterior cruciate ligament reconstruction. J Clin Anesth. 2008;20:521-527. [DOI] [PubMed] [Google Scholar]
- 40. Ozen M, Inan N, Tümer F, Uyar A, Baltaci B. The effect of 3-in-1 femoral nerve block with ropivacaine 0.375% on postoperative morphine consumption in elderly patients after total knee replacement surgery. Agri. 2006;18:44-50. [PubMed] [Google Scholar]
- 41. Singelyn FJ, Deyaert M, Joris D, Pendeville E, Gouverneur JM. Effects of intravenous patient-controlled analgesia with morphine, continuous epidural analgesia, and continuous three-in-one block on postoperative pain and knee rehabilitation after unilateral total knee arthroplasty. Anesth Analg. 1998;87:88-92. [DOI] [PubMed] [Google Scholar]
- 42. Marhofer P, Nasel C, Sitzwohl C, Kapral S. Magnetic resonance imaging of the distribution of local anesthetic during the three-in-one block. Anesth Analg. 2000;90:119-124. [DOI] [PubMed] [Google Scholar]
- 43. Capdevila X, Biboulet P, Bouregba M, Barthelet Y, Rubenovitch J, d’Athis F. Comparison of the three-in-one and fascia iliaca compartment blocks in adults: clinical and radiographic analysis. Anesth Analg. 1998;86:1039-1044. [DOI] [PubMed] [Google Scholar]
- 44. Lang SA, Yip RW, Chang PC, Gerard MA. The femoral 3-in-1 block revisited. J Clin Anesth. 1993;5:292-296. [DOI] [PubMed] [Google Scholar]
- 45. Capdevila X, Biboulet P, Morau D, et al. Continuous three-in-one block for postoperative pain after lower limb orthopedic surgery: where do the catheters go? Anesth Analg. 2002;94:1001-1006. [DOI] [PubMed] [Google Scholar]
- 46. Wanderer JP, Rathmell JP. A brief history of femoral nerve blocks. Anesthesiology. 2014;121:A21. [DOI] [PubMed] [Google Scholar]
- 47. Reid N, Stella J, Ryan M, Ragg M. Use of ultrasound to facilitate accurate femoral nerve block in the emergency department. Emerg Med Australas. 2009;21:124-130. [DOI] [PubMed] [Google Scholar]
- 48. Ma HH, Chou TA, Tsai SW, Chen CF, Wu PK, Chen WM. The efficacy of continuous versus single-injection femoral nerve block in Total knee Arthroplasty: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2020;21:121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Li S, Zhou J, Li X, et al. Analgesic Impact of Single-Shot Versus Continuous Femoral Nerve Block After Total Knee Arthroplasty: A Systematic Review and Meta-Analysis. Adv Ther. 2020;37:671-685. [DOI] [PubMed] [Google Scholar]
- 50. Dixit V, Fathima S, Walsh SM, et al. Effectiveness of continuous versus single injection femoral nerve block for total knee arthroplasty: A double blinded, randomized trial. Knee. 2018;25:623-630. [DOI] [PubMed] [Google Scholar]
- 51. Ma T, Liu Q, Zhou L, Yue K, Ding Z, Chen B. Continuous nerve block versus single-shot nerve block for total knee arthroplasty: a meta-analysis from randomized controlled trials. Minerva Anestesiol. 2020;86:205-216. [DOI] [PubMed] [Google Scholar]
- 52. Zhang J, Yuan Y, Zhang Y, Wang Y. Clinical effects of single femoral nerve block in combination with general anesthesia on geriatric patients receiving total knee arthroplasty. Pak J Med Sci. 2018;34:43-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Khan AA, Khan RI. Urinary Retention in Unilateral Total Knee Arthroplasty: Comparison between Continuous Epidural Analgesia and Single-Shot Femoral Nerve Block. J Coll Physicians Surg Pak. 2018;28:5-8. [DOI] [PubMed] [Google Scholar]
- 54. Thacher RR, Hickernell TR, Grosso MJ, et al. Decreased risk of knee buckling with adductor canal block versus femoral nerve block in total knee arthroplasty: a retrospective cohort study. Arthroplast Today. 2017;3:281-285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Kuang MJ, Xu LY, Ma JX, Wang Y, Zhao J, Lu B, Ma XL. Adductor canal block versus continuous femoral nerve block in primary total knee arthroplasty: A meta-analysis. Int J Surg. 2016;31:17-24. [DOI] [PubMed] [Google Scholar]
- 56. Wang D, Yang Y, Li Q, et al. Adductor canal block versus femoral nerve block for total knee arthroplasty: a meta-analysis of randomized controlled trials. Sci Rep. 2017;7:40721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Gao F, Ma J, Sun W, Guo W, Li Z, Wang W. Adductor Canal Block Versus Femoral Nerve Block for Analgesia After Total Knee Arthroplasty: A Systematic Review and Meta-analysis. Clin J Pain. 2017;33:356-368. [DOI] [PubMed] [Google Scholar]
