Abstract
Tarsal tunnel syndrome (TTS) is a neuropathy due to compression of the posterior tibial nerve and its branches.
It is usually underdiagnosed and its aetiology is very diverse. In 20% of cases it is idiopathic.
There is no test that diagnoses it with certainty. The diagnosis is usually made by correlating clinical history, imaging tests, nerve conduction studies (NCSs) and electromyography (EMG).
A differential diagnosis should be made with plantar fasciitis, lumbosacral radiculopathy (especially S1 radiculopathy), rheumatologic diseases, metatarsal stress fractures and Morton’s neuroma.
Conservative management usually gives good results. It includes activity modification, administration of pain relief drugs, physical and rehabilitation medicine, and corticosteroid injections into the tarsal tunnel (to reduce oedema).
Abnormally slow nerve conduction through the posterior tibial nerve usually predicts failure of conservative treatment.
Indications for surgical treatment are failure of conservative treatment and clear identification of the cause of the entrapment. In these circumstances, the results are usually satisfactory. Surgical success rates vary from 44% to 96%.
Surgical treatment involves releasing the flexor retinaculum from its proximal attachment near the medial malleolus down to the sustentaculum tali. Ultrasound-guided tarsal tunnel release is possible.
A positive Tinel’s sign before surgery is a strong predictor of surgical relief after decompression.
Surgical treatment achieves the best results in young patients, those with a clear aetiology, a positive Tinel’s sign prior to surgery, a short history of symptoms, an early diagnosis and no previous ankle pathology.
Cite this article: EFORT Open Rev 2021;6:1140-1147. DOI: 10.1302/2058-5241.6.210031
Keywords: diagnosis, tarsal tunnel syndrome, treatment
Introduction
Tarsal tunnel syndrome (TTS), first defined in 1962 by Keck1 and Lam2, is a compressive peripheral neuropathy of the posterior tibial nerve and its branches within the tarsal tunnel beneath the flexor retinaculum.3,4 The prevalence of TTS is low relative to other compressive neuropathies, although it is often underdiagnosed and even misdiagnosed as plantar fasciitis.1,4,5
According to Schon, nerve entrapment, neuropathy, and nerve dysfunction in the legs, ankles, and feet of athletes are not unusual problems.6 Often, the aforementioned problems are neglected as the more noticeable musculoskeletal lesion draws the orthopaedic surgeon’s attention. Commonly, with conservative management, including a sporadic injection of local anaesthetic with and without corticosteroid, resolution is attained. Hardly ever, symptoms are severe and diffuse enough to need administration of a tricyclic antidepressant medication to diminish the nerve irritability. In cases that fail to respond to conservative management and have well-localized neurologic findings, surgery might be indicated. During the surgical procedure, the nerve should be minimally manipulated. The surrounding veins, arteries, and fat must be relatively undisturbed. Crucial to comprehending and managing these conditions is a thorough knowledge of the peripheral neuroanatomy.6
The optimal treatment of TTS is still a controversial issue. The controversy is mainly due to its diagnostic difficulties.7–9 The purpose of this article is to review current knowledge on TTS and its treatment options.
Relevant anatomy of the tarsal tunnel
The flexor retinaculum joins the medial malleolus with the calcaneus to form the roof of the tarsal tunnel, which is an osteofibrous tunnel. Forming part of the wall and floor of this tunnel, covered by their own sheaths, are the tendons of the tibialis posterior, flexor digitorum longus and flexor hallucis longus. The tarsal tunnel is occupied by the posterior tibial artery and veins and the posterior tibial nerve. The posterior tibial nerve, after exiting the peroneal nerve above the popliteal fossa, runs down the back of the leg until it reaches the posteromedial aspect of the ankle. To reach the foot it passes through the tarsal tunnel and can be compressed at that level. The floor of the tarsal tunnel is formed by the talus, the calcaneum and the medial wall of the distal tibia. The flexor retinaculum forms the roof. The tibial nerve branches into the medial plantar and lateral plantar nerves, usually within the tarsal tunnel (Fig. 1).
Fig. 1.
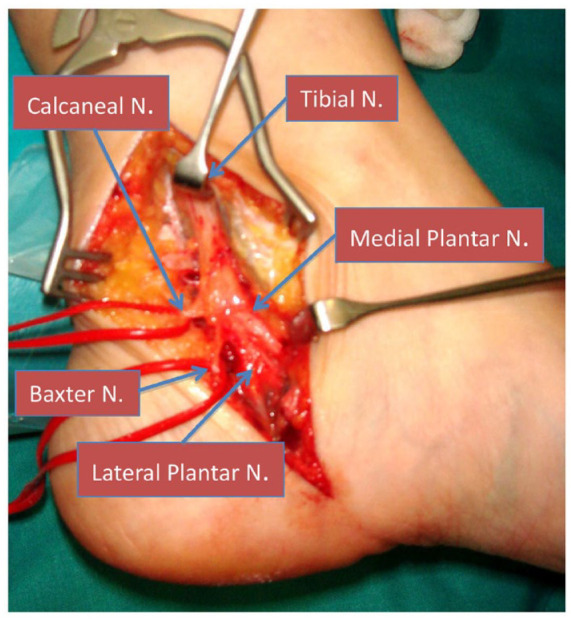
The anatomy of the posterior tibial nerve is variable. In this patient we can see the nerve and its main branches: medial plantar nerve, lateral plantar nerve, calcaneal nerve and the first branch of the lateral plantar nerve known as Baxter’s nerve.
