Abstract
Aneurysms of the left atrial appendage (LAA) are rare entities that often require surgical intervention. We demonstrate multimodality imaging features of a giant LAA aneurysm, with a focus on 3-dimensional blood flow dynamics by using 4-dimensional-flow cardiac magnetic resonance. (Level of Difficulty: Advanced.)
Key Words: cardiac magnetic resonance, computed tomography, echocardiography, hemodynamics
Abbreviations and Acronyms: AF, atrial fibrillation; CMR, cardiac magnetic resonance; CT, computed tomography; Cx, circumflex (artery); LA, left atrial/atrium; LAA, left atrial appendage; LAAA, left atrial appendage aneurysm; LV, left ventricular; SVT, supraventricular tachycardia; 4D, 4-dimensional
Graphical abstract
History of Presentation
A 38-year-old male patient presented with a recent syncopal episode in the setting of supraventricular tachycardia (SVT) and a history of palpitations and atypical chest pain for 1.5 years. He underwent an electrophysiology study for attempted SVT ablation. The study was aborted out of concern for a left atrial (LA) aneurysm.
Learning Objectives
-
•
To identify the exact location and extent of any cardiac aneurysm with multimodality imaging.
-
•
To understand that CMR with 4D flow enables clinicians to visualize and investigate complex blood flow dynamics in vivo.
Differential Diagnosis
The differential diagnosis comprised LA aneurysm and LA appendage (LAA) aneurysm (LAAA).
Investigations
Initial computed tomography (CT) ruled out a hemopericardium or another acute complication of attempted SVT ablation, and an aneurysm of the left atrium was diagnosed (Figures 1B and 1C, white arrows). The patient underwent further diagnostic work-up.
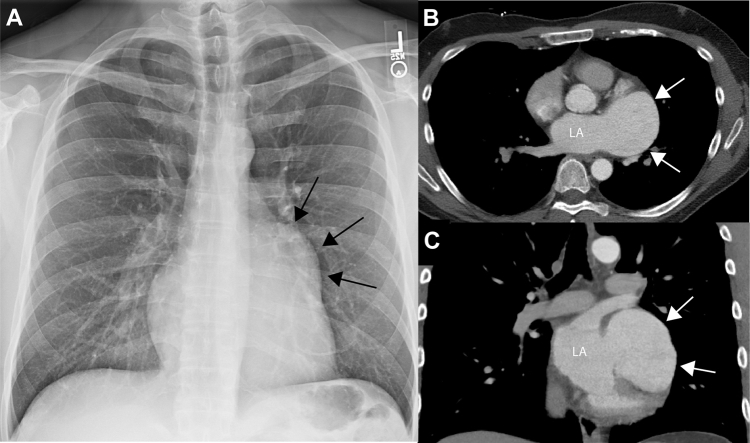
Figure 1.
Initial Radiograph and CT Imaging
(A) Chest radiograph showed dilatation of the left side of the heart (black arrows). (B and C) Contrast-enhanced computed tomography (CT) confirmed a giant left atrial appendage aneurysm with dimensions of 5.7 × 5.3 cc × 8.2 cm (white arrows). LA = left atrium.
Transthoracic echocardiography demonstrated moderate mitral regurgitation secondary to annular dilation and a 7.0 × 4.0 cm LA aneurysm without evidence of thrombus (Figures 2A and 2B).
Figure 2.