- 58. Ng YM, Martin F, Waterson HB, et al. A Randomised Controlled Trial of Local Infiltration Analgesia Versus Femoral Nerve Block for Postoperative Analgesia Following Total Knee Arthroplasty. Cureus. 2020;12:e10192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Grape S, Kirkham KR, Baeriswyl M, Albrecht E. The analgesic efficacy of sciatic nerve block in addition to femoral nerve block in patients undergoing total knee arthroplasty: a systematic review and meta-analysis. Anaesthesia. 2016;71:1198-1209. [DOI] [PubMed] [Google Scholar]
- 60. Hakkalamani S, Carroll AF, Ford C, Parkinson RW. Femoral versus combined femoral and sciatic nerve block in total knee replacement: a prospective comparative study. Orthopaedic Proceedings. 2018;91-B [Google Scholar]
- 61. Babazade R, Sreenivasalu T, Jain P, et al. A nomogram for predicting the need for sciatic nerve block after total knee arthroplasty. J Anesth. 2016;30:864-872. [DOI] [PubMed] [Google Scholar]
- 62. Zhang Z, Yang Q, Xin W, Zhang Y. Comparison of local infiltration analgesia and sciatic nerve block as an adjunct to femoral nerve block for pain control after total knee arthroplasty: A systematic review and meta-analysis. Medicine (Baltimore). 2017;96:e6829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Nagafuchi M, Sato T, Sakuma T, et al. Femoral nerve block-sciatic nerve block vs. femoral nerve block-local infiltration analgesia for total knee arthroplasty: a randomized controlled trial. BMC Anesthesiol. 2015;15:182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Tian Y, Tang S, Sun S, et al. Comparison between local infiltration analgesia with combined femoral and sciatic nerve block for pain management after total knee arthroplasty. J Orthop Surg Res. 2020;15:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Seo JH, Seo SS, Kim DH, Park BY, Park CH, Kim OG. Does Combination Therapy of Popliteal Sciatic Nerve Block and Adductor Canal Block Effectively Control Early Postoperative Pain after Total Knee Arthroplasty? Knee Surg Relat Res. 2017;29(4):276-281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. van der Wal M, Lang SA, Yip RW. Trans-sartorial approach for saphenous nerve block. Journal canadien d'anesthesie. 1993;40:542-546. [DOI] [PubMed] [Google Scholar]
- 67. Wong WY, Bjørn S, Strid JM, Børglum J, Bendtsen TF. Defining the Location of the Adductor Canal Using Ultrasound. Reg Anesth Pain Med. 2017;42:241-245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Leng JC, Harrison TK, Miller B, et al. A pilot study to assess adductor canal catheter tip migration in a cadaver model. J Anesth. 2015;29:308-312. [DOI] [PubMed] [Google Scholar]
- 69. Tan Z, Kang P, Pei F, Shen B, Zhou Z, Yang J. A comparison of adductor canal block and femoral nerve block after total-knee arthroplasty regarding analgesic effect, effectiveness of early rehabilitation, and lateral knee pain relief in the early stage. Medicine (Baltimore). 2018;97:e13391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Kuang MJ, Ma JX, Fu L, He WW, Zhao J, Ma XL. Is Adductor Canal Block Better Than Femoral Nerve Block in Primary Total Knee Arthroplasty? A GRADE Analysis of the Evidence Through a Systematic Review and Meta-Analysis. J Arthroplasty. 2017;32:3238-3248.e3. [DOI] [PubMed] [Google Scholar]
- 71. Jæger P, Zaric D, Fomsgaard JS, et al. Adductor canal block versus femoral nerve block for analgesia after total knee arthroplasty: a randomized, double-blind study. Reg Anesth Pain Med. 2013;38:526-532. [DOI] [PubMed] [Google Scholar]
