Abstract
Childhood adversity is a well-established risk factor for mental health problems during adolescence. Using data from the Fragile Families and Child Wellbeing Study and latent class analysis (LCA), we examined patterns of exposure to ten adverse childhood experiences (ACEs), including socioeconomic adversity, among non-Hispanic (NH) White, NH Black, and Hispanic 9 year olds and determined associations between membership in ACE exposure “classes” and depression and anxiety scores at age 15 (N = 2849). Parental separation/divorce, economic hardship, and paternal incarceration were the most common ACEs. ACE prevalence was significantly higher among Blacks and Hispanics. ACEs clustered into four classes for Whites and Hispanics and three classes for Blacks. Over half of Whites were classified in the ‘Low Adversity’ class. Conversely, most Black and Hispanic adolescents were classified in the ‘High Socioeconomic Adversity and Paternal Incarceration’ class, characterized by above average probabilities of experiencing family economic hardship, parental separation/divorce, low maternal education, and paternal incarceration. A small share of adolescents in all three racial/ethnic groups were in the ‘High Global Adversity’ class, characterized by high probability of exposure to most ACEs, including physical and psychological abuse. Finally, ACE class membership was differentially associated with anxiety and depression across the three racial/ethnic groups, with generally larger differences in mental health scores across ACE groups for Whites than for Blacks and Hispanics. Our findings suggest that studies on the associations between ACEs and health outcomes that do not include childhood economic adversity risk underestimating the role of ACEs on mental health among racial/ethnic minorities. Moreover, different patterns of ACE exposure are differentially linked to anxiety and depression, and ACE group membership differences in anxiety and depression vary by racial/ethnic group. Findings suggest the need for racially tailored prevention and intervention strategies.
Keywords: Adverse childhood experiences, Adolescent mental health, Racial disparities, Socioeconomic adversity
Highlights
-
•
In a U.S. sample of low-income children, 93% experienced at least one ACE in past year.
-
•
ACEs cluster differently for White, Black, and Hispanic adolescents.
-
•
Most White adolescents are in a low adversity class.
-
•
Most Black and Hispanic adolescents are in a high SES adversity and parental incarceration class.
-
•
There are race differences in relationships between ACE classes and mental health.
1. Introduction
Childhood adversity is a well-established risk factor for mental health problems throughout the life course, including adolescence (Kalmakis & Chandler, 2015; Hughes et al., 2017; Norman et al., 2012 for systematic reviews). In the United States, estimates of exposure to at least one adverse childhood experience (ACEs) range from 48% to two-thirds (Anda et al., 2006; Bethell et al., 2014; Campbell et al., 2016; Monnat & Chandler, 2015; Sacks & Murphey, 2019), with more than one-third of adults reporting multiple exposures (Bethell et al., 2014).
Traditional ACE measures include physical, verbal/emotional, and sexual abuse and parental divorce, domestic violence, incarceration, substance misuse, and mental illness.
Prior research documents the negative influences of ACEs on mental health among U.S. adolescents (Elmore & Crouch, 2020; Hunt et al., 2017; Lanier et al., 2018; Lew & Xian, 2019). For example, using Fragile Families and Child Well Being Study data, Hunt et al. (2017) found that children experiencing at least four ACEs by age 5 had over seven times greater odds of anxiety or depression at age 9 than those with fewer ACEs. Using the National Survey of Children's Health (NSCH), Lew and Xian (2019) found that adolescents ages 6–17 with higher ACE scores were three times more likely to experience anxiety or depression than those with lower ACE scores. Also using the NSCH, Elmore and Crouch (2020) found that all nine ACE measures they included were associated with greater odds of anxiety and depression among adolescents ages 8–17 and that children exposed to four or more ACEs had 1.7 times greater odds of anxiety and 2.2 greater odds of depression than their peers with lower or no ACE exposure.
The mental health consequences of ACE exposure have been linked to toxic stress and permanent changes in brain structure and development resulting from “exaggerated, frequent, and/or prolonged activation of the physiological stress response system” (McLaughlin, 2016, p. 6) and “repeated wear and tear on the body's physiological and psychological mechanisms [that] render the system unable to effectively respond to new stressors” (Liu et al., 2018, p. 89).
Although prior research has successfully built the evidence base documenting poor mental health outcomes among adolescents with ACEs, there remain important limitations. First, most research relies on the adversity measures captured in Felitti et al.’s (1998) foundational ACE study. However, those measures do not fully capture the range of adverse experiences that can affect health in adolescence or later life. This limitation is particularly relevant when researching more disadvantaged populations. The original ACE study was comprised of a comparatively advantaged sample (mostly White, college educated, insured). Finkelhor et al. (2015) suggest that socioeconomic status (SES) indicators are essential additions to the original ACE scale when examining relationships between ACEs and mental health. Indeed, Wade et al. (2014) found that several socioeconomic adversities, such as single-parenthood and economic hardship, emerged as more important than the conventional ACE measures in predicting health outcomes. These studies suggest that socioeconomic adversities may be more or just as important as the traditional ACE measures in influencing adolescent mental health. Childhood socioeconomic adversity can be viewed as a “fundamental cause of disease” (Link & Phelan, 1995) because it reduces access to knowledge, resources, networks, and experiences essential for development, thriving, and mental wellbeing. Accordingly, our study incorporates both traditional ACE measures and measures of childhood socioeconomic adversity.
Second, prior research in this area has mostly used an ACE count to measure the cumulative risk of adversities (Choi et al., 2019; Elmore & Crouch, 2020; Finkelhor et al., 2015; Hunt et al., 2017). This approach assumes that ACEs have an additive or linear dose effect and influence outcomes through similar mechanisms (Bergman & Magnusson, 1997; Hagan et al., 2016). This approach does not account for the important and dynamic interplay among adversities and precludes understanding the heterogeneous impacts of ACEs (Hagan et al., 2016). Researchers who instead adopt a mixture modeling approach, such as latent class analysis (LCA), have found that adversities occur in meaningful clusters (Berzenski & Yates, 2011; Hagan et al., 2016; Lanier et al., 2018; Lew & Xian, 2019). For example, using LCA with NSCH data, Lew and Xian (2019) found that children fell into one of four classes with almost half falling into a class characterized only by higher probability of having divorced parents. The other three classes were characterized by higher probabilities of parental mental health and substance use problems, higher probability of income hardship, and a global ACE class wherein children experienced higher probabilities of most ACEs compared to children in the other classes. LCA enables researchers to explore how different adversities may work together or separately to predict outcomes. LCA is also a “person-centered approach” to uncovering unobserved similarities and heterogeneities among subgroups based on the assumption that a sample includes a mixture of subpopulations (Masyn, 2017; McLachlan & Peel, 2000). As such, a growing body of studies have used LCA to understand how ACEs cluster (see Debowska et al., 2017 and O'Donnell et al., 2017 for reviews). Understanding how ACEs cluster to affect mental health can inform interventions that better screen for and target the specific pathways to ACE exposure and their association with later life outcomes. Our study builds on these previous studies by using LCA to understand how the class membership of ACEs is associated with adolescent mental health outcomes.
Finally, existing studies show significant racial disparities in ACE exposure and clustering. Compared to White adults, non-Whites report higher ACE prevalence (Cronholm et al., 2015; Mersky & Janczewski, 2018; Slopen et al., 2016). Using LCA to examine racial variation in ACE clusters in the NSCH, Maguire-Jack et al. (2020) found six ACE classes for White children, three for Black children, and five for Hispanic children. This study suggests that ACEs cluster differently by racial/ethnic group. Liu et al. (2018) similarly found racial/ethnic differences in ACE latent classes, but they focused on the overall level of adversity (i.e., low, moderate, high) rather than the specific ACEs in each class. They found that Black and Hispanic youth experienced more adversity and worse subjective physical health.
