Abstract
Objective:
The purpose of this study was to determine if early weight gain predicted remission at the end of treatment in a clinic sample of adolescents with anorexia nervosa (AN).
Method:
Sixty five adolescents with AN (mean age = 14.9 years, SD = 2.1), from two sites (Chicago n = 45; Columbia n = 20) received a course of manualized family-based treatment (FBT). Response to treatment was assessed using percent ideal body weight (IBW) with remission defined as having achieved ≥95% IBW at end of treatment (Session 20).
Results:
Receiver operating characteristic analyses showed that a gain of at least 2.88% in ideal body weight by Session 4 best predicted remission at end of treatment (AUC = 0.674; p = 0.024).
Discussion:
Results suggest that adolescents with AN, receiving FBT, who do not show early weight gain are unlikely to remit at end of treatment.
Keywords: adolescent anorexia nervosa, family-based treatment, early treatment response, receiver operating characteristic curves
Introduction
It has been suggested that eating disorder treatment research should work to disseminate information regarding the factors that influence response, rather than only reporting on the overall efficacy or effectiveness of a particular treatment.1 This is perhaps most relevant in the treatment of anorexia nervosa (AN), where identification of responders and non-responders to treatment is made more urgent by the myriad medical complications and relatively high mortality rates associated with the disorder.2 Treatment outcome studies for AN have focused on many possible factors that predict outcome. However, few published reports have provided meaningful information on treatment progress before the end of a treatment trial. Investigation of weight gain trajectory in adult patients with AN undergoing inpatient treatment has demonstrated that weight trajectory at Week 3 and Week 4 of the inpatient stay can accurately classify a majority of patients as responders or non-responders to treatment.3 Early response to treatment has also been shown to predict outcome in adults with binge eating disorder (BED)4,5 and bulimia nervosa (BN),6,7 as well as adolescents with BN.8 However, less is known about how early response may predict outcome in adolescents with AN.
In the only published report specifically investigating early response to outpatient treatment as a predictor of outcome in adolescent AN, Lock and colleagues9 found that weight gain by Session 2, 9, or 10 is predictive of positive outcome. These data were obtained in a randomized controlled trial (RCT) using family-based treatment for adolescent anorexia nervosa (FBT-AN). With the stringent inclusion criteria found in an RCT, however, the empirical question remains as to whether these findings would generalize to a more community-based sample. The current study seeks to expand these findings and examine the utility of early response in predicting outcome for a clinic sample of adolescents with AN10 and a sample from an open dissemination trial of FBT for adolescents with AN-spectrum disorders.11
Method
Participants
The sample consisted of 65 adolescents (89.2% female; mean age = 14.9 years, SD = 2.1; mean body mass index = 17.0, SD = 1.7; mean percent ideal body weight = 86.3, SD = 7.7; mean duration of illness = 13.8 months, SD = 12.5). The majority of participants were white (75.4%) and came from intact families (84.6%). All participants have been previously reported upon.10,11 Participants met full DSM-IV criteria for AN (70.8%) or a strict definition of partial AN (29.2%) [i.e., criterion A (weight ≤ 85% of expected) met in the recent past but recently achieved partial weight restoration through hospitalization prior to the initiation of outpatient treatment; or met DSM-IV criteria B-D and had engaged in significant dietary restriction, but was currently ≥ 85% of expected body weight]. Participants were consecutive admissions to one of the two outpatient eating disorders programs in university hospitals who received FBT-AN. All participants and their parents or legal guardians provided written informed consent for use of their data and study procedures were approved by the Institutional Review Board of The University of Chicago or Columbia University.
Measures
Weight (pounds) and height (inches) were measured to calculate participants’ percent ideal body weight (IBW) as derived from age- and sex-specific centers for disease control and prevention (CDC) growth charts for the United States.12 Remission from AN was defined as achieving at least 95% of IBW at end of treatment.9 In this sample, the mean number of sessions completed was 15.0 (SD = 5.7). For patients completing fewer than 20 sessions, %IBW was carried forward from the final session.
Procedure
All participants were seen following an initial intake appointment. Therapists were psychologists, psychiatrists, fellows in child and adolescent psychiatry, predoctoral psychology interns, or a master’s degree level child social worker. Treatment followed the published manual for FBT-AN.13
Statistical Analyses
Receiver operating characteristic (ROC) analyses were conducted to examine whether percent weight gain attained early in treatment was predictive of remission status. ROC analyses evaluated the association between percent IBW attained in Sessions 1 through 10 (the first half of treatment) and remission status at post-treatment. The relationship between percent IBW at each session and remission was evaluated using the ROC area under the curve (AUC) and corresponding 95% confidence interval. The AUC represents the probability that a randomly selected remitted patient would have a higher percent IBW at that session than a randomly selected non-remitted patient.