The lateral branch (lateral plantar nerve) generates a first branch known as the Baxter nerve10 that innervates the abductor digiti minimi and then passes through the abductor hallucis longus to the lateral surface of the foot. This nerve provides sensory innervation to the medial region of the calcaneus and lateral heel area, and motor function to the flexor digitorum brevis and quadratus plantae.11 Compression of the Baxter nerve can be the cause of talalgia, which is associated or not with plantar fasciitis. The nerve is usually compressed between the deep fascia of the abductor hallucis muscle and the inferomedial region of the quadratus plantae muscle.
These nerves provide sensation to the sole of the foot and control the intrinsic muscles of the foot. Exiting from the posterior tibial nerve is the medial calcaneal nerve, which passes through the flexor retinaculum to provide sensory innervation to the heel. Although there can be anatomical variations, in 25% of cases, the medial calcaneal nerve branches from the lateral plantar nerve.12–15 Generally the sensory disturbance in TTS affects the heel area because the calcaneal branches form before entering the tarsal tunnel.16
Singh and Kumar described a dorsal extension of the medial border of the plantar fascia (the deep fascia of the abductor hallucis muscle) as well as the medial septum.17 Heimkes et al dissected 60 feet, and observed that in almost all feet this medial septum was located between the medial and lateral plantar nerves, was attached to the deep fascia of the abductor hallucis muscle, and originated from the calcaneus or from the sheath of the flexor hallucis longus (Fig. 2).18 That is, in most cases the medial plantar nerve, lateral plantar nerve, Baxter nerve, and calcaneal branches run through different channels that are divided by osteofibrous structures. This structure explains why there can be isolated compression of each nerve branch in its corresponding osteofibrous tube.
Fig. 2.
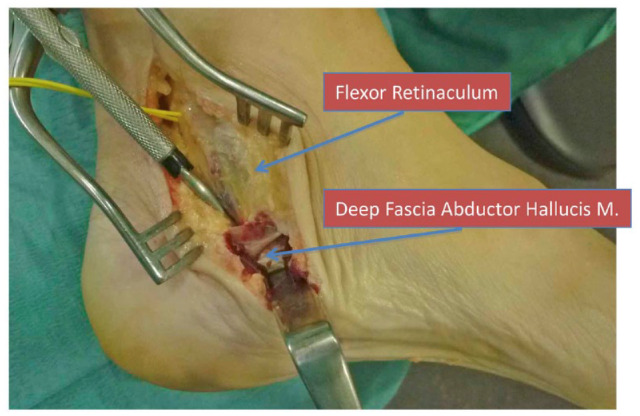
Deep fascia of the abductor hallucis muscle. It must be sectioned because it is also a frequent cause of isolated compression of some of the terminal branches of the tibial nerve.
Aetiology
Compression of the posterior tibial nerve and its branches can be extrinsic, as for example in sequelae of ankle fractures and sprains, foot deformities (flat foot, varus or valgus deformity of the foot), overweight and systemic diseases (rheumatoid arthritis, osteoarthritis, hyperlipidaemia, or diabetes) or intrinsic due to space-reducing lesions in the tarsal tunnel (perineural fibrosis, extraneural ganglion cysts, tophaceous tendinitis in the flexor hallucis longus-FHL tendon, osteophytes, hypertrophy of the flexor retinaculum, calcaneal osteochondroma, lipomas or other tumours, tendons or accessory muscles, and vascular anomalies).19–22 TTS has also been described in cases of tarsal coalition (posterior facet talocalcaneal coalition), medial plantar avulsion fractures of the calcaneus, and even in patients with tight footwear. It has been published that TTS is more frequent in avid runners, especially when hyperpronation of the foot occurs.23–32 Trauma and related bleeding or posterior adhesions can also cause TTS.13,30,33 However, in 20% of cases the aetiology of TTS is unclear, i.e. idiopathic.23–26,34 Table 1 summarizes the main causes of TTS.
Table 1.
Causes of tarsal tunnel syndrome (TTS)
| Extrinsic causes | Intrinsic causes |
|---|---|
| Poorly fitted shoes | Tendinopathy – tenosynovitis |
| Trauma | Perineural fibrosis |
| Anatomical/biomechanical alterations - Tarsal coalition - Varus/valgus hindfoot |
Osteophytes |
| Postsurgical scar | Retinaculum hypertrophy |
| Systemic diseases or inflammatory arthropathies | Space occupying lesions or mass effect - varicose veins - ganglion cyst - lipoma - neoplasia - neuroma |
| Generalized oedema of lower limbs | Arterial insufficiency (nervous ischemia) |
| Diabetes mellitus |
Clinical presentation
Patients with TTS complain of pain in the medial aspect of the ankle, with irradiation to the plantar aspect of the foot. Dysesthesia, paraesthesia, numbness, tingling and burning pain in the sole of the foot are common.3,13,27 Symptoms usually worsen with weight-bearing activities (prolonged standing or walking) and are relieved when the foot is placed in an elevated position.13,14
In the physical examination, it is rare to find neurological deficits. In addition, motor weakness of the intrinsic foot muscles is rare and difficult to assess.22,35 Mild sensory loss can sometimes be detected, although its precise assessment is difficult because of calluses on the sole of the foot.13 Deep palpation of the medial aspect of the ankle can cause pain.27,36 In addition, Tinel’s sign is usually present.20,22,35
There are other manoeuvres that can aid in the diagnosis. The dorsiflexion-eversion test is performed by maximal passive dorsiflexion and eversion of the foot while dorsiflexing the metatarsophalangeal joints.20,27 In an analysis of 44 feet diagnosed with TTS using electrodiagnostic testing, dorsiflexion-eversion manoeuvring reproduced or aggravated symptoms in 82% of cases, without causing symptoms in normal volunteers.13 It has also been reported that passive plantarflexion and inversion increase the intracompartmental pressure of the tarsal tunnel.35 Finally, continuous pressure on the posterior tibial nerve can produce tingling and numbness, the so-called Valleix phenomenon, which is positive in approximately one-third of cases.20,27 However, the specificity of the aforementioned manoeuvres is low.