We could find no study that used LCA to examine racial/ethnic differences in associations between ACEs and adolescent mental health. On the one hand, we might expect ACEs to have a stronger association with mental health for Black and Hispanic children because their racial status subjects them to the health-harming effects of racism, discrimination, and micro-aggressions (Grollman, 2012; Kessler et al., 1999; Williams et al., 1997). Stress process theory (Pearlin, 1989) would suggest that ACE exposure may compound or exacerbate the negative effects of everyday racialized stressors, leading to a stronger association with mental health for Black and Hispanic children than for White children. On the other hand, research finds that when exposed to adversity, Black young adults report better mental health and exhibit greater resilience than other racial/ethnic groups (Turner & Lloyd, 2003; Schilling et al., 2007; Youssef et al., 2017). Ultimately, if ACEs cluster differently by race/ethnicity and/or have differential associations with mental health outcomes, it would suggest the need for racially-tailored interventions for prevention and treatment.
The current study uses population-based data from a prospective U.S. urban birth cohort to answer the following research questions (RQ): (1) Which ACEs cluster together among adolescents, and are there racial/ethnic differences in ACE clustering? and (2) How do mental health outcomes vary across classes of ACE membership for non-Hispanic (NH) White, NH Black, and Hispanic adolescents? The current study addresses the limitations described above by including socioeconomic adversity along with traditional ACE measures (Cronholm et al., 2015; Mersky et al., 2017; Wade et al., 2014), using a “person-centered” LCA approach to understand how ACEs cluster together and how different clusters are associated with adolescent mental health, and examining differences between NH Whites, NH Blacks, and Hispanics in those associations.
2. Methods
2.1. Data
Data are from the Fragile Families and Child Wellbeing Study (FFCWS) that began in 2001. FFCWS is a longitudinal U.S. birth cohort study of parents and their children born in large cities with populations of 200,000 or more (Reichman et al., 2001). Mothers were first interviewed directly following the focal child's birth (Wave 1, 2001). Follow-ups were conducted when the child was approximately 1, 3, 5, 9 and 15 years old (Waves 2–6). Data for the most recent wave (Wave 6) were collected between 2014 and 2017. Our ACE measures were reported by parents during the Wave 5 follow-up when children were age 9. Our adolescent mental health outcome measures were collected from children during the Wave 6 follow-up when they were age 15. FFCWS oversamples single parent families. Accordingly, the sample is comprised of a larger share of low-income mothers and children relative to the general population. Given higher ACE exposure in low-income families (Walsh et al., 2019), our findings may not be generalizable to the overall population of children who live in large U.S. cities. Additional information regarding the FFCWS sampling procedures is available from Reichman et al. (2001).
The baseline sample included 4898 adolescents, which we restricted in several ways. First, we restricted the sample to adolescents whose mothers were surveyed at Wave 5 (N = 3515) and reported they lived with the target child for at least half of the time in the past year (N = 3290). We further limited the sample to adolescents who participated in the Wave 6 follow up and did not have missing data on our mental health indicators (N = 2956). Finally, due to small sample sizes for other racial/ethnic groups, we restricted our sample to NH Whites, NH Blacks, and Hispanics (N = 2849). The final analytic sample was 2849 adolescents and did not differ significantly on demographic measures from the baseline sample (baseline sample: mean [M]mother's age = 25.3, standard deviation [SD] = 6.1; Nmale = 2,556, 52%; analytic sample: Mmother's age = 25.2, SD = 6.0; Nmale = 1,009, 51%).
2.2. Outcomes
We examined two adolescent mental health outcomes at Wave 6 when the children were age 15 - self-reported depressive symptoms and anxiety. FFCWS administered a 5-item version of the Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977). Respondents indicated how they had been feeling in the past four weeks on five items measuring depressive symptoms on a 4-point scale ranging from strongly agree to strongly disagree. After reverse coding the single positively worded item (see Online Appendix Table 1), we summed responses to create a depressive symptoms index score, with possible scores ranging from 0 to 15 (Cronbach's α = 0.76). We measured anxiety using six items adapted from the Brief Symptom Inventory 18 (BSI 18) anxiety subscale originally developed to measure adolescents' psychological distress. Respondents were asked to think about the past four weeks and rate their agreement with each statement on a 4-point scale ranging from strongly agree to strongly disagree. We reverse coded and summed responses to create an anxiety index score with possible scores ranging from 0 to 18 (Cronbach's α = 0.76).
Table 1.
Descriptive statistics for analytic sample.
| Variables | Full Sample N=2849 | Non-Hispanic White N = 630 | Non-Hispanic Black N = 1478 | Hispanic N = 741 | p |
|---|---|---|---|---|---|
| Adolescent depressive symptoms | 4.06 (2.72) [0–15] | 3.70 (2.66) [0–13] | 4.14 (2.68) [0–14] | 4.21 (2.81) [0–15] | .001 |
| Adolescent anxiety | 4.83 (3.92) [0–18] | 4.71 (3.95) [0–18] | 4.76 (3.92) [0–18] | 5.10 (3.87) [0–18] | .10 |
| ACEs | |||||
| Parental separation or divorce | 68.1% | 46.2% | 80.2% | 62.6% | <.001 |
| Economic hardship | 65.4% | 40.5% | 74.4% | 68.4% | <.001 |
| Maternal low education | 42.6% | 29.2% | 40.7% | 57.9% | <.001 |
| Physical abuse | 22.7% | 19.8% | 28.1% | 14.2% | <.001 |
| Psychological abuse | 17.3% | 16.0% | 20.7% | 11.6% | <.001 |
| Parental depression | 16.5% | 17.9% | 17.1% | 14.2% | .12 |
| Neglect | 9.9% | 9.2% | 10.4% | 9.4% | .57 |
| Domestic violence | 5.0% | 3.3% | 4.0% | 8.4% | <.001 |
| Parental substance use | 30.2% | 30.3% | 29.8% | 30.9% | .85 |
| Paternal incarceration | 46.9% | 32.2% | 55.8% | 41.7% | <.001 |
| ACE count | 3.25 (1.78) | 2.48 (1.88) | 3.61 (1.66) | 3.19 (1.68) | <.001 |
| 0 | 7.3% | 18.1% | 3.5% | 5.7% | |
| 1 | 10.4% | 17.9% | 7.2% | 10.4% | |
| 2 | 15.7% | 18.9% | 13.6% | 17.1% | |
| 3 | 22.0% | 16.5% | 22.6% | 25.6% | |
| 4 | 20.8% | 12.9% | 24.3% | 20.8% | |
| 5 | 13.8% | 9.0% | 16.7% | 11.9% | |
| 6+ | 10.0% | 6.7% | 12.2% | 8.5% | |
| Mother's Characteristics | |||||
| Mother's age (baseline) | 25.20 (6.01) [15–43] | 27.51 (6.45) [15–43] | 24.35 (5.61) [15–43] | 24.92 (5.88) [15–43] | <.001 |
| Number of children under 18 | 2.74 (1.28) [1–8] | 2.54 (1.06) [1–7] | 2.83 (1.38) [1–8] | 2.73 (1.24) [1–7] | <.001 |
| Child Characteristics | |||||
| Sex | .79 | ||||
| Female | 48.9% | 47.9% | 48.8% | 49.8% | |
| Male | 51.1% | 52.1% | 51.2% | 50.2% |
Note. Table reports unweighted percentages or means (standard deviations) and [range]; p values are based on one-way ANOVA for continuous variables and chi-square tests for binary and categorical variables.