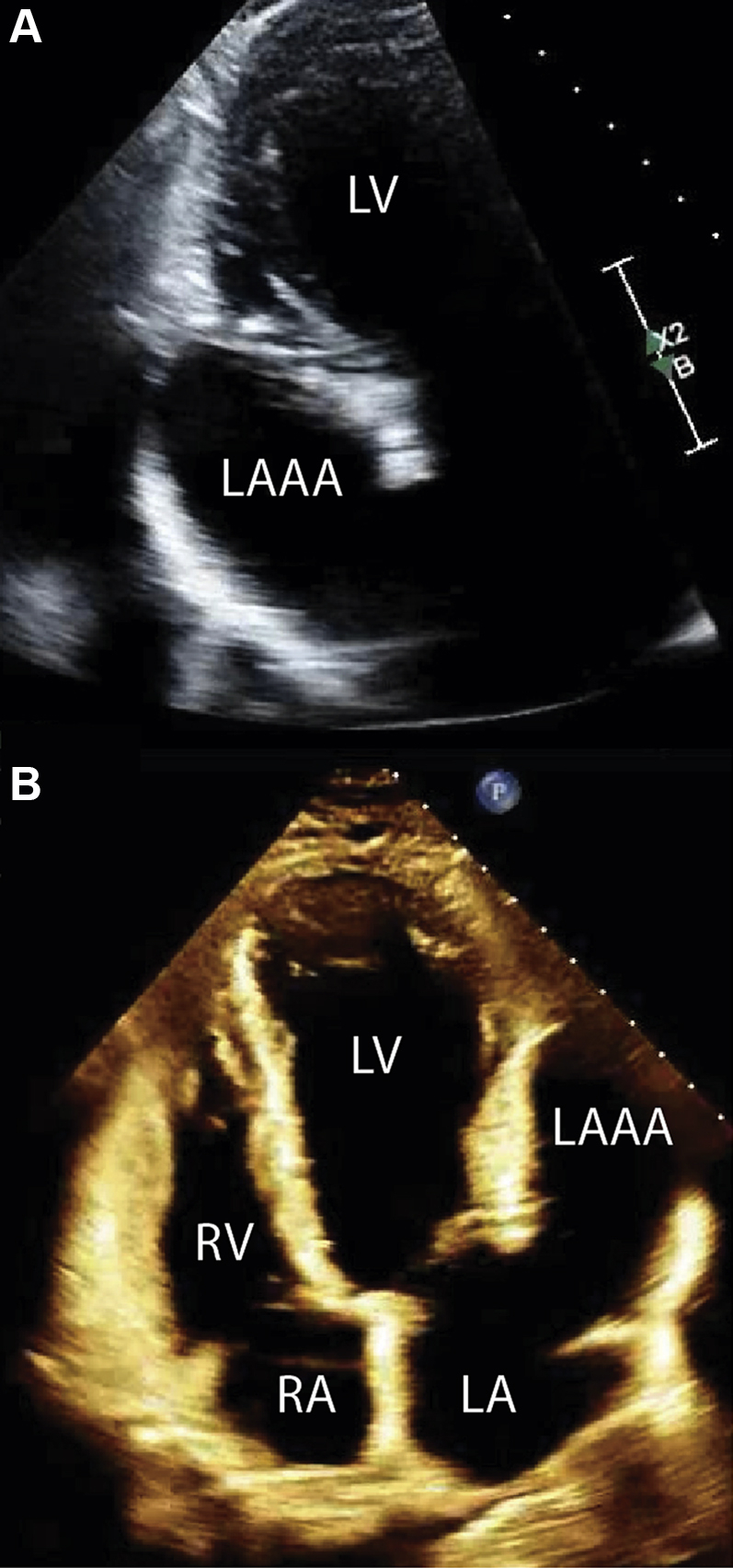
TTE Assessment
(A and B) Transthoracic echocardiography (TTE) confirmed the aneurysm of the left atrial appendage with no evidence of thrombus. LA = left atrium; LAAA = left atrial appendage aneurysm; LV = left ventricle; RA = right atrium; RV = right ventricle.