Diagnosis
There is currently no test that can reliably diagnose TTS. The diagnosis is usually made by correlating clinical history, imaging tests and nerve conduction studies (NCSs) / electromyography (EMG).4,2,37,38
Nerve conduction studies (NCSs) / electromyography (EMG)
NCSs/EMG can be useful for diagnosing TTS, given it can provide objective evidence of nerve compression in the tarsal tunnel or identify an alternative neurological cause (radiculopathy). However, the sensitivity and specificity of NCSs/EMG findings for TTS remain low.13 The finding most suggestive of TTS is the slowing of nerve conduction velocity through the tarsal tunnel.39 Plantar nerve NCSs require that their findings be compared with the asymptomatic healthy side. The diagnosis of TTS should not be based solely on alterations detected in the intrinsic foot muscles on EMG, given such alterations can also be observed in asymptomatic individuals.40 The sensitivity of NCSs of the medial and lateral plantar nerves for the diagnosis of TTS is not sufficiently high. The near nerve method (NNM) is a technique that allows recording large and clear potentials. In medial and lateral plantar nerve NCSs with NNM to diagnose TTS, ultrasound-assisted NNM can be useful because of its simplicity and safety. EMG and nerve conduction studies often produce false negatives.41–43 EMG is unreliable for confirming the compression of the tibial nerve and its branches.41
Imaging
Diagnostic imaging is often useful. Both ultrasound and magnetic resonance imaging (MRI) can be used, although their sensitivity has not been directly compared.31,44–47 In a study using MRI, a relevant pathology in the tarsal tunnel was identified in 88% of symptomatic cases.47 MRI could be of diagnostic value in identifying signs compatible with plantar muscular atrophy. In addition, MRI might reveal space-occupying lesions, such as tumours, cysts or varicosities.4
Measuring pressure in the tarsal tunnel
Measurement of the pressure in the tarsal tunnel below the flexor retinaculum and medial and lateral plantar tunnels, under the abductor hallucis, could make a reliable diagnosis of TTS.4 In living patients, Kumar et al 43 measured the pressure in the tarsal tunnel compartment in the neutral position and with plantar and dorsal flexion of the ankle using a water manometer. The values obtained were 4 to 7 mm Hg, 10 to 15 mm Hg and 15 to 20 mm Hg, respectively.
Trepman et al measured tarsal tunnel pressures in cadavers, performing measurements in neutral, supination and pronation positions in the ankle and foot.36 The highest measurement was in pronation, with a mean value of 32 ± 5 mm Hg (2–60 mm Hg). Rosson et al carried out measurements on cadavers in the tarsal tunnel and medial plantar and lateral plantar tunnels for various positions of the ankle and knee, obtaining the highest values with pronation. The values obtained were 1 to 33 mm Hg for the tarsal tunnel, 5 to 50 mm Hg for the medial plantar tunnel and 0 to 56 mm Hg for the lateral plantar tunnel.48 This study showed that not only the tarsal tunnel (posterior tibial nerve), but also the lateral plantar and medial plantar tunnels (lateral plantar and medial plantar nerves, respectively) need to be decompressed. The reason is that in the plantar tunnels the pressures are very high, even higher than in the tarsal tunnel 48. Both Rosson et al48 and Trepman et al36 used the same device, manufactured by Stryker (Stryker 295 IntraCompartmental Pressure Monitor System, Quick Pressure Monitor Set, Stryker, Kalamazoo, MI).
Differential diagnosis
When a patient presents with foot pain and paraesthesia, we need to consider entities other than TTS that can present similarly.49 Lumbosacral radiculopathy, especially S1 radiculopathy, can present with patchy sensory symptoms involving the sole of the foot and are commonly unilateral or asymmetric. If the symptoms are bilateral, polyneuropathy should be ruled out. Plantar fasciitis produces pain in the sole of the foot that is usually worse in the morning when the patient takes the first steps out of bed. However, the pain improves during the day. Rheumatologic diseases can themselves produce ankle and foot pain. Although such diseases can increase the risk of TTS, their prevalence alone is higher than that of TTS and, therefore, they are more likely to be the cause of the symptoms. Metatarsal stress fractures can occur from running and other weight-bearing physical activities, although they usually cause localized pain on the dorsum of the foot. Finally, Morton’s neuroma (interdigital neuroma between the third and fourth metatarsals) can also produce pain and paraesthesia, although usually without affecting the entire sole of the foot.49
Treatment of tarsal tunnel syndrome (TTS)
It is essential that the treatment of TTS be directed at the cause of the symptoms.13 However, such treatment remains a challenge because of the diagnostic difficulty and lack of clarity about which patients will benefit from conservative versus surgical treatment.