2.3. Exposures
We captured ACEs using ten indicators from Wave 5 when children were age 9. Six indicators were based on Felitti et al.’s (1998) landmark study: physical and psychological abuse and parental domestic violence, depression, substance use, and incarceration. Two indicators were from Anda et al.’s (2006) subsequent data collection: neglect and parental divorce/separation. Among our contributions to the literature is to include two additional indicators—economic hardship and maternal education—which have been found to have strong influences on children's mental health and which we use to capture socioeconomic adversity (Hughes et al., 2017). The FFCWS does not include sexual abuse by a household member. All ACEs in the FFCWS were parent-reported. A full list of ACEs we included, along with their operationalizations, is in Online Appendix Table 2.
Table 2.
Model fit of latent class analysis of childhood experiences by race.
| Race/Ethnicity | Model | BIC | Adj. LMR (p-value) |
|---|---|---|---|
| Full Sample (N =2849) | 1 Class | 28171.38 | – |
| 2 Classes | 27110.46 | 1145.85*** | |
| 3 Classes | 26733.54 | 459.18*** | |
| 4 Classes | 26675.86 | 143.54*** | |
| 5 Classes | 26698.53 | 64.10 | |
| 6 Classes | 26735.74 | 49.72 | |
| Non-Hispanic White (N = 630) | 1 Class | 6005.93 | – |
| 2 Classes | 5631.60 | 439.04*** | |
| 3 Classes | 5618.50 | 82.84 | |
| 4 Classes | 5642.83 | 45.92* | |
| 5 Classes | 5687.28 | 26.09^ | |
| 6 Classes | 5736.89 | 21.00** | |
| Non-Hispanic Black (N = 1478) | 1 Class | 14448.50 | – |
| 2 Classes | 14169.32 | 355.04*** | |
| 3 Classes | 13992.90 | 253.54* | |
| 4 Classes | 14025.06 | 47.53** | |
| 5 Classes | 14072.43 | 32.50 | |
| 6 Classes | 14125.15 | 27.23 | |
| Hispanic (N = 741) | 1 Class | 6945.82 | – |
| 2 Classes | 6839.90 | 176.19*** | |
| 3 Classes | 6792.73 | 118.23 | |
| 4 Classes | 6793.91 | 70.54^ | |
| 5 Classes | 6838.01 | 28.20* | |
| 6 Classes | 6882.77 | 31.43* |
Note. BIC=Bayesian Information Criterion. Adj. LMR-LRT = Adjusted Lo-Mendell-Rubin Likelihood Ratio Test. Boldface indicates best values for each model fit index. ***p < .001, **p < .01, *p < .05, ^p = .10.
Child abuse and neglect were assessed by subscales from the Parent Child Conflict Tactics Scales (Straus et al., 1998). Physical abuse (spanked, hit, slapped, shook), psychological abuse (threatened, called names, swore or cursed at child), and neglect (failure to provide supervision, unable to make sure child got to a doctor/hospital when needed) were each assessed with five items (see Online Appendix Table 2). Mothers were asked to identify how many times they engaged in each behavior in the past year. We recoded ‘has never happened’ and ‘has not happened in the past year’ to 0. To calculate maltreatment frequency, consistent with Straus (2001), we considered the midpoint of each category of each item and summed them. We then dichotomized the summed scores for each domain using the top 10th percentile score as a cutoff to indicate heavy/frequent abuse, a method used previously (Hunt et al., 2017; Zhang & Mersky, 2020).
Parental separation/divorce is a dichotomous variable indicating whether the biological parents were separated or divorced. Domestic violence perpetrated against the mother by the biological father or current partner was assessed by whether the child ever witnessed a physical fight between the mother and father or partner, or if the father or partner physically hurt the mother in front of the child. If the mother responded “yes” to either item, the child was exposed to domestic violence.
We measured parental depression with a dichotomous variable we created indicating whether the parent has a probable diagnosis of a major depressive episode in the past year. Parents were first asked about their feelings of dysphoria or anhedonia in the past year that lasted for two weeks or more, and if these symptoms occurred every day and for how long. If they endorsed the diagnostic screening questions, additional questions were asked to determine major depression (see Online Appendix Table 2 for questions, coding, and a note about sensitivity analyses for this measure).
Consistent with Felitti et al. (1998), we assessed parental substance use based on parents’ alcohol and drug use in the past year. Problem drinking was measured via an item asking parents how often they had 4 or more drinks in one day in the past 12 months. Based on the definition from National Institute on Alcohol Abuse and Alcoholism NIAAA (2021), we categorized parents as problem drinker if they reported having at least four drinks daily every day or almost every day, a few times a week, or a few times a month. Parental drug use was measured by questions asking parents whether they had used five types of illicit drugs or misused four types of prescription drugs in the past year (see Online Appendix Table 2). If parents reported illicit drug use or prescription drug misuse, we coded them as having any drug use. If either parent was coded as having problem drinking or any drug use, we coded parental substance use as “yes”.
Economic hardship was based on the ratio of total household income to the official U.S. Census Bureau poverty thresholds based on family composition. We categorized families at 200% or below the income-to-needs ratio as having economic hardship (Shaefer et al., 2015). Maternal low education was based on mothers' self-reported education collected in Wave 5. Mothers with a high school degree or less were classified as “low education”. Paternal incarceration was assessed using mothers' reports of whether the child's biological father had spent time in jail.
2.4. Covariates
Consistent with prior students on demographic predictors of ACE exposure (Lanier et al., 2018; Lew & Xian, 2019; Liu et al., 2018), covariates included adolescent sex, maternal age at baseline, and number of children under 18 living in the household at Wave 5 when the ACE variables were captured. We do not control for child physical health, as it may be highly influenced by mental health and could raise endogeneity concerns.
2.5. Analytical strategy
We first presented descriptive statistics for the sample overall and by race/ethnicity to identify racial/ethnic variation in the prevalence of each ACE and the two mental health outcomes. We used one-way analysis of variance (ANOVA) for continuous variables and chi-square tests for binary and categorical variables when comparing racial/ethnic differences. We then used latent class analysis (LCA) to classify patterns of ACEs using Mplus Version 8 (Muthén and Muthén, 2017). LCA is a statistical model to identify unobserved heterogenous latent subgroups based on a set of observed categorical variables (Collins & Lanza, 2010; Nylund-Gibson & Choi, 2018). We used LCA to group individuals into latent classes based on the probabilities of response patterns to the ACEs. This procedure enables us to identify which ACEs cluster together among different groups of adolescents. LCA is methodologically appropriate for modelling ACEs, which are categorical and zero-inflated because LCA is a semiparametric technique that only assumes within-class normality and local independence (Feldman et al., 2019). We first estimated latent classes for the whole sample. However, we found that there were measurement invariances across racial/ethnic groups, suggesting it would be inappropriate to identify latent classes for the sample as a whole.
Accordingly, we estimated separate latent class models for each of the three racial/ethnic groups. This allowed us to determine whether ACEs cluster differently by race/ethnicity (RQ1). To identify the optimal number of latent classes, we began with a one-class model and proceeded to test models with successively more classes. The choice of the optimal number of classes was based on the comparison of various class-size models using the Schwarz's Bayesian Information Criteria (BIC) and the adjusted Lo–Mendell–Rubin likelihood ratio test (LMR; Lo et al., 2001). Monte Carlo simulation studies showed that LMR and BIC are the most reliable for selecting the optimal number of classes (Nylund-Gibson et al., 2007; Tofighi & Enders, 2008). A smaller BIC indicates better model fit, while LMR offers a p-value for model comparison between the k-1 and k classes. A p-value <.05 indicates that the k-class model is statistically better than the k-1 class model. The size of the latent classes and our judgment of model interpretability were also considered in the final decision about number of classes.