- 72. Zhang LK, Zhang BY, Quan RF, Xu H, Sun YJ, Zhou JH. Single shot versus continuous technique adductor canal block for analgesia following total knee arthroplasty: A PRISMA-compliant meta-analysis. Medicine (Baltimore). 2019;98:e15539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Li C, Xu H, Shen B, et al. [Effect of continuous and single shot adductor canal blocks for postoperative analgesia and early rehabilitation after total knee arthroplasty]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2017;31:1049-1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Kayupov E, Okroj K, Young AC, et al. Continuous Adductor Canal Blocks Provide Superior Ambulation and Pain Control Compared to Epidural Analgesia for Primary Knee Arthroplasty: A Randomized, Controlled Trial. J Arthroplasty. 2018;33:1040-1044.e1. [DOI] [PubMed] [Google Scholar]
- 75. Leung P, Dickerson DM, Denduluri SK, et al. Postoperative continuous adductor canal block for total knee arthroplasty improves pain and functional recovery: A randomized controlled clinical trial. J Clin Anesth. 2018;49:46-52. [DOI] [PubMed] [Google Scholar]
- 76. Canbek U, Akgun U, Aydogan NH, Kilinc CY, Uysal AI. Continuous adductor canal block following total knee arthroplasty provides a better analgesia compared to single shot: A prospective randomized controlled trial. Acta Orthop Traumatol Turc. 2019;53:334-339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Turner JD, Dobson SW, Henshaw DS, et al. Single-Injection Adductor Canal Block With Multiple Adjuvants Provides Equivalent Analgesia When Compared With Continuous Adductor Canal Blockade for Primary Total Knee Arthroplasty: A Double-Blinded, Randomized, Controlled, Equivalency Trial. J Arthroplasty. 2018;33:3160-3166.e1. [DOI] [PubMed] [Google Scholar]
- 78. Tong QJ, Lim YC, Tham HM. Comparing adductor canal block with local infiltration analgesia in total knee arthroplasty: A prospective, blinded and randomized clinical trial. J Clin Anesth. 2018;46:39-43. [DOI] [PubMed] [Google Scholar]
- 79. Zhang LK, Li Q, Zhu FB, et al. Comparison of adductor canal block with periarticular infiltration analgesia in total knee arthroplasty: A meta-analysis of randomized controlled trials. Medicine (Baltimore). 2019;98:e18356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Chen J, Zhou C, Ma C, et al. Which is the best analgesia treatment for total knee arthroplasty: adductor canal block, periarticular infiltration, or liposomal bupivacaine? A network meta-analysis. J Clin Anesth. 2021;68:110098. [DOI] [PubMed] [Google Scholar]
- 81. Vlessides M. New Regional Technique Controls Post-TKA Pain. Anesthesiology News. 2012; Dec; 38:17. https://issuu.com/mcmahongroup/docs/mman0012_2012_tab
- 82. Yamak Altinpulluk E, Turan A. Future in regional anesthesia: new techniques and technological advancements. Minerva Anestesiol. 2021;87:85-100. [DOI] [PubMed] [Google Scholar]
- 83. Clint E, Elliott ST. The adductor canal catheter and interspace between the popliteal artery and the posterior capsule of the knee for total knee arthroplasty. Tech Reg Anesth Pain Manage. 2014;18:126-129. [Google Scholar]
- 84. Cong Z, Zhang L, Ma F. The efficacy and safety of the infiltration of the interspace between the popliteal artery and the capsule of the knee block in total knee arthroplasty: A prospective randomized trial protocol. Medicine (Baltimore). 2020;99:e21670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. VanderWielen BA, Fitzsimmons AJ, Kovacs AJ, Topolski MS. Community hospital implementation of the IPACK block reduces opioid use and length of stay after total knee arthroplasty. J Clin Anesth. 2020;65:109857. [DOI] [PubMed] [Google Scholar]
- 86. Eccles CJ, Swiergosz AM, Smith AF, Bhimani SJ, Smith LS, Malkani AL. Decreased Opioid Consumption and Length of Stay Using an IPACK and Adductor Canal Nerve Block following Total Knee Arthroplasty. J Knee Surg. 2021;34:705-711. [DOI] [PubMed] [Google Scholar]
- 87. El-Emam EM, El Motlb EAA. Ultrasound-Guided Adductor Canal Block versus Combined Adductor Canal and Infiltration between the Popliteal Artery and the Posterior Capsule of the Knee Block for Osteoarthritis Knee Pain. Anesth Essays Res. 2020;14:127-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Jung DW, Shon WY, Seo SS, Kim OG, Lee IS. Comparison of the postoperative analgesic effect for infiltration between the popliteal artery and the capsule of the posterior knee and that of periarticular multimodal drug injection in total knee arthroplasty: retrospective study in the immediate postoperative period. Knee Surg Relat Res. 2020;32:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Biehl M, Wild L, Waldman K, Haq F, Easteal RA, Sawhney M. The safety and efficacy of the IPACK block in primary total knee arthroplasty: a retrospective chart review. Journal Canadien d'Anesthesie. 2020;67:1271-1273. [DOI] [PubMed] [Google Scholar]