Treatment of TTS can be either surgical or non-surgical. The choice is usually made based on the aetiology of the problem and the degree of loss of function of the foot and ankle, and muscle atrophy.49–51
Surgical treatment is most useful for treating lesions that occupy space within the tarsal tunnel.13,31,52 In the absence of an identifiable lesion, the role of surgery is poorly defined; in fact, in these circumstances the results published in the literature are variable.53,54
Non-surgical treatment
Conservative management is usually successful. The goal is to relieve pain, inflammation and tissue stress. Abnormally slow nerve conduction through the posterior tibial nerve usually predicts failure of conservative treatment.49
Conservative management includes activity modification, pain relief drugs, physical and rehabilitation medicine, and corticosteroid injections into the tarsal tunnel (to reduce oedema).9,14,27,55
Pain-relieving drugs include oral analgesics (acetaminophen) and non-steroidal anti-inflammatory drugs (NSAIDs). Drugs for neuropathic pain (gabapentin, pregabalin, and tricyclic antidepressants) can be used. Topical medications (lidocaine and NSAIDs) can also be used.
Physical and rehabilitation medicine modalities for soft tissues that might help include cryotherapy, supportive inserts, changing to better fitting shoes or orthotic shoes, immobilization utilizing splints, ultrasound, iontophoresis, phonophoresis and E-stim. Calf stretching and nerve mobility or nerve gliding can also relieve symptoms. Strengthening the tibialis posterior can also help. Kinesiology tape can be used for arch support and biomechanical stress reduction.
Orthopaedic shoes can correct biomechanical abnormalities and unload the tarsal tunnel. A medial heel wedge or heel seat can reduce traction on the nerve by inverting the heel. Night splints and CAM (controlled ankle motion) walkers or temporary walking boots can also be used. Footwear with appropriate arch support can help reduce symptoms. If a ganglion cyst is present, it can be aspirated under ultrasound guidance.49
Surgical treatment
According to Kiel and Kaiser, the indications for surgical treatment of TTS are failure of conservative treatment and clear identification of the cause of the entrapment. In these circumstances, the results are usually satisfactory).49
Surgical treatment involves the release of the flexor retinaculum from its proximal attachment near the medial malleolus down to the sustentaculum tali, and sectioning the deep fascia of the abductor hallucis muscle to eliminate any possible compression of any of the terminal branches of the tibial nerve (Fig. 3). Surgical success rates vary from 44% to 96%. Patients who achieve better results are those with a clear aetiology, a positive Tinel’s sign prior to surgery, a younger age, those with a short history of symptoms, an early diagnosis, and no prior ankle pathology (Fig. 4).49
Fig. 3.
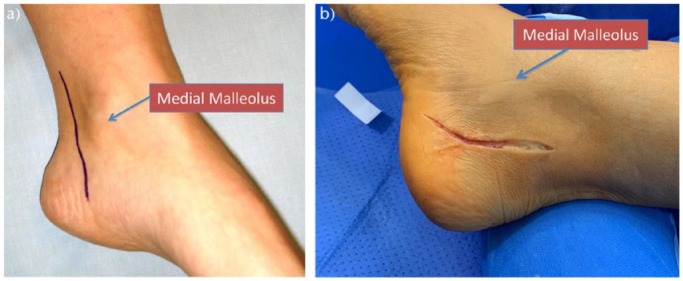
Surgical approach in tarsal tunnel syndrome (TTS): 5–6 cm incision, 1.5 cm posterior to the tibial malleolus, slightly arched towards the plantar region: (a) marked incision line; (b) surgical incision made.
Fig. 4.
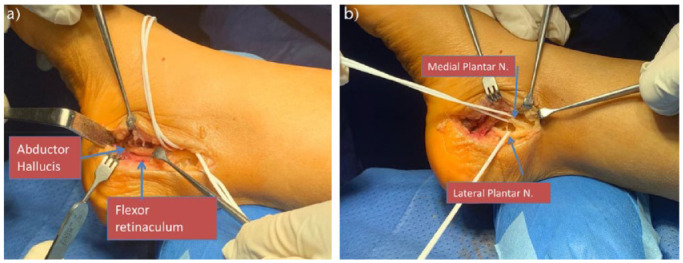
(a) Incision and opening of the flexor retinaculum longitudinally and in line with the skin incision. Note inside the posterior tibial nerve and how its branches pass deep to the abductor hallucis muscle; (b) identification of the medial plantar and lateral plantar branches of the tibial nerve.