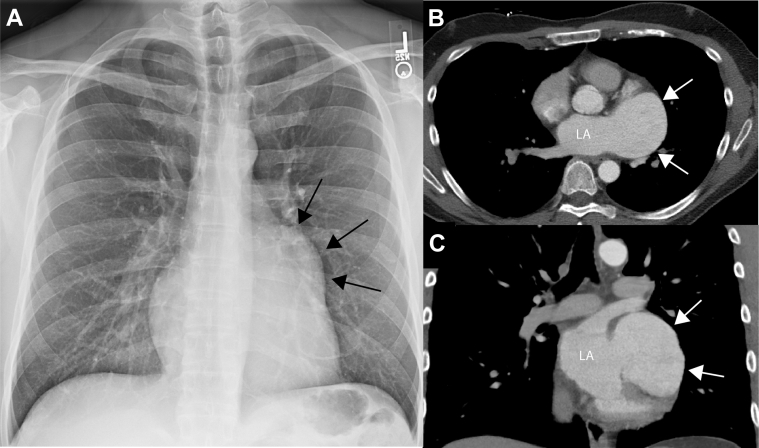
Cardiac magnetic resonance (CMR), including 4-dimensional (4D)-flow sequence, was performed to visualize the anatomy and confirm the absence of thrombus. The imaging showed a giant LAAA without thrombus (5.7 × 5.3 cc × 8.2 cm) (Figures 3A and 3B). LAAA volume was 174 mL; in comparison LA volume was 73 mL. The 4D-flow analysis revealed significant inflow and outflow between the left atrium and the LAAA (approximately 40 mL per cardiac cycle) (Figures 3C to 3E, Videos 1 and 2). Outflow from the LAAA into the left atrium was seen at 2 points during the cardiac cycle: during the conduit phase after mitral valve opening and immediately after the LA contraction (Figure 3E). In contrast, there were still areas of high stasis in the LAAA, mainly in its apex (Figures 3D1 and 3D2). Left ventricular (LV) function was normal (LV ejection fraction, 65%; no myocardial late enhancement after contrast enhancement [not shown]).
Figure 3.
CMR Including Advanced 4D-Flow Analysis of Blood Flow and Stasis in the LA and LAAA
(A) T2-weighted cardiac magnetic resonance (CMR) and (B) postcontrast magnetic resonance angiography also showed the left atrial appendage aneurysm (LAAA) without evidence of thrombus. The 4-dimensional (4D)-flow cardiac magnetic resonance–derived pathlines showed (C1) flow into the left atrial appendage aneurysm during atrial diastole and (C2) outflow during atrial systole. (D1) Stasis maps showed no areas of high stasis in the left atrium (LA); (D2) conversely, there was high stasis in the periphery of the whole left atrial appendage (LAA). (E) During 1 cardiac cycle, inflow and outflow between the left atrium and left atrial appendage was observed, totaling approximately 40 mL.
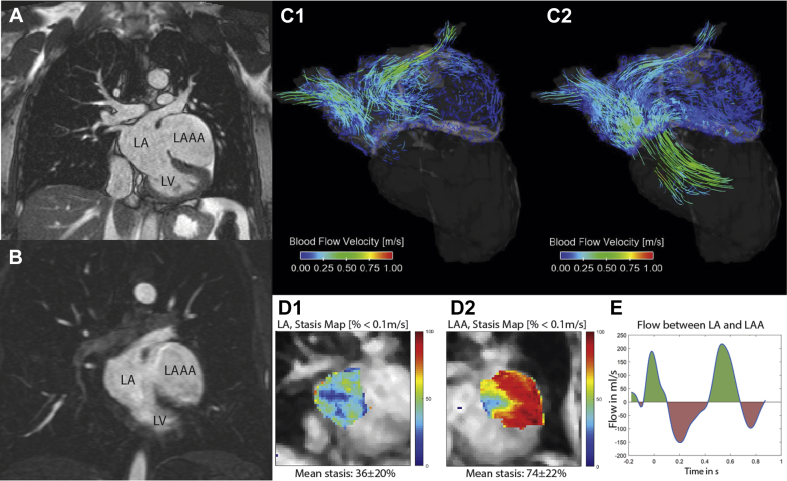
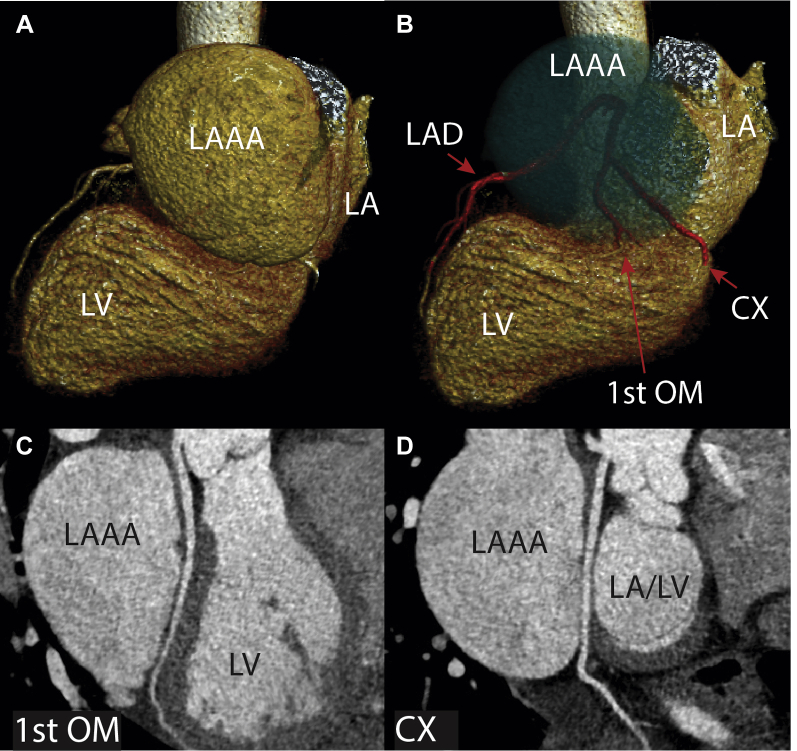
Coronary CT angiography was then performed to assess the relationship of the LAAA with the coronary arteries. The LAAA sat on top the circumflex artery (Cx) and its strong first obtuse marginal branch, but there was no sign of atherosclerosis or luminal compression (Figures 4A to 4D). However, there was extrinsic compression of the left ventricle in response to the LAAA (Figure 4B).