- 90. Sebastian MP, Bykar H, Sell A. Saphenous nerve and IPACK block. Reg Anesth Pain Med. 2019;rapm-2019-100750. [DOI] [PubMed] [Google Scholar]
- 91. Kehlet H, Andersen LØ. Local infiltration analgesia in joint replacement: the evidence and recommendations for clinical practice. Acta Anaesthesiol Scand. 2011;55:778-784. [DOI] [PubMed] [Google Scholar]
- 92. Ramamoorthy KG. Local infiltration analgesia following total knee arthroplasty. Indian J Anaesth. 2012;56:208-209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Meier M, Sommer S, Huth J, Benignus C, Thienpont E, Beckmann J. Local infiltration analgesia with additional intraarticular catheter provide better pain relief compared to single-shot local infiltration analgesia in TKA. Arch Orthop Trauma Surg. 2021;141:105-111. [DOI] [PubMed] [Google Scholar]
- 94. Andersen LØ, Husted H, Otte KS, Kristensen BB, Kehlet H. A compression bandage improves local infiltration analgesia in total knee arthroplasty. Acta Orthop. 2008;79:806-811. [DOI] [PubMed] [Google Scholar]
- 95. Li C, Qu J, Pan S, Qu Y. Local infiltration anesthesia versus epidural analgesia for postoperative pain control in total knee arthroplasty: a systematic review and meta-analysis. J Orthop Surg Res. 2018;13:112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Zhang LK, Ma JX, Kuang MJ, Ma XL. Comparison of periarticular local infiltration analgesia with femoral nerve block for total knee arthroplasty: a meta-analysis of randomized controlled trials. J Arthroplasty. 2018;33:1972-1978.e1974. [DOI] [PubMed] [Google Scholar]
- 97. Toftdahl K, Nikolajsen L, Haraldsted V, Madsen F, Tønnesen EK, Søballe K. Comparison of peri- and intraarticular analgesia with femoral nerve block after total knee arthroplasty: a randomized clinical trial. Acta Orthop. 2007;78:172-179. [DOI] [PubMed] [Google Scholar]
- 98. Xing Q, Dai W, Zhao D, Wu J, Huang C, Zhao Y. Adductor canal block with local infiltrative analgesia compared with local infiltrate analgesia for pain control after total knee arthroplasty: A meta-analysis of randomized controlled trials. Medicine (Baltimore). 2017;96:e8103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Ma J, Gao F, Sun W, Guo W, Li Z, Wang W. Combined adductor canal block with periarticular infiltration versus periarticular infiltration for analgesia after total knee arthroplasty. Medicine (Baltimore). 2016;95:e5701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Kakar P, Gagrani V, Deshmukh U, Popli G. Post-operative analgesia regime following joint replacement. Indian J Anaesth. 2011;55:305-306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Sweet WH, Mark VH, Hamlin H. Radiofrequency lesions in the central nervous system of man and cat: including case reports of eight bulbar pain-tract interruptions. J Neurosurg. 1960;17:213-225. [DOI] [PubMed] [Google Scholar]
- 102. Shealy CN. Percutaneous radiofrequency denervation of spinal facets. Treatment for chronic back pain and sciatica. J Neurosurg. 1975;43:448-451. [DOI] [PubMed] [Google Scholar]
- 103. Billesberger LM, Fisher KM, Qadri YJ, Boortz-Marx RL. Procedural Treatments for Knee Osteoarthritis: A Review of Current Injectable Therapies. Pain Res Manag. 2020;2020:3873098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Sylvester LN, Goree JH. Genicular Radiofrequency Ablation for Treatment of Post Total Knee Arthroplasty Posterior Thigh Pain: A Case Report. A A Case Rep. 2017;9:292-293. [DOI] [PubMed] [Google Scholar]
- 105. Protzman NM, Gyi J, Malhotra AD, Kooch JE. Examining the feasibility of radiofrequency treatment for chronic knee pain after total knee arthroplasty. PM R. 2014;6:373-376. [DOI] [PubMed] [Google Scholar]