Still et al evaluated the efficacy of intraoperative neuromonitoring (INM) as an adjunct to surgical tarsal tunnel decompression in 38 patients.56 INM was used to measure the voltage of the abductor hallucis and digiti quinti muscles before and after decompression. Intraoperative changes were acute and occurred within minutes of surgical decompression. Of the 38 patients studied, 29 (76%) had excellent results, with a mean change in microvolts of 2088.28 ± 1172.44 (684%) (p = 0.0004) and 2173.24 ± 1228.39 (742%) (p = 0.0014) for abductor hallucis and abductor digiti quinti, respectively. Thus, it appears that INM was a useful adjunct to surgical decompression of the tarsal tunnel.56
Yunoki et al analysed six cases of idiopathic TTS treated by tarsal tunnel opening, neurovascular decompression, and fascial release of the abductor hallucis muscle.7 In all cases, the preoperative nerve conduction test confirmed delayed sensory conduction velocity. The results were good, although in one case symptoms recurred.7
Iborra et al have described employing ultrasound-guided tarsal tunnel release for decompression of the tibial nerve, including its distal medial and lateral branches, to treat TTS in 81 patients.53 Of these, 76.5% had excellent results, 13.5% good results, and 10% poor results. The patients with the longest course of symptoms displayed the poorest results. Ultrasound-guided proximal and distal tarsal tunnel release for TTS provided very satisfactory results, similar to those of conventional and endoscopic techniques, with potentially lower risks, given it does not require exsanguinations of the leg and can be performed under local anaesthesia on an outpatient basis. A possible advantage is that it might decrease the risk of infection, wound complications or fibrosis. Another advantage of ultrasound-guided surgery over open or endoscopic techniques is that it can be performed bilaterally and in combination with other ultrasound-guided techniques, such as gastrocnemius lengthening and partial plantar fasciotomy. For Iborra et al, this technique could be the first surgical option for TTS decompression, given it has been shown to provide satisfactory results. However, these authors also mentioned that the learning curve is long, and that the technique requires a high-resolution ultrasound scanner and training to ensure the reliability of the ultrasound images. Therefore, they considered that further studies were needed to decide the best timing for surgery and to determine whether a surgical variant such as the hallucis abductor septum section could improve outcomes.53
Postoperative rehabilitation is essential and aims to protect joint and nerve integrity and control inflammation and pain. Contraction and adhesions of scar tissue must be avoided, while maintaining soft tissue and joint mobility. The long-term goal is to achieve normal gait, walking, and running.49
Prognosis
The prognosis of tarsal tunnel is variable.49 When the aetiology of the problem is a mass effect in the tarsal tunnel and it is detected early, the outcome is usually favourable. However, surgical decompression does not usually have a good prognosis in patients in whom no identifiable cause has been detected and who have not responded to conservative treatment. A positive Tinel’s sign before surgery is a strong predictor of surgical relief after decompression.49
A special situation concerns diabetes. A study of patients with diabetic neuropathy who also had positive Tinel’s sign and an enlarged tibial nerve on ultrasound showed no difference in symptoms or nerve size after surgical decompression of the tarsal tunnel.57 However, another publication on diabetic sensorimotor polyneuropathy has stated that release of the tarsal tunnel restored sensations in the sole of the foot.58
Rinkel et al have shown that patients with TTS have an increased risk of diabetic foot ulceration (DFU) due to elevated sensory thresholds. They evaluated the impact of TTS and initial sensory loss on DFU, given tibial nerve decompression could change the natural history of the disease (preventing diabetic foot disease and thus reducing the risk of amputation).59 It was observed that bilaterally affected patients have a poorer evolution compared to unilateral patients and controls, and they have a higher risk of developing DFU than unilateral patients. Thus, it appears that surgical decompression of the tarsal tunnel in diabetic patients with TTS might decrease the risk of developing DFU.60–62 Re-innervation of the desensitized foot is expected to be very rapid. This outcome makes this type of surgery a promising therapy to combat the increasingly burdensome and costly DFU pandemic.63,64 However, surgery for low extremities neuropathic disease (LEND) remains controversial.65
Complications
Untreated or refractory TTS can lead to neuropathies of the posterior tibial nerve and its branches, causing patients persistent pain. In addition, motor weakness and atrophy can subsequently develop. Postoperative complications include impaired surgical wound healing, infection and scar formation. Finally, surgical decompression sometimes does not adequately resolve pain and other symptoms.49
One important complication is the so-called ‘failed tarsal tunnel release’. In 2011, Gould stated that failed surgical releases of the tarsal tunnel might be due to a number of causes. Many of the failures are due to lack of appreciation of the involved anatomy or unsound surgical technique. When a deficient release is performed, a revision simply completes the necessary steps. When external scarring is the problem, barrier materials may be utilized to help protect the nerve after neurolysis. When intrinsic damage is the problem, nerve wrapping surgery technique, reconstruction, conduits, and nerve stimulators all play a role to re-establish function or improve pain.66
Another significant complication is the recurrence of tarsal tunnel syndrome after surgery. According to Gould, its main causes are deficient release, lack of comprehending or appreciation of the genuine anatomy implicated, variations in the anatomy of the nerve(s), failure to carry out the release accurately, bleeding with consequent scarring, damage to the nerve and branches, continuous hypersensitivity of the nerves, and pre-existing intrinsic damage to the nerve. Strategies include more thorough release, utilization of barrier materials to diminish adherence of the nerve to surrounding tissues to elude traction neuritis, excisions of neuromas utilizing conduits, and consideration of nerve stimulators and systemic medications to deal with continuous neural pain.67
Conclusions
Conservative management is usually successful. Abnormally slow nerve conduction through the posterior tibial nerve usually predicts failure of conservative treatment. Conservative management includes activity modification, pain relief drugs (acetaminophen, NSAIDs, drugs for neuropathic pain, topical medications), physical and rehabilitation medicine, and corticosteroid injections into the tarsal tunnel.