Results
Sixty-five participants were included in these analyses. There were no significant differences by site in terms of baseline characteristics or post-treatment outcome. A total of 31 patients (47.7%) achieved remission at end of treatment based upon a minimum of 95% IBW. The mean percent IBW at baseline was 89.7 (SD = 5.8) for the remitted group compared to 82.9 (SD = 6.9) for the non-remitted group (t63 = 4.35, p < 0.001). Those more likely to remit included males (85.7 vs. 43.1%, χ(1)2 = 4.55, p = 0.033), participants with a shorter duration of illness (9.7 vs. 17.6 years; t63 = 2.65, p < 0.010), and those with a sub-threshold AN diagnosis (73.7% vs. 37.0%; χ(1)2 = 7.27, p = 0.007).
To examine the association of early weight gain and subsequent remission, ROC analysis was conducted using weight gain as a percentage of baseline weight to standardize comparisons across individuals. ROC curves revealed that percent weight gain at Sessions 1, 3, and 4 was significantly associated with post-treatment remission status (all p < 0.05), with AUC values for those sessions ranging from 0.652 to 0.674 (refer Table 1). The strongest predictor of post-treatment remission was achievement of at least 2.88% weight gain by Session 4 (AUC = 0.674; p = 0.024). The ROC curve for percent weight gain at Session 4 is presented in Figure 1.
TABLE 1.
ROC analysis of percent weight gain to predict remission at end of treatment
| Session | AUC (95% CI) | Significance | % Weight Gain Cutpointa |
|---|---|---|---|
| 1 | 0.669 (0.538–0.800) | 0.019 | 0.05 |
| 2 | 0.572 (0.426–0.718) | 0.334 | 0.77 |
| 3 | 0.652 (0.513–0.790) | 0.042 | 1.61 |
| 4 | 0.674 (0.532–0.816) | 0.024 | 2.88 |
| 5 | 0.615 (0.464–0.766) | 0.143 | 3.72 |
| 6 | 0.619 (0.469–0.770) | 0.129 | 3.81 |
| 7 | 0.597 (0.446–0.749) | 0.217 | 5.53 |
| 8 | 0.629 (0.478–0.780) | 0.105 | 6.22 |
| 9 | 0.556 (0.397–0.715) | 0.486 | 7.50 |
| 10 | 0.547 (0.386–0.708) | 0.568 | 7.35 |
Cutpoint to achieve equal sensitivity and specificity.
FIGURE 1.
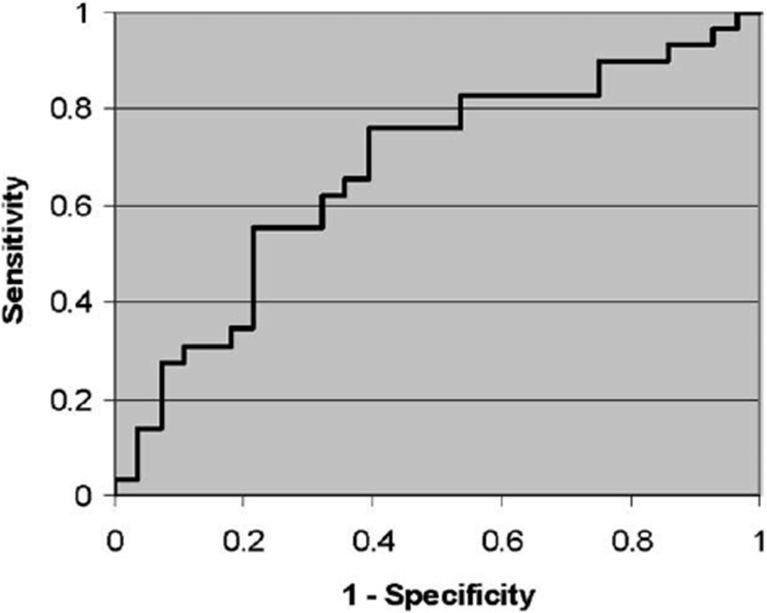
ROC curve of percent weight gain at Session 4 to predict remission at end of treatment.
Discussion
Weight gain by Session 4 of FBT predicts remission at post-treatment in adolescents with AN in a clinic sample. These findings are in concert with earlier work showing early weight gain predicted remission in a sample of adolescents treated as part of a RCT.9 Although there is a limited research reporting on early weight gain as a predictor of treatment response in AN, a growing body of literature shows that BN patients with early reductions in bingeing and purging and BED patients with early reductions in binge eating are more likely to respond at post-treatment. For instance, Fairburn et al.6 found that reduction in baseline purge frequency by 50% or greater at Week 4 (Session 6) predicted outcome at post-treatment and 8-month follow-up in adults with BN treated with either CBT or IPT. In adolescents with BN, Le Grange et al.8 showed that an 85% reduction in baseline binge eating and purging by Session 6 predicted outcome at post-treatment and 6-month follow-up. Similar results have also been found in adults with BED.4,5
There are a few limitations of the current study that should be noted. Outcome at Session 20 was established in terms of percent of ideal body weight with no concomitant psychological markers. Also, these findings need to be replicated in a larger sample of adolescents with AN. A strength of the study is that all participants received the same manualized treatment and this study contributes to what has been a dearth of literature examining early response in adolescents with AN. While one can speculate about the mechanisms of change in FBT-AN, our findings support the hypothesis that actively facilitating weight gain from the outset of treatment might have a positive impact on weight outcome. Alternatively, those families who engage in the protocol immediately and effectively may represent those who will continue to be successful over the course of treatment. Another strength is that we utilized clinical data from two specialist treatment sites. There were no differences between the samples from the two sites at either baseline or post-treatment, thereby strengthening the general-izability of our finding.