Next, we used the manual three-step BCH method (Bolck et al., 2004) to examine how class membership is associated with depression and anxiety for each racial/ethnic group, net of covariates (RQ2). We separately present associations between the covariates and class membership. The BCH approach provides less biased effect estimates compared to classify-analyze approaches because it takes into account classification uncertainty by using weights reflecting the measurement error of the latent class variable (see Asparouhov & Muthén [2014] for detailed description of the BCH method). A concern may be that our outcome variables are not normally distributed – one of the assumptions of BCH models. However, simulation studies have shown that the BCH method can yield unbiased estimates of the class-specific means of outcomes even when the underlying assumption of normality does not hold (e.g., Bakk & Vermunt, 2016).
We then used Wald tests to estimate the adjusted class-specific means of the outcome variables, and we conducted pairwise comparisons to determine whether the outcome variables between two classes are statistically different using the model constraint command in Mplus. Lastly, we used the full information maximum likelihood (FIML) estimation method for handling missingness at the enumeration stage, and listwise deletion at the last step of estimating the means of mental health outcomes with covariates as predictors of class membership and outcomes (Asparouhov & Muthén, 2014). Missing data on the ACE indicators ranged from 0 to 2.6%, and there were only 11 cases with missing values on covariates.
3. Results
3.1. Descriptive statistics
Sample characteristics are presented in Table 1. The unweighted average depressive symptoms and anxiety scores for the sample overall were 4.1 (SD = 2.7) and 4.8 (SD = 3.9), respectively. Scores ranged from 0 to 15 for depressive symptoms and 0 to 18 for anxiety. Average depression scores were 3.7 (SD = 2.7) for Whites, 4.1 (SD = 2.7) for Blacks, and 4.2 (SD = 2.8) for Hispanics. Average anxiety scores were 4.7 (SD = 4.0) for Whites, 4.8 (SD = 4.0) for Blacks, and 5.1 (SD = 3.9) for Hispanics.
In the sample overall, nearly 93% of adolescents experienced at least one of the ten ACEs in the past year. Parental separation/divorce, economic hardship, and paternal incarceration were the most common in all three racial/ethnic groups. Black mothers reported that their children experienced the highest mean ACE count (M = 3.6, SD = 1.7), followed by Hispanics (M = 3.2, SD = 1.7) and Whites (M = 2.5, SD = 1.9). The percentage of mothers reporting specific ACEs varied by racial/ethnic group. Black and Hispanic mothers were significantly more likely than White mothers to report parental separation/divorce, economic hardship, maternal low education, domestic violence, and paternal incarceration. Black mothers also reported significantly higher prevalence of physical abuse and psychological abuse than White and Hispanic mothers.
Weighted descriptive statistics are available in Online Appendix Table 3. Weighted values on depression and anxiety and ACE prevalence are lower than the unweighted values, reflecting the relative disadvantage of the FFCWS compared to adolescents in general. Despite these differences, the general trends observed in the weighted vs. unweighted samples are similar (for example, depression and anxiety scores are still lowest among NH Whites; ACE count is still highest among NH Blacks). We elected to not weight our analysis given that they are stratified by racial/ethnic group subsamples (consistent with Liu et al., 2018) and because we restricted our analysis to children living with mothers. As such, employing weights could introduce its own bias into the findings.
3.2. ACE latent classes
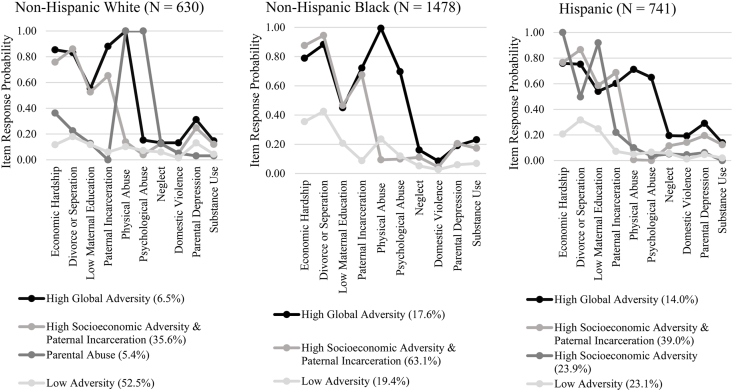
We fit models with one to five latent classes to cluster adolescents based on their experiences of adversity at age 9. We first estimated classes for all racial/ethnic groups together and found four distinct ACE classes (see top panel of Table 2 for full sample model fit information). However, measurement invariance tests of the 4-class model showed there were significant measurement differences across racial groups (Whites and Blacks: χ2[40] = 1467.94, p < .001, Whites and Hispanics: χ2[40] = 1890.80, p < .001, Blacks and Hispanics: χ2[40] = 1161.57, p < .001). Accordingly, we developed separate latent class models for each racial/ethnic group. Table 2 presents model fit information for the LCA models that helped inform the decision about how many classes sufficiently describe ACE heterogeneity. BIC and LMR p-values suggested a 4-class model for Whites and Hispanics and 3-classes for Blacks. Item-response probabilities and group membership prevalence values are presented in Fig. 1.
Fig. 1.
Item response probabilities and group membership prevalence for final LCA of adverse childhood experiences by race/ethnicity.
We labeled Class 1 as ‘High Global Adversity’, which included adolescents who experienced above average probabilities of physical and psychological abuse, economic hardship, parental separation/divorce, and paternal incarceration. Adolescents in this class also had higher probabilities than adolescents in the other classes of experiencing neglect, domestic violence, parental depression, and parental substance use (though the item response probabilities of these ACEs were comparatively low in all classes, including the ‘High Global Adversity’ class). We labeled Class 2 ‘High Socioeconomic (SES) Adversity and Paternal Incarceration’. Adolescents in this class had higher probabilities of experiencing family economic hardship, maternal low education, parental separation/divorce, and paternal incarceration relative to the other classes, but they had comparatively low probabilities of the other ACEs, notably physical and psychological abuse. Class 3 for NH Whites was the ‘Parental Abuse’ class, which was characterized by higher probabilities of only physical and psychological abuse. Class 3 for Hispanics was labeled as ‘High SES Adversity’, which included higher probabilities only of experiencing economic hardship, maternal low education, and parental separation/divorce. The final class for all three racial/ethnic groups was defined as ‘Low Adversity’ since probabilities for most ACEs were low.
3.3. Racial/ethnic variation in ACE class membership
There was important racial/ethnic variation in ACE class membership. Most White adolescents (52.5%) fell into the ‘Low Adversity’ class. The ‘High SES Adversity and Paternal Incarceration’ class was the next most common among Whites (35.6%). Only 6.5% of Whites were included in the ‘High Global Adversity’ class, and 5.4% were in the ‘Parental Abuse’ class. A much larger percentage of Black adolescents were in the ‘High SES Adversity and Paternal Incarceration’ class (63.1%), followed by the ‘Low Adversity’ class (19.4%), and ‘High Global Adversity’ class (17.6%). Over one third of Hispanic adolescents fell into the ‘High SES Adversity and Paternal Incarceration’ class (39.0%), 23.9% were in the ‘High SES Adversity’ (without paternal incarceration) class, 23.1% were in the ‘Low Adversity’ class, and 14% were in the ‘High Global Adversity’ class.