Physical and rehabilitation medicine modalities include: cryotherapy, supportive inserts (footwear with appropriate arch support, a medial heel wedge or heel seat), changing to better fitting shoes or orthotic shoes, immobilization using splints, ultrasound, iontophoresis, phonophoresis, E-stim, calf stretching and nerve mobility or nerve gliding, strengthening the tibialis posterior, kinesiology tape, night splints and CAM temporary walkers or walking boots. If a ganglion cyst is present, it can be aspirated under ultrasound guidance.
Indications for surgical treatment of TTS are failure of conservative treatment and clear identification of the aetiology of the problem. In these circumstances, the results are usually satisfactory, although success rates vary from 44% to 96%. Surgical treatment involves the release of the flexor retinaculum from its proximal attachment near the medial malleolus down to the sustentaculum tali. Patients who achieve better results are those who are younger, have no prior ankle pathology, have an early diagnosis, have a clear aetiology, have a positive Tinel’s sign prior to surgery, and have a short history of symptoms.
Footnotes
ICMJE Conflict of interest statement: The authors declare no conflict of interest relevant to this work.
OA licence text: This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Keck C. The tarsal-tunnel syndrome. J Bone Joint Surg [Am] 1962;44-A:180–182. [Google Scholar]
- 2. Lam SJ. Tarsal tunnel syndrome. J Bone Joint Surg [Br] 1967;49-B:87–92. [PubMed] [Google Scholar]
- 3. Hong CH, Lee HS, Lee WS, et al. Tarsal tunnel syndrome caused by posterior facet talocalcaneal coalition: a case report. Medicine (Baltimore) 2020;99:e20893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Iborra-Marcos A, Villanueva-Martinez M, Sanz-Ruiz P, Barrett SL, Zislis G. Ultrasound-guided proximal and distal tarsal decompression: an analysis of pressures in the tarsal, medial plantar, and lateral plantar tunnels. Foot Ankle Spec 2020;20:1–7. [DOI] [PubMed] [Google Scholar]
- 5. Alshami AM, Souvlis T, Coppieters MW. A review of plantar heel pain of neural origin: differential diagnosis and management. Man Ther 2008;13:103–111. [DOI] [PubMed] [Google Scholar]
- 6. Schon LC. Nerve entrapment, neuropathy, and nerve dysfunction in athletes. Orthop Clin North Am 1994;25:47–59. [PubMed] [Google Scholar]
- 7. Yunoki M. Analysis of surgical cases of tarsal tunnel syndrome in our department: case series and literature review. Asian J Neurosurg 2020;15:59–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kushner S, Reid DC. Medial tarsal tunnel syndrome: a review. J Orthop Sports Phys Ther 1984;6:39–45. [DOI] [PubMed] [Google Scholar]
- 9. McSweeney SC, Cichero M. Tarsal tunnel syndrome: a narrative literature review. Foot 2015;25:244–250. [DOI] [PubMed] [Google Scholar]
- 10. Baxter DE, Pfeffer GB. Treatment of chronic heel pain by surgical release of the first branch of the lateral plantar nerve. Clin Orthop Relat Res 1992;279:229–236. [PubMed] [Google Scholar]
- 11. Baxter DE, Pfeffer GB, Thigpen M. Chronic heel pain: treatment rationale. Orthop Clin North Am 1989;20:563–569. [PubMed] [Google Scholar]
- 12. Dellon AL. The four medial ankle tunnels: a critical review of perceptions of tarsal tunnel syndrome and neuropathy. Neurosurg Clin N Am 2008;19:629–648. [DOI] [PubMed] [Google Scholar]
- 13. Madani S, Doughty C. Lower extremity entrapment neuropathies. Best Pract Res Clin Rheumatol 2020;34:101565. [DOI] [PubMed] [Google Scholar]
- 14. Ahmad M, Tsang K, Mackenney PJ, Adedapo AO. Tarsal tunnel syndrome: a literature review. Foot Ankle Surg 2012;18:149–152. [DOI] [PubMed] [Google Scholar]
- 15. Havel PE, Ebraheim NA, Clark SE, Jackson WT, DiDio L. Tibial nerve branching in the tarsal tunnel. Foot Ankle 1988;9:117–119. [DOI] [PubMed] [Google Scholar]
- 16. Torres AL, Ferreira MC. Study of the anatomy of the tibial nerve and its branches in the distal medial leg. Acta Ortop Bras 2012;20:157–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Singh G, Kumar VP. Neuroanatomical basis for the tarsal tunnel syndrome. Foot Ankle Int 2012;33:513–518. [DOI] [PubMed] [Google Scholar]
- 18. Heimkes B, Posel P, Stotz S, Wolf K. The proximal and distal tarsal tunnel syndromes: an anatomical study. Int Orthop 1987;11:193–196. [DOI] [PubMed] [Google Scholar]
- 19. Cimino WR. Tarsal tunnel syndrome: review of the literature. Foot Ankle 1990;11:47–52. [DOI] [PubMed] [Google Scholar]