Figure 4.
Coronary CT Showing Relations Between LAAA and Coronary Arteries
(A and B) Volume-rendering technique from coronary computed tomography (CT) revealed the proximity of the left atrial appendage aneurysm (LAAA) to the circumflex (CX) and first obtuse marginal arteries (1st OM), as well as (B) an indentation of the left atrial appendage aneurysm on the left ventricle (LV). Curved centerline views of (C) the first obtuse marginal artery and (D) the circumflex artery showed narrowing of those vessels between the left atrial appendage aneurysm and the left ventricle. LA = left atrium; LAD = left anterior descending artery.
Surgical resection of the LAAA was recommended on the basis of the patient’s symptoms, supraventricular arrhythmia, risk of thrombus formation, and potential risk of rupture.
Management
The patient underwent LAAA resection through median sternotomy and with cardiopulmonary bypass. The left atrium was opened to visualize the internal os of the LAAA and to address mitral valve disease associated with the aneurysm (Figure 5A, Video 3). With care taken to identify the left Cx artery clearly, the aneurysm was sharply resected on the epicardial surface and was then oversewn in 2 layers with suture. Attention was then turned to the left atrium, and the os of the LAAA was examined and oversewn with 2 layers of suture from the endocardial side. After resection and repair, the left ventricle was pressurized with saline, and the mitral valve was found to be competent and without abnormality along the zone of coaptation. The maximum diameter of the resected LAAA measured approximately 9 cm (Figure 5B). Separation from cardiopulmonary bypass was routine. Intraoperative transesophageal echocardiography confirmed mitral valvular competence, complete LAA occlusion, normal postbypass ventricular function, and uncompromised flow in the left Cx artery. The patient was discharged on postoperative day 3 after a routine convalescence.
Figure 5.