Appendix Table 4 shows odds ratios (ORs) including 95% confidence intervals of the association between covariates and latent class membership. White and Black adolescents with older mothers had lower odds of being classified in each of the respective adversity classes compared to the ‘Low Adversity’ class (ORs ranged from 0.78 to 0.96). Having more young children in the household increased the odds of being in the ‘High Global Adversity’ and ‘High SES Adversity and Paternal Incarceration’ classes relative to the ‘Low Adversity’ class among Blacks (OR = 1.23 and 1.33) but decreased the odds of being in the ‘High SES Adversity and Paternal Incarceration’ among Hispanics (OR = 0.90). Adolescent sex was significant only for Hispanics; being female increased the odds of being in all three adversity classes compared to the ‘Low Adversity’ class (ORs ranged from 1.54 to 1.64).
3.4. ACE class membership and adolescent mental health
Finally, we examined whether ACE latent class membership at age 9 was associated with depressive symptoms and anxiety at age 15 (RQ2). Models include the covariates noted earlier.
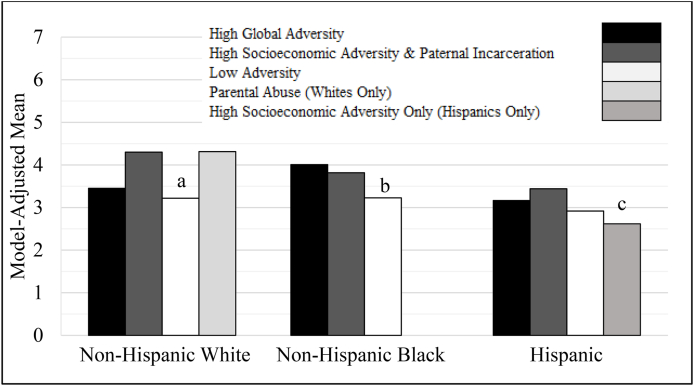
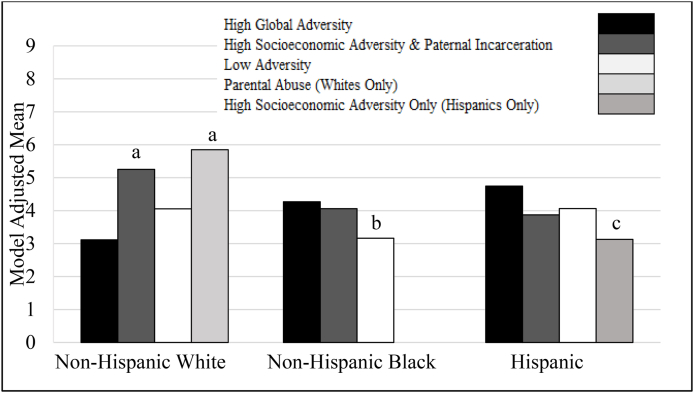
Fig. 2, Fig. 3 show model-adjusted means for depressive symptom and anxiety scores. Online Appendix Tables 5 and 6 show differences in mean scores by race/ethnicity and ACE class membership. White adolescents in the ‘Low Adversity’ class have a significantly lower model-adjusted mean depressive symptoms score (by about 1.1 points on a scale with a max of 13 for Whites) (M = 3.2, standard error [SE] = 0.8) than their peers in both the ‘High SES Adversity and Paternal Incarceration’ class (M = 4.3, SE = 0.6, p < .01) and the ‘Parental Abuse’ class (M = 4.3, SE = 0.9, p < .05) (Fig. 2). In terms of anxiety (Fig. 3), Whites in the ‘High SES Adversity and Paternal Incarceration’ class have an average depressive symptom score of 5.3 (SE = 0.9), which is 2.2 points higher than those in the ‘High Global Adversity’ class (M = 3.1, SE = 1.1, p < .01) and 1.2 points higher than their peers in the ‘Low Adversity’ class (M = 4.1, SE = 1.1, p < .05). Those in the ‘Parental Abuse’ class also have a significantly higher mean anxiety score (M = 5.9, SE = 1.2) than those in the ‘High Global Adversity’ class (M = 3.1, SE = 1.1, p < .01) and those in the ‘Low Adversity’ class (M = 4.1, SE = 1.1, p < .05).
Fig. 2.
Mean Depressive Symptoms at age 15 by ACE Class Membership and Race/Ethnicity
Notes: Means are model adjusted for mother's age, number of children under 18 in household, and adolescent sex. Unweighted. a = Among non-Hispanic Whites, the average depression score is significantly lower for those in the ‘Low Adversity’ class than both the ‘High Socioeconomic Adversity & Paternal Incarceration’ (p < .01) and ‘Parental Abuse’ classes (p < .05). b = Among non-Hispanic Blacks, the average depression score is significantly lower for those in the ‘Low Adversity’ class than those in either of the other two classes (p < .05). c = Among Hispanics, the average depression score is lower for those in the ‘High Socioeconomic Adversity’ class than the ‘High Socioeconomic Adversity & Paternal Incarceration’ class, but the difference is significant only at p < .10.
Fig. 3.
Mean Anxiety Score at age 15 by ACE Class Membership and Race/Ethnicity
Note. Means are model adjusted for mother's age, number of children under 18 in household, and adolescent sex. Unweighted. a = Among non-Hispanic Whites, the mean anxiety scores among those in the ‘High Socioeconomic Adversity & Paternal Incarceration’ class and the ‘Parental Abuse’ class are significantly higher than either the ‘High Global Adversity’ class (p < .01) or ‘Low Adversity’ class (p < .05). b = Among non-Hispanic Blacks, the mean anxiety scores among those in both the ‘High Global Adversity’ class and ‘High Socioeconomic Adversity & Paternal Incarceration’ class are significantly higher than the ‘Low Adversity’ class (p < .05). c = Among Hispanics, the mean anxiety score among those in the ‘High Global Adversity’ is significantly higher than the ‘High Socioeconomic Adversity’ class (p < .05).
Among Black adolescents, model-adjusted mean depressive symptom and anxiety scores were significantly higher for those in the ‘High SES Adversity and Paternal Incarceration’ (depression: M = 3.8, SE = 0.4; anxiety: M = 4.1, SE = 0.6) and ‘High Global Adversity’ classes (depression: M = 4.0, SE = 0.4; anxiety: M = 4.3, SE = 0.6) than those in the ‘Low Adversity’ class (depression: M = 3.2, SE = 0.5; anxiety: M = 3.2, SE = 0.7). However, the differences in average depression and anxiety scores across ACE groups for Blacks were smaller than the differences in scores across ACE groups for Whites (less than 1 point for depression scores and around 1 point for anxiety scores).
Finally, Hispanic adolescents in the ‘High SES Adversity’ class reported lower depressive symptoms scores (M = 2.6, SE = 0.8) than their peers in the ‘High SES Adversity and Paternal Incarceration’ class (M = 3.4, SE = 0.8), but this difference was small (less than 1 point) and was significant only at the p < .10 level. The only significant difference in anxiety scores for Hispanics was between the ‘High SES Adversity’ (M = 3.1, SE = 1.01) and the ‘High Global Adversity’ classes (M = 4.8, SE = 0.9) at the p < .05 level.
4. Discussion
This study used race-stratified latent class models to examine differences in the clustering of adverse childhood experiences (ACE) among NH White, NH Black, and Hispanic adolescents and to examine associations between ACE class membership at age 9 and adolescent depression and anxiety at age 15. Our study advances the literature on the relationship between ACEs and adolescent mental health by adding socioeconomic adversity to the traditional ACE measures, using a “person-centered” LCA approach to understand how ACEs cluster and how different clusters are associated with adolescent mental health, and examining association between ACE clusters and adolescent mental health outcomes for the three racial/ethnic groups. Several important findings emerged.