Future research is needed to determine if adolescents with AN who do not respond early on in FBT might benefit from an adjustment in this treatment approach or whether an alternative treatment approach should be considered. Alternatively, for those early responders, it remains unclear whether a full course of treatment is necessary.14 Dismantling studies may help clarify if there are specific treatment strategies presented in early sessions that may be particularly potent (e.g., empowering parents to make a united effort toward weight restoration, family meal). Further research is also needed to describe whether early non-responders may show certain characteristic profiles that are different from responders (e.g., single parent families, higher levels of obsessionality). Speculatively, early non-responders may have parents who are unable, at least initially, to confront the starvation head-on and perceive this treatment as less suitable or helpful for them and their families. Finally, this study underscores the importance of rapid and early weight gain in the treatment of adolescents with AN being associated with the likelihood of a good outcome.
Acknowledgments
Work on this paper was supported in part by grants from the NIMH (R01MH070620, PI: le Grange) and the NIH (K23MH074506, PI: Loeb).
References
- 1.Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Arch Gen Psychiatry 2002;59:877–883. [DOI] [PubMed] [Google Scholar]
- 2.Mitchell JE, Crow S. Medical complications of anorexia nervosa and bulimia nervosa. Curr Opin Psychiatry 2006;19:438–443. [DOI] [PubMed] [Google Scholar]
- 3.Hartmann A, Wirth C, Zeeck A. Prediction of failure of inpatient treatment of anorexia nervosa from early weight gain. Psychother Res 2007;17:218–229. [Google Scholar]
- 4.Grilo CM, Masheb RM, Wilson GT. Rapid response to treatment for binge eating disorder. J Consult Clin Psychol 2006;74:602–613. [DOI] [PubMed] [Google Scholar]
- 5.Grilo CM, Masheb RM. Rapid response predicts binge eating and weight loss in binge eating disorder: Findings from a controlled trial of orlistat with guided self-help cognitive behavioral therapy. Behav Res Ther 2007;45:2537–2550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fairburn CG, Agras WS, Walsh BT, Wilson GT, Stice E. Prediction of outcome in bulimia nervosa by early change in treatment. Am J Psychiatry 2004;161:2322–2324. [DOI] [PubMed] [Google Scholar]
- 7.Walsh BT, Sysko R, Parides MK. Early response to desipramine among women with bulimia nervosa. Int J Eat Disord 2006;39:72–75. [DOI] [PubMed] [Google Scholar]
- 8.Le Grange D, Doyle P, Crosby R, Chen E. Early response to treatment in adolescent bulimia nervosa. Int J Eat Disord 2008;41: 755–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lock J, Couturier J, Bryson S, Agras WS. Predictors of dropout and remission in family therapy for adolescent anorexia nervosa in a randomized clinical trial. Int J Eat Disord 2006;39:639–647. [DOI] [PubMed] [Google Scholar]
- 10.Le Grange D, Binford R, Loeb K. Manualized family-based treatment for anorexia nervosa: A case series. J Am Acad Child Adolesc Psychiatry 2005;44:41–46. [DOI] [PubMed] [Google Scholar]
- 11.Loeb KL, Walsh BT, Lock J, Le Grange D, Jones J, Marcus S. Open trial of family-based treatment for full and partial anorexia nervosa in adolescence: Evidence of successful dissemination. J Am Acad Child Adolesc Psychiatry 2007;46:792–800. [DOI] [PubMed] [Google Scholar]
- 12.National Center for Health Statistics. Health, United States, 2004 with chart book on trends in the health of Americans. Hyattsville, Maryland: Public Health Service, 2004. [Google Scholar]
- 13.Lock J, Le Grange D, Agras WS, Dare C. Treatment manual for anorexia nervosa: A family-based approach. New York: Guilford Press, 2001. [Google Scholar]
- 14.Lock J, Agras WS, Bryson S, Kraemer H. A comparison of short- and long-term family therapy for adolescent anorexia nervosa. J Am Acad Child Adolesc Psychiatry 2005;44:632–639. [DOI] [PubMed] [Google Scholar]