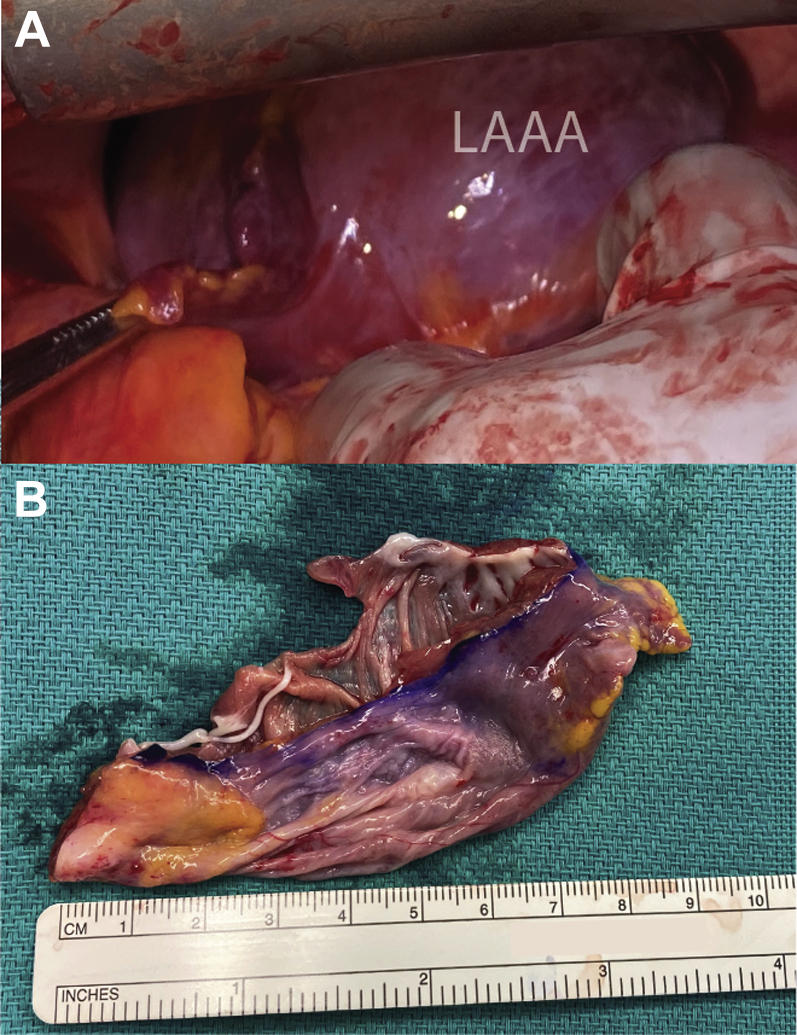
Intraoperative View and Resected LAAA
(A) Intraoperative view of the left atrial appendage aneurysm (LAAA). (B) The resected left atrial appendage aneurysm measured approximately 9 cm.
Discussion
In this case report, we present the first known CMR 4D-flow analysis in a case of LAAA. LAAA is a rare entity, with mainly single case reports and 1 review of multiple case reports published (1, 2, 3). These aneurysms can be congenital or acquired, and acquired LAAA is mainly related to mitral valve disease. In general, patients with LAAA receive the diagnosis between 30 and 50 years of age. Symptoms and complications can vary, ranging from chest discomfort, palpitations, and arrhythmias to even acute stroke caused by a thrombus in the LAAA; this emphasizes the importance of early diagnosis and adequate treatment (1).
Our patient was symptomatic for 1.5 years, with a recent syncopal episode in the setting of SVT that triggered further diagnostic work-up. The finding of left-sided cardiomegaly noted on the chest radiograph (Figure 1A) raised suspicion of a left-sided heart process. Echocardiography detected the abnormality and prompted further investigation to clarify whether the aneurysm arose from the left atrium or the LAA.
CMR allowed precise diagnosis and confirmed the absence of thrombus. The 4D-flow CMR is a novel technique used to visualize 3-dimensional blood flow dynamics in vivo (4). In this case, the 4D-flow sequence revealed significant flow between the left atrium and the LAA of approximately 40 mL over 1 cardiac cycle. However, LAA stasis maps, also derived from the 4D-flow sequence, showed areas of high stasis, especially in the apex of the LAAA. These areas are at risk for thrombus formation, whereas conversely, the left atrium had no areas of high stasis in its stasis maps.
Given the close proximity and potential involvement of the coronary arteries, coronary CT angiography was performed. There are a few rare cases of LAAA in which even myocardial infarction was caused, for example, in a 15-year-old male patient (1). Our patient showed no signs of coronary disease or relationship between the LAAA and the coronary arteries, but the LV shape was deformed by the size of the LAAA. Although this did not affect cardiac function and there was no sign of myocardial damage or infarction on CMR, the impact of this LV change on myocardial function and mechanics during exertion or further growth was unknown.