First, we found that about 93% of 9 year olds in the FFCWS sample had experienced at least one ACE in the past year. This is markedly higher than what has been reported in other studies (Anda et al., 2006; Bethell et al., 2014; Campbell et al., 2016; Monnat & Chandler, 2015; Sacks & Murphey, 2019), likely because the FFCWS oversamples low-income and single-mother families and because we included measures of economic hardship as ACE indicators. Over 65% of the sample experienced economic hardship, reflecting its importance in the lives of these children, with potential implications for their mental health throughout the life course. Consistent with previous studies (Maguire-Jack et al., 2020; Slopen et al., 2016), ACE prevalence was higher among Blacks and Hispanics than among Whites. Economic adversity measures that are not typically included in ACE studies were significantly and substantively more likely among Black and Hispanic adolescents than among White adolescents. These findings are consistent with fundamental cause theory (Link & Phelan, 1995) and support prior research suggesting that socioeconomic adversities that were not covered in the original ACE scale are important to consider especially when examining racial/ethnic differences in ACE exposure (Cronholm et al., 2015; Merskey; Janczewski, 2018; Slopen et al., 2016; Wade et al., 2014). Studies on the association between ACEs and health outcomes that do not include economic adversity risk underestimating the role of childhood adversity on later life health, particularly among racial/ethnic minorities.
Second, our findings add to the empirical base for understanding racial/ethnic differences in class membership of ACE exposure and demonstrate the diversity of contexts within which adolescents grow up. We found that a 4-class solution was the best fitting model for both White and Hispanic adolescents (though the fourth class was different for Whites vs. Hispanics), and a 3-class solution worked best for Black adolescents. Three of these classes were observed for all three racial/ethnic groups: ‘High Global Adversity’, ‘Low Adversity’, and ‘High SES Adversity with Paternal Incarceration’. A separate ‘Parental Abuse’ class was observed only for Whites, and a separate ‘High SES Adversity’ class without paternal incarceration was observed only for Hispanics. Researchers should be cautious when applying LCA to overall samples with subgroups that may have differential ACE exposures because the mechanisms driving exposures may vary across subgroups.
Our LCA results revealed important racial/ethnic differences in the clustering of ACEs. Over half of NH White adolescents were classified in the ‘Low Adversity’ class, characterized by below average probabilities of experiencing almost all ACEs. Conversely, most Black adolescents were classified in the ‘High SES Adversity and Paternal Incarceration’ class, characterized by above average probabilities of experiencing family economic hardship, parental separation, low maternal education, and paternal incarceration. Indeed, Black adolescents were almost twice as likely to be in this class than their White peers. Most Hispanic adolescents were split into either the ‘High SES Adversity and Paternal Incarceration’ class or the ‘High SES Adversity’ alone class.
Although it is difficult to compare findings related to class membership across studies that used different indicators, our findings at least partially align with those from prior studies (Liu et al., 2018; Maguire-Jack et al., 2020) that also found ACE class membership differences among Whites, Blacks, and Hispanics. Specifically, Maguire-Jack et al. (2020) found that the ‘Low Exposure’ class emerged in all three racial/ethnic groups. However, they did not find different proportions of ‘Low Exposure’ group membership by race/ethnicity, whereas we found that over half of Whites were in the ‘Low Adversity’ group compared to less than a quarter of Blacks and Hispanics. Consistent with Maguire-Jack et al. (2020), we found that a small share of adolescents from all three racial/ethnic groups were in the ‘High Global Adversity’ class, with Blacks having the highest and Whites having the lowest probability of membership in that class.
We expand on these previous studies that have examined racial/ethnic differences in ACE class membership by taking the next step to examine associations between ACE class membership and adolescent mental health outcomes – depression and anxiety. We found statistically significant, though meaningfully small differences in the association between ACE class membership and adolescent mental health for Blacks and Hispanics and marginally larger differences among Whites. Among Whites in particular, those classified in the ‘High SES Adversity and Paternal Incarceration’ group and in the ‘Parental Abuse’ group had significantly and meaningfully higher depression and anxiety scores than those in the ‘Low Adversity’ group. However, mean scores for those in the ‘High Global Adversity’ group were similar to those in the ‘Low Adversity’ group. This suggests there is something different about the experiences of the small share of White adolescents in the ‘High Global Adversity’ group (only 6.5%) that might somehow buffer them against deleterious mental health outcomes. Conversely, among Blacks, those in the ‘High Global Adversity’ group and the ‘High SES Adversity and Paternal Incarceration’ group had significantly higher mean depression and anxiety scores than those in the ‘Low Adversity’ group. However, the magnitude of these differences were relatively small (less than 1 point on scales of 15 and 18). Differences in mental health scores between ACE groups among Hispanics were also small. This may have to do with the nature of the FFCWS sample, which is comprised of comparatively disadvantaged families with comparatively high ACE prevalence. Samples comprised of more variability in ACE exposure and socioeconomic status may find larger differences. Small differences might also partially be due to the long time span (6 years) between the two waves of data.
Nevertheless, our finding that different patterns of ACE exposure are linked to different mental health outcomes among adolescents, and that these relationships vary by race/ethnicity, has important implications for intervention. Universal prevention and intervention programs that do not consider racial/ethnic differences in ACE clustering and differences in the relationship between ACE patterning and mental health outcomes might be ineffective in addressing mental health challenges. Intervention must be tailored to address the needs of the diverse adolescent population. Racially-tailored interventions to prevent ACEs or treat adolescents with a history of ACEs should also consider structural factors that might exacerbate poor mental health outcomes among racial/ethnic minority groups, such as internalized racism, racial prejudice and discrimination, and the U.S.'s historical legacy of structural racism (Williams & Sternthal, 2010).
4.2. Limitations
Results should be considered in light of limitations. First, the FFCWS data are self-reported and thus may be subject to underreporting. In particular, because ACEs are reported by mothers, substance use, domestic violence, and neglect may be underreported due to fears about criminal justice system or child protective service involvement. Second the FFCWS data do not include sexual abuse (an adversity that was included in the original Felitti et al., 's 1998 study). The data also do not include other types of adversities that can affect mental health and are more commonly experienced by racial/ethnic minorities than by Whites, such as neighborhood violence, racial/ethnic discrimination, and structural racism (Wade et al., 2014). Accordingly, our estimates of childhood adversity, while pronounced due to the nature of this sample, are actually conservative, particularly for Black and Hispanic children. Fourth, this study excluded several racial/ethnic minority groups with very small sample sizes. Fifth, data were from a predominantly low-income cohort born to unmarried mothers in large cities between 1998 and 2000, and we did not use survey weights because our analyses are stratified into three racial/ethnic group subsamples (Liu et al., 2018) and we restricted our analysis to children living with mothers. The unique nature of this sample and our decision to not employ weights means that our findings should not be viewed as generalizable, including to children in other cities and rural and suburban areas and children in more economically-advantaged families. ACE prevalence in our sample is much higher than in more representative studies, for example using data from the 2016 NSCH (Bethell et al., 2017). Finally, although we used two-waves of data across a six-year range to examine the relationship between ACE classes in childhood and mental health in adolescence, our findings should not be interpreted as causal.