- 106. González Sotelo V, Maculé F, Minguell J, Bergé R, Franco C, Sala-Blanch X. Ultrasound-guided genicular nerve block for pain control after total knee replacement: preliminary case series and technical note. Rev Esp Anestesiol Reanim. 2017;64:568-576. [DOI] [PubMed] [Google Scholar]
- 107. Qudsi-Sinclair S, Borrás-Rubio E, Abellan-Guillén JF, Padilla Del Rey ML, Ruiz-Merino G. A comparison of genicular nerve treatment using either radiofrequency or analgesic block with corticosteroid for pain after a total knee arthroplasty: a double-blind, randomized clinical study. Pain Pract. 2017;17:578-588. [DOI] [PubMed] [Google Scholar]
- 108. Agarwala S, Butani M, D’Mello J, Saksena S, Menon A. Decreasing hospital length of stay and enhancing recovery in Total Knee Arthroplasty. J Clin Orthop Trauma. 2020;11:122-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Becker DE, Reed KL. Local anesthetics: review of pharmacological considerations. Anesth Prog. 2012;59:90-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Gadsden J. Local Anesthetics: Clinical Pharmacology and Rational Selection. In: Hadzic A, ed. Hadzic’s Peripheral Nerve Blocks and Anatomy for Ultrasound-Guided Regional Anesthesia, 2e. New York, NY: The McGraw-Hill Companies; 2012:Chap 2. [Google Scholar]
- 111. Foster RH, Markham A. Levobupivacaine: a review of its pharmacology and use as a local anaesthetic. Drugs. 2000;59:551-579. [DOI] [PubMed] [Google Scholar]
- 112. Coppens SJR, Zawodny Z, Dewinter G, Neyrinck A, Balocco AL, Rex S. In search of the Holy Grail: poisons and extended release local anesthetics. Best Pract Res Clin Anaesthesiol. 2019;33:3-21. [DOI] [PubMed] [Google Scholar]
- 113. Ilfeld BM, Eisenach JC, Gabriel RA. Clinical Effectiveness of Liposomal Bupivacaine Administered by Infiltration or Peripheral Nerve Block to Treat Postoperative Pain. Anesthesiology. 2021;134:283-344. [DOI] [PubMed] [Google Scholar]
- 114. Yu ZX, Yang ZZ, Yao LL. Effectiveness of liposome bupivacaine for postoperative pain control in total knee arthroplasty: A PRISMA-compliant meta-analysis of randomized controlled trials. Medicine (Baltimore). 2018;97:e0171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Liu Y, Zeng JF, Zeng Y, Wu YG, Bao XC, Shen B. Comprehensive Comparison of Liposomal Bupivacaine with Femoral Nerve Block for Pain Control Following Total Knee Arthroplasty: An Updated Systematic Review and Meta-Analysis. Orthop Surg. 2019;11:943-953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Yayac M, Li WT, Ong AC, Courtney PM, Saxena A. The Efficacy of Liposomal Bupivacaine Over Traditional Local Anesthetics in Periarticular Infiltration and Regional Anesthesia During Total Knee Arthroplasty: A Systematic Review and Meta-Analysis. J Arthroplasty. 2019;34:2166-2183. [DOI] [PubMed] [Google Scholar]
- 117. Chen CM, Yun AG, Fan T. Efficacy of Liposomal Bupivacaine versus Ropivacaine in Adductor Canal Block for Total Knee Arthroplasty. J Knee Surg. 2020. doi: 10.1055/s-0040-1713114 [E-pub ahead of print] [DOI] [PubMed] [Google Scholar]
- 118. Ottoboni T, Quart B, Pawasauskas J, Dasta JF, Pollak RA, Viscusi ER. Mechanism of action of HTX-011: a novel, extended-release, dual-acting local anesthetic formulation for postoperative pain. Reg Anesth Pain Med. 2019;rapm-2019-100714. [DOI] [PubMed] [Google Scholar]
- 119. Lachiewicz PF, Lee GC, Pollak RA, Leiman DG, Hu J, Sah AP. HTX-011 Reduced Pain and Opioid Use After Primary Total Knee Arthroplasty: Results of a Randomized Phase 2b Trial. J Arthroplasty. 2020;35:2843-2851. [DOI] [PubMed] [Google Scholar]
- 120. Trescot AM. Cryoanalgesia in interventional pain management. Pain Physician. 2003;6:345-360. [PubMed] [Google Scholar]
- 121. Ilfeld BM, Gabriel RA, Trescot AM. Ultrasound-guided percutaneous cryoneurolysis providing postoperative analgesia lasting many weeks following a single administration: a replacement for continuous peripheral nerve blocks?: a case report. Korean J Anesthesiol. 2017;70:567-570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Dasa V, Lensing G, Parsons M, Harris J, Volaufova J, Bliss R. Percutaneous freezing of sensory nerves prior to total knee arthroplasty. Knee. 2016;23:523-528. [DOI] [PubMed] [Google Scholar]