- 20. Antoniadis G, Scheglmann K. Posterior tarsal tunnel syndrome: diagnosis and treatment. Dtsch Arztebl Int 2008;105:776–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Oh SJ, Meyer RD. Entrapment neuropathies of the tibial (posterior tibial) nerve. Neurol Clin 1999;17:593–615. [DOI] [PubMed] [Google Scholar]
- 22. López-Gavito E, Parra-Téllez P, Cornejo-Olvera R, Vázquez-Escamilla J.[Tarsal tunnel syndrome: review of the topic as a result of one case]. Acta Ortop Mex 2014;28:197–202. [PubMed] [Google Scholar]
- 23. Huynh W, Kuan J, Cordato DJ. Extraneural ganglionic cysts causing tarsal tunnel syndrome. Clin Neurophysiol 2020;131:1241–1242. [DOI] [PubMed] [Google Scholar]
- 24. Kim YS, Lee MK, Yi Y. Atypical musculoskeletal manifestations on flexor hallucis longus tendon of gout causing tarsal tunnel syndrome in diabetic patients: a case report. Medicine 2019;98:51(e18374). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Won SH, Kim J, Min TH, et al. Tarsal tunnel syndrome secondary to osteochondroma of the calcaneus: a case report. BMC Musculoskelet Disord 2020;21:491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Walley KC, Johns WL, Jackson JB, Gonzalez TA. Plantar medial avulsion fracture of the calcaneus with acute tarsal tunnel: case report and technique tip. Foot Ankle Int 2020;41:1002–1006. [DOI] [PubMed] [Google Scholar]
- 27. Lau JT, Daniels TR. Tarsal tunnel syndrome: a review of the literature. Foot Ankle Int 1999;20:201–209. [DOI] [PubMed] [Google Scholar]
- 28. Ferkel E, Davis WH, Ellington JK. Entrapment neuropathies of the foot and ankle. Clin Sports Med 2015;34:791–801. [DOI] [PubMed] [Google Scholar]
- 29. Jackson DL, Haglund BL. Tarsal tunnel syndrome in runners. Sports Med 1992;13:146–149. [DOI] [PubMed] [Google Scholar]
- 30. Takakura Y, Kitada C, Sugimoto K, Tanaka Y, Tamai S. Tarsal tunnel syndrome: causes and results of operative treatment. J Bone Joint Surg [Br] 1991;73:125–128. [DOI] [PubMed] [Google Scholar]
- 31. Nagaoka M, Satou K. Tarsal tunnel syndrome caused by ganglia. J Bone Joint Surg [Br] 1999;81-B:607–610. [DOI] [PubMed] [Google Scholar]
- 32. Julsrud ME. An unusual cause of tarsal tunnel syndrome. J Foot Ankle Surg 1995;34:289–293. [DOI] [PubMed] [Google Scholar]
- 33. Hendrix CL, Jolly GP, Garbalosa JC, Blume P, Dosremedios E. Entrapment neuropathy: the etiology of intractable chronic heel pain syndrome. J Foot Ankle Surg 1998;37:273e9. [DOI] [PubMed] [Google Scholar]
- 34. Komagamine J. Bilateral tarsal tunnel syndrome. Am J Med 2018;131:e319. [DOI] [PubMed] [Google Scholar]
- 35. Bailie DS, Kelikian AS. Tarsal tunnel syndrome: diagnosis, surgical technique, and functional outcome. Foot Ankle Int 1998;19:65–72. [DOI] [PubMed] [Google Scholar]
- 36. Trepman E, Kadel NJ, Chisholm K, Razzano L. Effect of foot and ankle position on tarsal tunnel compartment pressure. Foot Ankle Int 1999;20:721–726. [DOI] [PubMed] [Google Scholar]
- 37. Buxton WG, Dominick JE. Electromyography and nerve conduction studies of the lower extremity: uses and limitations. Clin Podiatr Med Surg 2006;23:531–543. [DOI] [PubMed] [Google Scholar]
- 38. Belen J. Orthodromic sensory nerve conduction of the medial and lateral plantar nerves: a standardization. Am J Phys Med 1985;64:17–23. [PubMed] [Google Scholar]
- 39. Galardi G, Amadio S, Maderna L, et al. Electrophysiologic studies in tarsal tunnel syndrome: diagnostic reliability of motor distal latency, mixed nerve and sensory nerve conduction studies. Am J Phys Med Rehabil 1994;73:193–198. [PubMed] [Google Scholar]
- 40. Boon AJ, Harper CM. Needle EMG of abductor hallucis and peroneus tertius in normal subjects. Muscle Nerve 2003;27:752–756. [DOI] [PubMed] [Google Scholar]
- 41. Nakano H, Shima H, Tei K, Saura R. Ultrasound-assisted near nerve method in nerve conduction study for the diagnosis of tarsal tunnel syndrome: a case report. Clin Neurophysiol Pract 2020;5:135–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Kamm CP, Scheidegger O, Rösler KM. Ultrasound-guided needle positioning in sensory nerve conduction study of the sural nerve. Clin Neurophysiol 2009;120:1342–1345. [DOI] [PubMed] [Google Scholar]
- 43. Kumar K, Deshpande S, Jain M, Nayak MG. Evaluation of various fibro-osseous tunnel pressures (carpal, cubital and tarsal) in normal human subjects. Indian J Physiol Pharmacol 1988;32:139–145. [PubMed] [Google Scholar]
- 44. Kerr R, Frey C. MR imaging in tarsal tunnel syndrome. J Comput Assist Tomogr 1991;15:280–286. [DOI] [PubMed] [Google Scholar]
- 45. Chhabra A, Subhawong TK, Williams EH, et al. High-resolution MR neurography: evaluation before repeat tarsal tunnel surgery. AJR Am J Roentgenol 2011;197:175–183. [DOI] [PubMed] [Google Scholar]