5. Conclusion
ACEs are common in the U.S. and contribute to poor physical and mental health outcomes throughout the life course. This study suggests that adversities occur in meaningful clusters, and the likelihood of experiencing adversities, their clustering, and their association with depression and anxiety vary by race/ethnicity. Studies examining associations between ACEs and health outcomes that do not include economic adversity risk underestimating the role of childhood adversity on later life health, particularly among racial/ethnic minorities. Moreover, researchers should not assume universal relationships between ACE exposure and mental health outcomes because differences in anxiety and depression scores across different ACE exposure clusters appear to vary between Whites, Blacks, and Hispanics. Ultimately, these findings suggest the need for racially-tailored treatment and interventions to address the diverse adolescent population.
Ethical statement
We have reviewed the Ethics in Publishing and Ethical Guidelines for Journal Publication documents and confirm that we have abided by all ethical guidelines in the production of this manuscript. We have no competing interests or financial interests to disclose.
Author statement
Xiaoyan Zhang: Conceptualization, Methodology, Analysis, Writing – Original Draft, Writing – Review & Editing, Visualization. Shannon Monnat: Conceptualization, Methodology, Writing – Original Draft, Writing – Review & Editing, Visualization, Supervision, Funding Acquisition.
Declaration of competing interest
None.
Acknowledgements
Monnat acknowledges support from the National Institute on Aging (NIA) Interdisciplinary Network on Rural Population Health and Aging (R24AG065159), the NIA Network on Life Course Health Dynamics and Disparities (2R24AG045061), the Syracuse University Center for Aging and Policy Studies, which receives center funding from the NIA (P30AG66583), and the Population Research Institute at Penn State, which receives center funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (P2CHD041025). Both authors acknowledge support from the Syracuse University Lerner Center for Public Health Promotion.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2021.100997.
Contributor Information
Xiaoyan Zhang, Email: xzhan147@syr.edu.
Shannon M. Monnat, Email: smmonnat@syr.edu.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Anda R.F., Felitti V.J., Bremner J.D., Walker K.D., Whitfield C., Perry B.D. The enduring effects of abuse and related adverse experiences in childhood: A convergence of evidence from neurobiology and epidemiology. European Archives of Psychiatry and Clinical Neuroscience. 2006;256(3):174–186. doi: 10.1007/s00406-005-0624-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asparouhov T., Muthén B. Auxiliary variables in mixture modeling: Three-step approaches using Mplus. Structural Equation Modeling. 2014;21:329–341. [Google Scholar]
- Bakk Z., Vermunt J.K. Robustness of stepwise latent class modeling with continuous distal outcomes. Structural Equation Modeling: A Multidisciplinary Journal. 2016;23(1):20–31. [Google Scholar]
- Bergman L.R., Magnusson D. A person-oriented approach in research on developmental psychopathology. Development and Psychopathology. 1997;9(2):291–319. doi: 10.1017/s095457949700206x. [DOI] [PubMed] [Google Scholar]
- Berzenski S.R., Yates T.M. Classes and consequences of multiple maltreatment: A person-centered analysis. Child Maltreatment. 2011;16(4):250–261. doi: 10.1177/1077559511428353. [DOI] [PubMed] [Google Scholar]
- Bethell C.D., Davis M.B., Gombojav N., Stumbo S., Powers K. 2017. October). Issue Brief: A national and across state profile on adverse childhood experiences among children and possibilities to heal and thrive.http://www.cahmi.org/projects/adverse-childhood-experiences-aces/ [Google Scholar]
- Bethell C.D., Newacheck P., Hawes E., Halfon N. Adverse childhood experiences: Assessing the impact on health and school engagement and the mitigating role of resilience. Health Affairs. 2014;33(12):2106–2115. doi: 10.1377/hlthaff.2014.0914. [DOI] [PubMed] [Google Scholar]
- Bolck A., Croon M., Hagenaars J. Estimating latent structure models with categorical variables: One-step versus three-step estimators. Political Analysis. 2004;12:3–27. [Google Scholar]
- Campbell J.A., Walker R.J., Egede L.E. Associations between adverse childhood experiences, high-risk behaviors, and morbidity in adulthood. American Journal of Preventive Medicine. 2016;50(3):344–352. doi: 10.1016/j.amepre.2015.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi J.K., Wang D., Jackson A.P. Adverse experiences in early childhood and their longitudinal impact on later behavioral problems of children living in poverty. Child Abuse & Neglect. 2019;98:104181. doi: 10.1016/j.chiabu.2019.104181. [DOI] [PubMed] [Google Scholar]
- Collins L.M., Lanza S.T. Vol. 718. Wiley; 2010. (Latent class and latent transition analysis: With applications in the social, behavioral, and health sciences). [Google Scholar]
- Cronholm P.F., Forke C.M., Wade R., Bair Merritt M., Davis M., Harkins-Schwarz M. Adverse childhood experiences: Expanding the concept of adversity. American Journal of Preventive Medicine. 2015;49:354–361. doi: 10.1016/j.amepre.2015.02.001. [DOI] [PubMed] [Google Scholar]
- Debowska A., Willmott D., Boduszek D., Jones A.D. What do we know about child abuse and neglect patterns of cooccurrence? A systematic review of profiling studies and recommendations for future research. Child Abuse & Neglect. 2017;70:100–111. doi: 10.1016/j.chiabu.2017.06.014. [DOI] [PubMed] [Google Scholar]
- Elmore A.L., Crouch E. The association of adverse childhood experiences with anxiety and depression for children and youth, 8 to 17 years of age. Academic Pediatrics. 2020;20(5):600–608. doi: 10.1016/j.acap.2020.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felitti V.J., Anda R.F., Nordenberg D., Williamson D.F., Spitz A.M., Edwards V., Koss M.P., Marks J.S. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. American Journal of Preventive Medicine. 1998;14(4):245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Finkelhor D., Shattuck A., Turner H., Hamby S. A revised inventory of adverse childhood experiences. Child Abuse & Neglect. 2015;48:13–21. doi: 10.1016/j.chiabu.2015.07.011. [DOI] [PubMed] [Google Scholar]
- Hagan M.J., Sulik M.J., Lieberman A.F. Traumatic life events and psychopathology in a high risk, ethnically diverse sample of young children: A person- centered approach. Journal of Abnormal Child Psychology. 2016;44(5):833–844. doi: 10.1007/s10802-015-0078-8. [DOI] [PubMed] [Google Scholar]
- Hughes K., Bellis M.A., Hardcastle K.A., Sethi D., Butchart A., Mikton C., Dunne M.P. The effect of multiple adverse childhood experiences on health: A systematic review and meta-analysis. The Lancet Public Health. 2017;2(8):e356–e366. doi: 10.1016/S2468-2667(17)30118-4. [DOI] [PubMed] [Google Scholar]
- Hunt T.K.A., Slack K.S., Berger L.M. Adverse childhood experiences and behavioral problems in middle childhood. Child Abuse & Neglect. 2017;67:391–402. doi: 10.1016/j.chiabu.2016.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalmakis K.A., Chandler G.E. Health consequences of adverse childhood experiences: A systematic review. Journal of the American Association of Nurse Practitioners. 2015;27(8):457–465. doi: 10.1002/2327-6924.12215. [DOI] [PubMed] [Google Scholar]
- Kessler R.C., Mickelson K.D., Williams D.R. The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. Journal of Health and Social Behavior. 1999;40(3):208–230. [PubMed] [Google Scholar]