Approximately 50% of patients with LAAA have a diagnosis of atrial fibrillation (AF), which is generally, and specifically in patients with LAAA, a major risk factor for thrombus formation (in patients with LAAA, the risk increases by 2.7) (1). Our patient did not have a history of AF but did have SVT, and we believe that he would have been considered at risk of AF development without adequate treatment of the LAAA.
Surgical therapy with aneurysmectomy is the gold standard for LAAA in patients without thrombus (as in our case; otherwise, anticoagulation should be introduced to resolve the thrombus first), and it is related to a very good outcome (1). This was also the case for our patient. He was able to be released in stable condition 3 days after surgery; follow-up has been unremarkable to date.
Follow-Up
After discharge, the patient received 14-day rhythm monitoring, which was negative for AF. He remains on a regimen of low-dose aspirin to date.
Conclusions
CMR with 4D flow helped to confirm the diagnosis of an LAAA and the absence of thrombus; the patient could then undergo successful aneurysmectomy.
Funding Support and Author Disclosures
Dr Pradella has reported support from the Bangerter-Rhyner Foundation and Freiwillige Akademische Gesellschaft Basel. Dr Allen has reported consulting for Circle Cardiovascular Imaging; has received an honorarium from Medscape; and has received a grant from the American Heart Association. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental videos, please see the online version of this paper.
Appendix
4D-Flow CMR Pathlines Complete. 4D-flow CMR–derived pathline visualization over 5 cardiac cycles showed early inflow of blood through the pulmonary veins into the LA and LAA. After mitral valve opening, initial outflow of blood from the LAA is observed, which is followed by a short inflow again. Just before mitral valve closure, the atrial kick initiates another outflow of blood from the LAA.
4D-Flow CMR Pathlines Between LA and LAA. 4D-flow CMR–derived pathlines originating from a plane between the LA and LAA visualize the complex inflow and outflow patterns of blood between the LA and the LAA during the cardiac cycle.
Intraoperative View. Intraoperative view of the LAA aneurysm located on top of the contracting left ventricle before cardioplegia.
References
- 1.Aryal M.R., Hakim F.A., Ghimire S., et al. Left atrial appendage aneurysm: a systematic review of 82 cases. Echocardiography. 2014;31:1312–1318. doi: 10.1111/echo.12667. [DOI] [PubMed] [Google Scholar]
- 2.Khanra D., Tiwari P., Kodliwadmath A., Duggal B. Giant left atrial appendage aneurysm and atrial fibrillation: chicken or the egg? BMJ Case Rep. 2019;12(8) doi: 10.1136/bcr-2019-231300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smeglin A., Merchan J., Maysky M., Johnstone M., Pastore J.O. Images in cardiovascular medicine: Giant left atrial appendage aneurysm. Circulation. 2008;118:2393–2394. doi: 10.1161/CIRCULATIONAHA.108.776146. [DOI] [PubMed] [Google Scholar]
- 4.Markl M., Frydrychowicz A., Kozerke S., Hope M., Wieben O. 4D flow MRI. J Magnet Res Imaging. 2012;36:1015–1036. doi: 10.1002/jmri.23632. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
4D-Flow CMR Pathlines Complete. 4D-flow CMR–derived pathline visualization over 5 cardiac cycles showed early inflow of blood through the pulmonary veins into the LA and LAA. After mitral valve opening, initial outflow of blood from the LAA is observed, which is followed by a short inflow again. Just before mitral valve closure, the atrial kick initiates another outflow of blood from the LAA.
4D-Flow CMR Pathlines Between LA and LAA. 4D-flow CMR–derived pathlines originating from a plane between the LA and LAA visualize the complex inflow and outflow patterns of blood between the LA and the LAA during the cardiac cycle.
Intraoperative View. Intraoperative view of the LAA aneurysm located on top of the contracting left ventricle before cardioplegia.