- 46. Tawfik EA, El Zohiery AK, Abouelela AAK. Proposed sonographic criteria for the diagnosis of idiopathic tarsal tunnel syndrome. Arch Phys Med Rehabil 2016;97:1093–1099. [DOI] [PubMed] [Google Scholar]
- 47. Frey C, Kerr R. Magnetic resonance imaging and the evaluation of tarsal tunnel syndrome. Foot Ankle 1993;14:159–164. [DOI] [PubMed] [Google Scholar]
- 48. Rosson GD, Larson AR, Williams EH, Dellon AL. Tibial nerve decompression in patients with tarsal tunnel syndrome: pressures in the tarsal, medial plantar, and lateral plantar tunnels. Plast Reconstr Surg 2009;124:1202–1210. [DOI] [PubMed] [Google Scholar]
- 49. Kiel J, Kaiser K. Tarsal tunnel syndrome. In: StatPearls [https://publons.com/journal/675344/statpearls-internet-treasure-island-fl-statpearls-/]. Treasure Island Florida, US: StatPearls Publishing, 2021. [date last accessed 27 September 2021] [PubMed] [Google Scholar]
- 50. Mansfield CJ, Bleacher J, Tadak P, Briggs MS. Differential examination, diagnosis and management for tingling in toes: Fellow’s case problem. J Manual Manip Ther 2017;25:294–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Tu P. Heel pain: diagnosis and management. Am Fam Physician 2018;97:86–93. [PubMed] [Google Scholar]
- 52. Pfeiffer WH, Cracchiolo A, III. Clinical results after tarsal tunnel decompression. J Bone Joint Surg [Am] 1994;76:1222–1230. [DOI] [PubMed] [Google Scholar]
- 53. Iborra Á, Villanueva-Martínez M, Barrett SL, Rodríguez-Collazo ER, Sanz-Ruiz P. Ultrasound-guided release of the tibial nerve and its distal branches: a cadaveric study. J Ultrasound Med 2019;38:2067–2079. [DOI] [PubMed] [Google Scholar]
- 54. Ward PJ, Porter ML. Tarsal tunnel syndrome: a study of the clinical and neurophysiological results of decompression. J R Coll Surg Edinb 1998;43:35–36. [PubMed] [Google Scholar]
- 55. Kavlak Y, Uygur F. Effects of nerve mobilization exercise as an adjunct to the conservative treatment for patients with tarsal tunnel syndrome. J Manipulative Physiol Ther 2011;34:441–448. [DOI] [PubMed] [Google Scholar]
- 56. Still GP, Pfau ZJ, Cordoba A, Jupiter DC. Intraoperative nerve monitoring for tarsal tunnel decompression: a surgical technique to improve outcomes. J Foot Ankle Surg 2019;58:1203–1209. [DOI] [PubMed] [Google Scholar]
- 57. Macaré van Maurik JF, Schouten MEL, ten Katen I, van Hal M, Peters EJ, Kon M. Ultrasound findings after surgical decompression of the tarsal tunnel in patients with painful diabetic polyneuropathy: a prospective randomized study. Diabetes Care 2014;37:767–772. [DOI] [PubMed] [Google Scholar]
- 58. Agarwal P, Sharma B, Sharma D. Tarsal tunnel release restores sensations in sole for diabetic sensorimotor polyneuropathy. J Clin Orthop Trauma 2020;11:442–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Rinkel WD, Castro Cabezas M, Birnie E, Coert JH. The natural history of tarsal tunnel syndrome in diabetic subjects. J Plast Reconstr Aesthet Surg 2020;73:1482–1489. [DOI] [PubMed] [Google Scholar]
- 60. Gondring WH, Tarun PK, Trepman E. Touch pressure and sensory density after tarsal tunnel release in diabetic neuropathy. Foot Ankle Surg 2012;18:241–246. [DOI] [PubMed] [Google Scholar]
- 61. Best TJ, Best CA, Best AA, Fera LA. Surgical peripheral nerve decompression for the treatment of painful diabetic neuropathy of the foot: a level 1 pragmatic randomized controlled trial. Diabetes Res Clin Pract 2019;147:149–156. [DOI] [PubMed] [Google Scholar]
- 62. Baltodano PA, Basdag B, Bailey CR, et al. The positive effect of neurolysis on diabetic patients with compressed nerves of the lower extremities: a systematic review and meta-analysis. Plast Reconstr Surg Glob Open 2013;1:e24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Zhang P, Lu J, Jing Y, Tang S, Zhu D, Bi Y. Global epidemiology of diabetic foot ulceration: a systematic review and meta-analysis. Ann Med 2017;49:106–116. [DOI] [PubMed] [Google Scholar]
- 64. Zhou B, Lu Y, Hajifathalian K, et al. ; NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet 2016;387:1513–1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Albers JW, Jacobson R. Decompression nerve surgery for diabetic neuropathy: a structured review of published clinical trials. Diabetes Metab Syndr Obes 2018;11:493–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Gould JS. The failed tarsal tunnel release. Foot Ankle Clin 2011;16:287–293. [DOI] [PubMed] [Google Scholar]
- 67. Gould JS. Recurrent tarsal tunnel syndrome. Foot Ankle Clin 2014;19:451–467. [DOI] [PubMed] [Google Scholar]