- Lanier P., Maguire-Jack K., Lombardi B., Frey J., Rose R.A. Adverse childhood experiences and child health outcomes: Comparing cumulative risk and latent class approaches. Maternal and Child Health Journal. 2018;22(3):288–297. doi: 10.1007/s10995-017-2365-1. [DOI] [PubMed] [Google Scholar]
- Lew D., Xian H. Identifying distinct latent classes of adverse childhood experiences among US children and their relationship with childhood internalizing disorders. Child Psychiatry and Human Development. 2019;50(4):668–680. doi: 10.1007/s10578-019-00871-y. [DOI] [PubMed] [Google Scholar]
- Link B.G., Phelan J. Social conditions as fundamental causes of disease. Journal of Health and Social Behavior, Extra Issue. 1995:80–94. [PubMed] [Google Scholar]
- Liu S.R., Kia-Keating M., Nylund-Gibson K.L. Patterns of adversity and pathways to health among White, Black, and Latinx youth. Child Abuse & Neglect. 2018;86:89–99. doi: 10.1016/j.chiabu.2018.09.007. [DOI] [PubMed] [Google Scholar]
- Maguire-Jack K., Lanier P., Lombardi B. Investigating racial differences in clusters of adverse childhood experiences. American Journal of Orthopsychiatry. 2020;90(1):106–114. doi: 10.1037/ort0000405. [DOI] [PubMed] [Google Scholar]
- Masyn K.E. Measurement invariance and differential item functioning in latent class analysis with stepwise multiple indicator multiple cause modeling. Structural Equation Modeling. A Multidisciplinary Journal. 2017;24:180–197. [Google Scholar]
- McLachlan G., Peel D. John Wiley & Sons, Inc; 2000. Finite mixture models. Wiley Series in Probability and Statistics. [Google Scholar]
- McLaughlin K.A. Future directions in Childhood adversity and youth psychopathology. Journal of Clinical Child and Adolescent Psychology. 2016;45(3):361–382. doi: 10.1080/15374416.2015.1110823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mersky J.P., Janczewski C.E. Racial and ethnic differences in the prevalence of adverse childhood experiences: Findings from a low-income sample of U.S. women. Child Abuse & Neglect. 2018;76:480–487. doi: 10.1016/j.chiabu.2017.12.012. [DOI] [PubMed] [Google Scholar]
- Mersky J.P., Janczewski C.E., Topitzes J. Rethinking the measurement of adversity: Moving toward second-generation research on adverse childhood experiences. Child Maltreatment. 2017;22(1):58–68. doi: 10.1177/1077559516679513. [DOI] [PubMed] [Google Scholar]
- Monnat S.M., Chandler R.F. Long term physical health consequences of adverse childhood experiences. The Sociological Quarterly. 2015;56(4):723–752. doi: 10.1111/tsq.12107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén L.K., Muthén Β.Ο. Muthén & Muthén; Los Angeles, CA: 2017. Mplus user's guide: Statistical analysis with latent variables. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism NIAAA . 2021. Drinking levels defined.https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking [Google Scholar]
- Norman R.E., Byambaa M., De R., Butchart A., Scott J., Vos T. The long-term health consequences of child physical abuse, emotional abuse, and neglect: A systematic review and meta-analysis. PLoS Medicine. 2012;9(11) doi: 10.1371/journal.pmed.1001349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nylund-Gibson K.L., Asparouhov T., Muthén Β.Ο. Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling: A Multidisciplinary Journal. 2007;14(4):535–569. [Google Scholar]
- Nylund-Gibson K.L., Choi A.Y. Ten frequently asked questions about latent class analysis. Translational Issues in Psychological Science. 2018;4(4):440–461. [Google Scholar]
- O'Donnell M.L., Schaefer I., Varker T., Kartal D., Forbes D., Bryant R., Silove D., Creamer M., McFarlane A., Malhi G., Felmingham K., Van Hoof M., Hadzi-Pavlovic D., Nickerson A., Steel Z. A systematic review of person-centered approaches to investigating patterns of trauma exposure. Clinical Psychology Review. 2017;57:208–225. doi: 10.1016/j.cpr.2017.08.009. [DOI] [PubMed] [Google Scholar]
- Pearlin L.I. The sociological study of stress. Journal of Health and Social Behavior. 1989;30(3):241–256. [PubMed] [Google Scholar]
- Radloff L.S. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Reichman N.E., Teitler J.O., Garfinkel I., McLanahan S.S. Fragile families: Sample and design. Children and Youth Services Review. 2001;23(4/5):303–326. [Google Scholar]
- Sacks V., Murphey D. The prevalence of adverse childhood experiences, nationally, by state, and by race or ethnicity. Child Trends. 2019 https://www.childtrends.org/publications/prevalence-adverse-childhood-experiences-nationally-state-race-ethnicity [Google Scholar]
- Schilling E.A., Aseltine R.H., Gore S. Adverse childhood experiences and mental health in young adults: A longitudinal survey. BMC Public Health. 2007;7(30) doi: 10.1186/1471-2458-7-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slopen N., Shonkoff J.P., Albert M.A., Yoshikawa H., Jacobs A., Stoltz R.…Williams D.R. Racial disparities in child adversity in the U.S. American Journal of Preventive Medicine. 2016;50(1):47–56. doi: 10.1016/j.amepre.2015.06.013. [DOI] [PubMed] [Google Scholar]
- Straus M.A. Transaction Publishers; 2001. Beating the devil out of them: Corporal punishment in American families and its effects on children. [Google Scholar]
- Straus M.A., Hamby S.L., Finkelhor D., Moore D.W., Runyan D. Identification of child maltreatment with the Parent-Child Conflict Tactics Scales: Development and psychometric data for a national sample of American parents. Child Abuse & Neglect. 1998;22(4):249–270. doi: 10.1016/s0145-2134(97)00174-9. [DOI] [PubMed] [Google Scholar]
- Tofighi D., Enders C.K. In: Advances in latent variable mixture models. Hancock G.R., Samuelsen K.M., editors. Information Age; Greenwich, CT: 2008. Identifying the correct number of classes in growth mixture models; pp. 317–341. [Google Scholar]
- Turner R.J., Lloyd D.A. Cumulative adversity and drug dependence in young adults: Racial/ethnic contrasts. Addiction. 2003;98:305–315. doi: 10.1046/j.1360-0443.2003.00312.x. [DOI] [PubMed] [Google Scholar]
- Wade R., Shea J.A., Rubin D., Wood J. Adverse childhood experiences of low-income urban youth. Pediatrics. 2014;134(1):e13–e20. doi: 10.1542/peds.2013-2475. [DOI] [PubMed] [Google Scholar]
- Walsh D., McCartnery G., Smith M., Armour G. Relationship between childhood socioeconomic position and adverse childhood experiences (ACEs): A systematic review. Jornal of Epidemiology & Community Health. 2019;73:1087–1093. doi: 10.1136/jech-2019-212738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R., Sternthal M. Understanding racial-ethnic disparities in health: Sociological contributions. Journal of Health and Social Behavior. 2010;51(Suppl):S15–S27. doi: 10.1177/0022146510383838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R., Yan Y., Jackson J.S., Anderson N.B. Racial differences in physical and mental health: Socio-economic status, stress and discrimination. Journal of Health Psychology. 1997;2(3):335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- Youssef N.A., Belew D., Hao G., Wang X., Treiber F.A., Stefanek M., Yassa M., Boswell E., McCall W.V., Su S. Racial/ethnic differences in the association of childhood adversities with depression and the role of resilience. Journal of Affective Disorders. 2017;208:577–581. doi: 10.1016/j.jad.2016.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L., Mersky J.P. Bidirectional relations between adverse childhood experiences and children's behavioral problems. Child and Adolescent Social Work Journal. 2020 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.